Abstract
Genetic testing for chronic disease susceptibility may motivate young adults for preventive behavior change. This nationally representative survey gave 521 young adults hypothetical scenarios of receiving genetic susceptibility results for heart disease, type 2 diabetes, and stroke and asked their (1) interest in such testing, (2) anticipated likelihood of improving diet and physical activity with high- and low-risk test results, and (3) readiness to make behavior change. Responses were analyzed by presence of established disease-risk factors. Respondents with high phenotypic diabetes risk reported increased likelihood of improving their diet and physical activity in response to high-risk results compared with those with low diabetes risk (odds ratio (OR), 1.82 (1.03, 3.21) for diet and OR, 2.64 (1.24, 5.64) for physical activity). In contrast, poor baseline diet (OR, 0.51 (0.27, 0.99)) and poor physical activity (OR, 0.53 (0.29, 0.99)) were associated with decreased likelihood of improving diet. Knowledge of genetic susceptibility may motivate young adults with higher personal diabetes risk for improvement in diet and exercise, but poor baseline behaviors are associated with decreased intention to make these changes. To be effective, genetic risk testing in young adults may need to be coupled with other strategies to enable behavior change.
Electronic supplementary material
The online version of this article (doi:10.1007/s12687-013-0140-6) contains supplementary material, which is available to authorized users.
Keywords: Genetic testing, Young adults, Chronic disease, Health behaviors, Prevention
Introduction
Common conditions, such as cardiovascular disease and type 2 diabetes cause significant morbidity and mortality in adulthood (Centers for Disease Control and Prevention 2011a, b). Early improvements in diet and exercise could have significant impact on preventing the onset and reducing the impact of these chronic diseases (Hu et al. 1999; Hu et al. 1997, 2001; Lloyd-Jones et al. 2007; Liu et al. 2012). Improving health behaviors among young adults therefore represents an important strategy for reducing the risk and burden of future morbidity (Hankinson et al. 2010; Liu et al. 1996; Pereira et al. 2005).
Because adherence to recommended diet and physical activity guidelines remains low among many young adults (Leslie et al. 2001; American Heart Association and American Stroke Association 2011; Centers for Disease Control and Prevention 2012), new strategies are needed to target health behavior change and maintenance in this population. Advances in genetic technology have uncovered hundreds of genetic loci associated with an increased risk of many complex conditions (National Human Genome Research Institute 2012). The current literature does not support the general use of genetic risk information to motivate behavior change (Marteau et al. 2010; McBride et al. 2010; Grant et al. 2013). A recent review of the effects of communicating genetic susceptibility results found mixed evidence on whether such testing motivates smoking cessation or improvement in diet or physical activity (Marteau et al. 2010). However, it is unknown whether such genetic testing has unique motivational value for young adults. A recent Pew Research Center survey found that young adults scored particularly well on a brief science knowledge quiz, although performance varied by respondents’ demographics (Pew Research Center for the People and the Press and American Association for the Advancement of Science 2009). Thus, this scientifically knowledgeable population may find genetic risk information particularly engaging. There are high hopes that clinicians may be able to leverage this property to motivate the adoption and maintenance of healthy lifestyle choices. If this potential new clinical tool proves effective among young adults, it will be important that those at highest risk for chronic diseases are at least equally, if not more, motivated for behavior change by genetic information than their low- or average-risk peers. Perhaps more importantly, low-risk genetic results must not demotivate them away from healthy behaviors. Finally, one understudied question is whether young adults identify an ideal time in the life course when they might be most likely to translate such motivation into behavior change.
We conducted a nationally representative internet-based survey of adults 25 to 30 years old to assess their interest in genetic susceptibility testing for chronic disease and their anticipated motivation for improving diet and exercise upon learning high- or low-risk results from such a test. We then analyzed responses by known chronic disease risk factors to evaluate whether those with these risk factors might have greater benefit from such testing. Specifically, our study was designed to answer three questions: (1) are young adults interested in a test that could tell them their genetic susceptibility for chronic diseases, specifically, heart disease, type 2 diabetes, and stroke?; (2) do they anticipate that higher risk genetic results on such testing would motivate them to improve their dietary and physical activity habits?; and (3) if so, when in life do they think they would make these health behavior improvements? We then tested the hypothesis that respondents who already have established risk factors for these three chronic diseases (family history, obesity, and poor baseline diet and physical activity) would be more responsive to this genetic susceptibility testing. That is, (1) young adults with these risk factors would be more interested in such testing, (2) they would anticipate a greater likelihood of improving their health behaviors, and (3) they would be more likely to act on this risk information now.
Methods
Survey sample and administration
Young adulthood, particularly ages 18 to 25, is a dynamic and transitional period, as some pursue higher education, some start families, and some enter the workforce. To reduce the effect of these transitions, we chose to define young adulthood in this study as ages 25 to 30 years, instead of using lower ages. The survey was conducted online in August 2011 with a national probability sample of 971 adults ages 25 to 30 years from the overall Knowledge Networks (KN 2012) panel. KN recruits its research panel using probability sampling techniques designed to represent both online and offline US populations. Panel members have been recruited via random-digit dialing (RDD) telephone sampling in the past and currently by address-based sampling with recruitment by US mail. Multiple recruitment samples are fielded throughout the year to offset attrition in the overall panel. Individual survey samples, including the sample used for the present study, are drawn randomly from this overall panel. For the present survey, invitations to complete the survey were sent to random samples of eligible members (adults aged 25 to 30) of the overall KN panel until the target sample size was reached. Further details of the KN panel recruitment are available online (KN 2012). Of 971 surveys fielded for the present study, 521 were completed (completion rate, 54 % as defined by American Association for Public Opinion Research 2011 standards). This completion rate does not account for the nonresponse of people recruited to be in the overall KN panel and is thus not a true response rate. The survey instrument was developed by the researchers and was piloted using a convenience sample of 12 young adults (age range, 23–26 years). The final survey took a median of 5 min to complete. The Partners Human Research Committee approved this study.
Measurements
Respondents were given brief information about chronic disease risk (Textbox) and were then asked how interested they would be in “ever having [a] genetic test for these diseases,” with response choices including “not at all interested,” “somewhat interested,” or “very interested.” Asked to imagine a hypothetical scenario in which this genetic test indicated they had “a higher-than-average genetic risk of getting these diseases (diabetes, heart disease, and stroke),” respondents were next asked how they would change their diets (five choices from “much less likely to eat a healthy diet” to “much more likely to eat a healthy diet”) and physical activity (fives choices from “much less likely to exercise” to “much more likely to exercise”). They were also asked when they would make this change with responses ranging in 5-year increments from “now” to “more than 20 years from now.” Respondents were asked the same questions about a hypothetical scenario of getting “lower-than-average” risk susceptibility results. Half of the respondents saw the “higher-than-average” scenario first, and half saw the “lower-than-average” scenario first.”
Textbox: Information provided to survey respondents about chronic disease risk
| Please read the following statements about chronic diseases like diabetes, heart disease, and stroke | |
| Americans are at high risk for these diseases as they get older | |
| Here are the average ages when these diseases first occur: | |
| Type 2 (adult-onset) diabetes | 53 years |
| Heart attack | 68 years |
| Stroke | 70 years |
| These diseases are caused in part by genetics and in part by health behaviors | |
| You can reduce your overall risk for these diseases by eating a healthy diet, getting plenty of exercise, and not smoking | |
| A simple genetic test can give you information about your genetic risk for these diseases | |
KN collects self-reported age, gender, race/ethnicity, and educational attainment from panel participants. We additionally asked respondents whether any immediate family member (mother, father, sister, or brother) had the following conditions: diabetes, heart disease, or stroke. Respondents were asked to describe their leisure time physical activity (outside of work) over the past year as “more active,” “less active,” or “about the same” compared with “most men or women [their] age”(Centers for Disease Control and Prevention 2005). Similarly, to assess diet quality, respondents were asked whether their usual diet was “more healthy,” “less healthy,” or “about the same” compared with “most men or women [their] age”. Respondents self-reported their weight and height, from which body mass index (BMI) was calculated as weight (in kilograms)/(height (in meters))2.
To assess diabetes risk, we asked respondents whether they had been told by a health professional that they had high blood pressure or gestational diabetes. We categorized each participant’s risk of type 2 diabetes or pre-diabetes using the American Diabetes Association (ADA) Diabetes Risk Test (http://www.diabetes.org/diabetes-basics/prevention/diabetes-risk-test). This validated algorithm uses BMI, age, race, immediate family history of diabetes, and personal history of hypertension or gestational diabetes to categorize respondents as having low, medium, or high risk for type 2 diabetes (Heikes et al. 2008).
Statistical analyses
We used post-stratification weights to adjust for probability of selection, panel coverage and nonresponse and used these weights in all analyses and presentation of results (KN). These weights were calculated based on the original probabilities of being sampled for the overall panel (base weight) and then adjusted for nonresponse and noncoverage in overall panel membership and for the present survey (post-stratification weight), based on the June 2011 Current Population Survey (US Census Bureau 2012).
We used weighted χ2 and t tests to compare categorical and continuous measures, respectively. If a χ2 test was found to be significant at p < 0.05 for a comparison of more than two groups (e.g., among the four race categories), then individual two-by-two χ2 tests against a reference group were used to detect specific between-group differences. Because of the distribution of responses to the hypothetical testing scenarios, we used weighted logistic regression to model the odds of being “much more likely” to improve one’s diet or physical activity in response to high-risk results and being “much less” or “somewhat less likely” to improve diet or physical activity with low-risk results. We performed univariate analyses and analyses adjusted for sex, race/ethnicity, educational attainment, and the self-reported baseline quality of the behavior in question (diet or physical activity). Among the subset of respondents anticipating improving their health behaviors, we performed similar logistic regression models for the odds of making that change now vs. five or more years from now. All tests were two-sided and presumed significant at α = 0.05. All analyses were performed on SAS v. 9.3 software (SAS, Inc., Cary, NC).
Results
Respondent characteristics
The mean (SE) age of the 521 respondents was 27.5 (0.1) years. About 50 % were men, 13 % were non-Hispanic black, and 19 % were Hispanic (Table 1). Thirty percent were obese (BMI ≥ 30 kg/m2), and an additional 32 % were overweight (BMI ≥ 25 kg/m2 and <30 kg/m2). Thirty-seven percent reported having a first-degree family member with heart disease, diabetes, or stroke, and 25 % were at medium or high ADA risk for type 2 diabetes. Compared with respondents, nonrespondents were more likely to have lower educational attainment but did not otherwise differ by age, sex, or race (Supplemental Table 1).
Table 1.
Interest in genetic susceptibility testing for chronic diseases among young adults
| Total (%) | Not interested (33 %) | Somewhat interested (47 %) | Very interested (20 %) | P value** | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 50 | 32 | 50 | 18 | 0.21 |
| Female | 50 | 33 | 44 | 23 | |
| Race/ethnicity | |||||
| Non-Hispanic white | 60 | 33 | 52 | 15 | Ref |
| Non-Hispanic black | 13 | 30 | 30 | 40 | <0.001 |
| Hispanic | 19 | 30 | 40 | 30 | 0.01 |
| Non-Hispanic other | 8 | 24 | 66 | 10 | 0.25 |
| Education | |||||
| High school or less | 39 | 34 | 40 | 26 | 0.16 |
| Some college or association degree | 29 | 35 | 48 | 17 | |
| ≥Bachelor degree | 32 | 29 | 54 | 17 | |
| Diet | |||||
| More healthy | 33 | 27 | 52 | 21 | 0.93 |
| Average | 43 | 33 | 46 | 21 | |
| Less healthy | 24 | 40 | 41 | 19 | |
| Physical activity | |||||
| More active | 28 | 28 | 52 | 20 | 0.88 |
| Average | 38 | 34 | 44 | 22 | |
| Less active | 34 | 35 | 46 | 19 | |
| Body mass index | |||||
| <25 kg/m2 | 38 | 31 | 50 | 19 | 0.84 |
| 25–30 kg/m2 | 32 | 37 | 43 | 20 | |
| ≥30 kg/m2 | 30 | 30 | 48 | 22 | |
| Heart disease, diabetes, or stroke family history* | |||||
| No | 64 | 37 | 45 | 18 | 0.21 |
| Yes | 36 | 26 | 50 | 24 | |
| ADA risk for diabetes | |||||
| Low | 75 | 33 | 46 | 21 | 0.92 |
| Medium or high | 25 | 31 | 49 | 20 | |
Data are survey-weighted percentages from the 521 respondents except for items with missing data: BMI (n = 519), family history of diabetes (n = 519), family history of heart disease (n = 519), family history of stroke (n = 519), diet (n = 519), and physical activity (n = 520). The survey-weighted mean (standard error) age of the respondents was 27.5 (0.1) years
*P < 0.05 in sample-weighted χ2 tests comparing those not interested vs. those somewhat or very interested; **P value corresponds to sample-weighted χ2 tests comparing those not interested or somewhat interested vs. those very interested
Interest in genetic testing
Two thirds of respondents reported at least some interest in a test that could tell them their genetic risk for heart disease, type 2 diabetes, and stroke (Table 1). Individuals with a first-degree family history of at least one of the three conditions were more likely to report at least some interest than those without family history (p < 0.05). Compared with non-Hispanic whites, non-Hispanic blacks and Hispanics were more likely to be very interested in the test (15, 40, and 30 % for whites, blacks, and Hispanics, respectively, p < 0.001 for blacks vs. whites and p = 0.01 for Hispanics vs. whites). Interest in the test did not differ by any other chronic disease risk factor examined. Interest in the test had a modest positive correlation with anticipated likelihood of improving one’s diet (Spearman’s coefficient, 0.28) and physical activity (Spearman’s coefficient, 0.30, p < 0.05 for both correlations).
Anticipated behavior change from hypothetical high-risk test results
Anticipated dietary change
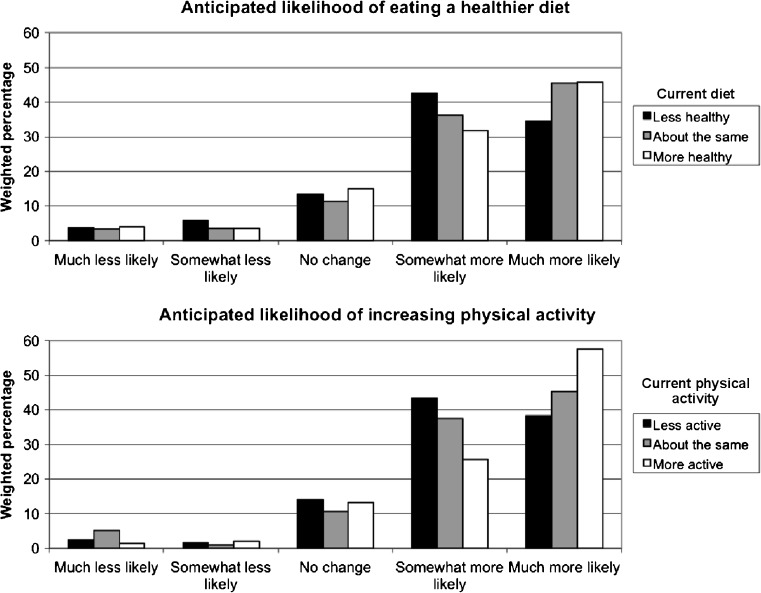
When given hypothetical high-risk genetic results for heart disease, type 2 diabetes, and stroke, 79 % of respondents said they would be “somewhat” or “much more” likely to eat a healthy diet (Fig. 1). This proportion did not vary significantly by sex, race/ethnicity, or educational attainment (p > 0.05 for all χ2 analyses). However, compared with all other respondents, individuals who anticipated that high-risk genetic results for type 2 diabetes would make them “much more likely” to eat a healthy diet were more likely to be women (OR vs. men, 1.62 (95 % CI, 1.05), 2.51), be black or Hispanic, and have a high school education or lower (OR vs. college degree or higher, 1.96 (95 % CI, 1.18), 3.26). In adjusted models, anticipating being “much more likely” to eat a healthy diet did not differ by BMI category or family history, but respondents in the medium or high ADA risk category were more likely to anticipate being “much more likely” to eat a healthy diet (Table 2). However, those with poorer-than-average dietary habits were half as likely as those with better-than-average dietary habits to anticipate that high-risk genetic results would make them “much more likely” to eat a healthy diet (OR, 0.51 (95 % CI, 0.27), 0.99). Similarly, those reporting poorer-than-average physical activity were less likely to anticipate being “much more likely” to eat a healthy diet, compared with those with better-than-average physical activity (OR, 0.53 (95 % CI, 0.29), 0.99).
Fig. 1.
Anticipated likelihood of improving health behaviors in response to high-risk genetic susceptibility for chronic disease, stratified by current self-reported health behaviors
Table 2.
Anticipated likelihood of improving health behaviors in response to high-risk genetic susceptibility for chronic diseases
| Diet | Physical activity | |||
|---|---|---|---|---|
| OR (95 % CI) | AOR (95 % CI) | OR (95 % CI) | AOR (95 % CI) | |
| Race | ||||
| Non-Hispanic white | Ref | Ref | Ref | Ref |
| Non-Hispanic black | 2.40* (1.18, 4.90) | 2.32* (1.13, 4.76) | 2.50 (0.90, 6.92) | 2.36 (0.84, 6.57) |
| Hispanic | 2.70* (1.44, 5.05) | 2.53* (1.33, 4.80) | 1.16 (0.56, 2.44) | 1.12 (0.51, 2.48) |
| Non-Hispanic other | 0.69 (0.30, 1.55) | 0.73 (0.31, 1.74) | 0.62 (0.27, 1.42) | 0.66 (0.29, 1.51) |
| Current diet | ||||
| Poorer than average | 0.63 (0.34, 1.18) | 0.51* (0.27, 0.99) | 0.81 (0.39, 1.68) | 0.75 (0.36, 1.57) |
| Average | 0.99 (0.61, 1.62) | 1.02 (0.62, 1.68) | 1.08 (0.59, 1.98) | 1.09 (0.57, 2.08) |
| Better than average | Ref | Ref | Ref | Ref |
| Current physical activity | ||||
| Poorer than average | 0.50* (0.29, 0.86) | 0.53* (0.29, 0.99) | 0.90 (0.46, 1.75) | 0.86 (0.44, 1.69) |
| Average | 0.75 (0.43, 1.29) | 0.64 (0.36, 1.14) | 0.97 (0.50, 1.87) | 0.96 (0.49, 1.87) |
| Better than average | Ref | Ref | Ref | Ref |
| BMI category | ||||
| <25 kg/m2 | Ref | Ref | Ref | Ref |
| 25–30 kg/m2 | 0.66 (0.39, 1.13) | 0.62 (0.36, 1.07) | 0.89 (0.49, 1.64) | 0.88 (0.47, 1.64) |
| ≥30 kg/m2 | 1.35 (0.80, 2.28) | 1.30 (0.71, 2.38) | 2.15* (1.08, 4.28) | 2.18* (1.03, 4.62) |
| Family history of chronic disease | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 1.13 (0.70, 1.82) | 1.05 (0.64, 1.74) | 1.69 (0.96, 2.97) | 1.68 (0.93, 3.03) |
| ADA diabetes risk | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium or high | 1.60 (0.98, 2.63) | 1.82* (1.03, 3.21) | 2.45* (1.20, 5.03) | 2.64* (1.24, 5.64) |
Odds ratios (OR) and 95 % confidence intervals (CI) correspond to weighted logistic regression models predicting being “much more likely” to improve diet or physical activity. Adjusted OR (AOR) are adjusted for sex, race, educational attainment, and baseline diet or PA, respectively in each column
*p < 0.05
Anticipated physical activity change
In the hypothetical scenario, most respondents (83 %) said they would be “somewhat” or “much more likely” to increase their physical activity habits on receiving high-risk genetic results (Fig. 1). As with the anticipated change in dietary patterns, this proportion did not vary by sex, race/ethnicity, or educational attainment. In adjusted models, compared with those with a BMI < 25 kg/m2, respondents with a BMI ≥ 30 kg/m2 were about twice as likely to anticipate that high-risk genetic results would make them “much more likely” to increase their physical activity (Table 2). Family history of diabetes, poor baseline diet, and poor baseline physical activity were not associated with being “much more likely” to increase physical activity in this hypothetical scenario. Respondents in the medium or high ADA risk category more often anticipated being “much more likely” to increase physical activity, compared with the low-risk group.
Anticipated timing of behavior change
Of those who said they would be more likely to improve their diets (79 % of total) and physical activity (83 % of total), 93 and 94 %, respectively, said they would do so now, as opposed to five or more years from now (Supplemental Table 2). Anticipated timing of dietary or physical activity change did not significantly differ by any of the risk factors examined, although the data suggested that respondents with overweight, obesity, or poor baseline diets or physical activity were more likely to defer behavior change to five or more years from now.
Anticipated behavior change from hypothetical low-risk test results
Few respondents reported that low-risk genetic susceptibility results would make then “much” or “somewhat less likely” to improve their diets (7 %) and physical activity (6 %). Those in a race/ethnic group other than white, black, or Hispanic and those in the BMI of 25–30 kg/m2 category more often anticipated a lower likelihood of eating a healthier diet in this scenario (Supplemental Table 3).
Discussion
Cardiovascular disease and type 2 diabetes pose a significant burden for the US healthcare system and preventive efforts should antecede the age of peak incidence. There is clearly need for improvement in the health behaviors of young adults. Recent surveys indicate that 42 % of young adults do not meet recommendations for moderate or vigorous physical activity (Centers for Disease Control and Prevention 2012), while only 53 % report “eat[ing] to obtain or maintain a healthy weight” (American Heart Association and American Stroke Association 2011). Changing these health behaviors is difficult: the numerous barriers to improving physical activity and dietary behaviors among young adults include time and financial constraints and psychosocial and cultural influences (Myers and Roth 1997; Escoto et al. 2012; James 2004; Turk et al. 2012; Krist et al. 2010; Walsh et al. 2009; Greaney et al. 2009).
Behavior change intervention studies targeting the diet and exercise habits of young healthy adults have had mixed results over short follow-up periods (Tully and Cupples 2011; Hivert et al. 2007; Calfas et al. 2000; Gokee LaRose et al. 2010; Jeffery and French 1999; Levine et al. 2007; Eiben and Lissner 2005; Lee et al. 2011; Poobalan et al. 2010). Behavior change interventions personalized to the risk factors, needs, and preferences of individuals have had modest success in preventing weight gain (Gokee LaRose et al. 2010; Eiben and Lissner 2005; Lee et al. 2011). For example, one small trial demonstrated that a “customized support package” of diet and exercise education, tailored to individual circumstances, improved physical activity and prevented weight gain after 1 year among healthy Swedish women aged 18 to 28 (Eiben and Lissner 2005). Personalized genetic risk information may augment the individualization of such strategies in this difficult-to-target age group. We hypothesized that young adults would be interested in genetic testing for chronic disease susceptibility. Although the majority of our respondents was at least “somewhat interested,” it is noteworthy that one third reported they would be “not at all interested” in such a test, consistent with previous studies (McGuire et al. 2009; Sanderson et al. 2004). Importantly for prevention, interest in genetic susceptibility testing in the present study was not lower among those at greater risk for chronic disease and, indeed, was higher for those with a family history of chronic disease and those in high-risk race/ethnic groups (Hispanics and non-Hispanic blacks). This racial difference is particularly intriguing in light of prior work showing that African-Americans might be less interested in genetic susceptibility testing (Hipps et al. 2003) and be less likely to participate in genetic susceptibility testing research (Hensley Alford et al. 2011). Interest in genetic testing may correlate with behavior change (Sanderson et al. 2010), and, similar to previous research (McGuire et al. 2009), we found that about 80 % of young adults anticipated being more likely to improve their diets and physical activity patterns in response to higher genetic susceptibility results for heart disease, type 2 diabetes, and stroke.
If genetic susceptibility testing for chronic disease risk motivates young adults in general for healthy behavior change, it will be important for clinicians to know in particular whether those at greatest risk will be motivated. Here, our results were mixed. We found that individuals with self-reported poor diets and physical activity levels were less inclined to improve their diets, and a similar nonsignificant direction of effect was observed for improvement in physical activity. However, after adjustment for these baseline behaviors, those in certain high-risk groups (Hispanics, non-Hispanic blacks, the obese, and those in the medium or high ADA diabetes risk category) anticipated a greater likelihood of making behavior changes in response to such genetic results. Of respondents anticipating that high-risk results would increase their likelihood of improving their health behaviors, the majority said they would make those changes now instead of five or more years from now. Very few responded that they would defer those changes to a future time. However, our data suggest that those who are overweight or obese or have poor baseline behaviors might be more likely to defer such changes. Future study should replicate these findings, which may have important public health implications. Because most Americans do not meet recommended goals for physical activity and dietary quality (likely including those who responded that their habits were “about the same” as their peers), our results suggest that at-risk individuals might benefit from genetic susceptibility testing for chronic disease to motivate behavior change. However, it may be particularly difficult to motivate those with self-perceived poor habits in the targeted health behaviors. We did not find any evidence that low-risk genetic susceptibility results would meaningfully demotivate respondents for healthy behaviors.
The results must be interpreted in the context of the study design. Recruiting young adults for survey participation is difficult, and each method has its drawbacks: young adults are less likely to have landline telephones, reducing the effectiveness of traditional RDD telephone sampling; online panels have difficulty with representativeness and response rates; address-based sampling may be difficult in a mobile, transitional young population; and cell-phone-based samples are not yet proven effective (Sax et al. 2003; Kaplowitz et al. 2004). Our use of a nationally representative panel recruited by mail and telephone, in addition to the 54 % completion rate, may limit the generalizability of our results. Second, the anticipated behavior changes that respondents reported in our hypothetical scenario may not necessarily correlate with actual behavior change in the face of genetic susceptibility testing. For example, self-reported intention to undergo genetic testing, as assessed with hypothetical vignettes, usually over-estimates actual test uptake (Lerman et al. 2002; Persky et al. 2007). Less is known about the correlation between anticipated diet and exercise changes with hypothetical genetic test results and actual long-term changes in these health behaviors. Third, we described hypothetical scenarios in which respondents were told they had high or low genetic susceptibility for three chronic diseases. No such single test result exists, although the decreasing cost of genomic testing makes it increasingly likely that one can simultaneously receive risk information for multiple conditions. We chose three common chronic conditions that share risk factors present from young adulthood, but these analyses cannot distinguish whether respondents found individual conditions more or less compelling. Fourth, the quality of diet and physical activity was self-reported and may not accurately reflect true health behaviors.
Future studies should prospectively examine whether genetic susceptibility information motivates young adults to change their health behavior for chronic disease prevention. While a small evidence base of trial data shows mixed results on whether genotype information can improve health behaviors including smoking, alcohol use, and diet (McBride et al. 2010; Hendershot et al. 2010; Marteau et al. 2010; Grant et al. 2013), few studies have focused specifically on young adults (Hendershot et al. 2010). This target population will likely require compelling risk information to motivate behavior change during young adulthood. It is unknown whether genotype information might have particular salience for young adults, who are more likely to have greater genetic knowledge than older adults (Ashida et al. 2011). Moreover, because genotype is shared within families, it may facilitate health behavior change within social networks (Centola 2011; McBride et al. 2010). Because knowledge alone is not necessarily sufficient to effect health behavior change, further research will need to examine how genetic risk information might interact with the barriers to physical activity and dietary improvement faced by young adults face, particularly those with poor baseline behaviors.
In summary, this study suggests that young adults at greater risk for future cardiovascular disease and type 2 diabetes may be receptive to genetic susceptibility information to help motivate that change. If prospective studies confirm these results, clinicians may be able to harness such genetic information to motivate young adults to achieve and maintain healthy behaviors, although such motivation will likely need to be coupled with interventions facilitating these changes, especially in individuals with the poorest diet and physical activity habits.
Electronic supplementary material
(PDF 65 kb)
(PDF 73 kb)
(PDF 83 kb)
Acknowledgments
JLV is supported by National Institutes of Health (NIH) National Research Service Award grant T32 HP12706 from the Health Resources and Services Administration and the by NIH Loan Repayment Program (National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)). RWG was supported by NIDDK R21DK084527: Using Genetic Risk Information to Enhance Diabetes Prevention. RCG was supported by R01HG02213, U01HG006500, K24AG027841, and R01HG005092. MFH is supported as a Research Scholar by the Fonds de la Recherche en Santé du Québec and as a Clinical Scientist by the Canadian Diabetes Association. This work was presented at the Society for General Internal Medicine national meeting in Orlando, FL, May 2012.
Conflict of interest
The authors declare that they have no conflicts of interest relevant to this study.
References
- American Association for Public Opinion Research (2011) Standard definitions: final dispositions of case codes and outcome rates for surveys. Available at http://www.aapor.org/Standard_Definitions2.htm
- American Heart Association, American Stroke Association (2011) 2011 Stroke Month Survey. Available at http://www.strokeassociation.org/STROKEORG/General/American-Stroke-Month-2011_UCM_426715_Article.jsp
- Ashida S, Goodman M, Pandya C, Koehly LM, Lachance C, Stafford J, Kaphingst KA. Age differences in genetic knowledge, health literacy and causal beliefs for health conditions. Public Health Genomics. 2011;14(4–5):307–316. doi: 10.1159/000316234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calfas KJ, Sallis JF, Nichols JF, Sarkin JA, Johnson MF, Caparosa S, Thompson S, Gehrman CA, Alcaraz JE. Project GRAD: two-year outcomes of a randomized controlled physical activity intervention among young adults. Am J Prev Med. 2000;18(1):28–37. doi: 10.1016/S0749-3797(99)00117-8. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2005) 2005–2006 National Health and Nutrition Examination Survey (NHANES) Physical Activity and Physical Fitness Questionnaire. Available at http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/sp_paq_d.pdf. Accessed 12 April 2012
- Centers for Disease Control and Prevention (2011a) Heart Disease and Stroke Fact Sheets. Avaialable at http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/index.htm. Accessed 12 April 2012
- National diabetes fact sheet: national estimates and general information of diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Centers for Disease Control and Prevention (2012) WEAT: Web enabled analysis tool for BRFSS analysis. Available at http://apps.nccd.cdc.gov/s_broker/WEATSQL.exe/weat/index.hsql. Accessed 10 April 2012
- Centola D. An experimental study of homophily in the adoption of health behavior. Science. 2011;334(6060):1269–1272. doi: 10.1126/science.1207055. [DOI] [PubMed] [Google Scholar]
- Eiben G, Lissner L. Health hunters-an intervention to prevent overweight and obesity in young high-risk women. Int J Obes. 2005;30(4):691–696. doi: 10.1038/sj.ijo.0803167. [DOI] [PubMed] [Google Scholar]
- Escoto KH, Laska MN, Larson N, Neumark-Sztainer D, Hannan PJ. Work hours and perceived time barriers to healthful eating among young adults. Am J Health Behav. 2012;36(6):786–796. doi: 10.5993/AJHB.36.6.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokee LaRose J, Tate DF, Gorin AA, Wing RR. Preventing weight gain in young adults: a randomized controlled pilot study. Am J Prev Med. 2010;39(1):63–68. doi: 10.1016/j.amepre.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RW, O'Brien KE, Waxler JL, Vassy JL, Delahanty LM, Bissett LG, Green RC, Stember KG, Guiducci C, Park ER, Florez JC, Meigs JB. Personalized genetic risk counseling to motivate diabetes rrevention: a randomized trial. Diabetes Care. 2013;36(1):13–19. doi: 10.2337/dc12-0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaney ML, Less FD, White AA, Dayton SF, Riebe D, Blissmer B, Shoff S, Walsh JR, Greene GW. College students' barriers and enablers for healthful weight management: a qualitative study. J Nutr Educ Behav. 2009;41(4):281–286. doi: 10.1016/j.jneb.2008.04.354. [DOI] [PubMed] [Google Scholar]
- Hankinson AL, Daviglus ML, Bouchard C, Carnethon M, Lewis CE, Schreiner PJ, Liu K, Sidney S. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304(23):2603–2610. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikes KE, Eddy DM, Arondekar B, Schlessinger L. Diabetes risk calculator: a simple tool for detecting undiagnosed diabetes and pre-diabetes. Diabetes Care. 2008;31(5):1040–1045. doi: 10.2337/dc07-1150. [DOI] [PubMed] [Google Scholar]
- Hendershot CS, Otto JM, Collins SE, Liang T, Wall TL. Evaluation of a brief web-based genetic feedback intervention for reducing alcohol-related health risks associated with ALDH2. Annals of behavioral medicine. Publ Soc Behav Med. 2010;40(1):77–88. doi: 10.1007/s12160-010-9207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley Alford S, McBride CM, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Participation in genetic testing research varies by social group. Public Health Genomics. 2011;14(2):85–93. doi: 10.1159/000294277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipps YG, Roberts JS, Farrer LA, Green RC. Differences between African Americans and Whites in their attitudes toward genetic testing for Alzheimer's disease. Genet Test. 2003;7(1):39–44. doi: 10.1089/109065703321560921. [DOI] [PubMed] [Google Scholar]
- Hivert MF, Langlois MF, Berard P, Cuerrier JP, Carpentier AC. Prevention of weight gain in young adults through a seminar-based intervention program. Int J Obes. 2007;31(8):1262–1269. doi: 10.1038/sj.ijo.0803572. [DOI] [PubMed] [Google Scholar]
- Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345(11):790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- Hu FB, Sigal RJ, Rich-Edwards JW, Colditz GA, Solomon CG, Willett WC, Speizer FE, Manson JE. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: A prospective study. JAMA. 1999;282(15):1433–1439. doi: 10.1001/jama.282.15.1433. [DOI] [PubMed] [Google Scholar]
- Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens CH, Willett WC. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med. 1997;337(21):1491–1499. doi: 10.1056/NEJM199711203372102. [DOI] [PubMed] [Google Scholar]
- James DC. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: application of a culturally sensitive model. Ethn Health. 2004;9(4):349–367. doi: 10.1080/1355785042000285375. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Publ Health. 1999;89(5):747–751. doi: 10.2105/AJPH.89.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplowitz MD, Hadlock TD, Levine R. A comparison of web and mail survey response rates. Publ Opin Q. 2004;68(1):94–101. doi: 10.1093/poq/nfh006. [DOI] [Google Scholar]
- Knowledge Networks Knowledge Panel Design Summary (2012). Available at http://www.knowledgenetworks.com/knpanel/KNPanel-Design-Summary.html. Accessed 6 February 2012
- Krist AH, Woolf SH, Johnson RE, Rothemich SF, Cunningham TD, Jones RM, Wilson DB, Devers KJ. Patient costs as a barrier to intensive health behavior counseling. Am J Prev Med. 2010;38(3):344–348. doi: 10.1016/j.amepre.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Lee TJ, Cameron LD, Wunsche B, Stevens C. A randomized trial of computer-based communications using imagery and text information to alter representations of heart disease risk and motivate protective behaviour. Br J Health Psychol. 2011;16(Pt 1):72–91. doi: 10.1348/135910710X511709. [DOI] [PubMed] [Google Scholar]
- Lerman C, Croyle RT, Tercyak KP, Hamann H. Genetic testing: psychological aspects and implications. J Consult Clin Psychol. 2002;70(3):784–797. doi: 10.1037/0022-006X.70.3.784. [DOI] [PubMed] [Google Scholar]
- Leslie E, Fotheringham MJ, Owen N, Bauman A. Age-related differences in physical activity levels of young adults. Med Sci Sports Exerc. 2001;33(2):255–258. doi: 10.1097/00005768-200102000-00014. [DOI] [PubMed] [Google Scholar]
- Levine MD, Klem ML, Kalarchian MA, Wing RR, Weissfeld L, Qin L, Marcus MD. Weight gain prevention among women. Obesity. 2007;15(5):1267–1277. doi: 10.1038/oby.2007.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller AC, Lloyd-Jones DM. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125(8):996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K, Ruth KJ, Flack JM, Jones-Webb R, Burke G, Savage PJ, Hulley SB. Blood pressure in young blacks and whites: relevance of obesity and lifestyle factors in determining differences. The CARDIA Study. Coronary artery risk development in young adults. Circulation. 1996;93(1):60–66. doi: 10.1161/01.CIR.93.1.60. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Liu K, Colangelo LA, Yan LL, Klein L, Loria CM, Lewis CE, Savage P. Consistently stable or decreased body mass index in young adulthood and longitudinal changes in metabolic syndrome components: the Coronary Artery Risk Development in Young Adults Study. Circulation. 2007;115(8):1004–1011. doi: 10.1161/CIRCULATIONAHA.106.648642. [DOI] [PubMed] [Google Scholar]
- Marteau TM, French DP, Griffin SJ, Prevost AT, Sutton S, Watkinson C, Attwood S, Hollands GJ (2010) Effects of communicating DNA-based disease risk estimates on risk-reducing behaviours. Cochrane database of systematic reviews (Online) (10):CD007275. doi:10.1002/14651858.CD007275.pub2 [DOI] [PubMed]
- McBride CM, Koehly LM, Sanderson SC, Kaphingst KA. The behavioral response to personalized genetic information: will genetic risk profiles motivate individuals and families to choose more healthful behaviors? Annu Rev Publ Health. 2010;31:89–103. doi: 10.1146/annurev.publhealth.012809.103532. [DOI] [PubMed] [Google Scholar]
- McGuire AL, Diaz CM, Wang T, Hilsenbeck SG. Social networkers' attitudes toward direct-to-consumer personal genome testing. Am J Bioeth. 2009;9(6–7):3–10. doi: 10.1080/15265160902928209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers RS, Roth DL. Perceived benefits of and barriers to exercise and stage of exercise adoption in young adults. Health Psychol. 1997;16(3):277–283. doi: 10.1037/0278-6133.16.3.277. [DOI] [PubMed] [Google Scholar]
- National Human Genome Research Institute (2012) Catalog of Published Genome-Wide Association Studies. Available at http://www.genome.gov/gwastudies/. Accessed 23 February 2012
- Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR, Jr, Ludwig DS. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- Persky S, Kaphingst KA, Condit CM, McBride CM. Assessing hypothetical scenario methodology in genetic susceptibility testing analog studies: a quantitative review. Genet Med. 2007;9(11):727–738. doi: 10.1097/GIM.0b013e318159a344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center for the People and the Press, American Association for the Advancement of Science (2009) Scientific achievements less prominent than a decade ago: public praises science; scientists fault public, media. Pew Research Center for the People and the Press, Washington, DC
- Poobalan AS, Aucott LS, Precious E, Crombie IK, Smith WC. Weight loss interventions in young people (18 to 25 year olds): a systematic review. Obes Rev. 2010;11(8):580–592. doi: 10.1111/j.1467-789X.2009.00673.x. [DOI] [PubMed] [Google Scholar]
- Sanderson SC, O'Neill SC, Bastian LA, Bepler G, McBride CM. What can interest tell us about uptake of genetic testing? Intention and behavior amongst smokers related to patients with lung cancer. Public Health Genomics. 2010;13(2):116–124. doi: 10.1159/000226595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson SC, Wardle J, Jarvis MJ, Humphries SE. Public interest in genetic testing for susceptibility to heart disease and cancer: a population-based survey in the UK. Prev Med. 2004;39(3):458–464. doi: 10.1016/j.ypmed.2004.04.051. [DOI] [PubMed] [Google Scholar]
- Sax LJ, Gilmartin SK, Bryant AN. Assessing response rates and nonresponse bias in web and paper surveys. Res High Educ. 2003;44(4):409–432. doi: 10.1023/A:1024232915870. [DOI] [Google Scholar]
- Tully MA, Cupples ME. UNISTEP (university students exercise and physical activity) study: a pilot study of the effects of accumulating 10,000 steps on health and fitness among university students. J Phys Activ Health. 2011;8(5):663–667. doi: 10.1123/jpah.8.5.663. [DOI] [PubMed] [Google Scholar]
- Turk MW, Sereika SM, Yang K, Ewing LJ, Hravnak M, Burke LE. Psychosocial correlates of weight maintenance among black & white adults. Am J Health Behav. 2012;36(3):395–407. doi: 10.5993/AJHB.36.3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau Current Population Study (CPS) (2012). Available at http://www.census.gov/cps/. Accessed 6 February 2012
- Walsh JR, White AA, Greaney ML. Using focus groups to identify factors affecting healthy weight maintenance in college men. Nutr Res (New York, NY) 2009;29(6):371–378. doi: 10.1016/j.nutres.2009.04.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 65 kb)
(PDF 73 kb)
(PDF 83 kb)