Delirium or acute confusional state is characterized by an acute disruption of cognition and attention (American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders (4th ed.), text revision, 2000). Delirium is the leading complication of hospitalization for older adults (Milisen et al., 2001; Young & Inouye, 2007), with the prevalence ranging from 11% and 42% in acute care settings (Siddiqi, Horne, House, & Holmes, 2006). The development of delirium is associated with important negative consequences including increased morbidity and mortality, protracted hospital stay, increased use of health care resources and, greater burden for caregivers (Cole, 2004; Inouye, Rushing, Foreman, Palmeiri, & Pompei, 1998; McCusker, Cole, Dendukuri, & Belzile, 2003; O’Keeffe & Lavan, 1999). Evidence also suggests that symptoms persist in about a third of patients (Siddiqi et al., 2006), and that these patients have a poor prognosis (McAvay et al., 2006).
Older adults with chronic conditions, physiological impairments, decreased reserve, and numerous medications represent a group especially vulnerable to the adverse effects of hospitalization, including delirium. Because hospitalization of older adults is common, accounting for greater than 49% of all days of hospital care, the potential for the occurrence of delirium in this setting is high (The Administration on Aging, 2004). Primary prevention of this complication is therefore of paramount importance to patients, families, and health care institutions because of the physical, emotional, and financial burdens of caring for the older adult who is suffering from delirium.
The etiology of delirium is believed to be intrinsically multifactorial in older persons with a number of factors contributing to increased risk. Therefore, for an intervention strategy to be effective, it should target the multifactorial origins of delirium with multicomponent interventions that address more than one risk factor (Inouye et al., 1999; Inouye, 2006). Previous studies have documented that delirium is preventable in 40% of cases (Inouye, 2006). Several studies have demonstrated that multicomponent interventions, when implemented by an interdisciplinary team of health care providers, comprise the most effective strategy for delirium prevention for medical patients in the hospital setting (Flaherty et al., 2003; Inouye et al., 1999; Lundstrom, Edlund, Lundstrom, & Gustavson, 1999; Rapp, 2001, Weber, Coverdale, & Kunik, 2004), most notably the Hospital Elder Life Program (HELP) (Inouye, Bogardus, Baker, Leo- Summers, & Cooney, 2000). The HELP program consists of a trained interdisciplinary staff who implement intervention protocols targeted toward six previously identified risk factors for delirium (Inouye et al., 1999). The unique strengths of the HELP model include the targeted nature of the interventions, early intervention focusing on prevention, well-trained interdisciplinary staff dedicated to the program, standardized intervention protocols, tracking of adherence to all protocols, and built-in quality assurance procedures (Inouye et al., 2000). HELP has been demonstrated to be effective with a 40% risk reduction in delirium rates in a study of 852 patients (Inouye et al.,1999), and a 67% risk reduction in rates of functional decline in a study of 1507 patients (Inouye et al., 2000). Cost-effectiveness has been demonstrated for acute hospital costs in a study of 852 patients (Rizzo et al., 2001), with cost savings of $831 per patient which offset intervention costs in intermediate risk patients. For long-term nursing home costs, the HELP intervention resulted in cost savings of $9446 per long-term nursing home patient in a longitudinal study of 801 patients, where patients were followed for one year after discharge (Leslie et al., 2005). In addition, significant cost savings have been demonstrated at dissemination sites in the U.S. of over $1.2 million annually (Rubin et al., 2006)) and in Australia (Caplan & Harper, 2007). The HELP program has been disseminated to over 60 hospitals in the U.S. and internationally.
The intervention strategy for this study called the Family HELP Program (Fam-HELP) is an adaptation and extension of the HELP program (HELP, © 1999 Sharon K. Inouye, MD, MPH). The four protocols of the Fam-HELP program were selected from those considered to be most amenable to family implementation (see Table 1). This work is important because it builds on the HELP program’s existing, extensive body of work and extends its benefits by training family caregivers with an important role in delirium prevention efforts in the acute care setting. The potential role that family caregivers could play in delirium prevention in the older adult population and how nurses could facilitate this process has been unexplored. Family caregivers are an untapped resource who can collaborate with nurses in delirium prevention efforts for older hospitalized adults. Previous studies on family interventions for delirium have focused on older adult patients who have already become delirious (Chatham, 1978; Gagnon et al., 2002) and not on preventive interventions. In these previous published studies, family interventions for the delirious patient have involved an integrated approach to management which involves educating family members about the nature of the delirium syndrome, its potential treatment, and increasing family caregivers’ self confidence in decision making related to the delirious older adult. Previous studies focused on the effect of family interventions on the family caregiver and did not consider the effect of the interventions on delirium prevention for the patient.
Table 1.
Targeted Risk Factors and Intervention Protocols of the HELP Program and Rationale for Inclusion in the Family-HELP Program
| Targeted Risk Factor and Eligible Patients |
HELP Standardized Intervention Protocols |
Rationale for Inclusion in Family-HELP program |
|---|---|---|
| Cognitive impairment Patients with baseline Mini Mental State Examination score (MMSE) < 20 | Orientation protocol | Providing memory cues such as a clock or family photos helps orient patients to their surroundings and are readily accessible for family caregivers from the home |
| Therapeutic-activities protocol | Cognitively stimulating activities such as discussing current events and reminiscing are often part of the typical daily interaction between older adults and their family caregivers (Bogardus et al., 2003) | |
| Sleep deprivation All patients | Nonpharmacologic sleep protocol | |
| Immobility Patients with a Katz ADL score < 10 | Early mobilization protocol | |
| Visual impairment Patients with visual acuity worse than 20/70 on binocular near vision testing | Vision protocol | Family caregivers are often used to ensuring that the older adult has access to and wears glasses and uses other visual aids (Cole, 2004) |
| Hearing impairment Patients hearing </=6/12 whispers on Whisper Test | Hearing protocol | Hearing deficits are often a major focus of family caregivers as deficits impact their ability to communicate with the older adult (Mulrow et al., 1990) |
| Dehydration Patients with ratio of blood urea nitrogen to creatinine>/= 18 | Dehydration protocol | |
Note. HELP protocols selected for the Family-HELP Program are shown in boldface. Adapted from “A Multicomponent Intervention To Prevent Delirium in Hospitalized Older Patients,” by S. K. Inouye, S. T. Bogardus Jr., C. S. Williams, L. Leo-Summers, D. Acampora, T. R. Holford, T. R., et al., 1999, New England Journal of Medicine, 340, p. 676. Adapted with permission of the author. Copyright 1999 by the Hospital Elder Life Program.
The purpose of this study was to examine the feasibility of a nurse-supported, multicomponent family intervention program for delirium prevention in the older hospitalized adult derived from the widely implemented Hospital Elder Life Program. It is important to stress that the family interventions are intended to complement the HELP program, not supplant the HELP program. Thus, these interventions should ideally be implemented as part of a HELP program to allow extension of the benefits through application of the interventions by family caregivers. To evaluate the feasibility of family interventions, we utilized the Calgary Family Intervention Model (CFIM) (Wright & Leahey, 1984, 2000) as a conceptual framework. The CFIM, which is a family nursing intervention model, is one way that health care professionals can conceptualize family support and better understand how nurses can support family caregivers’ participation. The CFIM has been used to test interventions that involve the patient and family to improve outcomes of care (Addington, Collins, McCleery, & Addington, 2005; Martin-Arafeh, Watson, & Baird, 1999; Riley-Doucet, 2005; Simpson, Yeung, Kwan, Wah, 2006) and supports a multicomponent approach to delirium prevention. According to the model, it is not one, but several factors that enhance the likelihood that interventions will be more effective and useful to patients and families. The assumption of the CFIM is that the nurse and the family, in interaction, can affect the patient’s health. The CFIM guides intervention implementation by suggesting that family interventions should be related to the problems that the nurse, patient, and family have collaborated on and thus provides the theoretical basis for a collaborative effort between the nurse and the family in a multi-component intervention program to prevent delirium in the older hospitalized adult.
A descriptive exploratory design was used to gain information about family participation in the Fam-HELP program, the multicomponent intervention for delirium prevention. The study population included family caregivers, defined as a spouse, blood relative or significant other, of hospitalized adults, age 65 or older. A nonprobability sampling strategy was employed to obtain a convenience sample of family caregivers of hospitalized patients, age 65 or greater, on an inpatient acute medical unit at the Massachusetts General Hospital, a 900-bed academic medical center with 47,000 acute inpatient admissions per year, serving a large regional and referral population.
Our goal was to have at least ten family caregivers participate in the Fam-HELP program, track completion of assigned interventions, and complete a questionnaire upon discharge of the older adult. The inclusion criteria were designed to be as inclusive as possible and to assure that patients, by having at least one targeted risk factor for delirium, would benefit from the program. Potentially eligible older patients were admitted to the designated study unit, were age 65 or older, had no delirium at the time of admission, had at least one of the four targeted risk factors for delirium at baseline screening (cognitive impairment, ADL impairment, vision impairment, hearing impairment); and were able to read, write, and communicate in English. Older patients were excluded for an inability to give informed consent as determined by the Evaluation to Sign Consent Measure (DeRenzo, Conley, & Love, 1998), inability to communicate verbally (e.g., coma, mechanical ventilation, severe aphasia, profound dementia; severe/profound hearing loss), combative behavior or severe psychotic disorder, airborne precautions (e.g., tuberculosis, measles), anticipated discharge within 48 hours, or refusal by the patient, family caregiver, or physician.
Potentially eligible family caregivers were a spouse, blood relative, or significant other of eligible older adults, who was able to read, write, and communicate in English, and able to visit daily for intervention protocol completion. Family caregivers were excluded for refusal to participate.
Subject Enrollment
All patients age 65 or older were invited to participate within twenty-four hours of admission to the study unit. Dual consent was obtained verbally and in writing from both the older adult patient and the family caregiver. To evaluate the capacity of the older adult inpatient to consent to participate, the Evaluation to Sign Consent (ESC) Measure was used (DeRenzo, Conley, & Love, 1998). If the older adult did not meet the ESC criteria for capacity to give consent, the patient was excluded (see Exclusion criteria). The consent process included a verbal review by the principal investigator of all elements of the IRB-approved written consent form. Once consent was obtained, the subject was screened for at least one of the targeted risk factors (cognitive impairment, ADL impairment, vision impairment, hearing impairment), and for the presence of delirium using standardized assessment tools for measurement. The patient was asked to identify the significant family caregiver with whom they have the closest relationship. The identified family caregiver was contacted by the principal investigator to offer participation and obtain informed consent. The screening and enrollment process was completed within 48 hours of admission. This study received institutional review board approval from the participating hospital facility.
Intervention Program
The Family-HELP Program (Fam-HELP) was adapted with permission from the Hospital Elder Life Program (HELP ©, 1999) volunteer protocols for family implementation. Fam-HELP was implemented by the family caregiver who was trained in the protocols by a member of the research team. Four risk factors for delirium (i.e., cognitive impairment, impairment of activities of daily living (ADL), vision impairment, and hearing impairment) were targeted for intervention by the five protocols of the Fam-HELP. These interventions were selected for their appropriateness and safety for family implementation in the hospital since the protocols involve activities commonly performed by caregivers for older adults at home.
Study Procedures
Upon enrollment in the study, the family caregiver was given detailed instruction in the five intervention protocols of the Fam-HELP by a member of the research team. Family caregivers were instructed on the use of a standardized Family Caregiver Tracking Form to record daily frequency of intervention completion and reasons for non-completion. The value of recording both the completion of the intervention or its non-completion, plus reasons for non-completion when appropriate, was emphasized as an integral component for evaluation of the feasibility of the family caregiver delirium prevention program. Within twenty-four hours of anticipated discharge, the older adult and family caregiver were asked to complete a written questionnaire to examine the barriers and facilitators to participation in the Fam-HELP. To examine nurses’ experience with the program, an anonymous, written questionnaire was made available daily for all 64 floor nurses for 14 days midway through data collection and again for 14 days after subject enrollment was closed.
The above methods contributed different and important aspects to understanding of the feasibility of the Fam-HELP. Self-tracking of completion of assigned intervention protocols with reasons for non-completion, provided descriptive data on the ability of family caregivers to complete recommended interventions for the targeted risk factors. The family and older adult subject questionnaires were developed to identify barriers and facilitators for participation in the Fam-HELP, including those related to the staff nurse. The staff nurse questionnaire contributed important information from the nursing perspective on their potential role in supporting family caregiver participation.
Measurement
Study variables examined included patient and family caregiver demographics; risk factors for delirium (cognitive impairment, ADL impairment, visual impairment, hearing impairment); and intervention completion. The feasibility of family implementation of a multicomponent intervention protocol was based on: 1) dual sources of evidence from family caregivers that included self-tracking of intervention completion and data gathered from family caregivers’ questionnaire responses on the barriers and facilitators for their participation in the Fam-HELP; 2) data gathered from older adult patients’ questionnaire responses on the barriers and facilitators for their participation in the Fam-HELP; and, 3) data gathered from the responses of staff nurses on an anonymous, written questionnaire on the nurses’ experience with the Fam-HELP. All written questionnaires included both Likert-type rating scales and open-ended questions.
All assessments were completed by members of the research team who had no role in the Fam- HELP intervention and who were blinded to the nature of the study. Demographic data was collected from older adult and family caregiver participants to describe their baseline characteristics. In addition, assessments were completed at admission for risk factors for delirium to select the appropriate intervention protocols, including the Mini-Mental® State Examination (MMSE®) (Copyright ©, PAR, 2001, used with permission) (Folstein, Folstein, & McHugh, 1975 for cognitive impairment; the Katz Index of Independence in Activities of Daily Living (ADL) (Katz, Ford, & Maskowitz, 1963) for ADL impairment; the standard bedside Jaeger test for vision impairment; the Whisper test for hearing impairment (MacPhee, Crowther, & McAlpine, 1988); evaluation by the Confusion Assessment Method (CAM) to exclude delirious patients at baseline (Inouye, van Dyck, Alessi, Balkin, Siegal, & Horwitz, 1990); and a brief medical record review for the older adult’s medical history. The MMSE® measures cognitive functioning on a scale of 0 (poor) to 30 (excellent), with a score of less than 24 indicating cognitive impairment. The Katz Index of ADL score ranks adequacy of performance in seven daily functions (feeding, dressing, grooming, walking, transferring, bathing, and toileting) on a scale of 0 to 14. An overall score of 10 to 14 is considered to indicate independent function; 5 to 9 indicates moderate impairment; and 4 or less indicates severe functional impairment. The standard bedside Jaeger test measures binocular near vision with scores worse than 20/70 after correction indicating vision impairment. The Whisper Test measures hearing according to the number of 12 whispers heard, with 6 or fewer indicating hearing impairment. Accepted cutpoints were used for assignment to the intervention protocols (Inouye et al., 2000).
Completion of interventions was based on family caregiver tracking as done/not done on the Family Caregiver Tracking Form. Daily intervention completion was defined as the actual number of intervention protocols completed/total number of protocols assigned. Overall rates of completion for each intervention protocol were measured as number of times completed/number of times assigned. Intervention completion was recorded as “complete” if the family caregiver completed all parts of the assigned protocol for the total number of times it was to be given. “Incomplete” indicated that the family caregiver completed some but not all parts of the protocol for the required number of times or did not deliver any of the parts of the protocol. These rates were summed across all patients and presented as aggregates. Highest and lowest completion rates for each intervention protocol were also presented.
Data Analysis
Analysis included statistical summaries of quantitative data and content analysis of qualitative data. Demographic data and quantitative data related to intervention completion were analyzed using descriptive statistics. Content analysis was used to analyze the family caregivers’, older adults’, and nurses’ responses to open-ended questions. The questionnaires for family caregivers, older adults, and staff nurses each involved separate content analysis procedures to develop a robust understanding of the differences and similarities among the three groups.
The content analysis procedure was based on Mayring's (2000) inductive category development and Field and Morse's (1985) thematic analysis. Inductive category development involved formulating categories that were related closely to the data, without imposing a prior theoretical framework (Mayring, 2000). This required grouping similar responses into categories. Thematic analysis involved developing a coding scheme based on categories. Codes with similar meanings were grouped together as categories and a term, often from the literature, was used to describe them, for example ‘support’. Categories were then drawn together into dominant themes that ran throughout the entire set of questionnaires (Field and Morse, 1985), for example “support’ and ‘shared goals’ were grouped together under the theme ‘partnership’. Once dominant themes were captured for each set of questionnaires, further analysis included assessment for common overarching themes among those generated from family caregivers’, older adults’, and the staff nurses’ responses.
The content analysis involved several steps completed independently for the family caregiver, older adult, and staff nurse questionnaires. In the first step, initial identification of themes was recorded immediately after reviewing a questionnaire. The research team members read all of the questionnaire responses to become familiar with the data and develop ideas about emerging themes. Next, themes were tentatively grouped into categories, which were labeled using the subject’s own language (Mayring, 2000). In the third step, clear coding rules and operational definitions were developed by making decisions about inclusion and exclusion criteria for responses that reflected family caregivers’, older adults’ or staff nurses’ experiences of participating in the Fam-HELP. Intercoder reliability was cross-checked twice, where two members of the research team coded the same questionnaire. Reliability was calculated as number of agreements/total number of agreements + disagreements, and agreement was required to exceed 80% by the second check. Finally, interpretation of the results included counting frequencies to make inferences about the relative significance of categories to the participants. As the data were analyzed, the research team mapped out the elements that might facilitate implementation of the family protocols and those that might inhibit implementation.
Trustworthiness of the study was established through well-established procedures, including review of emerging codes with the research team (credibility); rich description of the data (transferability); and a careful audit trail (dependability and confirmability) (Lincoln & Guba, 1985).
Results
Characteristics of the Sample
Patients
Forty-two older adult patients were approached to participate and of these, fifteen (36%) met the screening criteria and consented to participate. Older adult subject demographics are shown in Table 2. The majority of participants had more than one targeted risk factor for delirium present at baseline screening. Eighty-five percent of older adult patients had at least two of the four targeted risk factors and 69% had three or four risk factors. Of the fifteen study patients, none developed delirium during participation from baseline to discharge.
Table 2.
Demographic and Risk Factor Characteristics of Older Adult Patient Participants
| Characteristic | mean (range; median) (N=15) |
|---|---|
| SOCIODEMOGRAPHIC | |
| Age | 77.8, (68–85; 79) |
| Female, n, (%) | 10, (66.7) |
| Race, n, (%) | |
| Asian | 1, (6.7) |
| Black | 3, (20) |
| White | 11, (73.3) |
| Ethnicity, n, (%) | |
| Non-Hispanic | 12, (80) |
| Living Situation, n, (%) | |
| Does not live alone | 14, (93.3) |
| Independence n, (%) | |
| Lives independently a | 10, (66.7) |
| Living Children, mean | 3 |
| Admitting Diagnosis, n, (%) | |
| Angina, chest pain | 1, (6.7) |
| Congestive heart failure | 4, (26.7) |
| Dehydration | 1, (6.7) |
| Hypoglycemia | 1, (6.7) |
| Pneumonia | 4, (26.7) |
| Renal failure | 4, (26.7) |
| RISK FACTORS | |
| Cognitive impairment | 15, (100) |
| ADL impairment | 14, (93.3) |
| Vision impairment, n, (%) | 10, (66.7) |
| Hearing impairment, n, (%) | 10, (66.7) |
Lives independently denotes no help required for activities of daily living including eating, dressing, walking, grooming, bathing, toileting
Family caregivers
Fifteen family caregivers of enrolled older hospitalized adults consented to participate in the Fam-HELP program. Family caregiver demographics are shown in Table 3. The mean age of the sample of 15 family caregivers was 61.2 years with a broad range of age 30 to 82 years depending on the relationship of the caregiver to the older adult patient. The most frequent relationship of the family caregiver to the older adult patient was as an adult child (n=6, 40%), followed by other blood relative (n=4, 26.7%), spouse (n=3, 20%), and significant other (n=2, 13.3%).
Table 3.
Demographic Characteristics of Family Caregiver Participants
| Characteristic | mean (range; median) (N=15) |
|---|---|
| SOCIODEMOGRAPHIC | |
| Age | 61.2, (30–82; 65) |
| Female, n, (%) | 11, (73.3) |
| Race, n, (%) | |
| Asian | 0, (0) |
| Black | 3, (20) |
| White | 12, (80) |
| Ethnicity, n, (%) | |
| Non-Hispanic | 11, (73.3) |
| Education, n, (%) | |
| Less than high school | 3, (20) |
| High school or equivalent | 9, (60) |
| Some college | 2, (13.3) |
| College graduate or above | 1, (6.7) |
| Relationship to patient, n, (%) | |
| Spouse | 3, (20) |
| Significant other | 2, (13.3) |
| Adult child | 6, (40) |
| Other blood relativea | 4, (26.7) |
Other blood relatives included 2 nieces, 1 cousin, and 1 granddaughter
Intervention Protocols of the Fam-HELP Completed By Family Caregivers
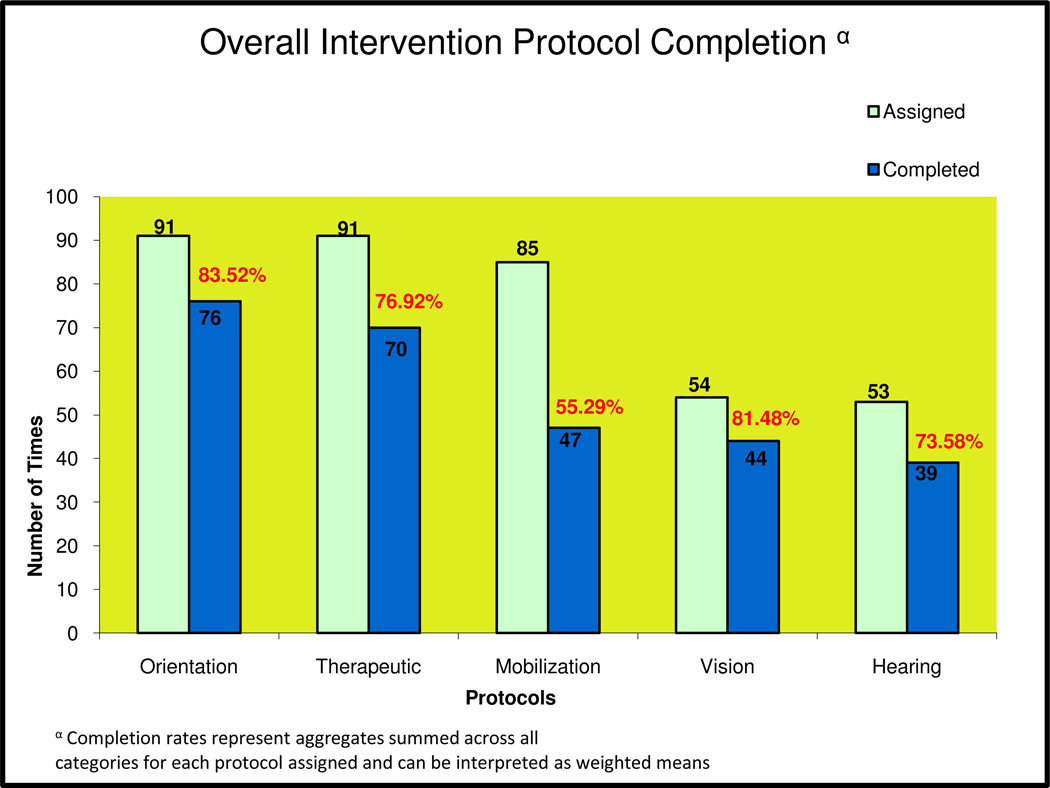
Overall intervention completion based on family caregiver tracking as done/not done on the Family Caregiver Tracking Form was highest for the orientation protocol (83.5%), followed closely by the vision protocol (81.5%), therapeutic activities protocol (76.9%) and hearing protocol (73.6%). The lowest overall completion rate was for the early mobilization protocol (55.3%). The completion rates represent aggregates summed across all categories for each protocol assigned and can be interpreted as a weighted mean value. Intervention completion is compared among the five protocols in relation to the number of times the protocol was assigned in Figure 1. The orientation and therapeutic activities protocols were assigned most frequently (91 times each) since cognitive impairment was a baseline risk factor in all 15 enrolled older adult participants. The early mobilization protocol was also assigned with a high frequency (85 times) as ADL impairment was a baseline risk factor for 90% of older adults. Vision impairment and hearing impairment, which were each a baseline risk factor for 60% of older adult participants, were assigned less frequently (54 and 53 times respectively). Based on the tracking of intervention completion by the ten family caregivers, the highest and lowest completion rates for each of the five protocols are noted in Figure 1 and represent the full range of completion rates for each protocol. The range of values for the early mobilization protocols was wide and the lowest completion rate (41%) and highest completion rate (90.3%) were lower than those for any of the four other protocols. The orientation protocol had the narrowest range between highest (100%) and lowest completion (76.3%) rates.
Figure 1.
Overall intervention completion rates in relation to times assigned
Note: Range of completion for protocols; Orientation (76.3–100%); Therapeutic Activities (63.8–98.1%); Mobilization (41.0–90.3%); Vision (74.1–96.4%); Hearing (69.2–94.4%)
On the Family Caregiver Questionnaire, 93% of family caregivers (n=13) indicated that both the orientation and therapeutic activities protocols were “not at all difficult” to perform and 86% (n=12) indicated the vision protocol was “not at all difficult” to complete. The majority (71.4%, n=10) rated the hearing protocol as “slightly difficult” to complete. Fifty seven percent indicated the early mobilization protocol was “moderately difficult” to perform. No scores of “to a great extent difficult” were given by any of the participants for any of the protocols.
Thirty-eight of the 64 staff nurses employed on the study unit completed an anonymous Staff Nurse Questionnaire with a response rate of 59.4%. Twenty-one questionnaires were completed during a two week period at the half way point of data collection. Seventeen additional questionnaires were completed during a two week period after data collection was closed. Staff nurses noted that collaborative efforts between the nurse and the family caregiver can positively affect participation in the Fam-HELP. For example, the nurse, through the systematic use of this intervention program, may determine that an older adult is delirious or has risk factors for delirium. Through open communication and effective collaboration with involved family, staff nurses believed the best outcome for the older adult could be achieved. Nurses noted that when they encountered challenges to engaging family caregivers in collaboration, family participation in the Fam-HELP was less effective. While the process of using the Fam-HELP protocols was deemed useful, the lack of time available to do so successfully was identified as a barrier. Staff nurses noted that the regulatory environment of acute inpatient care and financial constraints experienced in these settings has lead to tremendous amounts of documentation – and there often exists limited staff to complete this work.
The analysis of questionnaires given to family caregivers and older adults at the time of discharge, and to staff nurses at the midpoint and at completion of the study revealed three common overarching themes related to participation in the Fam-HELP: partnership, therapeutic relationships, and environment. These themes are exemplified by nurses working closely with the patient and family in a partnership, listening and being present to establish a therapeutic relationship, and providing a calm, unhurried environment, to support family caregivers’ participation in the Fam-HELP. Facilitators and barriers to participation in the FAM-HELP, specific examples, and recommendations for clinical practice are shown in Table 4 and Table 5.
Table 4.
The Three Overarching Themes Drawn From Family Caregivers’, Older Adult Patients’, and Nurses’ Responses (N=67) on Facilitators to Participation in the Fam-HELP
| Theme | Facilitator | Example | Recommendations for Practice | |
|---|---|---|---|---|
| Partnership (n=55, 82%) |
|
“Mom’s nurses and I had an open, evolving line of communication and I really felt they valued and respected my input into her care making me feel I was no longer alone in the burden of keeping her safe.” |
|
|
| (Family caregiver) | ||||
| Therapeutic Relationships (n=56, 84%) |
|
“The nurse took the time to speak with us, calmed my wife’s nerves about walking with me when I was ill. She shared with us how her own mom had recently been in the hospital, and even though she was a nurse, she too was afraid to help her engage in her usual activities because she was so sick. I felt like we were talking human to human, person to person, instead of being told what to do. Her reassurance and encouragement was based not only on her ‘book smarts’ but also her own life experience. My wife and I now felt we had an ally in the whole impersonal hospital environment.” |
|
|
| (Family caregiver) | ||||
| Environment (n=50, 75%) |
|
“When the unit was adequately staffed, I felt like I could maximize the patient and family caregiver’s potential for participation….I was more able to cluster nursing care thus minimizing interruptions and could allow them the space, quiet time and privacy they needed to complete the activities while still being accessible.” |
|
|
| (Staff nurse) | ||||
Table 5.
The Three Overarching Themes Drawn From Family Caregivers’, Older Adult Patients’, and Nurses’ Responses (N=67) on Barriers to Participation in the Fam-HELP
| Theme | Barrier | Example | Recommendations for Practice | |
|---|---|---|---|---|
| Partnership (n=55, 82%) |
|
“As the main caregiver for my mom, I wanted to be respected as a member of her plan of care. The nurses and doctors told me they would involve me in decisions, but never asked for my input. This is not how I viewed being part of a team.” |
|
|
| (Family caregiver) | ||||
| Therapeutic Relationships (n=56, 84%) |
|
“I’m sure this happens at other hospitals too….The nurses get distracted by other things they have to do. We would get interrupted for a time when the nurse was trying to answer our questions. It would have been nice if the nurse could have sat there when the request for support was made without any distractions or interruptions, but on the unit this was quite difficult.” |
|
|
| (Family caregiver) | ||||
| Environment (n=50, 75%) |
|
“My wife and I were trying to read the newspaper out loud together. The noise coming from outside in the hall drowned us both out. It was too loud and too cramped for me to even carry on a conversation more than a few seconds. I wish that there was more privacy and noise control….” |
|
|
| (Older adult patient) | ||||
Partnership involved the process of developing relationships- between the nurse and the older adult patient and their family caregiver- that would facilitate participation in the Fam-HELP. Family participation in Fam-HELP could be challenging and was facilitated by a sense of sharing in caregiving with nursing staff. When family caregiver and older adult participants experienced the nurse as having lack of respect, poor follow through, inflexibility, or difficult attitudes, the partnership was viewed as a challenge.
The theme of therapeutic relationships involved making connections - between the nurse and patient and between the nurse and family caregiver – and feeling supported. Patients and family caregivers noted that when the nurse offered both the caregiver and the patient time for teaching, for asking questions, and for establishing a partnership, a therapeutic relationship was forged. Conversely, a therapeutic relationship did not develop in the context of poor listening, distractions, and being unresponsive to expressed needs. In the absence of a therapeutic relationship, participation in the Fam-HELP was viewed as much more of a challenge by all three groups of participants.
A supportive physical environment empowered patients and families to participate in Fam-HELP, providing adequate space, privacy, and available staff to facilitate care. Conversely, cramped quarters, frequent interruptions, and staff shortages made it difficult for older adult patients, family caregivers, and the nurses caring for them to participate in the Fam-HELP.
Discussion
This study adds to the growing body of literature examining multicomponent interventions for delirium prevention, confirms other work done in this area (Flaherty et al., 2003; Inouye et al., 1999, 2000; Lundstrom et al., 1999; Rapp, 2001; Weber, Coverdale, & Kunik, 2004), and extends the work of the HELP program to include family caregivers in delirium prevention efforts in the acute care setting. The results of this study support the feasibility of family participation in a delirium prevention program in the acute care setting. The orientation, therapeutic activities, vision, and hearing protocols were each completed by family caregivers at least 75% of the time. The early mobilization protocol, which presented the biggest challenge for family caregivers to complete, was completed just over 50% of the time. Difficulty with participation in the early mobilization protocol was linked to fears about the older adult’s compromised physical state and symptoms of pain, shortness of breath, fatigue, and nausea. Staff nurses played an integral role in providing education about the importance of mobility and supporting successful completion. Continuing feedback from staff nurses was important to allow both patients and family caregivers to develop increased autonomy in completing the early mobilization activities.
Although the program does appear to be feasible, key to successful implementation in the future will be incorporation of facilitators and minimization of barriers for participation identified by participants (see recommendations in Tables 4 and 5). Facilitators included developing a therapeutic relationship with a sense of partnership between nursing staff, family caregivers, and older adult patients. The availability of nursing staff to provide educational reinforcement, emotional support, and opportunities for caregivers and patients to express their concerns was critical to developing a therapeutic relationship with the nurse. Staff nurse participants repeatedly identified the importance of in-depth knowledge of the older patients’ and family’s needs and communication skills that foster positive interactions.
The facilitators and barriers that emerged from this study were generally consistent with the concept of family-centered care described previously (Leahey, 1987; Wright & Leahey, 1987). Family-centered care empowers patients and their families, fostering their active participation in caregiving and decision making (Dunst & Trivette, 1996). Family-centered care studies have identified strategies that enhance nurse-family partnerships which include spending time with patients and families, showing empathy, respecting family opinions, supporting a non-hurried environment, and willingly explaining procedures and treatments (Boykoff, 2006; Hupcey, 2008). A systematic review of 31 family care studies found that when staff facilitate communication of family members’ needs by promoting expression of fears, concerns, and feelings, family members’ distress diminishes (Rutledge, Donaldson, & Pravikoff, 2000).
The major limitation of this small, pilot study was the lack of any measured outcomes. Although of the fifteen study patients, none developed delirium during participation, the effect of Fam-HELP on delirium prevention remains unclear, and is an important area for future investigation. Other limitations include the small, convenience sample with limited generalizability, since participants may not represent the full range of older patient and family caregiver experiences in acute care. In addition, only written questionnaires were used to gather qualitative data. The use of qualitative interviewing may have been more useful for understanding the meaning of a program to its participants and providing richer data for content analysis (Kale, 1996).
Conclusion
The Fam-HELP program demonstrates that active engagement of family caregivers in preventive interventions for delirium is feasible. Thus, a noteworthy strength of this work is the potential to enhance family participation in HELP programs, which may help to improve effectiveness of HELP models for delirium prevention, and potentially sustain these effects after hospital discharge. Given that delirium has poor outcomes, frequent persistence beyond discharge, tremendous costs, high caregiver burden, and is often preventable, the public health implications of family participation in delirium prevention are substantial (Inouye, Schlesinger, & Lydon, 1999).
From this study, recommendations have been developed to maximize family participation in Fam-HELP, including: 1) Workshops for staff nurses on various aspects of delirium, to include risk factors, clinical presentation, and prevention strategies, with an emphasis on how to work in partnership with family caregivers; 2) A letter introducing the geriatric specialist nurse on the unit to be given to family caregivers of older adults on admission, giving the family caregiver the opportunity to discuss any concerns; and, 3) Posters on all the units to support the Fam-HELP program. These strategies can help to facilitate a partnership between the older adult, family caregiver, and staff nurse with the goal of supporting a culture of family-centered care. Thus, this study may help us to more sensitively and effectively integrate family caregivers into acute care and discharge planning, and lays the groundwork to test these interventions to optimize patient care and outcomes.
Contributor Information
Deborah A. Rosenbloom-Brunton, Acute Care Nurse Practitioner Program, Graduate Program in Nursing, Massachusetts General Hospital Institute of Health Professions, 36 First Avenue, Boston, MA 02129, drosenbloom@mghihp.edu.
Elizabeth A. Henneman, School of Nursing, University of Massachusetts Amherst, Amherst, Massachusetts.
Sharon K. Inouye, Aging Brain Center, Milton & Shirley F. Levy Family Chair, Institute for Aging Research, Hebrew SeniorLife, Boston, Massachusetts, Professor of Medicine, Harvard Medical School, Cambridge, Massachusetts. Staff Physician, Beth Israel Deaconess Medical Center, Boston, Massachusetts, AgingBrainCenter@hsl.harvard.edu.
References
- Addington J, Collins A, McCleery A, Addington D. The role of family work in early psychosis. Schizophrenia Research. 2005;79(1):77–83. doi: 10.1016/j.schres.2005.01.013. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision. American Psychiatric Association; 2000. [Google Scholar]
- Bogardus ST, Desai MM, Williams CS, Leo-Summers LM, Acampora D, Inouye SK. The effects of a targeted multicomponent delirium intervention on postdischarge outcomes for hospitalized older adults. American Journal of Medicine. 2003;114:383–390. doi: 10.1016/s0002-9343(02)01569-3. [DOI] [PubMed] [Google Scholar]
- Bohn U, Wright LM, Moules NJ. A family systems nursing interview following a myocardial infarction: The power of commendations. Journal of Family Nursing. 2003;9(2):151–165. [Google Scholar]
- Caplan GA, Harper EL. Recruitment of volunteers to improve vitality in the elderly: The REVIVE* study. Internal Medicine Journal. 2007;37:95–100. doi: 10.1111/j.1445-5994.2007.01265.x. [DOI] [PubMed] [Google Scholar]
- Chatham MA. The effect of family involvement on patient’ manifestations of postcardiotomy psychosis. Heart & Lung. 1978;7:995–999. [PubMed] [Google Scholar]
- Cole MG. Delirium in elderly patients. American Journal of Geriatric Psychiatry. 2004;12:7–21. [PubMed] [Google Scholar]
- DeRenzo EG, Conley RR, Love R. Assessment of the capacity to give consent to research participation: State of the art and beyond. Journal of Health Care Law Policy. 1998;1(1):66–87. [PubMed] [Google Scholar]
- Duhamel F, Talbot LR. A constructivist evaluation of family systems nursing interventions with families experiencing cardiovascular and cerebrovascular illness. Journal of Family Nursing. 2004;10(1):12–32. [Google Scholar]
- Dunst CJ, Trivette CM. Family matters. Empowerment, effective helpgiving practices and family-centered care. Pediatric Nursing. 1996;22(4):334–337. [PubMed] [Google Scholar]
- Field AP, Morse JM. Nursing research: The application of qualitative approaches. London: Croom Helm; 1985. [Google Scholar]
- Flaherty JH, Raghavan S, Bakshi S, Moinuddin A, Morley JE. A model for managing delirious older inpatients. Journal of the American Geriatrics Society. 2003;51:1031–1051. doi: 10.1046/j.1365-2389.2003.51320.x. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gagnon P, Charbonneau C, Allard P, Soulard C, Dumont S, Fillion L. Delirium in advanced cancer: A psychoeducational intervention for family caregivers. Journal of Palliative Care. 2002;18(4):253–261. [PubMed] [Google Scholar]
- Hupcey JE. Establishing the nurse-family relationship in the intensive care unit. Western Journal of Nursing Research. 2008;20(2):180–194. doi: 10.1177/019394599802000204. [DOI] [PubMed] [Google Scholar]
- Inouye SK, Bogardus ST, Jr, Williams CS, Leo-Summers L, Acampora D, Holford TR, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. New England Journal of Medicine. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- Inouye SK, Bogardus ST, Jr, Baker DI, Leo-Summers L, Cooney LM., Jr The Hospital Elder Life Program: A model of care to prevent cognitive and functional decline in older hospitalized patients. Journal of the American Geriatrics Society. 2000;48(12):1697–1706. doi: 10.1111/j.1532-5415.2000.tb03885.x. [DOI] [PubMed] [Google Scholar]
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized older persons: predictive model and interrelationship with baseline vulnerability. Journal of the American Medical Association. 1996;275:852–857. [PubMed] [Google Scholar]
- Inouye SK, Rushing JT, Foreman MD, Palmeiri RM, Pompei P. Does delirium contribute to poor outcomes? A three site epidemiological study. Journal of General Internal Medicine. 1998;13:234–242. doi: 10.1046/j.1525-1497.1998.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inouye SK, Schlesinger MJ, Lydon TJ. Delirium: A symptom of how hospital care is failing older persons and a window to improve quality of hospital care. American Journal of Medicine. 1999;106:565–573. doi: 10.1016/s0002-9343(99)00070-4. [DOI] [PubMed] [Google Scholar]
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: The Confusion Assessment Method. A new method for detection of delirium. Annals of Internal Medicine. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Maskowitz RW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kvale S. Inter Views: An introduction to qualitative research interviewing. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- Leahey M. Families and chronic illness: Assumptions, assessment, and interventions. In: Wright LM, Leahey M, editors. Families and chronic illness. Springhouse, PA: Springhouse; 1987. pp. 55–76. [Google Scholar]
- Leahey M, Harper-Jacques S. Family-nurse relationships: Core assumptions and clinical implications. Journal of Family Nursing. 1996;2(2):133–151. [Google Scholar]
- Leslie DL, Zhang Y, Bogardus ST, Holford R, Leo-Summers L, Inouye SK. Consequences of preventing delirium in hospitalized older adults on nursing home costs. Journal of American Geriatrics Society. 2005;53:405–409. doi: 10.1111/j.1532-5415.2005.53156.x. [DOI] [PubMed] [Google Scholar]
- Lincoln YS, Guba EG. Naturalistic inquiry. London: Sage; 1985. [Google Scholar]
- Lundstrom M, Edlund A, Lundstrom G, Gustavson Y. Reorganization of nursing and medical care to decrease the incidence of postoperative delirium and improve rehabilitation outcome in elderly patients treated for femoral neck fractures. Scandinavian Journal of Caring Sciences. 1999;13:193–200. [PubMed] [Google Scholar]
- MacPhee GJ, Crowther JA, McAlpine CH. A simple screening test for hearing impairment in elderly patients. Age Aging. 1988;17:347–351. doi: 10.1093/ageing/17.5.347. [DOI] [PubMed] [Google Scholar]
- Martin-Arafeh JM, Watson CL, Baird SM. Promoting family centered care in high-risk pregnancy. Journal of Perinatal Neonatal Nursing. 1999;13(1):27–42. doi: 10.1097/00005237-199906000-00004. [DOI] [PubMed] [Google Scholar]
- Mayring P. [Retrieved November 25, 2006];Qualitative content analysis. 2000 :24. from http://wwww,qualitative-research,net/fqs-texte/2-00/1 -OOmayring-e.pdf. [Google Scholar]
- McAvay GJ, van Ness PH, Bogardus ST, Zhany H, Leslie DL, Leo-Summers LS, et al. Older adults discharged from the hospital with delirium: One year outcomes. Journal of the American Geriatrics Society. 2006;54:1245–1250. doi: 10.1111/j.1532-5415.2006.00815.x. [DOI] [PubMed] [Google Scholar]
- McCusker J, Cole M, Abrahamowicz M, Han L, Podoba JE, Ramman-Haddad L. Environmental risk factors for delirium in hospitalized older people. Journal of the American Geriatrics Society. 2001;49:1327–1334. doi: 10.1046/j.1532-5415.2001.49260.x. [DOI] [PubMed] [Google Scholar]
- Milisen K, Foreman MD, Abraham IL, DeGeest S, Godderis J, Vandermeulen E, et al. A nurse led interdisciplinary intervention program for delirium in elderly hip fracture patients. Journal of the American Geriatrics Society. 2001;49:523–532. doi: 10.1046/j.1532-5415.2001.49109.x. [DOI] [PubMed] [Google Scholar]
- Mulrow CD, Aguilar C, Endicott JF, Velez R, Tuley MR, Charlip WS, et al. Association between hearing impairment and quality of life of elderly individuals. Journal of the American Geriatrics Society. 1990;38(1):45–50. doi: 10.1111/j.1532-5415.1990.tb01595.x. [DOI] [PubMed] [Google Scholar]
- O’Keeffe ST, Lavan JN. Clinical significance of delirium subtypes in older people. Age and Aging. 1999;28:115–119. doi: 10.1093/ageing/28.2.115. [DOI] [PubMed] [Google Scholar]
- Riley-Doucet C. Beliefs about the controllability of pain: Congruence between older adults with cancer and their family caregivers. Journal of Family Nursing. 2005;11(3):225–241. doi: 10.1177/1074840705279157. [DOI] [PubMed] [Google Scholar]
- Rizzo JA, Bogardus ST, Leo-Summers L, Williams CS, Acampora D, Inouye SK. Multicomponent targeted intervention to prevent delirium in hospitalized older patients: what is the economic value? Medical Care. 2001;39:740–752. doi: 10.1097/00005650-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Rubin FH, Williams JT, Lescisin DA, Mook WJ, Hassan S, Inouye SK. Replicating the Hospital Elder Life Program (HELP) in a community hospital and demonstrating effectiveness using administrative data. Journal of American Geriatrics Society. 2006;54:969–974. doi: 10.1111/j.1532-5415.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- Rutledge DN, Donaldson NE, Pravikoff DS. Caring for families of patients in acute or chronic health care settings. Journal of Clinical Innovations. 2000;3(2):1–26. [Google Scholar]
- Siddiqi N, Horne AO, House AO, Holmes JD. Occurrence and outcome of delirium in medical inpatients: A systematic review. Age and Aging. 2006;35:350–364. doi: 10.1093/ageing/afl005. [DOI] [PubMed] [Google Scholar]
- Simpson P, Yeung FK, Kwan AT, Wah WK. Family systems nursing: A guide to mental health care in Hong Kong. Journal of Family Nursing. 2006;12(3):276–291. doi: 10.1177/1074840706291436. [DOI] [PubMed] [Google Scholar]
- The Administration on Aging. A profile of older Americans. Washington, D.C.: American Association of Retired Persons; 2004. [Google Scholar]
- Weber JB, Coverdale JH, Kunik ME. Delirium: Currents trends in prevention and treatment. Journal of Internal Medicine. 2004;34:115–121. doi: 10.1111/j.1444-0903.2004.00549.x. [DOI] [PubMed] [Google Scholar]
- Wright LM, Leahey M. Families and life-threatening illness: Assumptions, assessment, and interventions. In: Leahey M, Wright LM, editors. Families and life threatening illness. Springhouse, PA: Springhouse; 1987. pp. 45–58. [Google Scholar]
- Wright LM, Leahey M. A guide to family assessment and intervention. 4th ed. Philadelphia: F. A. Davis; 2000. [Google Scholar]
- Young J, Inouye SK. Delirium in older people. British Medical Journal. 2007;334:842–846. doi: 10.1136/bmj.39169.706574.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]