Abstract
Background
Laparoscopic cholecystectomy (LC) is the gold standard procedure for gallbladder removal. Conversion to an open procedure is sometimes deemed necessary, especially in complex cases in which a prolonged laparoscopic operative time is anticipated. A prolonged LC case is thought to be associated with increased complications and cost and therefore generally discouraged. The purpose of this study was to test this assumption, and compare outcomes and cost of converted and prolonged LC cases.
Methods
By using institutional National Surgical Quality Improvement Program and financial databases, we retrospectively reviewed and compared prolonged laparoscopic cases (Long-LC) with converted (CONV) procedures. Surgical times, length of stay (LOS), 30-day complications, operative room, and total hospital charges were compared between the 2 groups.
Results
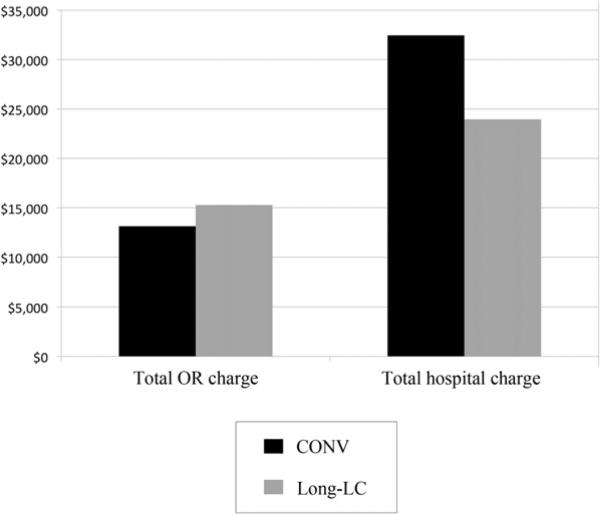
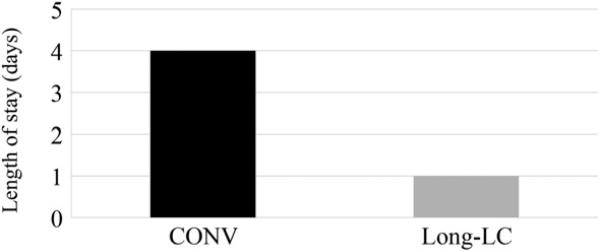
A total of 101 Long-LC and 66 CONV cases met our inclusion criteria. Long-LC cases were 19 minutes longer than CONV cases (123 vs 104 min; P <.01). No differences in postoperative complications were found between the 2 groups (P > .05). When Poisson regression was used, we found that LOS was significantly shorter in the Long-LC compared with CONV group (1 day vs 4 days; P < .01). Long-LC cases had greater operative charges ($15,278 vs $13,128; P < .01). However, hospital charges for Long-LC cases were 26% less than for CONV cases ($23,946 vs $32,446; P < .01).
Conclusion
Conversion is associated with a 3-day increase in LOS. Long-LC cases have greater operative room charges, but overall hospital charges were 26% less than CONV cases. Our data suggest that decision making regarding conversion should focus on safety and not time considerations.
Within a decade after the first Laparoscopic Cholecystectomy (LC) was performed in 1985, this approach became the gold standard procedure for the treatment of gallstone disease.1,2 Now, more than 700,000 LCs are performed annually in the United States. The benefits of the laparoscopic approach for the patient include decreased surgical trauma, less postoperative pain, shorter hospital stay, and faster recovery.3 Despite several “relative” contraindications in the early days of laparoscopy, such as previous upper abdominal surgery, pregnancy, and cirrhosis, LC has proven to be feasible and safe for most patients.4-6 The benefits of this approach, however, rapidly disappear when a case is converted to open surgery. Despite improved surgical technology and increased surgical skills with laparoscopic technique, conversion rates of up to 10% continue to be reported.7-14
Several patient-related factors have been identified that are associated with increased risk of conversion, including male gender and older age.11,15-17 Intraoperative factors, however, are the final determinant of why a surgeon converts a laparoscopic case to open. Such intraoperative factors lead to conversions that can be divided to enforced conversions, which result from intraoperative complications (eg, organ damage, bleeding), or elective conversions, which are caused by a lack of progression and difficult dissection leading to prolonged operative times.11,18 The latter follows the assumption that a prolonged laparoscopic case is associated with increased cost and complications.
The aim of this study is to compare operative times, postoperative outcome, and cost between patients who underwent a long laparoscopic case with those that were converted to open surgery to determine whether a long LC is indeed associated with increased adverse outcomes and cost.
METHODS
Data source and study population
After obtaining approval from the institutional review board, we used the appropriate Current Procedure Terminology codes (47600 and 47562) and our own institutional National Surgical Quality Improvement Program (NSQIP) database to identify all patients who had undergone open and laparoscopic cholecystectomy between January 2002 and September 2009. The NSQIP is a prospective clinical database that was designed and launched by the American College of Surgeons to provide feedback to hospitals for quality improvement purposes. The variables that are collected include patient demographics, preoperative risk factors, laboratory values, intraoperative variables, and 30-day postoperative mortality and morbidity outcomes for patients undergoing surgical procedures in both inpatient and outpatient settings. This system allows easy and quick analysis of data with occasional multilayered filtering and complex patient criteria settings.
On the basis of the operating time distribution, the longest 10% of the LC cases were selected and considered as the long laparoscopic group (Long-LC). Because converted LCs are coded with open cholecystectomies, we reviewed the operative reports of all open cases in our institutional NSQIPS database and identified those that had a conversion from laparoscopic to open surgery (CONV). Preoperative variables, including age, gender, body mass index (BMI), and comorbid conditions such as diabetes, hypertension, congestive heart failure, and smoking behavior, were examined along with emergency admission status. Outcome variables studied from the NSQIP database were surgical times, 30-day mortality and morbidity, and length of hospital stay (LOS). Other outcome measures included operative room (OR) charges, anesthesia charges, recovery room charges, and total hospital charges. These data were collected from patient financial records. Cases that included operations or treatments unrelated to gallbladder disease within the same hospital admission were excluded from the analysis, except if these procedures or treatments were the consequences or complications of cholecystectomy.
Statistical analysis
Initially, all variables and outcome measures were plotted, and the Shapiro-Wilk normality test was performed to determine distribution. Demographics and comorbidities were evaluated between the 2 groups to determine comparability. Dichotomous and ordinal variables such as male gender, diabetes, smoking behavior, congestive heart failure, hypertension, American Society of Anesthesiologists (ASA) classification, and emergency admission were compared by the use of the χ2 test. Continuous nonparametric data, including age and BMI, were compared by use of the Wilcoxon ranked sum test and revealed significant differences between the 2 groups for age but not for BMI.
Because there were baseline differences in the patient groups, Poisson regression was selected as the appropriate multivariate model for the comparison of outcome variables, including OR times, LOS, and hospital charges controlling for ASA score, hypertension, male gender, age. All variables were entered into 3 generalized linear Poisson models with LOS, OR times, and hospital charges subsequently selected as dependent variables. Complication rates (dichotomous variable) were compared by the use of logistic regression; we also controlled for the baseline preoperative differences. To identify group as a possible predictor of complication rate, all 4 preoperative comorbidities were entered into a hierarchical logistic regression model, where the dependent variable was overall complication rate. Independent variables in the model were sequentially removed until all remaining variables in the model showed significance. Medians are reported for the data. A P value of less than .05 was considered statistically significant.
RESULTS
Between January 2002 and September 2009, 1,122 laparoscopic and 167 open cholecystectomies were performed at our institution and entered in to the NSQIP database. OR time distribution revealed a positively skewed distribution for LC procedures (Fig 1). The median OR time of all LC cases was 63 minutes, with a LOS of 0 days (most of cases were day-surgery cases). A total of 70 cases were converted to open surgery. The conversion rate was 6% on the basis of the cases entered to our NSQIP database.
Fig 1.
Operative room (OR) time distribution for all laparoscopic cholecystectomies. The longest 10% of cases were selected and used as the Long-LC group (highlighted area).
The longest 10% of LC cases were selected on the basis of the OR time distribution and defined as cases that required prolonged operating time. In this group, it resulted in a median OR time of 123 minutes, which was nearly double the overall average OR time of 63 minutes. A total of 101 cases met our inclusion criteria stated previously and were categorized as the longest laparoscopic group (Long-LC). A total of 66 converted cases met our inclusion criteria and were entered to the converted group (CONV).
Demographics for each group are summarized in Table I. Age and distribution of male gender were significantly greater in the CONV group than in the Long-LC group (age: 62 vs 44 years, CONV versus Long-LC group, respectively; P < .01; male gender: 53% vs 29%, CONV versus Long-LC respectively; P <.01). BMI and co-morbid conditions were similar between the 2 groups, with the exception of hypertension, which was more prevalent in the CONV group (58% vs 29%, CONV versus Long-LC, respectively; P < .01). The rate of emergency surgery was similar (15% vs 8%, CONV versus Long-LC, respectively; P > .05). Patients in the CONV group, however, were more likely to have an ASA score of III or greater (32% vs 11%, CONV versus Long-LC; P > .05; Table II). The most common reasons for conversion were difficult dissection secondary to severe inflammation, dense adhesions, or unusual anatomy. Intraoperative cholangiography was not performed in either of the groups.
Table I.
Demographics for Long-LC and CONV group
| Characteristics | Long-LC | CONV | P value |
|---|---|---|---|
| Male gender, % | 29 | 53 | <.01 |
| Age, yr | 44 | 62 | <.01 |
| BMI, kg/m2 | 30 | 28 | NS |
BMI, Body mass index; CONV, conversion; Long-LC, long laparoscopy; NS, not significant.
Table II.
Preoperative comorbid conditions and confounders
| Long-LC | CONV | P value | |
|---|---|---|---|
| Hypertension, % | 29 | 58 | <.01 |
| Diabetes, % | 12 | 21 | NS |
| Smoking, % | 15 | 11 | NS |
| CHF, % | 0 | 2 | NS |
| Emergency admission, % | 8 | 15 | NS |
| ASA classification, % | <.01 | ||
| • 1, Healthy | 22 | 8 | |
| • 2, Mild systemic disease | 67 | 58 | |
| • 3, Severe systemic disease | 11 | 32 | |
| • 4, Life-threatening | 0 | 3 |
ASA, American Society of Anesthesiologists; CHF, congestive heart failure; CONV, conversion; Long-LC, long laparoscopy; NS, not significant.
No mortality was observed in the 2 groups. CONV cases were significantly shorter in terms of operating time than Long-LC cases (104 vs 123 minutes, CONV versus Long-LC, respectively; P <.01). There were no significant differences in the postoperative complication rates as collected by NSQIP between the 2 groups (4.5% vs 6.9%, CONV versus Long-LC respectively; P >.05; Table III). One CBD injury occurred in the CONV group. The LOS was 3 days longer for the CONV group (4 vs 1 day, CONV versus Long-LC, respectively; P < .01; Fig 2).
Table III.
NSQIP complication rates for the 2 groups
| Long-LC | CONV | P value | |
|---|---|---|---|
| Total complication rate, % | 6.9 | 4.5 | NS |
| Superficial skin infection, % | 3.9 | 4.5 | NS |
| Postoperative pneumonia, % | 1 | 0 | NS |
| Urinary tract infection, % | 1 | 0 | NS |
| Blood transfusion, % | 0 | 0 | NS |
CONV, Conversion; Long-LC, long laparoscopy; NS, not significant; NSQIP, National Surgical Quality Improvement Program.
Fig 2.
Differences between LOS between CONV (black bar) and Long-LC (grey bar) groups (P < .01). Long-LC cases are associated with shorter hospital stay.
As expected, and because of the shorter surgical times, OR charges were significantly lower in the CONV group than in the Long-LC group ($9,520 vs $11,121, CONV versus Long-LC, respectively; P < .01) along with the anesthesia charge ($1,107 vs $1,240, CONV versus Long-LC, respectively; P < .01). Total OR charges were also significantly lower in the CONV than the Long-LC group ($13,128 vs $15,278, CONV versus Long-LC, respectively; P < .01). The total hospital charges, however, demonstrated a different trend, with increased cost for the CONV group compared with the Long-LC, reflecting the greater postoperative stay ($32,446 vs $23,946, CONV versus Long-LC, respectively; P < .01; Table IV and Fig 3). Thus, a long-LC was associated with a 26% reduction in costs compared with CONV cases.
Table IV.
Hospital charges
| Long-LC | CONV | P value | |
|---|---|---|---|
| Median operative time | 123 | 104 | <.01 |
| Initial OR charge | 1,353 | 1,353 | NS |
| OR charge | 11,121 | 9,520 | <.01 |
| Anesthesia charge | 1,240 | 1,107 | <.01 |
| Recovery room charge | 1,368 | 1,449 | <.01 |
| Total OR charge | 15,278 | 13,128 | <.01 |
| Total hospital charge | 23,946 | 32,446 | <.01 |
All charges are shown in dollars.
CONV, Conversion; Long-LC, long laparoscopy; NS, not significant; OR, operating room.
Fig 3.
Total OR charge and total hospital charge. CONV group (black bar) and Long-LC group (grey bar) are shown. Although OR charges are greater for Long-LC cases, overall hospital charges are less for these cases as the result of shorter hospital stay.
DISCUSSION
Despite 2 decades of increased experience and improvements in laparoscopic surgery and technology, conversion to open surgery occurs with rates that have remained stable between 5% and 10%.7,10,12 Tang and Cuschieri11 reviewed the available literature between 1990 and 2005 and identified 110 publications on the subject of conversion. They divided conversions into elective conversions, undertaken as the result of a difficult dissection, or enforced conversions, performed as the result of a serious operative complication (bleeding or bile duct injury). Lo et al19 found that an early conversion in elderly patients with acute cholecystitis is favorable. Such data have focused the surgeon's attention on operative times as a primary determinant of conversion with the hypothesis that a long LC is associated with adverse outcomes and a quick decision to convert leads to better results. This principle is further highlighted in medico-legal cases, where a delay in converting to traditional cholecystectomy can be used as evidence of poor surgical judgment.20,21 Our series provides a contemporary overview of the impact of OR times on LC outcomes.
In our study, we compared outcomes of patients undergoing a Long-LC (median OR time 123 min, which was double that of overall median OR time of 63 min) to those who had a converted case. As expected, patients in the CONV group were older and more frequently male, which are reported risk factors for conversion.15-19,22-33 The CONV group also had greater preoperative ASA scores and some comorbidities, such as hypertension (Table II). We corrected for these differences by using a multivariate analysis. Following such adjustments, we found that CONV cases were significantly shorter in terms of OR times but were associated with a 3-day increase in LOS compared with the Long-LC group. Despite the longer OR times in Long-LC group, the complication rates between these cases and CONV cases were similar, suggesting that a long laparoscopic case per se is not associated with increased complications.
The other variable of interest in this study was hospital charges. Both Long-LC and CONV cases began with the basic OR charge for laparoscopic surgeries, as both procedures began as such. Once the procedure was converted, the significantly reduced OR time resulted in reduced total OR charges for the CONV group. The 3-day longer hospital stay, however, that followed a conversion, resulted in increased nonoperative charges for the CONV group, with eventual overall hospital charges being $8,500 greater than the Long-LC group (35% increase in total charges).
Our findings indicate that conversion of LC to open surgery is associated with significant disadvantages to the patient (increased LOS) and the health care system (increased cost), with no apparent advantage (similar complication rates). Although we acknowledge that conversion of laparoscopic cases is sometimes necessary and at times a sign of good surgical judgment, we believe that this contemporary review challenges some of the long-held belief that prolonged LCs are associated with more adverse events. We thus believe that elective conversions as the result of concerns with surgical time alone are not justified.
Also, the legal practice of using long laparoscopic times before conversion as evidence of poor surgical judgment may not be accurate. In our practice, we pursue a laparoscopic case as long as progress is being made in terms of dissection and safety is not compromised. On the basis of our findings, the circumstances and the causes of conversion require significant attention to improve both the clinical and financial outcome of minimally invasive surgeries in the future. This is of particular importance and relevance in this era, where our residents are graduating with much greater competency in dealing with complex laparoscopic cases. In fact many of the graduating chief residents finish with very limited experience in open cholecystectomy; thus, the fall-back position of converting to open surgery, which appeared safe 15 years ago, may in fact not be the case.34-40
Our study has several strengths and weaknesses. Our data cover a time period during which competency with LC was high and is determined on the basis of an accurate data source (NSQIP), and we believe it provides insight in to current practice of LC. Using our own institutional data, we were able to track charges accurately by reviewing the charts of all patients individually. However, such a single institutional review also provides some weaknesses. The results are primarily determined from data from 1 academic institution, with relatively small sample size for our CONV group. In other studies investigators have used larger patient populations and included both academic and smaller community hospitals, with number of converted cases in some studies exceeding 20041; however, detailed charge analysis are not feasible in such studies.
Our analysis also revealed that 8% (n = 97) of our patients had an open cholecystectomy, with no attempt at a laparoscopic dissection. This rate is comparable with that reported in other studies.7,13 A recent study from the Veterans Health Administration hospitals reported an open cholecystectomy rate of 9% between years 2005 and 2008,7 similar to the rate reported from a contemporary review of an academic medical center.13 To understand this observation better, we compared the percentage of ASA category III (severe systemic disease) patients in CONV to open cholecystectomy cases and found that the rate of ASA III patients was significantly greater in open cholecystectomies than in the CONV group (49% vs 32%, open versus CONV respectively; P < .05), indicating that our institution favored the open approach for ill patients. This bias in our study needs to be considered when looking at this data.
We controlled between the groups using NSQIP-defined comorbidities; however, there may be other relevant differences between the groups that were not captured by the database, including level of experience of the surgeon. This will be an important future objective for our studies. Although we found no difference between emergency admission rate between CONV and Long-LC cases (Table II), this rate was nearly twice as high in the CONV group, raising the possibility for a statistical error considering the relative small numbers. Finally, our charge and cost analysis, which was based on our institution's charging model, can be different from other hospitals’ charging system. The percentage increase in cost, however, can be used as a guide to increase costs associated with converted surgeries at other institutions. We did not perform a cost analysis for routine cholecystectomies because we believe this will provide a bias comparison for costs. Our objective was to assess cost implications for complex cholecystectomies, and, thus, a comparison between Long-LC and CONV seemed most appropriate to us.
In conclusion, this study found that long-LC is associated with increased surgical times but this was not associated with an increase in complications. Although OR charges were greater for long-LC cases, the CONV group had a longer LOS and greater overall hospital charges. These findings suggest that there is an inevitable paradigm shift in our current laparoscopic era and open surgery may no longer be a better alternative, even when surgeons face the prospect of a long laparoscopic case. Our other studies have tried to understand the circumstances under which conversions occur, to help develop guidelines to reduce conversion rates.42
Acknowledgments
Supported by the National Center for Image Guided Therapy under training grant R25 CA089017.
Footnotes
This work has been selected for oral presentation at the 2011 Academic Surgical Congress, Huntington Beach, CA.
REFERENCES
- 1.Begos DG, Modlin IM. Laparoscopic cholecystectomy: from gimmick to gold standard. J Clin Gastroenterol. 1994;19:325–30. doi: 10.1097/00004836-199412000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Sain AH. Laparoscopic cholecystectomy is the current “gold standard” for the treatment of gallstone disease. Ann Surg. 1996;224:689–90. doi: 10.1097/00000658-199611000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006:CD006231. doi: 10.1002/14651858.CD004788.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ji W, Li LT, Wang ZM, Quan ZF, Chen XR, Li JS. A randomized controlled trial of laparoscopic versus open cholecystectomy in patients with cirrhotic portal hypertension. World J Gastroenterol. 2005;11:2513–7. doi: 10.3748/wjg.v11.i16.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karayiannakis AJ, Polychronidis A, Perente S, Botaitis S, Simopoulos C. Laparoscopic cholecystectomy in patients with previous upper or lower abdominal surgery. Surg Endosc. 2004;18:97–101. doi: 10.1007/s00464-003-9001-4. [DOI] [PubMed] [Google Scholar]
- 6.Glasgow RE, Visser BC, Harris HW, Patti MG, Kilpatrick SJ, Mulvihill SJ. Changing management of gallstone disease during pregnancy. Surg Endosc. 1998;12:241–6. doi: 10.1007/s004649900643. [DOI] [PubMed] [Google Scholar]
- 7.Kaafarani HM, Smith TS, Neumayer L, Berger DH, Depalma RG, Itani KM. Trends, outcomes, and predictors of open and conversion to open cholecystectomy in Veterans Health Administration hospitals. Am J Surg. 2010;200:32–40. doi: 10.1016/j.amjsurg.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Low SW, Iyer SG, Chang SK, Mak KS, Lee VT, Madhavan K. Laparoscopic cholecystectomy for acute cholecystitis: safe implementation of successful strategies to reduce conversion rates. Surg Endosc. 2009;23:2424–9. doi: 10.1007/s00464-009-0374-x. [DOI] [PubMed] [Google Scholar]
- 9.Wiseman JT, Sharuk MN, Singla A, et al. Surgical management of acute cholecystitis at a tertiary care center in the modern era. Arch Surg. 2010;145:439–44. doi: 10.1001/archsurg.2010.54. [DOI] [PubMed] [Google Scholar]
- 10.Livingston EH, Rege RV. A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg. 2004;188:205–11. doi: 10.1016/j.amjsurg.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Tang B, Cuschieri A. Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg. 2006;10:1081–91. doi: 10.1016/j.gassur.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Ballal M, David G, Willmott S, Corless DJ, Deakin M, Slavin JP. Conversion after laparoscopic cholecystectomy in England. Surg Endosc. 2009;23:2338–44. doi: 10.1007/s00464-009-0338-1. [DOI] [PubMed] [Google Scholar]
- 13.Wolf AS, Nijsse BA, Sokal SM, Chang Y, Berger DL. Surgical outcomes of open cholecystectomy in the laparoscopic era. Am J Surg. 2009;197:781–4. doi: 10.1016/j.amjsurg.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Harboe KM, Bardram L. The quality of cholecystectomy in Denmark: outcome and risk factors for 20,307 patients from the national database. Surg Endosc. 2011;25:1630–41. doi: 10.1007/s00464-010-1453-8. [DOI] [PubMed] [Google Scholar]
- 15.Merriam LT, Kanaan SA, Dawes LG, et al. Gangrenous cholecystitis: analysis of risk factors and experience with laparoscopic cholecystectomy. Surgery. 1999;126:680–5. discussion 85-6. [PubMed] [Google Scholar]
- 16.Rosen M, Brody F, Ponsky J. Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg. 2002;184:254–8. doi: 10.1016/s0002-9610(02)00934-0. [DOI] [PubMed] [Google Scholar]
- 17.Wiebke EA, Pruitt AL, Howard TJ, et al. Conversion of laparoscopic to open cholecystectomy. An analysis of risk factors. Surg Endosc. 1996;10:742–5. doi: 10.1007/BF00193048. [DOI] [PubMed] [Google Scholar]
- 18.Peters JH, Krailadsiri W, Incarbone R, et al. Reasons for conversion from laparoscopic to open cholecystectomy in an urban teaching hospital. Am J Surg. 1994;168:555–8. doi: 10.1016/s0002-9610(05)80121-7. discussion 58-9. [DOI] [PubMed] [Google Scholar]
- 19.Lo CM, Fan ST, Liu CL, Lai EC, Wong J. Early decision for conversion of laparoscopic to open cholecystectomy for treatment of acute cholecystitis. Am J Surg. 1997;173:513–7. doi: 10.1016/s0002-9610(97)00005-6. [DOI] [PubMed] [Google Scholar]
- 20.Low A, Decker D, Kania U, Hirner A. Forensic aspects of complicated laparoscopic cholecystectomy [in German]. Chirurg. 1997;68:395–402. doi: 10.1007/s001040050204. [DOI] [PubMed] [Google Scholar]
- 21.McLean TR. Risk management observations from litigation involving laparoscopic cholecystectomy. Arch Surg. 2006;141:643–8. doi: 10.1001/archsurg.141.7.643. discussion 48. [DOI] [PubMed] [Google Scholar]
- 22.Liu CL, Fan ST, Lai EC, Lo CM, Chu KM. Factors affecting conversion of laparoscopic cholecystectomy to open surgery. Arch Surg. 1996;131:98–101. doi: 10.1001/archsurg.1996.01430130100022. [DOI] [PubMed] [Google Scholar]
- 23.Schafer M, Krahenbuhl L, Buchler MW. Predictive factors for the type of surgery in acute cholecystitis. Am J Surg. 2001;182:291–7. doi: 10.1016/s0002-9610(01)00702-4. [DOI] [PubMed] [Google Scholar]
- 24.Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M. A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg. 2001;181:520–5. doi: 10.1016/s0002-9610(01)00633-x. [DOI] [PubMed] [Google Scholar]
- 25.Fried GM, Barkun JS, Sigman HH, et al. Factors determining conversion to laparotomy in patients undergoing laparoscopic cholecystectomy. Am J Surg. 1994;167:35–9. doi: 10.1016/0002-9610(94)90051-5. discussion 39-41. [DOI] [PubMed] [Google Scholar]
- 26.Alponat A, Kum CK, Koh BC, Rajnakova A, Goh PM. Predictive factors for conversion of laparoscopic cholecystectomy. World J Surg. 1997;21:629–33. doi: 10.1007/pl00012288. [DOI] [PubMed] [Google Scholar]
- 27.Bingener-Casey J, Richards ML, Strodel WE, Schwesinger WH, Sirinek KR. Reasons for conversion from laparoscopic to open cholecystectomy: a 10-year review. J Gastrointest Surg. 2002;6:800–5. doi: 10.1016/s1091-255x(02)00064-1. [DOI] [PubMed] [Google Scholar]
- 28.Kama NA, Doganay M, Dolapci M, Reis E, Atli M, Kologlu M. Risk factors resulting in conversion of laparoscopic cholecystectomy to open surgery. Surg Endosc. 2001;15:965–8. doi: 10.1007/s00464-001-0008-4. [DOI] [PubMed] [Google Scholar]
- 29.Kanaan SA, Murayama KM, Merriam LT, et al. Risk factors for conversion of laparoscopic to open cholecystectomy. J Surg Res. 2002;106:20–4. doi: 10.1006/jsre.2002.6393. [DOI] [PubMed] [Google Scholar]
- 30.Rutledge D, Jones D, Rege R. Consequences of delay in surgical treatment of biliary disease. Am J Surg. 2000;180:466–9. doi: 10.1016/s0002-9610(00)00520-1. [DOI] [PubMed] [Google Scholar]
- 31.Lein HH, Huang CS. Male gender: risk factor for severe symptomatic cholelithiasis. World J Surg. 2002;26:598–601. doi: 10.1007/s00268-001-0275-1. [DOI] [PubMed] [Google Scholar]
- 32.Sikora SS, Kumar A, Saxena R, Kapoor VK, Kaushik SP. Laparoscopic cholecystectomy–can conversion be predicted? World J Surg. 1995;19:858–60. doi: 10.1007/BF00299786. [DOI] [PubMed] [Google Scholar]
- 33.Shea JA, Healey MJ, Berlin JA, et al. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg. 1996;224:609–20. doi: 10.1097/00000658-199611000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schulman CI, Levi J, Sleeman D, et al. Are we training our residents to perform open gall bladder and common bile duct operations? J Surg Res. 2007;142:246–9. doi: 10.1016/j.jss.2007.03.073. [DOI] [PubMed] [Google Scholar]
- 35.Namias N, McKenney MG, Sleeman D, Hutson DG. Trends in resident experience in open and laparoscopic cholecystectomy. Surg Laparosc Endosc. 1997;7:245–7. [PubMed] [Google Scholar]
- 36.Helling TS, Khandelwal A. The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg. 2008;12:153–8. doi: 10.1007/s11605-007-0378-6. [DOI] [PubMed] [Google Scholar]
- 37.Chung RS, Wojtasik L, Pham Q, Chari V, Chen P. The decline of training in open biliary surgery: effect on the residents’ attitude toward bile duct surgery. Surg Endosc. 2003;17:338–40. doi: 10.1007/s00464-002-8621-4. discussion 41. [DOI] [PubMed] [Google Scholar]
- 38.Chung RS, Ahmed N. The impact of minimally invasive surgery on residents’ open operative experience: analysis of two decades of national data. Ann Surg. 2010;251:205–12. doi: 10.1097/SLA.0b013e3181c1b18e. [DOI] [PubMed] [Google Scholar]
- 39.Chung R, Pham Q, Wojtasik L, Chari V, Chen P. The laparoscopic experience of surgical graduates in the United States. Surg Endosc. 2003;17:1792–5. doi: 10.1007/s00464-002-8922-7. [DOI] [PubMed] [Google Scholar]
- 40.Karvonen J, Salminen P, Grönroos JM. Bile duct injuries during open and laparoscopic cholecystectomy in the laparoscopic era: alarming trends. Surg Endosc. 2011;25:2906–10. doi: 10.1007/s00464-011-1641-1. [DOI] [PubMed] [Google Scholar]
- 41.Jenkins PJ, Paterson HM, Parks RW, Garden OJ. Open cholecystectomy in the laparoscopic era. Br J Surg. 2007;94:1382–5. doi: 10.1002/bjs.5854. [DOI] [PubMed] [Google Scholar]
- 42.Lengyel BI, Azagury D, Varban O, et al. Laparoscopic cholecystectomy after a quarter century: why do we still convert? Surg Endosc. 2012;26:508–13. doi: 10.1007/s00464-011-1909-5. [DOI] [PMC free article] [PubMed] [Google Scholar]