Abstract
Haemoglobinopathies including the thalassemias and sickle cell disease are known to be prevalent inherited disorders in most Arab countries with varying prevalence rates and molecular characterisation. β-thalassemia is encountered in polymorphic frequencies in almost all Arab countries with carrier rates of 1–11 % and a varying number of mutations. The most widespread mutation in Lebanon, Egypt, Syria, Jordan, Tunisia and Algeria is the IVS-I-110 (G>A). In the Eastern Arabian Peninsula, the Asian Indian mutations (IVS-I-5 (G>C), codons 8/9 (+G) and IVS-I (−25 bp del)) are more common. The α-thalassemias are encountered in the majority of Arab countries in frequencies ranging from 1 to 58 % with the highest frequencies reported from Gulf countries. The (−α3.7) mutation is the most frequent followed by the non-deletional α2 polyadenylation signal mutation (AATAAA>AATAAG) and the α2 IVS1 5-bp deletion. The rates of sickle cell trait in Arab countries range from 0.3 to 30 %, with the Benin, the Arab-Indian and the Bantu haplotypes constituting the bulk of the haplotypes, leading to two major phenotypes; a mild one associated with the Arab-Indian and a severe one with the Benin and Bantu haplotypes. Public health approaches targeting prevention of haemoglobinopathies in Arab countries include newborn screening for sickle cell disease, and premarital screening for carriers of β-thalassemia and sickle cell disease. These services are still patchy and inadequate in many Arab countries recommending the upgrade of these services with strengthening of the education and training of health care providers and raising public awareness on the feasibility of prevention and care for haemoglobinopathies.
Keywords: Arab, Haemoglobinopathies, Newborn screening, Premarital screening, Thalassemia, Sickle cell trait, Sickle cell disease
Introduction
Haemoglobinopathies are considered among the most common autosomal recessive disorders affecting humans and are defined by the presence of qualitative and/or quantitative abnormalities affecting the globin chains. Among the qualitative abnormalities, the most common is haemoglobin (Hb)S (β6(A3)Glu→Val) causing sickle cell disease (SCD). The most frequent of quantitative abnormalities with reduced or absent synthesis of α- or β-globin chains lead to α- and β-thalassemias, respectively (Weatherall and Clegg 2001).
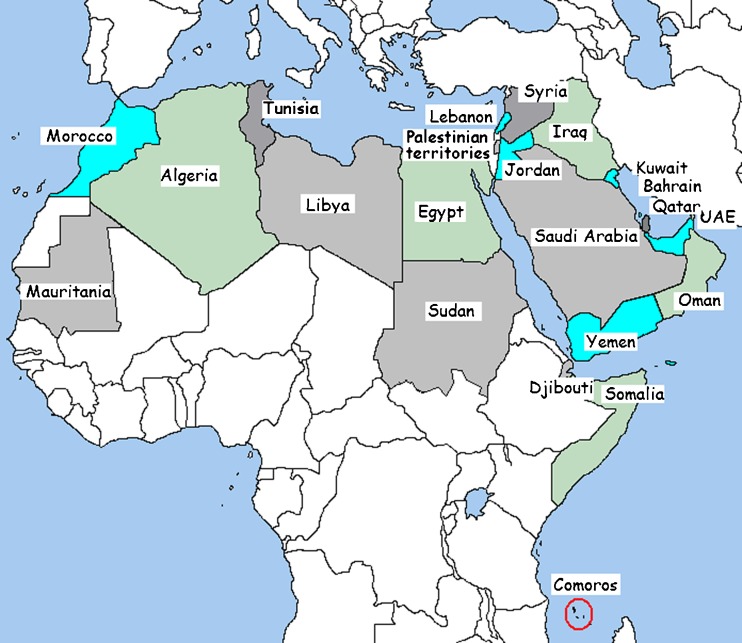
The standard definition of the Arab world comprises the 22 states and territories (UNDP 2012) of the Arab League stretching over more than 13 million km2 from the Atlantic Ocean in the west to the Arabian Sea in the east, and from the Mediterranean Sea in the north to the Horn of Africa and the Indian Ocean in the southeast (Fig. 1). It has a combined population of around 350 million people, one third of which is under 15 years of age (World Health Organization 2010).
Fig. 1.
Map of 22 Arab countries
The economies of Arab countries vary considerably with GNI per capita ranging from a high of over US$40,000 in Kuwait, Qatar, and UAE, to around US$1,000 in Comoros, Mauritania, Sudan, and Yemen (World Bank 2012). Health deficits impede human development in many Arab countries and limit scientific research and hence the paucity of data from some Arab countries in this review.
Incidence and prevalence rates of recessive genetic diseases, such as haemoglobinopathies could be influenced by the demographic and cultural characteristics of the population studied. The populations of many Arab countries are characterised by marriage at a young age, large family sizes and advanced maternal and paternal ages. Consanguineous marriage is customary in most if not all Arab communities and intra-familial unions currently account for 20–50 % of all marriages. First cousin unions are especially popular and constitute almost one quarter of all marriages in many Arab countries, particularly the paternal parallel subtype (Bittles 2012; Hamamy and Bittles 2008). Moreover, Arab populations exhibit significant levels of genetic diversity resulting from the admixture with other populations extending from east and south Asia to Europe and Africa (Teebi and Teebi 2005) and resulting in the present day molecular profile of the haemoglobinopathies which are known to be common genetic diseases among Arabs with reported carrier rates of 1–11 % for β-thalassaemia, 1–58 % for α-thalassaemia and 0.3–30 % for sickle cell trait (Al-Gazali et al. 2006; Alwan and Modell 1997; Haj Khelil et al. 2010; Hamamy and Alwan 1994; Teebi and Farag 1997).
This high frequency could be related to the selective advantage of carriers against falciparum malaria, to the large family size with multiple affected children, to the high consanguinity rates, to the general low availability of public health measures directed at the care and prevention of these disorders and maybe to other as yet unknown factors.
Despite the high rates of haemoglobinopathies, many Arab countries face major challenges in providing comprehensive and up-to-date care and prevention services due to paucity of resources, presence of other competing priorities of communicable and non-communicable disorders, such as cardiovascular diseases, cancer and diabetes, due to the insufficient number of trained health professionals in this field, and to the inadequate data on the real magnitude, health and economic burden of haemoglobinopathies. Currently, community genetic services, such as newborn screening (NBS), premarital carrier screening, prenatal screening, genetic counselling, education and registries are available in some Arab countries, though, in most, these services remain patchy and selective. Further impediments facing prevention and care initiatives include the low genetic literacy among the health sector and the public with lack of awareness about genetic risks and possibilities for prevention of these disorders coupled by certain cultural, legal and religious limitations, such as the cultural fear of families with genetic diseases to be stigmatised within their community and the legal and religious restrictions to selective abortion of an affected foetus.
To highlight the need for defining priorities to implement care and prevention programs on a community level, this review aims at portraying the epidemiological profile of haemoglobinopathies in Arab countries and the currently available services. Knowledge of the molecular defects allows the development and improvement of diagnostic tests and management protocols for these disorders.
Methods
An extensive literature search was performed accessing the Medline database (PubMed 2012) and the World Health organisation Index Medicus for Eastern Mediterranean Region database (WHO 2012). Keywords used in the search included the name of an Arab country combined with each of the following search terms: haemoglobinopathies, β-thalassemia, α-thalassemia, sickle cell, NBS, neonatal screening, premarital screening, genetic services, genetic counselling and consanguinity.
Search for relevant data also included the database of the Catalogue for Transmission Genetics in Arabs (Center for Arab Genomic Studies 2012), which covers genetic disorders in Arab populations and is maintained by the Centre for Arab Genomic Studies (CAGS) in Dubai as well as reviewing relevant textbooks.
Epidemiological profile of β- and α-thalassemias in Arab countries
β-thalassemia is encountered in polymorphic frequencies in almost all Arab countries with carrier rates ranging from 1 to 11 % as detailed in Table 1. Heterozygous carriers of β-thalassaemia are usually symptom free. Their haematology is mostly characterised by a mild anaemia, reduced MCV and MCH values (60–70 fL and 19–23 pg, respectively), a raised level of HbA2 (3.5–7.0 %), and normal or slightly elevated HbF. Homozygosity or compound heterozygosity to β-thalassaemia defects will classically lead to the transfusion-dependent β-thalassemia major, which is a health problem in almost all Arab countries. An intermediate clinical phenotype (between the two above extremes) may be induced by a variety of genetic modulators modifying either heterozygous or homozygous β-thalasemia leading to what is labelled as β-thalassemia intermedia (Weatherall and Clegg 2001).
Table 1.
β-thalassemia carrier rates in Arab countries
| Country | % β-thalassemia carriers (available sample number) (reference) | % α-thalassemia carriers (available sample number) (reference) |
|---|---|---|
| Algeria | 1.5–3 % (Boudrahem-Addour et al. 2009; Labie et al. 1990) | 4.6 % (153) (Mesbah-Amroun et al. 2008) |
| Bahrain | 2.9 % (5,685) (Al-Arrayed et al. 2003) | 24.3 % (10,327) (Mohammed et al. 1992) |
| 2 % (500) (Al-Arrayed et al. 1997) | ||
| 2.8 % (1,070) (Almutawa and Alqamish 2008) | ||
| Comoros | 1 % (Badens et al. 2000) | |
| Egypt | 1.2 (1,000) (Nafei 1992) | 9.25 % (410) (Rizk et al. 2005) |
| 9–10 % (Teebi 2010) | ||
| 9 % (1,000) (El-Beshlawy et al. 2007) | ||
| 5–9 % (El-Beshlawy and Youssry 2009) | ||
| Iraq | 4.6 % in Basra, southern Iraq (1,064) (Hassan et al. 2003) | |
| 4.4 % in Baghdad, central Iraq (502) (Yahya et al. 1996) | ||
| 3.7 % in Dohuk, northern Iraq (1,182) (Al-Allawi and Al-Dousky 2010) | 1 % in Baghdad (502) (Yahya et al. 1996) | |
| 4.14 % in Sulaimania, northeast Iraq (1,472) (Jalal et al. 2008) | ||
| Jordan | 3.04 % (1,020) (Babiker et al. 1999) | 2.26 % in Badia region (1,020) (Babiker et al. 1999) |
| 5.93 % (2,858) (Sunna et al. 1996) | 3.1 % in North Jordan (1,000) (Bashir et al. 1992) | |
| 3.5 % (1,000) (Bashir et al. 1992) | 3.5 % in Jordan valley (456) (Bashir et al. 1991) | |
| 3.3 % (456) (Bashir et al. 1991) | ||
| Kuwait | 3 % (Galanello et al. 2003) | 26/5 % (94) (Diejomaoh et al. 2000) |
| 4.6 % (345) (Simsek et al. 1993) | ||
| Lebanon | 2–3 % (Charafeddine et al. 2008) | Less than 1 % (Teebi and Farag 1997) |
| Libya | 7.8 % (1,350) (Jain 1985) | <1–5 % (Teebi and Farag 1997) |
| Mauritania | 1.12–11.1 %, overall 2.57 % (700) (Deyde et al. 2002) | |
| Morocco | 1.5–3 % (Agouti et al. 2007) | <1–5 % (Teebi and Farag 1997) |
| 2.2 % (Haj Khelil et al. 2010) | ||
| Oman | 0.2–3.9 %, overall 2.2 % (6,342) (Al-Riyami and Ebrahim 2003; Al-Riyami et al. 2001) | |
| 4 % (Rajab et al. 2000) | 38.9 %. (White et al. 1986) | |
| 1.5 % (1,000) (White et al. 1993) | 48.5 % (7,837) (Alkindi et al. 2010) | |
| 2.8 % (7,837) (Alkindi et al. 2010) | 58.3 % (87) (Hassan et al. 2010) | |
| 2.4 % (790) (White et al. 1986) | ||
| Palestinian territories | 4.3 % (1,650) (Sirdah et al. 1998) | |
| 3.5 % in West Bank (Darwish et al. 2005). | ||
| 2.6 % in Gaza (21,825) (Tarazi et al. 2007) | ||
| Qatar | 8.85 (712) (Tremblay et al. 2011) | |
| Saudi Arabia | 3 % (840) (Ganeshaguru et al. 1987) | 28 % in Al-Qatif and 16.3 % in Al-Hasa (12,220) (Nasserullah et al. 1998) |
| 3.22 % (488,315) (Alhamdan et al. 2007) | 43.3 % (840) (Ganeshaguru et al. 1987) | |
| 3.4 % in Al-Hasa (8,918) (Al-Suliman 2006) | 30 % in Qateef, 11 % in Dammam, 7 % in Al-Khobar (29,246) (Al-Awamy 2000) | |
| 0.165 % in Qassim (38,153) (El-Tayeb et al. 2008) | 35.7 % in Qatif (24,012) (Nasserullah et al. 2003) | |
| Syria | 5 % (Galanello et al. 2003) | <1–5 % (Teebi and Farag 1997) |
| Tunisia | 2.2 % (44,299) (Fattoum 2006) | 5.48 % (44,299) (Fattoum 2006) |
| 3.1 % in Kebili (1,400) (Mseddi et al. 1999) | 2 % all Tunis and 4 % Northern Region (304) (Zorai et al. 2002) | |
| 7.38 % (529) (Siala et al. 2008) | ||
| UAE | 1.7 % (4,221) (White et al. 1986) | 49 % (418) (Baysal 2001; El-Kalla and Baysal 1998; Haj Khelil et al. 2010) |
| 8.3 % (Al-Gazali et al. 2005) | ||
| Yemen | 4.43 % (699) (Al-Nood 2009) | 8.6 % (699) (Al-Nood 2009) |
| 2.4 % (721) (White et al. 1986) |
The α-thalassemias are encountered in the majority of Arab countries in frequencies ranging from 1 to 58 % (Table 1), with the highest frequencies reported from Gulf countries (Al-Gazali et al. 2006; Alwan and Modell 1997; Hamamy and Alwan 1994; Teebi and Farag 1997). α-thalassemias could present in one of four clinical phenotypes ranging from a silent carrier state due to a single alpha gene deletion with no or minimal haematological changes and no clinical consequences to a fatal haemoglobin Barts hydrops fetalis due to deletion of all four alpha genes (Galanello et al. 2003) The two other phenotypes are the α-thalassemia minor due to deletion of two genes and haemoglobin H disease due to deletion of three of the four alpha genes leading to a phenotype resembling β-thalassemia intermedia (Weatherall and Clegg 2001).
The spectrum of β-thalassemia mutations in Arab countries
The molecular defects responsible for β-thalassemia are mostly point mutations, and more than 200 of such mutations have been described worldwide. The number of mutations detected in each population varies depending on its origin and interaction with other populations as well as the methods used for characterisation, although generally a handful of these mutations are responsible for the bulk of cases in a particular population. Among Arabs, the heterogeneity of these mutations varies from 44 different mutations in UAE to 10 in Eastern Saudi Arabia (Al-Ali et al. 2005; Baysal 2001). The most widespread and common mutation among Arabs is the IVS-I-110 (G>A). The latter mutation has its highest prevalence in Cyprus and Greece (Baysal et al. 1992; Kattamis et al. 1990) giving the notion that it maybe of Greek origin. Among Arabs, this mutation is most frequent in Lebanon, Egypt, Syria, Jordan and parts of Saudi Arabia (Table 2), and it decreases in frequency as we move to the east where it becomes rare in the Eastern Arabian peninsula to be replaced by the Asian Indian mutations (IVS-I-5 (G>C), codons 8/9 (+G) and IVS-I (−25 bp del)) which are most common in Oman, UAE and Bahrain. IVS-I-110 is however, still frequent in Western Arab countries namely Tunisia and Algeria but becomes less frequent as we move west to Morocco (Table 2). In the latter North African countries, codon 39 (C>T), becomes the most frequent. Codon 39 is most prevalent in the isolated island of Sardinia and in mainland Italy (Rosatelli et al. 1992) and is also a frequent mutation in the Arabian Peninsula (Table 2). Other Mediterranean mutations include IVS-I-1 (G>A) and IVS-I-6 (T>C) which have been reported in polymorphic frequencies in most Arab countries, with highest rates in Palestinian territories, Syria and Egypt. On the other hand, the East Mediterranean mutation IVS-II-I (G>A) is more frequent in the Eastern parts of the Arab world adjacent to Iran where its highest world rates are reported (Najmabadi et al. 2001). Similarly, we see that the Kurdish mutations codons 44 (−C) and 36/37 (−T) seen in northern Iraqi Kurdish population are also frequent in nearby Arab countries like Saudi Arabia, Qatar and Bahrain (Table 2). Some mutations like codon 6 (−A) are believed to be of North African origin with their highest frequencies in Algeria and Morocco (Boudrahem-Addour et al. 2009; Lemsaddek et al. 2004). Other mutations with possible origin in Arab countries include IVS-II-745 (C>G) which has its highest frequency worldwide in Jordan (Sadiq et al. 2001), IVS-I-2 (T>G) almost unique to Tunisia with rates reaching about 20 % (Laradi et al. 2000) and codon 29 (C>T) with rates reaching around 10 % in Lebanon where it may have originated (Makhoul et al. 2005). Codon 37 (G>A) on the other hand, may have Palestinian origin where rates in excess of 11 % are seen (El-Latif et al. 2002), and IVS-II-848 (C>A) may have Egyptian origin with a reported rate of 11 % (Hussein et al. 1993).
Table 2.
Most frequent β-thalassemia mutations in Arab countries
| Country (no of chromosomes) | % of most common β-thalassemia mutations in Arab countries and their origin | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IVS-1–110 (G>A) | IVS-I-1 (G>A) | IVS-II-1 (G>A) | Codon 5 (−CT) | IVS-II-745(C>G) | Codon 37 (G>A) | IVS-I-6 (T>C) | Codon 39 (C>T) | Codon 6 (−A) | IVS-I-5 (G>C) | IVS-I −25 bp | Codon 8/9 (+G) | Codon 44 (−C) | Codon 8 (−AA) | Other frequent mutations | ||
| East MED | East MED | East MED | East MED | East MED | East MED | MED | West MED | North African | Asian-Indian | Asian Indian | Asian-Indian | Kurdish | Turkish | |||
| Algeria (210) | 26.4 | 9.1 | 0.9 | – | – | – | 6.2 | 25.9 | 12.9 | 1.5 | – | – | – | 0.9 | Boudrahem-Addour et al. (2009) | |
| Algeria (239) | 24.6 | 11.7 | – | – | 0.9 | – | 3.3 | 27.6 | 17.1 | 0.4 | – | – | – | – | −29 (A>G; 3.8 %); IVS1–2 (T>C; 3.3 %) | Bennani et al. (1994) |
| Bahrain (66) | 1.5 | 3 | 6.1 | – | – | 24.2 | 16.7 | 36.1 | 1.5 | 4.5 | – | Jassim et al. (1998) | ||||
| Egypt (51) | 31.4 | 17.6 | 5.9 | 2 | 5.9 | – | 17.6 | 2 | – | – | – | – | – | – | −87 (C>G; 7.8 %) | Hussein et al. (2007) |
| Egypt (95 pts) | 25.8 | 19 | 2.1 | – | 6.4 | 1 | 36.3 | 1 | – | – | – | – | – | – | −87 (C>G; 3.2 %); IVS-II-848 (1.6 %) | El-Gawhary et al. (2007)* |
| Egypt (71) | 41 | 13 | 3 | 3 | 3 | 1.4 | 13 | 1.4 | 3 | – | – | – | – | – | IVS-II-848 (11.0 %) | Hussein et al. (1993) |
| Upper Egypt (188) | 57.4 | 9.6 | 5.3 | 20.2 | 2.1 | 1.1 | −87 (C>G; 4.3 %) | Jiffri et al. (2010) | ||||||||
| Iraq, Northern (375) | 7.7 | 12.8 | 24.5 | 7.5 | 0.3 | – | 5.1 | 4.8 | – | 4.8 | – | 10.1 | 4.5 | 10.9 | Al-Allawi et al. (2006), Al-Allawi et al. (2010a), and Jalal et al. (2010) | |
| Jordan (240) | 25 | 10 | 15 | 3.8 | 14.2 | 6.3 | 8.3 | 4.6 | 1.3 | 1.3 | – | – | – | 0.8 | Sadiq et al. (2001) | |
| Kuwait (123) | 6.5 | 5.7 | 25.2 | – | – | – | 5.7 | 15.4 | – | 14.6 | 7.3 | 2.4 | 0.8 | 5.7 | Codon 36/37 (−T; 9.8 %) | Adekile et al. (1994) |
| Lebanon (520) | 34.2 | 15 | 8.7 | 5 | 1.2 | – | 14.4 | <1 | – | – | – | – | 1.2 | 2.5 | Codon 29 (C>T; 9.6 %) | Makhoul et al. (2005) |
| Morocco (187) | 3.21 | 8.56 | – | – | 0.53 | – | 13.9 | 26.2 | 13.37 | 0.5 | 0.5 | – | – | 9.63 | −29 (A>G; 4.28 %); IVS1–2 (T>C;2.14 %) | Lemsaddek et al. (2004) |
| Morocco (158) | 5.7 | 5.06 | 2.5 | 7.6 | 3.16 | 3.16 | 26.58 | 5.7 | 13.91 | −29 (A>G; 6.33 %); IVS1–2 (T>C;5.06 %) | Agouti et al. (2008) | |||||
| Oman (174) | 0.5 | 1.1 | 3.6 | 4.5 | 0.5 | 4.5 | 73 | 4.5 | 3.4 | 1.1 | – | Codon 30 (G>C) (4.5 %) | Hassan et al. (2010) | |||
| Oman (99 pt) | 0.5 | 1.0 | 3.6 | 0.5 | – | 0.5 | – | 1.0 | – | 61.6 | 5.6 | – | – | – | 619 bp deletion (4 %); Hb Dhofar (6.6 %) | Daar et al. (1998) |
| Palestinian WB (136) | 9.5 | 4.4 | 4.4 | 8.1 | – | 11.3 | 48.5 | 2.2 | – | – | – | 2.9 | – | El-Latif et al. (2002) | ||
| Palestinian WB & Gaza (88 carrier couples) | 22.2 | 9.7 | 6.2 | 8 | 12 | 13.6 | 9 | 8.5 | 2.8 | |||||||
| Palestinian WB (148) | 17.6 | 9 | 2.9 | 2.5 | 0.3 | 10.4 | 28.7 | 4.6 | 0.3 | 1.1 | – | 1.4 | – | – | Codon 106/107 (+G; 6.8 %); IVS-II-848 (2.5 %) | Darwish et al. (2005) |
| Palestinian Gaza | 37.5 | 20 | 1.0 | 10 | – | 1.0 | 7.5 | 11.5 | 5 | – | – | – | – | – | Ayesh et al. (2005) and Filon et al. (1995) | |
| Qatar (65) | 6.2 | 1.5 | 9.2 | – | – | – | – | 1.5 | – | 35.4 | 6.2 | 26.1 | 3.1 | 3.1 | Codon 15 (G>A; 3.1 %) | Al-Obaidli et al. (2007) |
| Saudi Arabia, Eastern (88) | – | 5.8 | 27.5 | 1.5 | 1.5 | – | 4.4 | 20.3 | – | 23.2 | 4.4 | – | 1.5 | Al-Ali et al. (2005) | ||
| Saudi Arabia, Eastern (196 pts) | 2.55 | 3.83 | 22.2 | 3.06 | 0.51 | 7.14 | 25 | 13.3 | 13 | 1.53 | 0.51 | 2.08 | Al-Sultan et al. (2011) | |||
| Saudi Arabia, Eastern (53) | 15.1 | 32.1 | 1.9 | 22.6 | 3.8 | 7.5 | 15.1 | El-Harth et al. (1999) | ||||||||
| Saudi Arabia, Western (297) | 13.5 | 4 | 17.5 | 2.4 | 1 | 7.7 | 19.2 | 2.7 | 7.4 | 2 | 2 | Codon 26 (G>A); HbE (9.1 %) | Abuzenadah et al. (2011) | |||
| Saudi Arabia (186) | 26.9 | 12.9 | 12.9 | 12.9 | 12.9 | 1.07 | El-Hazmi et al. (1995) | |||||||||
| Syria (141) | 24.1 | 17.0 | 4.2 | 8.5 | 1.4 | 1.4 | 4.2 | 6.4 | – | – | 0.7 | 1.4 | – | 0.7 | −30 (T>A; 7.1 %); Codon 15 (G>A; 3.5 %) | Kyriacou et al. (2000) |
| Tunisia (118) | 10.81 | 4.32 | 1.62 | – | 2.16 | 1.08 | 0.54 | 43.78 | 7.02 | 3.24 | – | – | 1.62 | 0.54 | IVS-II-849 (A>C; 4.32 %) | Chouk et al. (2004) |
| Tunisia (475) | 21 | 4.5 | 0.6 | 0.4 | 2.6 | – | 0.6 | 49 | 2.6 | 1.0 | – | – | 3.8 | 0.2 | IVS-I-2 (T>G; 3.0 %) | Fattoum et al. (2004) |
| Tunisia (121) | 15.7 | 3.31 | – | – | – | – | 2.48 | 48.76 | 1.65 | – | – | – | 1.65 | – | IVS-I-2 (T>G; 19.83 %) | Laradi et al. (2000) |
| UAE (647) | 1.2 | – | 3.6 | 2.6 | – | 0.2 | 1.6 | 2.8 | – | 56.7 | 11.0 | 3.9 | 0.9 | 2.8 | HbS alleles excluded | Baysal (2011) |
| UAE (626) | 0.6 | 0.6 | 2.9 | 1.6 | – | 0.2 | 1.6 | 2.7 | – | 47.6 | 6.2 | 4.3 | 0.6 | 1.9 | The series included 21.9 % HbS alleles | Baysal (2005) |
A limited number of studies utilised RFLP and sequence haplotypes in attempts to determine the origin and history of various β-thalassemia mutations in some Arab countries, particularly in Lebanon and North Africa. Table 3 outlines the RFLP haplotypes associated with common β-thalassemia mutations reported in some Arab countries. It shows that in the majority of cases, each mutation is associated with mainly one particular haplotype in various countries and this is consistent with a common origin. The following is a brief overview of the available data:
IVS-I-110 was found to be associated with a single RFLP haplotype (haplotype I) in Lebanon, in the Palestinian territories and in Tunisia, similar to the findings from Cyprus (El-Latif et al. 2002; Filon et al. 1994; Flint et al. 1993; Makhoul et al. 2005). Haplotype I is also the predominant of two haplotypes seen in Egypt, Morrocco and Algeria (Flint et al. 1993; Haj Khelil et al. 2010). IVS-I-110 is associated with four RFLP haplotypes (I, II, IV and IX) in Turkey, suggesting that it may have originated in Turkey (Anatolia) probably in the Neolithic period, and then spread to other parts in the Eastern Mediterranean area and North Africa by the Greeks, Phoenicians or later by Othmans (Haj Khelil et al. 2010; Tadmouri et al. 2001; Tadmouri and Gulen 2003). Sequence haplotypes have supported the latter suggestion since it was found that IVS-I-110 was associated with six haplotypes in Turkey, two in Lebanon and two in Algeria and Tunisia (Haj Khelil et al. 2010; Perrin et al. 1998; Tadmouri et al. 2001; Zahed et al. 2002).
Codon 39 is a Western Mediterranean mutation of possibly a Roman origin, having its highest worldwide prevalence in Sardinia where it is associated with nine different haplotypes (Pirastu et al. 1987). Its distribution in the Arab world is more or less consistent with the reign of the Roman Empire, which extended up to the fifth century bc. It is associated with a single RFLP haplotype in Palestinian territories and Lebanon (haplotype II, which is also the most common haplotype in Sardinia) and with three, four and six haplotypes in Morrocco, Algeria and Tunisia, respectively (Agouti et al. 2008; El-Latif et al. 2002; Haj Khelil et al. 2010; Makhoul et al. 2005). The latter has led Haj Khelil and her co-workers to suggest a possible local origin of this mutation in North Africa (Haj Khelil et al. 2010).
IVS-1-6 was found to be associated with multiple haplotypes in Lebanon (VI, VII and I) compared with its relative homogeneity in European populations where it is also frequently encountered, suggesting a possible ancient Eastern Mediterranean origin (Flint et al. 1993; Makhoul et al. 2005).
IVS-1-1 has its highest frequency in eastern Europe (Henderson et al. 2009) and it is seen in association with haplotype V in Lebanon and Palestinian Arabs but with multiple haplotypes including V in North Africa probably reflecting independent origins in these two parts of the Arab world (El-Latif et al. 2002; Haj Khelil et al. 2010; Makhoul et al. 2005).
IVS-II-1 has been linked to different haplotypes in various parts of the world. It is associated with haplotypes III in Lebanon and I and III in Palestinian Arabs (Makhoul et al. 2005; El-Latif et al. 2002; Filon et al. 1994). It was linked to multiple haplotypes (mainly III, but also I, II, V, X and atypical) in Iran where it has one of its highest frequencies worldwide (Najmabadi et al. 2001; Rahimi et al. 2003). The latter together with almost restricted occurrence in Eastern Arab countries neighbouring Iran, suggests possible origin from the latter country, mostly during the reign of the Persian Empire.
IVS1.5 is an ancient Asian Indian mutation having its highest frequencies and highest haplotype diversity in the Indian subcontinent (Gupta et al. 2003). The commonest haplotype among Asian Indians is haplotype VII, which is the only haplotype with which it is associated among the Lebanese, confirming Asian Indian origin in the latter Arab population (Flint et al. 1993; Makhoul et al. 2005). To our knowledge, no studies of haplotypes associated with this mutation have been reported from eastern Arabian Peninsula where it is most frequent, though its distribution in the latter region is consistent with the strong trade links between this region and Indian subcontinent throughout history.
Table 3.
RFLP haplotypes associated with common β-thalassemia in Arab countries
| Mutation | Country | |||||
|---|---|---|---|---|---|---|
| Lebanon | Palestinian territories | Egypt | Morocco | Algeria | Tunisia | |
| IVS-I-110 (G>A) | I | I | I-II | I-II | I-II | I |
| Codon 39 (C>T) | II | II | II | II-I-Nd | II-I-B | II-I-5a-Nd-A-Nc |
| IVS-I-1 (G>A) | V | V | V | V-IX | V-I-III-IX-A | V |
| IVS-I-6 (T>C) | VI-VII-I | VI-VII | VI | VI-VII | – | VI |
| IVS-II-1 (G>A) | III | I-III | III | III | – | – |
| IVS-I-5 (G>C) | VII | I | – | – | – | – |
| Codon 8/9 (+G) | I | I | – | – | – | – |
| Codon 6 (−A) | – | – | V | IX-III | IX-I-A | IX-V-A |
| Codon 8 (−AA) | IV-VII | IV | – | IV-VI-VII | – | IV |
| IVS-II-745 (C>G) | VII | – | VII | VII | VII | VII |
| Codon 5 (−CT) | V | III | – | III | – | – |
| References | Makhoul et al. (2005) | El-Latif et al. (2002) and Filon et al. (1994) | Flint et al. (1993) | Agouti et al. (2008) | Bennani et al. (1994) and Rouabhi et al. (1988) | Flint et al. (1993 and Haj Khelil et al. (2010) |
Further studies are still required to determine the haplotypes associated with various mutations in other Arab countries to have a better understanding of the origin and spread of these mutations in the Arab world.
Deniz is an electronic database for thalassemia mutations in the Arab world which catalogues the frequencies of β-thalassemia mutations in 14 Arab countries derived from the analysis of 3,138 chromosomes by 36 laboratories. Of the 57 β-globin gene mutations reported in Arabs, IVS-I-110 (G>A), IVS-I-5 (G>C), IVS-I-6 (T->C), IVS-II-1 (G>A) and IVS-I-1 (G>A) are the most encountered and they account for approximately two thirds of the Arab chromosomes registered in Deniz (Tadmouri and Gulen 2003).
The spectrum of α-thalassemia mutations in Arab countries
In contrast to β-thalassemias, α-thalassemias are mostly due to deletions involving one or both α-genes leading to α+ or α0 defects, respectively. However, several non-deletional defects have been noted in considerable frequencies in some parts of the world including some Arab countries (Harteveld and Higgs 2010). Among Arabs the most frequent mutation detected in all reports up to date is the (−α3.7) also called the rightwards deletion which is due to the deletion of a 3.7 kb fragment leaving practically one functional α gene and therefore an α+ defect (Table 4). Other frequently encountered mutations among Arabs include the non-deletional α2 polyadenylation signal mutation (AATAAA>AATAAG) and the α2 IVS1 5-bp deletion. The former mutation which was first described among Saudi Arabs and thus labelled the Saudi polyadenylation signal mutation leads to a more severe α+ defect than the single gene deletion and is denoted as (αpolyA1α) or (αPA−1α). The α2 IVS1 5 bp deletion (c.95+2_95+6delTGAGG) removes five nucleotides from donor IVS-I leading to failure of stable mRNA formation (Orkin et al. 1981) and is labelled as (α−5ntα) or (αHph1α) and is also frequent in other Mediterranean countries (Abu-Ghoush 2008; Baysal et al. 1992; Curuk 2007; Di et al. 1986; El-Kalla and Baysal 1998; Hadavi et al. 2007; Kanavakis et al. 2000; Mesbah-Amroun et al. 2008; Oron-Karni et al. 2000; Siala et al. 2008; Yavarian et al. 2005). Other α+ mutations including (−α4.2) (leftwards deletion) and Hb Constant Spring (a termination codon mutation) were reported, though infrequently, in several studies from Arab countries (Table 4). The α0 defects on the other hand, are either absent or seen only sporadically in most Arab countries and therefore Hb Bart’s hydrops fetalis (homozygosity to an α0 defect (− −/− −)) is almost absent (Al-Allawi et al. 2010b), while HbH (usually due to compound heterozygosity to and α0 and α+) is not common. Thus in many Arab countries, particularly in the Arabian Peninsula, the majority of cases of HbH disease are actually due to homozygosity to the common polyadenylation signal mutation (αpolyA1α/αpolyA1α) (Adekile et al. 1994; El-Kalla and Baysal 1998; Haider and Adekile 2005; Hellani et al. 2009)
Table 4.
Spectrum of α-thalassemia gene mutations in Arab countries
| Country | Most frequent α-thalassemia gene mutations (reference) |
|---|---|
| Algeria | Among 153 blood donors screened for 10 α-thalassemic determinants: 2.9 % had the (−α3.7), 0.6 % the α2 initiation codon T>C (αNco1α), and the (α−5ntα), (−(α)20.5) and (− −MED-1) at 0.3 % each (Mesbah-Amroun et al. 2008) |
| Bahrain | Among 97 α-thalassemia chromosomes, the most common was the (α poly A1α) (53 %), followed by (− α3.7) (32 %), (α−5ntα) (12 %), (− α4.2) (2 %) and (α poly A2α) (1 %). The cause of HbH disease is consistently (αpoly A1α/αpoly A1α), other genotypes are rare (Jassim et al. 2001) |
| Among 410 umbilical cord blood samples, 9.5 % were identified as α thalassaemia. The percentage of the different genotypes detected was: 4.5 % for (−α/αα), 3 % for (−α/–α), 1.75 % for (− −/αα) and 0.25 % HbH disease (− −/− α). No cases of Hb Bart’s hydrops fetalis (− −/− −) were detected (Rizk et al. 2005) | |
| Iraq | Among 51 individuals with unexplained hypochromia and/or microcytosis from the Dohuk region in northern Iraq, 51 % had the (−α3.7/αα), 23.5 % the (− −MED-I/α α), 9.8 % the (−α 3.7/–α 3.7) and 3.9 % the (−α4.2/αα), other genotypes were sporadic . On the other hand, all 9 HbH cases studied had the (−α3.7/− −MED-I) genotype (Al-Allawi et al. 2009) |
| Jordan | Among 430 α-thalassemic patients investigated: 43 % had the (−α3,7), followed by the (αpolyA1α) in 31 %, the (α−5ntα) and the (− −MED-I) in 18 % and 7 % respectively. Among 33 patients with HbH disease 60.6 %, 15.1 %, 12.2 % and 12.2 % had the (α poly A1α/αpoly A1α), (αpoly A1α/− −MED-I), (−α3.7/− −MED-I) and (α−5ntα/− −MED-I), respectively (Abu-Ghoush 2008) |
| Kuwait | Among 17 HbH patients 70.8 % had the (αpoly A1α/αpoly A1α), while 25 % had the (αpoly A1α/–α3.7)and 4.2 % were undetermined (Haider and Adekile 2005) |
| Of the 30 chromosomes from 15 patients with HbH disease, 86.7 % carried the (αpolyA1α), 10 % had (−α3.7), and 3.3 % had the (α−5ntα) (Adekile et al. 1994) | |
| Saudi Arabia | Among 41 patients suffering from microcytic, hypochromic anemia from the eastern province, the most common alpha determinant was the (−α3.7) in 64 % followed by the (αpoly A1α) in 41 % (Hellani et al. 2009) |
| A study to determine the deletional forms of α-thalassemia revealed that the (−α/αα) varied between 9.6 and 38.8 %, while the (−α/–α) ranged from 5 to 12.7 % in various regions of the kingdom (El-Hazmi and Warsy 1999) | |
| In Eastern region, it was found that 45 % carried the (−α3.7), while another 15 % had a non-deletional defect (ααT), later found to be (αpolyA1α) (Al-Awamy 2000; Higgs et al. 1983) | |
| Tunisia | No α0-thal alleles were found among 304 blood samples. Among cord blood samples from northeastern region, the (−α3.7) was the most common defect (4.5 % allele frequency) followed by (αpoly A1α) in 1.8 %, while (α−5ntα) and the (−α4.2) in 0.9 % each (Zorai et al. 2002) |
| Testing 20 index cases with Hb Barts at birth revealed that 35 % had the (−α3.7/αα), 25 % had the (α−5ntα/αα), 5 % (−α3.7/−α3.7), while αcd23GAG>stop, αcd119CCT>TCT and α+6C>G were carried by 5 % each. In 7 families with HbH: 5 had the genotype (αpoly A1α/αpoly A1α), two had the (−α3.7/− −MED-I) (Siala et al. 2008) | |
| UAE | Among 418 consecutive cord blood samples: 33.5 % were (−α3.7/αα), 11 % were (−α3.7/−α3.7), 1.4 % (α−5ntα/αα), 1.2 % (−α4.2/αα), 0.7 % each for (αpolyA1α/αα) and (αCSα/αα). Other sporadic mutations included (αpolyA2α/αα). In 22 patients with HbH disease or HbH-like syndrome, 9 were (αpolyA1α/−α3.7), 6 were homozygous for the (αpolyA1α) mutation, 2 were homozygous for Hb CS, and 5 were compound heterozygous for either (αpolyA1α), (αCSα), (α−5ntα), or (− −MED-I), with the (−α3.7) (El-Kalla and Baysal 1998; Haj Khelil et al. 2010) |
The SCD in Arab countries
Over the generations, the HbS gene has reached high frequencies in regions with past or present history of malaria endemicity due to the selective advantage of carriers to falciparum malaria. However, population migration has played a major role in distributing HbS gene even to malaria non-endemic regions. SCD is most common among people from Africa, India, the Caribbean, the Middle East and the Mediterranean. The rates of sickle cell trait in Arab countries range from 0.3 to 30 % (Table 5). SCD is a symptomatic condition resulting from the tendency of red cells to sickle upon deoxygenation due to the presence of HbS. It could be due to homozygosity of HbS (sickle cell anemia-SS) or compound heterozygosity to β-thalassemia and sickle gene (Lal and Vichinsky 2011). Worldwide, the βS gene has been found to be associated with five different major β-globin cluster haplotypes, which favours its multicentric origin (Kulozik et al. 1986; Serjeant 1989). These haplotypes are named in reference to their supposed places of origin and include: the Benin (Central West Africa), Senegal (West Africa), the Bantu (Central, East and Southern Africa), the Cameroon and the Arab-Indian haplotypes (Arabian Peninsula and India). These haplotypes are important determinants of disease severity and HbF levels in patients with SCA, with the Arab-Indian and Sengal haplotypes being associated with higher HbF levels and milder clinical presentation in homozygous patients. On the other hand, the other three haplotypes are associated with low HbF and more severe clinical phenotypes with the Bantu haplotype being the most severe (Ogedegbe 2007). Among Arabs three of the five major haplotypes constitute the bulk of the haplotypes associated with the βS mutation. These haplotypes are the Benin, the Arab-Indian and the Bantu haplotypes, while the other two haplotypes are sporadic (Table 6). Thus and as anticipated, it would be expected to find two major phenotypes among Arabs, a mild one associated with the Arab-Indian and a severe one with the Benin and Bantu haplotypes. Table 6 shows the distribution of the three major haplotypes in various Arab countries and clearly shows that in the Eastern Arabian Peninsula, the Arab Indian haplotype is most frequent, while among other Arab countries in Eastern Mediterranean and North Africa, the Benin haplotype predominates. This distribution is probably best explained by the supposed origin of the sickle cell mutation, with the Arab-Indian mutation originating in the Indus valley on the Indian subcontinent and subsequently spreading to Iran and Eastern Arabian Peninsula through trade routes and historical interactions (Daar et al. 2000; Rahgozar et al. 2000). The Benin haplotype on the other hand, has originated in Central West Africa and then spread vertically via population movement by trans-Saharan migration to North Africa and thence across the Mediterranean Sea to Southern Europe and the Eastern Mediterranean region (Serjeant 1989). Another possible explanation is a direct spread from Africa through the red sea to Western part of Arabian Peninsula and from there to other Arab countries, via slave trade or immigration. However, the possibility of an independent origin of any of the above haplotypes in Arabs cannot be ruled out (Serjeant 1989).
Table 5.
rates of sickle cell trait and sickle cell disease in Arab countries
| Country | Sickle cell trait rate (available sample number) (reference) | Sickle cell disease rate (available sample number) (reference) |
|---|---|---|
| Algeria | 0.8–3.5 % (Haj Khelil et al. 2010) | – |
| Bahrain | 13–14.2 % (Al-Arrayad 2006) | 1.1–1.37 % (Al-Arrayad 2006) |
| 13.8 % (5,685) (Al-Arrayed et al. 2003) | 1.2 % (5,685) (Al-Arrayed et al. 2003) | |
| 11.2 % (10,327) (Mohammed et al. 1992) | 2.1 % (10,327) (Mohammed et al. 1992) | |
| 13 % (500) (Al-Arrayed et al. 1997) | 1.6 % (500) (Al-Arrayed et al. 1997) | |
| 16.4 % (1,070) (Almutawa and Alqamish 2008) | 1.3 % (1,070) (Almutawa and Alqamish 2008) | |
| 16.3 % (2,000) (Al-Arrayed 2005) | 0.9 % (2,000) (Al-Arrayed 2005) | |
| 0.8 % (17,000) (Al-Arrayed 2007) | ||
| 0.67 % (Rajab et al. 2006) | ||
| Egypt | 0.3 % (1,000) (Nafei 1992) | |
| Iraq | 6.5 % (1,064 in Basra) (Hassan et al. 2003) | |
| 1.2 % (1,182 in Duhok) (Al-Allawi and Al-Dousky 2010) | ||
| 0.27 % (1,472 in Sulaimani Northeast Iraq) (Jalal et al. 2008) | ||
| Jordan | 3.17–4.45 % (2,858 in Northern Jordan) (Sunna et al. 1996) | |
| 1 % (1,000 in Northern Jordan) (Bashir et al. 1992) | ||
| 0.44 (456 in Jordan valley) (Bashir et al. 1991) | ||
| 4–6 % (181) (Talafih et al. 1996) | ||
| Libya | 4.51 % (Jain 1985) | 0.37 % (Jain 1985) |
| 3.3 % (545 in Benghazi) (Jain 1979) | ||
| Morocco | 1.2 % (Haj Khelil et al. 2010) | |
| Oman | 5.8 % range 0.2/10 % (6,342) (Al-Riyami and Ebrahim 2003; Al-Riyami et al. 2001) | 0.2 % (6,342) (Al-Riyami and Ebrahim 2003) |
| 10 % (Rajab et al. 2000) | 0.117 % (1,757 registered cases/1.5 million population) (Rajab et al. 2000) | |
| 6.1 % (1,000) (White et al. 1993) | ||
| 4.8 % (7,837) (Alkindi et al. 2010) | 0.3 % (7,837) (Alkindi et al. 2010) | |
| Saudi Arabia | 4.2 % (488,315) (Alhamdan et al. 2007) | 0.26 % (488,315) (Alhamdan et al. 2007) |
| 21.14 % (24,012 in Qatif) (Nasserullah et al. 2003) | 2.57 % (24,012 in Qatif) (Nasserullah et al. 2003) | |
| 1.3 % in Northern, 21.3 % in Eastern, 7.5 % in North Western, 12 % in South Western and 0.8 % in Central provinces (30,055) (El-Hazmi and Warsy 1999) | 3.8 % in Eastern, 0.88 % in North Western, 1.7 % in South Western provinces (30,055) (El-Hazmi and Warsy 1999) | |
| 4.4 % in Al-Khobar, 6.7 % in Dammam and 17.9 % in Qatif (5,630) (Al-Awamy et al. 1984) | 0.24 % (5,682) 1.45 % in Eastern 0.24 % in Southwestern, 0.06 % in Central (Al-Qurashi et al. 2008). | |
| 25.9 % (960)) (El-Hazmi and Warsy 1994) | 2.92 % (960 in Al-Qatif) (El-Hazmi and Warsy 1994) | |
| 2.35 % in Al-Qatif, 1.08 % in Al-Hasa (12,220) (Nasserullah et al. 1998) | ||
| 0.252 % (38,153 in Al-Qassim) (El-Tayeb et al. 2008) | ||
| 5.7 % (Ganeshaguru et al. 1987) | ||
| Tunisia | 1.89 % (44,299) (Fattoum 2006) | |
| 4.9 % in south Tunis, kebili (1,400) (Mseddi et al. 1999) | ||
| UAE | 1.5 % (9,165 UAE citizens) (Al-Hosani et al. 2005) | 0.07 % (9,165 UAE citizens) (Al-Hosani et al. 2005) |
| Yemen | 2.2 % (Al-Nood et al. 2004) | 0.9 % (White et al. 1986) |
Table 6.
Most frequent sickle cell gene associated haplotypes in Arab countries
| Countries | Number of chromosomes | Benin (%) | Arab-Indian (%) | Bantu (%) | Other haplotypes (%) | Reference |
|---|---|---|---|---|---|---|
| Algeria | 20 | 100.0 | – | – | – | Pagnier et al. (1984) |
| Bahrain | 37 | 2.7 | 89.2 | 5.4 | 2.7 | Al-Arrayed (1995) |
| Egypt | 28 | 100.0 | – | – | – | El-Hazemi et al. (1999) |
| Iraq (Northern) | 128 | 69.5 | 12.5 | 7.8 | 10.2 | Al-Allawi et al. (2012) |
| Jordan | 20 | 80.0 | 20.0 | – | – | El-Hazemi et al. (1999) |
| Kuwait | 125 | 11.2 | 80.8 | 5.7 | 2.4 | Adekile (2001) |
| Lebanon | 100 | 73.0 | 10.0 | 15 | 2.0 | Inati et al. (2003) |
| Oman | 117 | 52.1 | 26.7 | 21.4 | – | Daar et al. (2000) |
| Palestinian West Bank | 118 | 88.1 | – | 5.1 | 6.8 | Samarah et al. (2009) |
| Saudi Arabia (southwestern) | 124 | 98.5 | 1.5 | – | – | El-Hazemi et al. (1999) |
| Saudi Arabia (eastern) | 50 | – | 94.0 | 4.0 | 2.0 | Kulozik et al. (1986) |
| Syria | 18 | 66.7 | 33.3 | – | – | El-Hazemi et al. (1999) |
| Tunisia | 66 | 94.0 | – | – | 6.0 | Abbes et al. (1991) |
| UAE | 94 | 22.0 | 52.0 | 26.0 | El-Kalla and Baysal (1998) |
Community genetic services addressing haemoglobinopathies in Arab countries
The published data on care and prevention services for haemoglobinopathies in Arab countries are quite scanty. An idea about the facilities provided can be obtained from research papers published in local or international journals. Community genetic services mainly include population screening programs, such as NBS for sickle cell anaemia, and premarital screening for carriers of β-thalassemia. Islamic teachings in medical genetics and practice emphasise the importance of counselling, education and screening for the prevention of genetic diseases. With the exception of prenatal diagnosis (PND) and the selective abortion of an affected foetus, there is little that is controversial in the application of genetics in different Arab countries (Al-Aqeel 2007; El-Hazmi 2007; Hamamy and Bittles 2008).
NBS for common haemoglobinopathies in Arab countries
NBS for haemoglobinopathies allows the identification of affected infants soon after birth promoting tertiary prevention through prophylactic treatment and comprehensive care prior to the development of clinical complications. Neonatal screening for sickle cell anaemia with the early institution of prophylactic penicillin use and pneumococcal vaccination helps in reducing the rates of mortality from infections. Identification of sickle cell carriers points to couples at risk of having affected children who could be offered prospective genetic counselling and information on future reproductive options and feasible prevention measures including PND.
NBS programs for sickle cell anaemia and trait have been implemented in a number of Arab countries providing important data on birth rates and allowing both the prophylactic management of diseased infants and counselling for carrier parents.
The national NBS program for haemoglobinopathies in Bahrain funded by the national budget was implemented in May 2007 to screen for SCD, α-thalassemia and G6PD deficiency. A total number of 38,940 newborns were screened between the years 2007 and 2010 giving an average birth rate for SCD of 0.58 % with a gradual decline from 0.7 to 0.41 % over this period (Al-Arrayed and Al-Hajeri 2012). The decline of SCA birth rate from 2.1 % in 1985 to 0.9 % in 2002 (Al-Arrayed 2005) and then to 0.7 % in 2007 could be related to the increased public awareness following the extensive campaigns implemented over the past 20 years (Al-Arrayed and Al-Hajeri 2012) The sickle cell trait prevalence of 16.3 % in 2002 compares with previous estimates of 11 % in 1986, 13 % among students screened in 1998 and 14 % in 2001 (Al-Arrayed 2005).
A study on 7,837 consecutive cord blood samples from April 2005 to March 2007 in Oman showed that 429 neonates were carriers for HbS (5.48 %) (Alkindi et al. 2011). The samples also showed the presence of Hb Barts indicating the presence of α-thalassemia genes in 48.5 % of the neonates though no case of HbH was detected (Alkindi et al. 2010).
In a prospective study, cord blood samples from 504 neonates from the Qatif area of the Eastern Province of Saudi Arabia were analysed by complete blood counts and cellulose acetate Hb electrophoresis with confirmation of HbS by citrate agar Hb electrophoresis. The prevalence of α-thalassaemia was reported as 40 % and the sickle cell gene was seen in 23.4 % of cord blood neonatal samples (Quadri et al. 2000).
In Tunisia, a pilot study conducted over a one year period in two Tunisian maternity hospitals with screening of 9,148 newborns for HbS showed that 76 cases were sickle cell carriers (1.9 %) and one case had SCD. This pilot experiment has demonstrated the feasibility of SCD neonatal detection using a lower cost method where blood samples were collected using a Whatman A4 paper sheet and the tests were done using isoelectrofocusing. This method also allowed detection of other main structural Hb variants (Hajer et al. 2012).
In the UAE, sickle cell anaemia screening at birth was implemented in 2001 in Abu Dhabi Emirate only (Al-Gazali et al. 2005).
Carrier screening programs for common haemoglobinopathies
Community-based haemoglobinopathies care and prevention strategies which include mass education campaigns, carrier screening and genetic counselling have proved highly acceptable in a wide range of cultural settings and have led to a marked fall in the number of children born with these disorders (Samavat and Modell 2004). Premarital screening program (PMS) is a comprehensive program that tests those who are planning to get married for various inherited or acquired disorders. A major obstacle to implement a successful screening program in Arab countries is the general low awareness regarding genetic diseases and the feasibility of their prevention. The various practices of premarital screening are burdened with social and ethical dilemmas including stigmatisation, privacy and autonomy which implies that carrier screening programmes and the associated services should be implemented in a manner that respects the population’s religious and cultural views (WHO 2006).
The objective of premarital screening to detect haemoglobinopathy carriers of is to offer couples who are at a high risk of having an affected baby the information on all aspects of the condition including care and prevention options that enable the couple to make an informed reproductive decision and choice. Community programs for premarital screening to detect haemoglobinopathies carriers have been initiated in a number of Arab countries including Bahrain, Iraq, Jordan, Oman, Palestinian territories, Saudi Arabia, Tunisia and the UAE.
Although carrier screening programmes should be strictly voluntary, many Arab countries are currently implementing mandatory PMS to detect β-thalassemia carriers. However, these programs maintain the autonomy of decision for the couple after delivery of results, including the decision to proceed with the marriage plan, reproduction decisions and decisions to go through PND with or without selective termination of an affected foetus.
A service for premarital counselling was initiated in Bahrain in 1992 and was voluntary in the first few years where 20 % of the married couples attended premarital counselling. In 2004, a law was issued by the king of Bahrain where PMC became mandatory, while at the same time, the decisions on marriage and reproduction choices remain strictly the decisions of the couples themselves after receiving confidential counselling sessions. A study assessing knowledge on SCD among 2,000 persons selected from the general public showed that 93 % had heard of SCD, with 84 % recognising it as a hereditary condition while 89 % knew that it can be diagnosed by a blood test (Al-Arrayed and Al-Hajeri 2010). As part of the National Student Screening Project to determine the prevalence of genetic blood disorders and raise awareness among young Bahrainis, 11th-grade students from 38 schools (5,685 students) were screened and provided with organised lectures and leaflets about these disorders (Al-Arrayed et al. 2003).
β-thalassemia is the most frequent haemoglobinopathy in Egypt with a carrier rate of 5.3–9 % and an estimated 1,000 infants born each year with β-thalassaemia major among the national 1.5 million live births. The estimated average financial cost for β-thalassaemia management in Egypt is $10 million/year and is on the increase. The registered cases of β-thalassaemia in the main centers in Egypt are 9,912 patients with the highest numbers in the haematology unit of the New Cairo University Children Hospital (El-Beshlawy and Youssry 2009). Carrier detection by premarital and/or early antenatal screening for thalassemia is not mandatory and not widely applied in Egypt with few limited attempts in the domain of prevention of thalassemia implemented in some centers in Egypt. Screening for β-thalassemia carriers among Egyptian school-age children from different geographical areas was implemented from 1993 to 2005. There are, however, a limited number of available premarital screening centres that are generally difficult to access by the public and their services are considered too costly by most of those who need them (El-Beshlawy and Youssry 2009).
β-thalassemia is a common inherited haematological disorder in Iraq, with an average prevalence of carriers of about 4 % and an estimated 15,000 registered thalassemia major/intermedia patients throughout the country. The huge burden on the already precarious resources by this huge number of patients has led the health authorities to search for a prevention strategy. In the Kurdistan region in the north of the country where around 20 % of the population of Iraq reside, pilot studies were initiated in 2006 to determine the service indicators for β-thalassaemia prevention and the molecular basis of this condition in the region (Al-Allawi et al. 2006; Al-Allawi and Al-Dousky 2010; Jalal et al. 2010, 2008). These studies showed that a PMS was feasible and after consultation with the religious scholars in the region, the local government took a decision to make premarital screening for haemoglobinopathies mandatory by law (Al-Allawi 2008). The program of β-thalassaemia premarital screening for carrier detection was implemented in 2008 by all health authorities in the Kurdistan region, based on the principles of premarital screening, counselling and PND. Preliminary results of the first 3 years (2008–2010) revealed that more than 115,000 individuals were screened and 3.7/1,000 of the couples were identified to be at risk of having children with a major haemoglobinopathy. Of couples at risk, 91 % proceeded with their marriage as scheduled. Of the latter 38 % sought PND in early pregnancy by chorionic villus sampling. The remaining couples either did not seek PND or came late in second trimester, when it is not permissible to perform selective abortion. All couples who underwent PND and had an affected foetus chose to terminate pregnancy (Al-Allawi 2011). The main problems facing the program included the limited awareness of the population on inherited disorders, the high rate of consanguineous marriage (24–27 %), the cost of PND (which is not fully covered by the local authorities) and the limited time between mandatory testing and the actual marriage limiting annulations of marriage plans due to social reasons. Moreover, some couples were not convinced by the results of the screening test given to them. On the other hand, religious beliefs had a limited impact on decisions related to the selective termination of pregnancies with affected foetus.
The program of national mandatory premarital screening for β-thalassemia carriers in Jordan was officially launched in June 2004 after obtaining the consent of the Kingdom Mofti (the highest religious figure in the Kingdom). The basic objectives of the program included primary prevention, as well as early and effective management of affected. The program undertakes screening by estimation of MCV for both partners of the couple contemplating marriage. The report given to the couple following the screening test does not show the results of the test so as to ensure confidentiality. If both partners of the couple prove to have MCV levels pointing to their possible carriers status, their blood samples are further analysed by haemoglobin electrophoresis to estimate the haemoglobin A2 level. If both partners of the couple are diagnosed as carriers, they are provided with genetic counselling explaining their risk of having an affected child and the available prevention measures before giving them the report that is required to certify their marriage. Genetic counselling helps the couple reach the autonomous decisions governing their future marriage plans and reproductive options with no coercion from the health personnel (Hamamy and Al-Hait 2007). Some couples decide to separate especially if the marriage is an arranged marriage. Misconceptions of the carrier status are expected to arise with inevitable stigmatisation, particularly for the female partner. Among 48 at-risk couples screened in 2006, three carrier couples were known to have separated before marriage; however, the exact number is not known, and the outcome of those who decided to marry in spite of the risk is also not known (Hamamy et al. 2007).
The first community genetic service in the Sultanate of Oman was established in 1999 as the national program for the control of genetic blood disorders. It is an integrated strategy combining the best possible patient care, as a first objective, coupled with community education, high-risk population screening and genetic counselling. The program was implemented by regional teams with an administrative setup adequately trained to provide quality care, premarital screening for carrier detection, counselling, health education and data collection (Rajab and Jaffar 2008).
In September 2000, Palestinian West Bank and Gaza adopted a prevention program of obligatory premarital screening for β-thalassaemia carriers among couples contemplating marriage before issuing a marriage certificate. Taking into account social concerns, males were tested initially and the female partner was invited for testing only if her male partner had the basic parameters suspicious of a β-thalassaemia carrier status. From April 2003 to May 2005, 21,825 blood samples from 19,712 couples were collected and analysed. Both partners were carriers in 19 couples, among which, 14 couples decided to separate while five continued with their marriage plans. According to the working protocol of the program, carrier couples were counselled by social and medical specialists. They were given the test results and received genetic and social advice regarding the cancellation of the marriage process because of the possible deleterious consequences on their offspring. If the carrier couple refused to cancel their marriage then both partners had to sign a declaration that stated that they had undertaken the premarital tests, that both were carriers for β-thalassaemia and that both had been counselled by specialists and advised to discontinue the marriage process and seek a new partner. Since the implementation of this program, there has been a reduction in the officially registered births of children with β-thalassaemia major in Gaza strip from 15 births in the year 2000 to 4 births in the year 2005 (Tarazi et al. 2007).
In Saudi Arabia, a national PMS for the most prevalent disorders (thalassemia and sickle cell anaemia) was initiated in 2004 on a voluntary basis in all regions of Saudi Arabia and became compulsory in 2005 where all couples contemplating marriage have to be screened for carrier status before issuing their marriage certificate (Al-Sulaiman et al. 2010). In a cross-sectional, population-based study conducted as part of the national PMS program which covered 207,333 couples applying for a marriage license from February 2004 to January 2005, 2,375 (2.14 %) were declared high risk couples because both partners in a couple were diagnosed to be carriers for a haemoglobinopathy (sickle cell, β-thalassaemia). Of the latter 89.6 % proceeded with their marriage plans. The paper suggests that if the timing of screening was modified to a timing that is well ahead of the arrangements and date of marriage, the number of couples who may decide to separate would be higher (Alhamdan et al. 2007). In another cohort of 129 at-risk individuals who received counselling following premarital screening for haemoglobinopathies, 127 (98 %) decided to proceed with their planned marriage following counselling. The reasons given for their decisions to proceed with the marriage included the commitment to previous family agreement and family pressures (48 %), existing love story (34 %), not being convinced by the PMS results (5 %) and other reasons (13 %). Among the children born within these marriages, 15 % were diseased. The authors suggest that despite the fact that the majority of the participants in this study continued with their marriage, the PMS program is an effective tool for the identification of high-risk population to give them the knowledge for early detection of the disease in their children where more than 50 % of the families screened their children for the targeted diseases for early identification and management. The compliance with the results of this program is increasing with the updated reports from Ministry of Health in Saudi Arabia indicating that the percentage of couples proceeding with their marriage plans dropped to 60.2 % over 2 years (Al-Sulaiman et al. 2010). Among 1.5 million marriage proposals, the frequency of voluntary cancellation of marriage plans among at-risk couples showed more than 5-fold increase between 2004 and 2009 (from 9.2 to 51.9 %). Marriage certificates were issued irrespective of the results and compliance with medical advice was voluntary (Memish and Saeedi 2011). In another study, the marriage status of 934 at-risk couples was determined from the original screening program records in the Ministry of Health showing that 824 married (88.2 %) and 110 (11.8 %) did not. Among 104 at-risk couples who did not proceed with their marriage plans, 28.8 % knew their disease or carrier status before screening compared with 18 % of the 478 at-risk couples who proceeded with their marriage. Couples proceeding with marriage plans said that it was too late to cancel their wedding plans and that they feared social stigmatisation. The at-risk couples who did not marry reported being influenced by prior knowledge of their disease or carrier status and knowledge of the disease in affected family members. Approximately half of all studied at-risk couples (46.4 %) thought that it is best to undergo screening before proceeding with the engagement and wedding plans. Marriage decisions among the 27.6 % of couples who received genetic counselling services did not differ significantly from those who received no counselling. Strengthening public health education and knowledge on genetic diseases, especially before individuals plan to marry through mass media messages and through the school curriculum was recommended. Conducting the premarital screening well in advance of the marriage arrangements and wedding plans is crucial to avoid the social embarrassment of cancelling the marriage. One option to be explored is the introduction of screening during secondary school years (Alswaidi et al. 2012).
In the UAE, premarital genetic counselling, mainly for thalassaemia and sickle cell anaemia, is offered at two primary health care centres in Abu Dhabi within the genetic clinics. Premarital testing for these disorders is encouraged by the government but is not mandatory. However, the option of selective abortion of an affected foetus is not legal in the UAE and therefore not available to at-risk couples (Al-Gazali et al. 2005).
Prenatal genetic diagnosis for haemoglobinopathies in Arab countries
PND is recognised as an important option for the prevention of serious genetic diseases for couples with an increased genetic risk in most developed countries. There are several ethical, legal, social and religious implications regarding pregnancy termination of an affected foetus. Some of these implications are unique to Arab countries.
Amniocentesis and chorionic villus sampling for obtaining foetal cells can be performed by skilled and experienced obstetricians in many Arab countries, and most molecular laboratories are capable of diagnosing single gene disorders, such as the haemoglobinopathies. However, there is a diversity of opinions among Islamic institutions on the issue of pregnancy termination, ranging from an absolute prohibition of abortion at any time to permission for pregnancy termination before the 120th day of gestation under specific circumstances. All Arab countries permit abortion to save the life of a pregnant woman, but otherwise they differ quite widely in their legal indications for selective termination of a pregnancy with a severely affected foetus (Al-Aqeel 2007), in Tunisia, for example, selective abortion of an affected foetus is permissible under civil law (Chaabouni et al. 2001).
PND for β-thalassemia in Egypt showed that in 14 out of 22 PND, the parents chose to continue pregnancy (selective termination of pregnancy rate was 36.3 %). The mean gestation period at the time of PND was 14 (10–18) weeks. All mothers had a previous affected pregnancy, and 13 had two or more previous affected pregnancies (Elgawhary et al. 2008). On the other hand, a more recent study presenting the current status of the PND services and results from the largest thalassaemia centre in Egypt treating 3,000 patients showed that all 24 women who underwent prenatal testing and received a diagnosis that the foetus is affected by β-thalassemia major opted for pregnancy termination. The study demonstrated that PND is feasible and acceptable in Egypt, a Muslim country, provided an in-depth discussion, which also addresses the religious considerations of prevention, is held with the couples (El-Beshlawy et al. 2012). A prestructured questionnaire was administered to families in Saudi Arabia who have children affected by a major haemoglobinopathy to assess their attitude and acceptability of PND and selective termination of affected foetus. Among the 32 families who were interviewed, the majority accepted PND (81.3 %). The attitude towards abortion was, however, greatly influenced by religious values (Alkuraya and Kilani 2001). In Lebanon, 83 couples at risk for a haemoglobin disorder in their children, mostly β-thalassaemia were interviewed to evaluate their attitude towards first-trimester PND. Fifty-nine per cent of the couples were in favour of PND, 23 % were uncertain at the time of the interview and 18 % were opposed to such testing, because of their religious conviction against termination of a pregnancy. Another important factor which seems to influence choice was the cost of the test (Zahed and Bou-Dames 1997). Among another group of families having thalassemia major children, the majority were in favour of a preventive approach based on heterozygote screening and the possibility of PND (Der Kaloustian et al. 1987).
Among 88 at-risk couples from the West Bank and Gaza, 130 prenatal samples assessing β-thalassemia major in foetus from January 1999 to July 2005 were drawn. Samples showed 25 (19.2 %) cases of β-thalassemia major, 67 (51.5 %) cases of β-thalassemia carriers and 38 cases (29.2 %) of unaffected homozygotes. The 25 affected foetuses were aborted according to the wishes of the parents indicating a very good acceptability for PND of β-thalassemia in afflicted families (Ayesh et al. 2005)
Preimplantation genetic diagnosis
Unlike PND, preimplantation genetic diagnosis (PGD) offers couples an option that avoids the difficult decision of selective termination of an affected pregnancy. PGD is a process in which embryos developed by in vitro fertilisation (IVF) are tested for particular genetic diseases before being implanted in the uterus. PGD has been proposed as a valuable alternative to PND. PGD is permissible in Islam provided the sperms and oocytes are from the husband and wife (Al-Sulaiman et al. 2010).
The acceptability of PGD has been explored in some studies in Saudi Arabia which is at present the only Arab country where PGD is available. Thirty couples attending the King Faisal Specialist Hospital and Research Centre in Riyadh were interviewed using a semi-structured questionnaire. Eight of the 30 couples (27 %) would only accept PGD, four (13 %) only PND, three (10 %) either technology and the remainder would accept neither or were unsure. The main concerns of those who would accept neither technology were related to personal religious views. Specific concerns about PGD were related to the IVF procedure, the risk of multiple pregnancies, the chance of mistakes and the chance of not getting pregnant. A high proportion of couples (six out of seven; 86 %) who had a child with thalassemia expressed interest in PGD, and all would be prepared to use this technology to avoid having an affected child (Al-Sulaiman and Hewison 2006). For PGD families, the most stressful aspect of the whole procedure was the psychological stress of waiting to learn if pregnancy had been established. PGD is not an easy option for families, and counselling services are needed to advise, prepare and support them through all the difficult stages that the technology entails (Al-Sulaiman et al. 2010). In Lebanon, 97 women with a previously affected thalassemic child were offered a genetic counselling session followed by administering a questionnaire through direct interview. Sixty-eight per cent of women considered PGD a better alternative to PND. The most important perceived advantage of PGD was the avoidance of termination of an affected pregnancy (Farra et al. 2008)
Conclusions and recommendations
The considerable challenge posed by the high prevalence rates of haemoglobinopathies in Arab countries calls for the development of care and prevention national programmes through the establishment of public health services that do not require sophisticated technical facilities but are primarily based on strengthening the training of health professionals and on public education. The strategies adopted should, however, be carefully selected to match the unique demographic, cultural and religious characteristics of each population and take into consideration the priorities set and the resources available. Community services that have proven their efficacy in lowering the prevalence rate of β-thalassemia and SCD while at the same time offering timely management include NBS and premarital screening to detect carriers of these disorders coupled with genetic counselling. However, experience in some countries had shown that if options are not made available to carrier couples, such programmes will not be effective in reducing the burden of haemoglobinapathies. In particular, the issue of selective termination of an affected foetus remains fraught, with marked attitudinal differences between countries involving both the religious and legal authorities and families who are directly affected. Some studies have recommended screening for carriers of haemoglobinopathies among high school students, ahead of marriage arrangements. Prerequisites for considering such options would be to raise awareness through targeted education of the public. Given the knowledge barrier experienced by many health care providers in the implementation of health interventions at community level, structured courses and educational campaigns to train and educate primary health care workers in premarital, preconceptionl and prescreening counselling should be considered essential components of any national strategy for the prevention of haemoglobinopathies. Knowledge of the molecular defects in each country allows the development and improvement of diagnostic tests and management protocols for these disorders.
Contributor Information
Hanan A. Hamamy, Email: Hananhamamy@yahoo.com
Nasir A. S. Al-Allawi, Email: nallawi@yahoo.com
References
- Abbes S, Fattoum S, Vidaud M, Goossens M, Rosa J. Sickle cell anemia in the Tunisian population: haplotyping and HB F expression. Hemoglobin. 1991;15:1–9. doi: 10.3109/03630269109072480. [DOI] [PubMed] [Google Scholar]
- Abu-Ghoush MW. Subtypes of alpha thalassemia diagnosed at a Medical Center in Jordan. TAF Prev Med Bull. 2008;7(5):373–376. [Google Scholar]
- Abuzenadah AM, Hussein IM, Damanhouri GA, Sayes FM, Gari MA, Chaudhary AG, Zaher GF, Al-Attas A, Al-Qahtani MH. Molecular basis of beta-thalassemia in the western province of Saudi Arabia: identification of rare beta-thalassemia mutations. Hemoglobin. 2011;35:346–357. doi: 10.3109/03630269.2011.588508. [DOI] [PubMed] [Google Scholar]
- Adekile AD. Sickle cell disease in Kuwait. Hemoglobin. 2001;25:219–225. doi: 10.1081/HEM-100104030. [DOI] [PubMed] [Google Scholar]
- Adekile AD, Gu LH, Baysal E, Haider MZ, Al-Fuzae L, Aboobacker KC, Al-Rashied A, Huisman TH. Molecular characterization of alpha-thalassemia determinants, beta-thalassemia alleles, and beta S haplotypes among Kuwaiti Arabs. Acta Haematol. 1994;92:176–181. doi: 10.1159/000204216. [DOI] [PubMed] [Google Scholar]
- Agouti I, Badens C, Abouyoub A, Khattab M, Sayah F, Barakat A, Bennani M. Genotypic correlation between six common beta-thalassemia mutations and the XmnI polymorphism in the Moroccan population. Hemoglobin. 2007;31:141–149. doi: 10.1080/03630260701285050. [DOI] [PubMed] [Google Scholar]
- Agouti I, Badens C, Abouyoub A, Levy N, Bennani M. Molecular basis of beta-thalassemia in Morocco: possible origins of the molecular heterogeneity. Genet Test. 2008;12:563–568. doi: 10.1089/gte.2008.0058. [DOI] [PubMed] [Google Scholar]
- Al-Aqeel AI. Islamic ethical framework for research into and prevention of genetic diseases. Nat Genet. 2007;39:1293–1298. doi: 10.1038/ng.2007.14. [DOI] [PubMed] [Google Scholar]
- Al-Hosani H, Salah M, Osman HM, Farag HM, Anvery SM. Incidence of haemoglobinopathies detected through neonatal screening in the United Arab Emirates. East Mediterr Health J. 2005;11:300–307. [PubMed] [Google Scholar]
- Al-Ali AK, Al-Ateeq S, Imamwerdi BW, Al-Sowayan S, Al-Madan M, Al-Muhanna F, Bashaweri L, Qaw F (2005) Molecular bases of beta-thalassemia in the Eastern Province of Saudi Arabia. J Biomed Biotechnol 322–325 [DOI] [PMC free article] [PubMed]
- Al-Allawi N. The preventive program for hemoglobinopathies in Duhok: an option or a necessity. Duhok Med J. 2008;2(1):1–4. [Google Scholar]
- Al-Allawi N. Molecular characterization of inherited haematological disorders in Iraqis: trying to bridge the gap. HUGO J. 2011;5:124. [Google Scholar]
- Al-Allawi NA, Al-Dousky AA. Frequency of haemoglobinopathies at premarital health screening in Dohuk, Iraq: implications for a regional prevention programme. East Mediterr Health J. 2010;16:381–385. [PubMed] [Google Scholar]
- Al-Allawi NA, Jubrael JM, Hughson M. Molecular characterization of beta-thalassemia in the Dohuk region of Iraq. Hemoglobin. 2006;30:479–486. doi: 10.1080/03630260600868097. [DOI] [PubMed] [Google Scholar]
- Al-Allawi NA, Badi AI, Imanian H, Nikzat N, Jubrael JM, Najmabadi H. Molecular characterization of alpha-thalassemia in the Dohuk region of Iraq. Hemoglobin. 2009;33:37–44. doi: 10.1080/03630260802626053. [DOI] [PubMed] [Google Scholar]
- Al-Allawi NA, Hassan KM, Sheikha AK, Nerweiy FF, Dawood RS, Jubrael J (2010a) Beta-thalassemia mutations among transfusion-dependent thalassemia major patients in Northern Iraq. Mol Biol Int 2010:479282 [DOI] [PMC free article] [PubMed]
- Al-Allawi NA, Shamdeen MY, Rasheed NS. Homozygosity for the Mediterranean α-thalassemic deletion (hemoglobin Barts hydrops fetalis) Ann Saudi Med. 2010;30:153–155. doi: 10.4103/0256-4947.60523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Allawi NA, Jalal SD, Nerwey FF, Al-Sayan GO, Al-Zebari SS, Alshingaly AA, Markous RD, Jubrael JM, Hamamy H. Sickle cell disease in the Kurdish population of northern Iraq. Hemoglobin. 2012;36:333–342. doi: 10.3109/03630269.2012.692344. [DOI] [PubMed] [Google Scholar]
- Al-Arrayad S (2006) Genetic diseases in Bahrain. In: Tadmouri GO, Taleb Al-Ali M, Al-Khaja N (eds) Genetic disorders in the Arab World: Bahrain. Centre for Arab Genomic Studies, Dubai
- Al-Arrayed S. Beta globin gene haplotypes in Bahraini patients with sickle cell anemia. Bahrain Med Bull. 1995;17(1):15–20. [Google Scholar]
- Al-Arrayed S. Campaign to control genetic blood diseases in Bahrain. Community Genet. 2005;8:52–55. doi: 10.1159/000083340. [DOI] [PubMed] [Google Scholar]
- Al-Arrayed (2007) WHO-TIF meeting on the management of Hemoglobin disorders, Nicosia, Cyprus, 16–18 November
- Al-Arrayed S, Al-Hajeri A. Public awareness of sickle cell disease in Bahrain. Ann Saudi Med. 2010;30:284–288. doi: 10.4103/0256-4947.65256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Arrayed S, Al-Hajeri A. Newborn screening services in Bahrain between 1985 and 2010. Adv Hematol. 2012;2012:903219. doi: 10.1155/2012/903219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Arrayed S, Hafadh N, Al-Serasi S. Premarital counselling: an experience from Bahrain. East Med Health J. 1997;3:415–419. [Google Scholar]
- Al-Arrayed S, Hafadh N, Amin S, Al-Mukhareq H, Sanad H. Student screening for inherited blood disorders in Bahrain. East Mediterr Health J. 2003;9:344–352. [PubMed] [Google Scholar]
- Al-Awamy BH. Thalassemia syndromes in Saudi Arabia. Meta-analysis of local studies. Saudi Med J. 2000;21:8–17. [PubMed] [Google Scholar]
- Al-Awamy BH, Al-Muzan M, Al-Turki M, Serjeant GR. Neonatal screening for sickle cell disease in the Eastern Province of Saudi Arabia. Trans R Soc Trop Med Hyg. 1984;78:792–794. doi: 10.1016/0035-9203(84)90023-3. [DOI] [PubMed] [Google Scholar]
- Al-Gazali LI, Alwash R, Abdulrazzaq YM. United Arab Emirates: communities and community genetics. Community Genet. 2005;8:186–196. doi: 10.1159/000086764. [DOI] [PubMed] [Google Scholar]
- Al-Gazali L, Hamamy H, Al-Arrayad S. Genetic disorders in the Arab world. BMJ. 2006;333:831–834. doi: 10.1136/bmj.38982.704931.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhamdan NA, Almazrou YY, Alswaidi FM, Choudhry AJ. Premarital screening for thalassemia and sickle cell disease in Saudi Arabia. Genet Med. 2007;9:372–377. doi: 10.1097/GIM.0b013e318065a9e8. [DOI] [PubMed] [Google Scholar]
- Alkindi S, Al-Zadjali S, Al-Madhani A, Daar S, Al-Haddabi H, Al-Abri Q, Gravell D, Berbar T, Pravin S, Pathare A, Krishnamoorthy R. Forecasting hemoglobinopathy burden through neonatal screening in Omani neonates. Hemoglobin. 2010;34:135–144. doi: 10.3109/03630261003677213. [DOI] [PubMed] [Google Scholar]
- Alkindi S, Pathare A, Al-Madhani A, Al-Zadjali S, Al-Haddabi H, Al-Abri Q, Gravell D, Mathew M, Krishnamoorthy R. Neonatal Screening: mean haemoglobin and red cell indices in cord blood from Omani neonates. Sultan Qaboos Univ Med J. 2011;11:462–469. [PMC free article] [PubMed] [Google Scholar]
- Alkuraya FS, Kilani RA. Attitude of Saudi families affected with hemoglobinopathies towards prenatal screening and abortion and the influence of religious ruling (Fatwa) Prenat Diagn. 2001;21:448–451. doi: 10.1002/pd.76. [DOI] [PubMed] [Google Scholar]
- Almutawa F, Alqamish J. Prevalence of hemoglobinopathies among candidates attending premarital counseling in Bahrain. J Bahrain Med Soc. 2008;20(4):145–149. [Google Scholar]
- Al-Nood H. Thalassemia trait in outpatient clinics of Sana’a City, Yemen. Hemoglobin. 2009;33:242–246. doi: 10.1080/03630260903039594. [DOI] [PubMed] [Google Scholar]
- Al-Nood H, Al-Ismail S, King L, May A. Prevalence of the sickle cell gene in Yemen: a pilot study. Hemoglobin. 2004;28:305–315. doi: 10.1081/HEM-200037708. [DOI] [PubMed] [Google Scholar]
- Al-Obaidli A, Hamodat M, Fawzi Z, Abu-Laban M, Gerard N, Krishnamoorthy R. Molecular basis of thalassemia in Qatar. Hemoglobin. 2007;31:121–127. doi: 10.1080/03630260701288815. [DOI] [PubMed] [Google Scholar]
- Al-Qurashi MM, El-Mouzan MI, Al-Herbish AS, Al-Salloum AA, Al-Omar AA. The prevalence of sickle cell disease in Saudi children and adolescents. A community-based survey. Saudi Med J. 2008;29:1480–1483. [PubMed] [Google Scholar]
- Al-Riyami A, Ebrahim GJ. Genetic blood disorders survey in the Sultanate of Oman. J Trop Pediatr. 2003;49(Suppl 1):i1–i20. [PubMed] [Google Scholar]
- Al-Riyami AA, Suleiman AJ, Afifi M, Al-Lamki ZM, Daar S. A community-based study of common hereditary blood disorders in Oman. East Mediterr Health J. 2001;7:1004–1011. [PubMed] [Google Scholar]
- Al-Sulaiman A, Hewison J. Attitudes to prenatal and preimplantation diagnosis in Saudi parents at genetic risk. Prenat Diagn. 2006;26:1010–1014. doi: 10.1002/pd.1544. [DOI] [PubMed] [Google Scholar]
- Al-Sulaiman A, Saeedi M, Al-Suliman A, Owaidah T. Postmarital follow-up survey on high risk patients subjected to premarital screening program in Saudi Arabia. Prenat Diagn. 2010;30:478–481. doi: 10.1002/pd.2507. [DOI] [PubMed] [Google Scholar]
- Al-Sulaiman A, Al-Odaib A, Al-Rejjal R, Hewison J. Preimplantation genetic diagnosis in Saudi Arabia: parents’ experience and attitudes. Prenat Diagn. 2010;30:753–757. doi: 10.1002/pd.2532. [DOI] [PubMed] [Google Scholar]
- Al-Suliman A. Prevalence of beta-thalassemia trait in premarital screening in Al-Hassa, Saudi Arabia. Ann Saudi Med. 2006;26:14–16. doi: 10.5144/0256-4947.2006.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Sultan A, Phanasgaonkar S, Suliman A, Al-Baqushi M, Nasrullah Z, Al-Ali A. Spectrum of beta-thalassemia mutations in the eastern province of Saudi Arabia. Hemoglobin. 2011;35:125–134. doi: 10.3109/03630269.2011.553567. [DOI] [PubMed] [Google Scholar]
- Alswaidi FM, Memish ZA, O’Brien SJ, Al-Hamdan NA, Al-Enzy FM, Alhayani OA, Al-Wadey AM. At-risk marriages after compulsory premarital testing and counseling for beta-thalassemia and sickle cell disease in Saudi Arabia, 2005–2006. J Genet Couns. 2012;21:243–255. doi: 10.1007/s10897-011-9395-4. [DOI] [PubMed] [Google Scholar]
- Alwan A and Modell B (1997) Community control of genetic and congenital disorders. EMRO Technical Publication Series 24: WHO Regional Office for the Eastern Mediterranean Region, Egypt
- Ayesh SK, Al-Sharef WA, Nassar SM, Thawabteh NA, Abu-Libdeh BY. Prenatal diagnosis of beta-thalassemia in the West Bank and Gaza. Saudi Med J. 2005;26:1771–1776. [PubMed] [Google Scholar]
- Babiker MM, Bashir N, Sarsour N. Prevalence of thalassaemia in schoolchildren in north-eastern Badia, Jordan. East Mediterr Health J. 1999;5:1165–1170. [PubMed] [Google Scholar]
- Badens C, di Martinez MF, Thuret I, Michel G, Mattei JF, Cappellini MD, Lena-Russo D. Molecular basis of haemoglobinopathies and G6PD deficiency in the Comorian population. Hematol J. 2000;1:264–268. doi: 10.1038/sj.thj.6200042. [DOI] [PubMed] [Google Scholar]
- Bashir N, Barkawi M, Sharif L. Prevalence of haemoglobinopathies in school children in Jordan Valley. Ann Trop Paediatr. 1991;11:373–376. doi: 10.1080/02724936.1991.11747532. [DOI] [PubMed] [Google Scholar]
- Bashir N, Barkawi M, Sharif L, Momani A, Gharaibeh N. Prevalence of hemoglobinopathies in north Jordan. Trop Geogr Med. 1992;44:122–125. [PubMed] [Google Scholar]
- Baysal E. Hemoglobinopathies in the United Arab Emirates. Hemoglobin. 2001;25:247–253. doi: 10.1081/HEM-100104033. [DOI] [PubMed] [Google Scholar]
- Baysal E. Molecular heterogeneity of beta-thalassemia in the United Arab Emirates. Community Genet. 2005;8:35–39. doi: 10.1159/000083336. [DOI] [PubMed] [Google Scholar]
- Baysal E. Molecular basis of beta-thalassemia in the United Arab Emirates. Hemoglobin. 2011;35:581–588. doi: 10.3109/03630269.2011.634706. [DOI] [PubMed] [Google Scholar]
- Baysal E, Indrak K, Bozkurt G, Berkalp A, Aritkan E, Old JM, Ioannou P, Angastiniotis M, Droushiotou A, Yuregir GT. The beta-thalassaemia mutations in the population of Cyprus. Br J Haematol. 1992;81:607–609. doi: 10.1111/j.1365-2141.1992.tb03000.x. [DOI] [PubMed] [Google Scholar]
- Bennani C, Bouhass R, Perrin-Pecontal P, Tamouza R, Malou M, Elion J, Trabuchet G, Beldjord C, Benabadji M, Labie D. Anthropological approach to the heterogeneity of beta-thalassemia mutations in northern Africa. Hum Biol. 1994;66:369–382. [PubMed] [Google Scholar]
- Bittles A (2012) The global prevalence of consanguinity. Available from http://www.consang.net/
- Boudrahem-Addour N, Zidani N, Carion N, Labie D, Belhani M, Beldjord C. Molecular heterogeneity of beta-thalassemia in Algeria: how to face up to a major health problem. Hemoglobin. 2009;33:24–36. doi: 10.1080/03630260802626061. [DOI] [PubMed] [Google Scholar]
- Center for Arab Genomic Studies (2012). Available from http://www.cags.org.ae/ctga_search.html
- Chaabouni H, Chaabouni M, Maazoul F, M’rad R, Jemaa LB, Smaoui N, Terras K, Kammoun H, Belghith N, Ridene H, Oueslati B, Zouari F. Prenatal diagnosis of chromosome disorders in Tunisian population. Ann Genet. 2001;44:99–104. doi: 10.1016/S0003-3995(01)01046-2. [DOI] [PubMed] [Google Scholar]
- Charafeddine K, Isma’eel H, Charafeddine M, Inati A, Koussa S, Naja M, Taher A. Survival and complications of beta-thalassemia in Lebanon: a decade’s experience of centralized care. Acta Haematol. 2008;120:112–116. doi: 10.1159/000171088. [DOI] [PubMed] [Google Scholar]
- Chouk I, Daoud BB, Mellouli F, Bejaoui M, Gerard N, Dellagi K, Abbes S. Contribution to the description of the beta-thalassemia spectrum in Tunisia and the origin of mutation diversity. Hemoglobin. 2004;28:189–195. doi: 10.1081/HEM-120040305. [DOI] [PubMed] [Google Scholar]
- Curuk MA. Hb H (beta4) disease in Cukurova, Southern Turkey. Hemoglobin. 2007;31:265–271. doi: 10.1080/03630260701297279. [DOI] [PubMed] [Google Scholar]
- Daar S, Hussein HM, Merghoub T, Krishnamoorthy R. Spectrum of beta-thalassemia mutations in Oman. Ann N Y Acad Sci. 1998;850:404–406. doi: 10.1111/j.1749-6632.1998.tb10504.x. [DOI] [PubMed] [Google Scholar]
- Daar S, Hussain HM, Gravell D, Nagel RL, Krishnamoorthy R. Genetic epidemiology of HbS in Oman: multicentric origin for the betaS gene. Am J Hematol. 2000;64:39–46. doi: 10.1002/(SICI)1096-8652(200005)64:1<39::AID-AJH7>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- Darwish HM, El-Khatib FF, Ayesh S. Spectrum of beta-globin gene mutations among thalassemia patients in the West Bank region of Palestine. Hemoglobin. 2005;29:119–132. doi: 10.1081/HEM-200058581. [DOI] [PubMed] [Google Scholar]
- Der Kaloustian VM, Khudr A, Firzli S, Dabbous I. Psychosocial and economic profile of a sample of families with thalassaemic children in Lebanon. J Med Genet. 1987;24:772–777. doi: 10.1136/jmg.24.12.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyde VM, Lo BB, Khalifa IO, Ly B, Ball A, Fattoum S. Epidemiological profile of hemoglobinopathies in the Mauritanian population. Ann Hematol. 2002;81:320–321. doi: 10.1007/s00277-002-0471-6. [DOI] [PubMed] [Google Scholar]
- Di RA, Novelletto A, Aliquo MC, Bianco I, Tagarelli A, Brancati C, Colombo B, Felicetti L. Molecular basis for HbH disease in Italy: geographical distribution of deletional and nondeletional alpha-thalassemia haplotypes. Am J Hum Genet. 1986;39:631–639. [PMC free article] [PubMed] [Google Scholar]
- Diejomaoh FM, Haider MZ, Dalal H, Abdulaziz A, D’Souza TM, Adekile AD. Influence of alpha-thalassemia trait on the prevalence and severity of anemia in pregnancy among women in Kuwait. Acta Haematol. 2000;104:92–94. doi: 10.1159/000039757. [DOI] [PubMed] [Google Scholar]
- El-Beshlawy A, Youssry I. Prevention of hemoglobinopathies in Egypt. Hemoglobin. 2009;33(Suppl 1):S14–S20. doi: 10.3109/03630260903346395. [DOI] [PubMed] [Google Scholar]
- El-Beshlawy A, Kaddah N, Moustafa A, Mouktar G, Youssry I. Screening for beta-thalassaemia carriers in Egypt: significance of the osmotic fragility test. East Mediterr Health J. 2007;13:780–786. [PubMed] [Google Scholar]
- El-Beshlawy A, El-Shekha A, Momtaz M, Said F, Hamdy M, Osman O, Meshaal S, Gafaar T, Petrou M. Prenatal diagnosis for thalassaemia in Egypt: what changed parents’ attitude? Prenat Diagn. 2012;32:777–782. doi: 10.1002/pd.3901. [DOI] [PubMed] [Google Scholar]
- Elgawhary S, Elbaradie Sahar MY, Rashad WM, Mosaad M, Abdalla MA, Ezzat G, Wali YA, Elbeshlawy A. Prenatal diagnosis of beta-thalassemia in Egypt: implementing accurate high-tech methods did not reflect much on the outcome. Pediatr Hematol Oncol. 2008;25:541–548. doi: 10.1080/08880010802313509. [DOI] [PubMed] [Google Scholar]
- El-Gawhary S, El-Shafie S, Niazi M, Aziz M, El-Beshlawy A. Study of beta-thalassemia mutations using the polymerase chain reaction–amplification refractory mutation system and direct DNA sequencing techniques in a group of Egyptian thalassemia patients. Hemoglobin. 2007;31:63–69. doi: 10.1080/03630260601057104. [DOI] [PubMed] [Google Scholar]
- El-Harth EH, Kuhnau W, Schmidtke J, Stuhrmann M, Nasserallah Z, Al-Shahiri A. Identification and clinical presentation of beta thalassaemia mutations in the eastern region of Saudi Arabia. J Med Genet. 1999;36:935–937. [PMC free article] [PubMed] [Google Scholar]
- El-Hazemi MAF, Warsy AS, Bashir N, et al. Haplotypes of the â-globin gene as prognostic factors in sickle cell disease. East Mediterr Health J. 1999;5(6):1154–1158. [PubMed] [Google Scholar]
- El-Hazmi MA. Islamic teachings of bioethics in relation to the practice of medical genetics. Saudi Med J. 2007;28:1781–1787. [PubMed] [Google Scholar]
- El-Hazmi MA, Warsy AS. The frequency of glucose-6-phosphate dehydrogenase phenotypes and sickle cell genes in Al-Qatif oasis. Ann Saudi Med. 1994;14:491–494. doi: 10.5144/0256-4947.1994.491. [DOI] [PubMed] [Google Scholar]
- El-Hazmi MA, Warsy AS. Appraisal of sickle-cell and thalassaemia genes in Saudi Arabia. East Mediterr Health J. 1999;5:1147–1153. [PubMed] [Google Scholar]
- El-Hazmi MA, Al-Swailem AR, Warsy AS. Molecular defects in beta-thalassaemias in the population of Saudi Arabia. Hum Hered. 1995;45:278–285. doi: 10.1159/000154314. [DOI] [PubMed] [Google Scholar]
- El-Kalla S, Baysal E. Alpha-thalassemia in the United Arab Emirates. Acta Haematol. 1998;100:49–53. doi: 10.1159/000040863. [DOI] [PubMed] [Google Scholar]
- El-Kalla S, Baysal E. Genotype-phenotype correlation of sickle cell disease in the United Arab Emirates. Pediatr Hematol Oncol. 1998;15:237–242. doi: 10.3109/08880019809028790. [DOI] [PubMed] [Google Scholar]
- El-Latif MA, Filon D, Rund D, Oppenheim A, Kanaan M. The beta+−IVS-I-6 (T–>C) mutation accounts for half of the thalassemia chromosomes in the Palestinian populations of the mountain regions. Hemoglobin. 2002;26:33–40. doi: 10.1081/HEM-120002938. [DOI] [PubMed] [Google Scholar]
- El-Tayeb EN, Yaqoob M, Abdur-Rahim K, Gustavson KH. Prevalence of beta-thalassaemia and sickle cell traits in premarital screening in Al-Qassim, Saudi Arabia. Genet Couns. 2008;19:211–218. [PubMed] [Google Scholar]
- Farra C, Nassar AH, Usta IM, Salameh P, Souaid M, Awwad J. Acceptance of preimplantation genetic diagnosis for beta-thalassemia in Lebanese women with previously affected children. Prenat Diagn. 2008;28:828–832. doi: 10.1002/pd.2067. [DOI] [PubMed] [Google Scholar]
- Fattoum S. Hemoglobinopathies in Tunisia. An updated review of the epidemiologic and molecular data. Tunis Med. 2006;84:687–696. [PubMed] [Google Scholar]
- Fattoum S, Messaoud T, Bibi A. Molecular basis of beta-thalassemia in the population of Tunisia. Hemoglobin. 2004;28:177–187. doi: 10.1081/HEM-120040307. [DOI] [PubMed] [Google Scholar]
- Filon D, Oron V, Krichevski S, Shaag A, Shaag Y, Warren TC, Goldfarb A, Shneor Y, Koren A, Aker M. Diversity of beta-globin mutations in Israeli ethnic groups reflects recent historic events. Am J Hum Genet. 1994;54:836–843. [PMC free article] [PubMed] [Google Scholar]
- Filon D, Oron V, Shawa R, Elborno E, Najjar K, Tulchinsky T, Rachmilewitz E, Rund D, Oppenheim A. Spectrum of beta-thalassemia mutations in the Gaza area. Hum Mutat. 1995;5:351–353. doi: 10.1002/humu.1380050416. [DOI] [PubMed] [Google Scholar]
- Flint J, Harding RM, Clegg JB, Boyce AJ. Why are some genetic diseases common? Distinguishing selection from other processes by molecular analysis of globin gene variants. Hum Genet. 1993;91:91–117. doi: 10.1007/BF00222709. [DOI] [PubMed] [Google Scholar]
- Galanello R, Eleftheriou A, Traeger-Synedinos J, Old J, Petrou M, Angastiniotis M. Prevention of thalassaemia and other haemoglobin disorders, vol. 1. Nicosia: Thalassaemia International Federation Publications; 2003. [PubMed] [Google Scholar]
- Ganeshaguru K, Acquaye JK, Samuel AP, Hassounah F, Agyeiobese S, Azrai LM, Sejeny SA, Omer A. Prevalence of thalassaemias in ethnic Saudi Arabians. Trop Geogr Med. 1987;39:238–243. [PubMed] [Google Scholar]
- Gupta A, Hattori Y, Gupta UR, Sarwai S, Nigam N, Singhal P, Agarwal S. Molecular genetic testing of beta-thalassemia patients of Indian origin and a novel 8-bp deletion mutation at codons 36/37/38/39. Genet Test. 2003;7:163–168. doi: 10.1089/109065703322146894. [DOI] [PubMed] [Google Scholar]
- Hadavi V, Taromchi AH, Malekpour M, Gholami B, Law HY, Almadani N, Afroozan F, Sahebjam F, Pajouh P, Kariminejad R, Kariminejad MH, Azarkeivan A, Jafroodi M, Tamaddoni A, Puehringer H, Oberkanins C, Najmabadi H. Elucidating the spectrum of alpha-thalassemia mutations in Iran. Haematologica. 2007;92:992–993. doi: 10.3324/haematol.10658. [DOI] [PubMed] [Google Scholar]
- Haider M, Adekile A. Alpha-2-globin gene polyadenylation (AATAAA–>AATAAG) mutation in hemoglobin H disease among Kuwaitis. Med Princ Pract. 2005;14(Suppl 1):73–76. doi: 10.1159/000086187. [DOI] [PubMed] [Google Scholar]
- Haj Khelil A, Denden S, Leban N, Daimi H, Lakhdhar R, Lefranc G, Ben CJ, Perrin P. Hemoglobinopathies in North Africa: a review. Hemoglobin. 2010;34:1–23. doi: 10.3109/03630260903571286. [DOI] [PubMed] [Google Scholar]
- Hajer S, Neila T, Sondess HF, Fekria O, Nabila A, Mahbouba K, Melika D, Faida O, Amina B, Raja B, Hedi R, Sadok M, Naima K, Slaheddine F, Taieb M. A lower-cost protocol for sickle cell disease neonatal screening in Tunisia. Ann Saudi Med. 2012;32:49–52. doi: 10.5144/0256-4947.2012.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamamy H and Al-Hait S (2007) Premarital Screening program for beta-thalassemia in Jordan. Available from http://ambassadors.net/archives/issue21/selectedstudy.htm
- Hamamy H, Alwan A. Hereditary disorders in the Eastern Mediterranean Region. Bull World Health Organ. 1994;72:145–154. [PMC free article] [PubMed] [Google Scholar]
- Hamamy H, Bittles AH. Genetic clinics in Arab communities: meeting individual, family and community needs. Public Health Genom. 2008;12:30–40. doi: 10.1159/000153428. [DOI] [PubMed] [Google Scholar]
- Hamamy H, Al-Hait S, Alwan A, Ajlouni K. Jordan: communities and community genetics. Community Genet. 2007;10:52–60. doi: 10.1159/000096282. [DOI] [PubMed] [Google Scholar]
- Harteveld CL, Higgs DR. Alpha-thalassaemia. Orphanet J Rare Dis. 2010;5:13. doi: 10.1186/1750-1172-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan MK, Taha JY, Al-Naama LM, Widad NM, Jasim SN. Frequency of haemoglobinopathies and glucose-6-phosphate dehydrogenase deficiency in Basra. East Mediterr Health J. 2003;9:45–54. [PubMed] [Google Scholar]
- Hassan SM, Hamza N, Jaffer Al-Lawatiya F, Jaffer MA, Harteveld CL, Rajab A, Giordano PC. Extended molecular spectrum of beta- and alpha-thalassemia in Oman. Hemoglobin. 2010;34:127–134. doi: 10.3109/03630261003673147. [DOI] [PubMed] [Google Scholar]
- Hellani A, Fadel E, El-Sadadi S, El-Sweilam H, El-Dawood A, Abu-Amero KK. Molecular spectrum of alpha-thalassemia mutations in microcytic hypochromic anemia patients from Saudi Arabia. Genet Test Mol Biomarkers. 2009;13:219–221. doi: 10.1089/gtmb.2008.0123. [DOI] [PubMed] [Google Scholar]
- Henderson S, Timbs A, McCarthy J, Gallienne A, Van MM, Masters G, May A, Khalil MS, Schuh A, Old J. Incidence of haemoglobinopathies in various populations—the impact of immigration. Clin Biochem. 2009;42:1745–1756. doi: 10.1016/j.clinbiochem.2009.05.012. [DOI] [PubMed] [Google Scholar]
- Higgs DR, Goodbourn SE, Lamb J, Clegg JB, Weatherall DJ, Proudfoot NJ. Alpha-thalassaemia caused by a polyadenylation signal mutation. Nature. 1983;306:398–400. doi: 10.1038/306398a0. [DOI] [PubMed] [Google Scholar]
- Hussein IR, Temtamy SA, El-Beshlawy A, Fearon C, Shalaby Z, Vassilopoulos G, Kazazian HH., Jr Molecular characterization of beta-thalassemia in Egyptians. Hum Mutat. 1993;2:48–52. doi: 10.1002/humu.1380020109. [DOI] [PubMed] [Google Scholar]
- Hussein G, Fawzy M, Serafi TE, Ismail EF, Metwally DE, Saber MA, Giansily M, Schved JF, Pissard S, Martinez PA. Rapid detection of beta-thalassemia alleles in Egypt using naturally or amplified created restriction sites and direct sequencing: a step in disease control. Hemoglobin. 2007;31:49–62. doi: 10.1080/03630260601057088. [DOI] [PubMed] [Google Scholar]
- Inati A, Taher A, Bou AW, Koussa S, Kaspar H, Shbaklo H, Zalloua PA. Beta-globin gene cluster haplotypes and HbF levels are not the only modulators of sickle cell disease in Lebanon. Eur J Haematol. 2003;70:79–83. doi: 10.1034/j.1600-0609.2003.00016.x. [DOI] [PubMed] [Google Scholar]
- Jain RC. Haemoglobinopathies in Libya. J Trop Med Hyg. 1979;82(6):128–132. [PubMed] [Google Scholar]
- Jain RC. Sickle cell and thalassaemic genes in Libya. Trans R Soc Trop Med Hyg. 1985;79:132–133. doi: 10.1016/0035-9203(85)90257-3. [DOI] [PubMed] [Google Scholar]
- Jalal SD, Al-Alawi NA, Faraj AH, Ahmed NH. Prevalence of hemoglobinopathies in Sulaimani-Iraq. Dohuk Med J. 2008;2(1):71–79. [Google Scholar]
- Jalal SD, Al-Allawi NA, Bayat N, Imanian H, Najmabadi H, Faraj A. Beta-thalassemia mutations in the Kurdish population of northeastern Iraq. Hemoglobin. 2010;34:469–476. doi: 10.3109/01676830.2010.513591. [DOI] [PubMed] [Google Scholar]
- Jassim N, Merghoub T, Pascaud O, al MH, Ducrocq R, Labie D, Elion J, Krishnamoorthy R, Arrayed SA. Molecular basis of beta-thalassemia in Bahrain: an epicenter for a Middle East specific mutation. Ann N Y Acad Sci. 1998;850:407–409. doi: 10.1111/j.1749-6632.1998.tb10505.x. [DOI] [PubMed] [Google Scholar]
- Jassim N, Al-Arrayed S, Gerard N, Al-Mukharraq H, Al-Ajami A, Ducrocoq R, et al. Molecular basis of á-thalassemia in Bahrain. Bahrain Med Bull. 2001;23(1):3–7. [Google Scholar]
- Jiffri EH, Bogari N, Zidan KH, Teama S, Elhawary NA. Molecular updating of beta-thalassemia mutations in the Upper Egyptian population. Hemoglobin. 2010;34:538–547. doi: 10.3109/03630269.2010.526440. [DOI] [PubMed] [Google Scholar]
- Kanavakis E, Papassotiriou I, Karagiorga M, Vrettou C, Metaxotou-Mavrommati A, Stamoulakatou A, Kattamis C, Traeger-Synodinos J. Phenotypic and molecular diversity of haemoglobin H disease: a Greek experience. Br J Haematol. 2000;111:915–923. doi: 10.1046/j.1365-2141.2000.02448.x. [DOI] [PubMed] [Google Scholar]
- Kattamis C, Hu H, Cheng G, Reese AL, Gonzalez-Redondo JM, Kutlar A, Kutlar F, Huisman TH. Molecular characterization of beta-thalassaemia in 174 Greek patients with thalassaemia major. Br J Haematol. 1990;74:342–346. doi: 10.1111/j.1365-2141.1990.tb02593.x. [DOI] [PubMed] [Google Scholar]
- Kulozik AE, Wainscoat JS, Serjeant GR, Kar BC, Al-Awamy B, Essan GJ, Falusi AG, Haque SK, Hilali AM, Kate S. Geographical survey of beta S-globin gene haplotypes: evidence for an independent Asian origin of the sickle-cell mutation. Am J Hum Genet. 1986;39:239–244. [PMC free article] [PubMed] [Google Scholar]
- Kyriacou K, Al-Quobaili F, Pavlou E, Christopoulos G, Ioannou P, Kleanthous M. Molecular characterization of beta-thalassemia in Syria. Hemoglobin. 2000;24:1–13. doi: 10.3109/03630260009002268. [DOI] [PubMed] [Google Scholar]
- Labie D, Bennani C, Beldjord C. Beta-thalassemia in Algeria. Ann N Y Acad Sci. 1990;612:43–54. doi: 10.1111/j.1749-6632.1990.tb24289.x. [DOI] [PubMed] [Google Scholar]
- Lal A, Vichinsky EP. Sickle cell disease. In: Hoffbrand AV, Catovsky D, Tuddenham EGD, Green AR, editors. Postgraduate haematology. 6. Chichester: Wiley-Blackwell; 2011. pp. 109–125. [Google Scholar]
- Laradi S, Haj KA, Omri H, Chaieb A, Mahjoub T, Benlimam H, Amri F, Saad A, Miled A, Leturcq F, Ben CJ, Beldjord C. Molecular analysis and prenatal diagnosis of beta-thalassemia: about our experience in central Tunisia. Ann Biol Clin (Paris) 2000;58:453–460. [PubMed] [Google Scholar]
- Lemsaddek W, Picanco I, Seuanes F, Nogueira P, Mahmal L, Benchekroun S, Khattab M, Osorio-Almeida L. The beta-thalassemia mutation/haplotype distribution in the Moroccan population. Hemoglobin. 2004;28:25–37. doi: 10.1081/HEM-120028884. [DOI] [PubMed] [Google Scholar]
- Makhoul NJ, Wells RS, Kaspar H, Shbaklo H, Taher A, Chakar N, Zalloua PA. Genetic heterogeneity of Beta thalassemia in Lebanon reflects historic and recent population migration. Ann Hum Genet. 2005;69:55–66. doi: 10.1046/j.1529-8817.2004.00138.x. [DOI] [PubMed] [Google Scholar]
- Memish ZA, Saeedi MY. Six-year outcome of the national premarital screening and genetic counseling program for sickle cell disease and beta-thalassemia in Saudi Arabia. Ann Saudi Med. 2011;31:229–235. doi: 10.4103/0256-4947.81527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesbah-Amroun H, Rouabhi F, Ducrocq R, Elion J. Molecular basis of alpha-thalassemia in Algeria. Hemoglobin. 2008;32:273–278. doi: 10.1080/03630260802004301. [DOI] [PubMed] [Google Scholar]
- Mohammed AM, Al-Hilli F, Nadkarni KV, Bhagwat GP, Bapat JP. Hemoglobinopathies and glucose-6-phosphate dehydrogenase deficiency in hospital births in Bahrain. Ann Saudi Med. 1992;12:536–539. doi: 10.5144/0256-4947.1992.536. [DOI] [PubMed] [Google Scholar]
- Mseddi S, Gargouri J, Labiadh Z, Kassis M, Elloumi M, Ghali L, Dammak J, Harrabi M, Souissi T, Frikha M. Prevalence of hemoglobin abnormalities in Kebili (Tunisian South) Rev Epidemiol Sante Publique. 1999;47:29–36. [PubMed] [Google Scholar]
- Nafei A. Prevalence of hemogolobinopathies and study of their genetics. Tanta Med J. 1992;20(1):467–480. [Google Scholar]
- Najmabadi H, Karimi-Nejad R, Sahebjam S, Pourfarzad F, Teimourian S, Sahebjam F, Amirizadeh N, Karimi-Nejad MH. The beta-thalassemia mutation spectrum in the Iranian population. Hemoglobin. 2001;25:285–296. doi: 10.1081/HEM-100105221. [DOI] [PubMed] [Google Scholar]
- Nasserullah Z, Al-Jame A, AbuSrair H, Al-Qatari G, Al-Naim S, Al-Aqib A, Mokhtar M. Neonatal screening for sickle cell disease, glucose-6-phosphate dehydrogenase deficiency and a-thalassemia in Qatif and Al Hasa. Ann Saudi Med. 1998;18:289–292. doi: 10.5144/0256-4947.1998.289. [DOI] [PubMed] [Google Scholar]
- Nasserullah Z, Alshammari A, Abbas MA, Abu-Khamseen Y, Qadri M, Jafer SA, Wabel MA. Regional experience with newborn screening for sickle cell disease, other hemoglobinopathies and G6PD deficiency. Ann Saudi Med. 2003;23:354–357. doi: 10.5144/0256-4947.2003.354. [DOI] [PubMed] [Google Scholar]
- Ogedegbe HO. β-globin gene cluster haplotype analysis as a predictor of sickle cell disease severity. Labmedicine. 2007;38(9):563–568. [Google Scholar]
- Orkin SH, Goff SC, Hechtman RL. Mutation in an intervening sequence splice junction in man. Proc Natl Acad Sci U S A. 1981;78:5041–5045. doi: 10.1073/pnas.78.8.5041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oron-Karni V, Filon D, Shifrin Y, Fried E, Pogrebijsky G, Oppenheim A, Rund D. Diversity of alpha-globin mutations and clinical presentation of alpha-thalassemia in Israel. Am J Hematol. 2000;65:196–203. doi: 10.1002/1096-8652(200011)65:3<196::AID-AJH4>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- Pagnier J, Mears JG, Dunda-Belkhodja O, Schaefer-Rego KE, Beldjord C, Nagel RL, Labie D. Evidence for the multicentric origin of the sickle cell hemoglobin gene in Africa. Proc Natl Acad Sci U S A. 1984;81:1771–1773. doi: 10.1073/pnas.81.6.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin P, Bouhassa R, Mselli L, Garguier N, Nigon VM, Bennani C, Labie D, Trabuchet G. Diversity of sequence haplotypes associated with beta-thalassaemia mutations in Algeria: implications for their origin. Gene. 1998;213:169–177. doi: 10.1016/S0378-1119(98)00200-5. [DOI] [PubMed] [Google Scholar]
- Pirastu M, Galanello R, Doherty MA, Tuveri T, Cao A, Kan YW. The same beta-globin gene mutation is present on nine different beta-thalassemia chromosomes in a Sardinian population. Proc Natl Acad Sci U S A. 1987;84:2882–2885. doi: 10.1073/pnas.84.9.2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PubMed (2012) http://www.ncbi.nlm.nih.gov/PubMed
- Quadri MI, Islam SI, Nasserullah Z. The effect of alpha-thalassemia on cord blood red cell indices and interaction with sickle cell gene. Ann Saudi Med. 2000;20:367–370. doi: 10.5144/0256-4947.2000.367. [DOI] [PubMed] [Google Scholar]
- Rahgozar S, Poorfathollah AA, Moafi AR, Old JM. Beta S gene in Central Iran is in linkage disequilibrium with the Indian-Arab haplotype. Am J Hematol. 2000;65:192–195. doi: 10.1002/1096-8652(200011)65:3<192::AID-AJH3>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Rahimi Z, Karimi M, Haghshenass M, Merat A. Beta-globin gene cluster haplotypes in sickle cell patients from southwest Iran. Am J Hematol. 2003;74:156–160. doi: 10.1002/ajh.10422. [DOI] [PubMed] [Google Scholar]
- Rajab A and Jaffar MA (2008) Genetic diseases in the Sultanate of Oman: public health perspective. Genetic disorders in Arab populations: a 2008 update. In: Tadmouri GO, Taleb Al-Ali M, Al-Khaja N (eds) Genetic disorders in the Arab World: Oman. Centre for Arab Genomic Studies, Dubai
- Rajab AG, Patton MA, Modell B. Study of hemoglobinopathies in Oman through a national register. Saudi Med J. 2000;21:1168–1172. [PubMed] [Google Scholar]
- Rajab KE, Issa AA, Mohammed AM, Ajami AA. Sickle cell disease and pregnancy in Bahrain. Int J Gynaecol Obstet. 2006;93:171–175. doi: 10.1016/j.ijgo.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Rizk S, Zayed S, Aziz M. Identification of five common Alpha-thalassaemia genotypes among a group of Egyptian neonates by single tube PCR. Med J Cairo Univ. 2005;73(3):483–488. [Google Scholar]
- Rosatelli MC, Tuveri T, Scalas MT, Leoni GB, Sardu R, Faa V, Meloni A, Pischedda MA, Demurtas M, Monni G. Molecular screening and fetal diagnosis of beta-thalassemia in the Italian population. Hum Genet. 1992;89:585–589. doi: 10.1007/BF00221942. [DOI] [PubMed] [Google Scholar]
- Rouabhi F, Lapoumeroulie C, Amselem S, Krishnamoorthy R, Adjrad L, Girot R, Chardin P, Benabdji M, Labie D, Beldjord C. DNA haplotype distribution in Algerian beta thalassaemia patients. An extended evaluation by family studies and representative molecular characterization. Hum Genet. 1988;79:373–376. doi: 10.1007/BF00282180. [DOI] [PubMed] [Google Scholar]
- Sadiq MF, Eigel A, Horst J. Spectrum of beta-thalassemia in Jordan: identification of two novel mutations. Am J Hematol. 2001;68:16–22. doi: 10.1002/ajh.1143. [DOI] [PubMed] [Google Scholar]
- Samarah F, Ayesh S, Athanasiou M, Christakis J, Vavatsi N. Beta(S)-globin gene cluster haplotypes in the West Bank of Palestine. Hemoglobin. 2009;33:143–149. doi: 10.1080/03630260902861873. [DOI] [PubMed] [Google Scholar]
- Samavat A, Modell B. Iranian national thalassaemia screening programme. BMJ. 2004;329:1134–1137. doi: 10.1136/bmj.329.7475.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serjeant GR. Geography and the clinical picture of sickle cell disease. An overview. Ann N Y Acad Sci. 1989;565:109–119. doi: 10.1111/j.1749-6632.1989.tb24157.x. [DOI] [PubMed] [Google Scholar]
- Siala H, Ouali F, Messaoud T, Bibi A, Fattoum S. alpha-Thalassaemia in Tunisia: some epidemiological and molecular data. J Genet. 2008;87:229–234. doi: 10.1007/s12041-008-0036-0. [DOI] [PubMed] [Google Scholar]
- Simsek M, Nassar K, Baner A. Incidence and genotype distribution of alpha-thalassemias in Kuwait. Med Princ Pract. 1993;3(4):181–184. [Google Scholar]
- Sirdah M, Bilto YY, El-Jabour S, Najjar K. Screening secondary school students in the Gaza strip for beta-thalassaemia trait. Clin Lab Haematol. 1998;20:279–283. doi: 10.1046/j.1365-2257.1998.00037.x. [DOI] [PubMed] [Google Scholar]
- Sunna EI, Gharaibeh NS, Knapp DD, Bashir NA. Prevalence of hemoglobin S and beta-thalassemia in northern Jordan. J Obstet Gynaecol Res. 1996;22:17–20. doi: 10.1111/j.1447-0756.1996.tb00929.x. [DOI] [PubMed] [Google Scholar]
- Tadmouri GO, Gulen RI. Deniz: the electronic database for beta-thalassemia mutations in the Arab world. Saudi Med J. 2003;24:1192–1198. [PubMed] [Google Scholar]
- Tadmouri GO, Garguier N, Demont J, Perrin P, Basak AN. History and origin of beta-thalassemia in Turkey: sequence haplotype diversity of beta-globin genes. Hum Biol. 2001;73:661–674. doi: 10.1353/hub.2001.0075. [DOI] [PubMed] [Google Scholar]
- Talafih K, Hunaiti AA, Gharaibeh N, Gharaibeh M, Jaradat S. The prevalence of hemoglobin S and glucose-6-phosphate dehydrogenase deficiency in Jordanian newborn. J Obstet Gynaecol Res. 1996;22:417–420. doi: 10.1111/j.1447-0756.1996.tb01050.x. [DOI] [PubMed] [Google Scholar]
- Tarazi I, Al-Najjar E, Lulu N, Sirdah M. Obligatory premarital tests for beta-thalassaemia in the Gaza Strip: evaluation and recommendations. Int J Lab Hematol. 2007;29:111–118. doi: 10.1111/j.1751-553X.2006.00836.x. [DOI] [PubMed] [Google Scholar]
- Teebi A, Farag T. Teebi A (2010) Genetic disorders among Arab populations. 2. New York: Springer; 1997. [Google Scholar]
- Teebi A, Farag T. Genetic disorders among Arab populations. Oxford monographs on medical genetics No. 30. New York: Oxford University Press; 1997. [Google Scholar]
- Teebi AS, Teebi SA. Genetic diversity among the Arabs. Community Genet. 2005;8:21–26. doi: 10.1159/000083333. [DOI] [PubMed] [Google Scholar]
- Tremblay C, Hamilton B, Sala M, Paoloni J, Chalabi H. Prevalence of haemoglobinopathy in sportsmen in Qatar. Br J Sports Med. 2011;45:317. doi: 10.1136/bjsm.2011.084038.21. [DOI] [Google Scholar]
- UNDP (2012) Arab Human Development Reports (AHDR)—United Nations Development Programme. Available from http://www.arab-hdr.org/undpcos.aspx
- Weatherall DJ, Clegg JB. Thalassemia syndromes. 4. Oxford: Blackwell; 2001. [Google Scholar]
- White JM, Byrne M, Richards R, Buchanan T, Katsoulis E, Weerasingh K. Red cell genetic abnormalities in Peninsular Arabs: sickle haemoglobin, G6PD deficiency, and alpha and beta thalassaemia. J Med Genet. 1986;23:245–251. doi: 10.1136/jmg.23.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White JM, Christie BS, Nam D, Daar S, Higgs DR. Frequency and clinical significance of erythrocyte genetic abnormalities in Omanis. J Med Genet. 1993;30:396–400. doi: 10.1136/jmg.30.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medical genetic services in developing countries: the ethical, legal and social implications of genetic testing and screening. Geneva: WHO; 2006. [Google Scholar]
- WHO (2012) http://www.emro.who.int/HIS/VHSL/
- World Bank (2012) http://data.worldbank.org/indicator/NY.GNP.PCAP.CD
- World Health Organization (2010) http://rho.emro.who.int/rhodata/InstantAtlasMaps/AllIndicators/atlas.html
- Yahya H, Khalel K, Al-Allawi N, Helmi F. Thalassaemia genes in Baghdad, Iraq. East Mediterr Health J. 1996;2:315–319. [Google Scholar]
- Yavarian M, Karimi M, Zorai A, Harteveld CL, Giordano PC. Molecular basis of Hb H disease in southwest Iran. Hemoglobin. 2005;29:43–50. [PubMed] [Google Scholar]
- Zahed L, Bou-Dames J. Acceptance of first-trimester prenatal diagnosis for the haemoglobinopathies in Lebanon. Prenat Diagn. 1997;17:423–428. doi: 10.1002/(SICI)1097-0223(199705)17:5<423::AID-PD68>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Zahed L, Demont J, Bouhass R, Trabuchet G, Hanni C, Zalloua P, Perrin P. Origin and history of the IVS-I-110 and codon 39 beta-thalassemia mutations in the Lebanese population. Hum Biol. 2002;74:837–847. doi: 10.1353/hub.2003.0013. [DOI] [PubMed] [Google Scholar]
- Zorai A, Harteveld CL, Bakir A, Van DP, Falfoul A, Dellagi K, Abbes S, Giordano PC. Molecular spectrum of alpha-thalassemia in Tunisia: epidemiology and detection at birth. Hemoglobin. 2002;26:353–362. doi: 10.1081/HEM-120016372. [DOI] [PubMed] [Google Scholar]