Abstract
Background
Abdominal aortic calcification (AAC) is a marker of subclinical atherosclerotic disease and an independent predictor of subsequent vascular morbidity and mortality. This study was conducted to investigate the association of AAC with lifestyle and risk factors of cardiovascular disease.
Methods
The results of the abdominal computed tomography of 380 patients who visited Chungnam National University Hospital for a health checkup from January 1, 2008 to December 31, 2009 were reviewed. A six-point scale was used in grading the overall severity of the calcification in three areas of the abdominal aorta, including the area superior to the renal artery, the upper-half area inferior to the renal artery, and the lower-half area inferior to the renal artery, in addition to the common iliac artery. The association of the AAC severity with the age, lifestyle factors, and risk factors of cardiovascular disease was analyzed via multiple linear regression analysis.
Results
In the male subjects, the age, presence of dyslipidemia and smoking were positively related to AAC, but exercising was negatively related to AAC (total R2 = 0.563). In the female subjects, the age and presence of diabetes mellitus, hypertension, and dyslipidemia were positively related to AAC, but exercising was negatively related to AAC (total R2 = 0.547).
Conclusion
AAC was related to both the male and female subjects' age, presence of dyslipidemia, and exercising, to smoking in the male subjects and to the presence of diabetes mellitus and hypertension in the female subjects.
Keywords: Aorta, Calcification, Atherosclerosis, Life Style
INTRODUCTION
Once atherosclerosis develops, atheromatous plaque or fibrous fatty plaque forms, narrowing the blood vessel lumen and weakening the media. Consequently, ischemic heart disease, cerebrovascular disease or peripheral arterial disease is induced.1,2) In most advanced atheroma cases, a partial or extensive calcium deposit is observed. Therefore, blood vessel calcification implies the pathology of atherosclerosis or subclinical cardiovascular disease.3,4) According to the Multiple Risk Factor Intervention Trial,5) the risk factors of atherosclerosis include aging, the male sex, family history, genomic abnormality, high cholesterol levels, hypertension, smoking, diabetes, obesity, insufficient exercise, stress, and drinking.
Since the representative change in the blood vessels due to atherosclerosis has been known to be a form of calcification, many studies on the association of calcification with clinical diseases have been conducted. In particular, studies on the association of calcification in the coronary artery and the aortic arch with cardiovascular disease have been widely conducted. Iribarren et al.6) measured the level of aortic calcification through a chest X-ray and reported that the level is related to coronary artery disease and ischemic heart disease. Oei et al.7) measured the calcification level of the coronary artery using electron beam computed tomography (CT) and suggested that the level is associated with body mass index (BMI), aging, the male sex, diabetes, smoking, an increase in the total cholesterol level, and a low level of high density lipoprotein (HDL). Studies on the relationship between abdominal aortic calcification (AAC) and clinical symptoms are being actively conducted. Wilson et al.8) measured the calcification level of the abdominal aorta using lumbar X-ray and reported that the level was associated with the prevalence and mortality rate of coronary artery and cerebrovascular diseases. Sun and Jang9) measured the calcification levels of the abdominal aorta and the common iliac artery using multidetector row CT and reported that the level was associated with hypertension, diabetes, chronic kidney dysfunction, coronary artery disease, and cerebrovascular disease. As described above, many studies on the association of blood vessel calcification with a high cholesterol level, hypertension, diabetes, and cardiovascular disease have been conducted, but few studies exist on the association of lifestyle habits such as smoking, drinking, exercise, and obesity. In this study, the associations of AAC level with lifestyle and the risk factors of cardiovascular disease were evaluated.
METHODS
1. Study Subjects
Of the 15,432 patients who visited the Health Promotion Center of Chungnam National University Hospital in Daejon between January 1, 2008 and December 31, 2009, 426 patients who underwent an abdominal CT scan for a health checkup or who were advised to undergo an abdominal CT scan after they completed an abdominal sonography were included first. Among them, 46 patients whose drinking, smoking, and exercise data were omitted were excluded. Finally 380 subjects (209 male and 171 female) were selected and their medical records were retrospectively reviewed.
2. Study Methods
1) Data collection
The basic data on subjects' age, drinking amount per drinking day, weekly drinking frequency, daily smoking amount (in packs), total smoking period (in years), exercise time per session (in minutes), weekly exercise frequency, presence of hypertension, dyslipidemia, and diabetes were obtained through records on a questionnaire in the health checkup, which the subjects were asked to accomplish. Their body measurements such as their waist measurements and BMI and the results of their blood tests such as the levels of their fasting blood glucose, total cholesterol, and triglycerides were obtained from their health checkup data. Their weekly exercise time (in min/wk) was calculated using their weekly exercise frequency and exercise time per session. In the present study, diabetes was indicated if the subject was receiving diabetes treatments or if his/her fasting blood glucose level was 126 mg/dL or higher.10) Hypertension was indicated if the subject was receiving hypertension treatments, if his/her systolic blood pressure was 140 mm Hg or higher or if his/her diastolic blood pressure was 90 mm Hg or higher.11) Dyslipidemia was indicated if the subject was receiving treatments for dyslipidemia, if his/her total cholesterol level was 240 mg/dL or higher or if his/her triglycerides level was 200 mg/dL or higher.12) Abdominal obesity was indicated if the waist measurement of a male subject was 90 cm or greater or that of a female subject, 85 cm or greater.13) If the BMI was 25 kg/m2 or greater, the subject was acknowledged as obese.14)
2) Abdominal aortic calcification score measurement
To evaluate the calcification level of the abdominal aorta and the common iliac artery, multidetector row CT (Brilliance 64; Philips, Amsterdam, Netherlands) images were analyzed. The calcification levels in three areas of the abdominal aorta, including the area superior to the renal artery, the upper-half area inferior to the renal artery, and the lower-half area inferior to the renal artery, in addition to the common iliac artery, were measured. The calcification was estimated using the modified criteria which was previously suggested for grading calcification levels:15) grade 0 for cases without calcifications; grade 1 for cases with one or two minimal non-contiguous calcifications without 50% circumference involvement; grade 2 for cases with three or more non-contiguous calcification lesions on less than 50% of the blood vessel wall, or one lesion on 50% or more of the blood vessel wall; grade 3 for cases with two or more non-contiguous calcification lesions on 50% or more of the blood vessel wall; grade 4 for cases with multiple lesions on 50% or more of the blood vessel wall or with only one completely concentric calcification lesion; and grade 5 for cases with multiple completely concentric calcification lesions. The calcification grades were based on the calcification index (CI) (0-5). Only one physician assessed the lesions to avoid individual bias. The calcification level was expressed as the total CI (0-20) in four lesions.
3. Statistical Analysis
For the gender comparisons of the AAC scores, obesity, abdominal obesity, hypertension, diabetes, a high cholesterol level, and smoking pack-years, an independent samples t-test and chi-square test were used. To investigate the association of the AAC score with age, BMI, waist circumference, weekly exercise time, drinking amount, smoking pack-years, hypertension, total cholesterol, triglycerides level, and fasting blood glucose level, a Pearson correlation analysis and independent t-test were conducted. The contribution of the general characteristics of the subjects and cardiovascular disease to the AAC score was investigated through a stepwise multiple linear regression analysis by inputting the significant variables obtained from the Pearson correlation analysis and the independent samples t-test as independent variables and setting the AAC score as a dependent variable. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Statistical significance was recognized with a P-value of 0.05 or lower.
RESULTS
1. General Characteristics of the Subjects
The female subjects were generally older than the male subjects, and had fewer smoking pack-years and lower AAC scores, but more male subjects had diabetes, obesity, and dyslipidemia. More male subjects suffered from hypertension and abdominal obesity than female subjects, but their difference was not statistically significant. The weekly exercise time (± SD) of the male subjects was 102.15 (± 97.08) minutes/week, and of the female subjects, 123.25 (± 123.83) minutes/week. The weekly drinking amount (± SD) of the male subjects was 6.11 (± 10.70) drinks/week, and of the female subjects, 4.94 (± 13.09) drinks/week. There was no statistically significant difference in weekly exercise time and weekly drinking amount between male and female subjects (Table 1).
Table 1.
Characteristics of the subjects
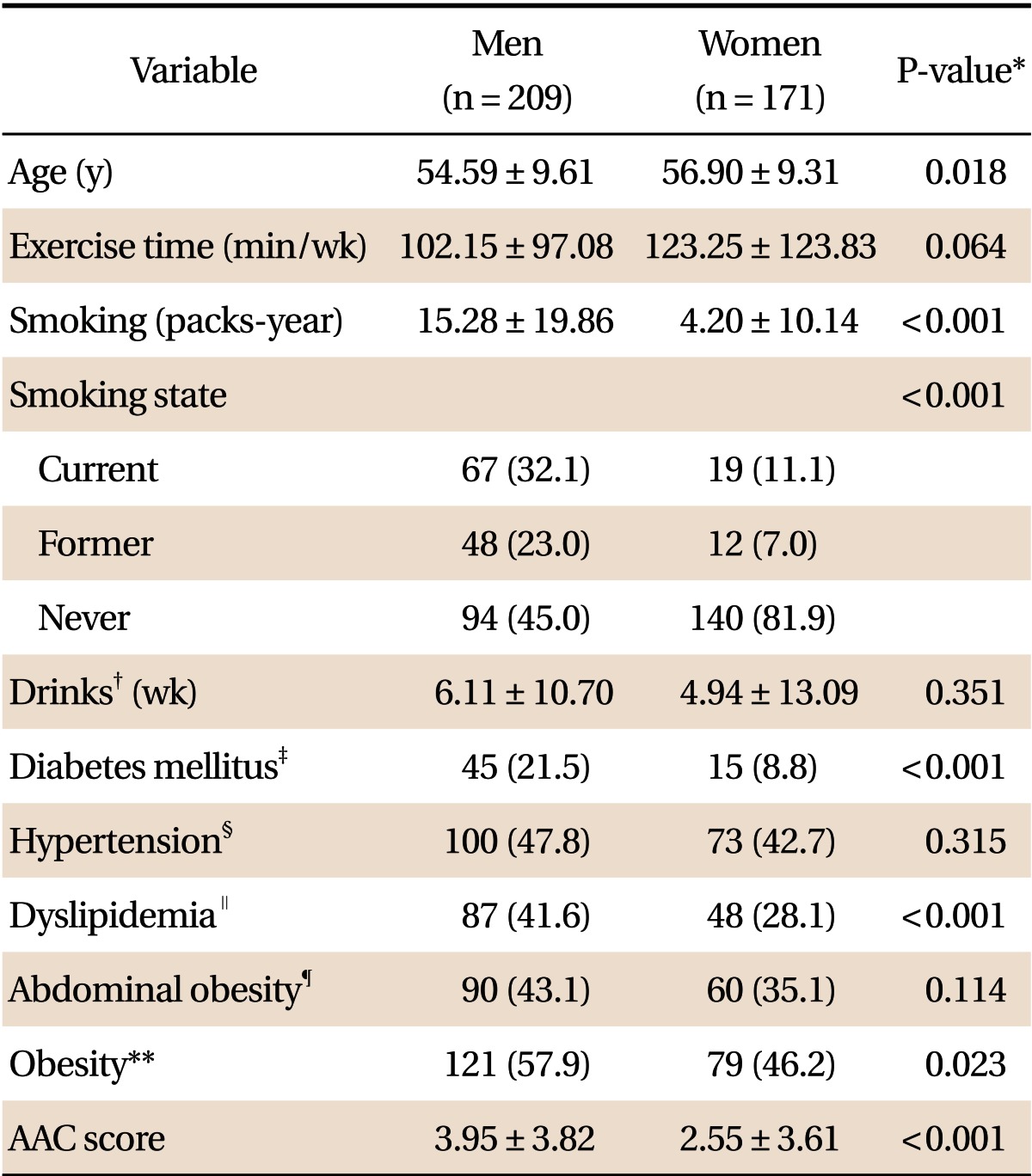
Values are presented as mean ± SD or number (%).
AAC score: abdominal aortic calcification score.
*By independent samples t-test or chi-square test. †One drink was considered to be 14 g of alcohol. ‡Diabetes mellitus was defined as fasting blood sugar level ≥ 126 mg/dL or use of anti-diabetic medication. §Hypertension was defined as systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90 mm Hg or use of anti-hypertensive medication. ∥Dyslipidemia was defined as total cholesterol level ≥ 240 mg/dL or triglyceride level ≥ 200 mg/dL or use of anti-dyslipidemia medication. ¶Abdominal obesity was defined as waist circumference ≥ 90 cm in men or 85 cm in women. **Obesity was defined as body mass index ≥ 25 kg/m2.
2. Univariate Analysis of the Association of the Abdominal Aortic Calcification Scores with the Subjects' Characteristics
The male AAC scores were significantly positively correlated with their age (r = 0.626, P < 0.001) and smoking pack-years (r = 0.349, P < 0.001) and significantly negatively correlated (r = -0.406, P < 0.001) with their weekly exercise time. The female AAC scores were positively correlated only with their age (r = 0.679, P < 0.001) and also significantly negatively correlated with their weekly exercise time (r = -0.391, P < 0.001). The male AAC scores were significantly high in the presence of dyslipidemia (P < 0.001), whereas the female AAC scores were significantly high in the presence of abdominal obesity (P < 0.001), hypertension (P < 0.001), diabetes (P < 0.001), and dyslipidemia (P < 0.001) (Table 2).
Table 2.
Relationships between abdominal aortic calcification score and characteristics of the subjects
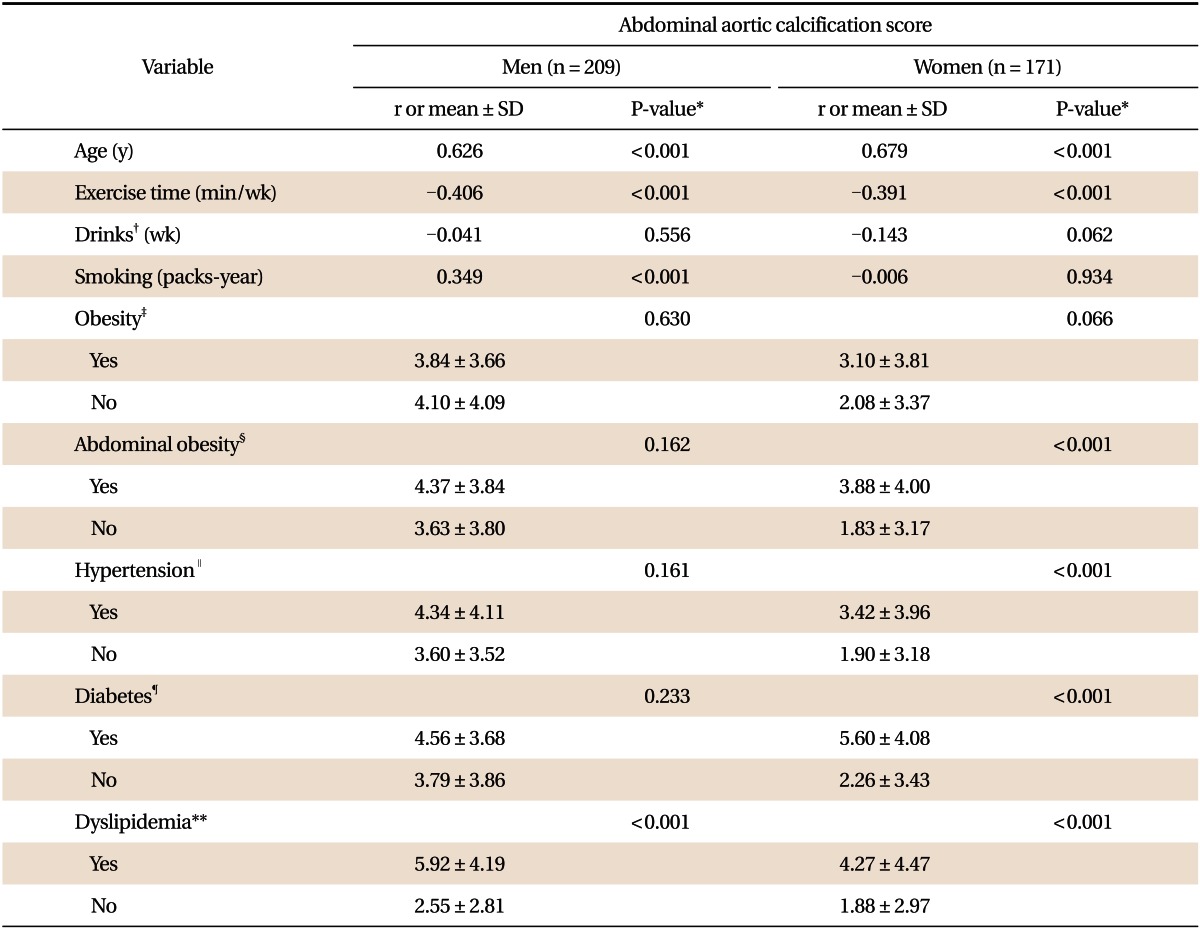
r: correlation coefficient.
*By Pearson correlation analysis or independent samples t-test. †One drink was considered to be 14 g of alcohol. ‡Obesity was defined as body mass index ≥ 25 kg/m2. §Abdominal obesity was defined as waist circumference ≥ 90 cm in men or 85 cm in women. ∥Hypertension was defined as systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90 mm Hg or use of anti-hypertensive medication. ¶Diabetes mellitus was defined as fasting blood sugar level ≥ 126 mg/dL or use of anti-diabetic medication. **Dyslipidemia was defined as total cholesterol level ≥ 240 mg/dL or triglyceride level ≥ 200 mg/dL or use of anti-dyslipidemia medication.
3. Explanatory Power of the Variables That Affected the Abdominal Aortic Calcification Score
To investigate the explanatory power (R2) of the variables that affected the AAC score, the significant variables (male: age, weekly exercise time, smoking pack-years, and dyslipidemia; and female: age, weekly exercise time, abdominal obesity, hypertension, diabetes, and dyslipidemia) obtained from the univariate analysis were set as independent variables, and the AAC score was set as the dependent variable, in a stepwise multiple linear regression analysis. The age showed the greatest explanatory power of 39.2% to the male AAC scores, followed by a high cholesterol level (10.1%), weekly exercise time (5.1%), and smoking pack-years (1.9%). The total explanatory power of these variables in male subjects was 56.3%. In female subjects, their age showed the greatest explanatory power of 46.1% to their AAC scores, followed by their weekly exercise time (2.6%), diabetes (2.2%), hypertension (2.3%), and high cholesterol level (1.5%). The total explanatory power of these variables in female subjects was 54.7% (Table 3).
Table 3.
Multiple linear regression analysis of characteristics of subjects on the abdominal aortic calcification score
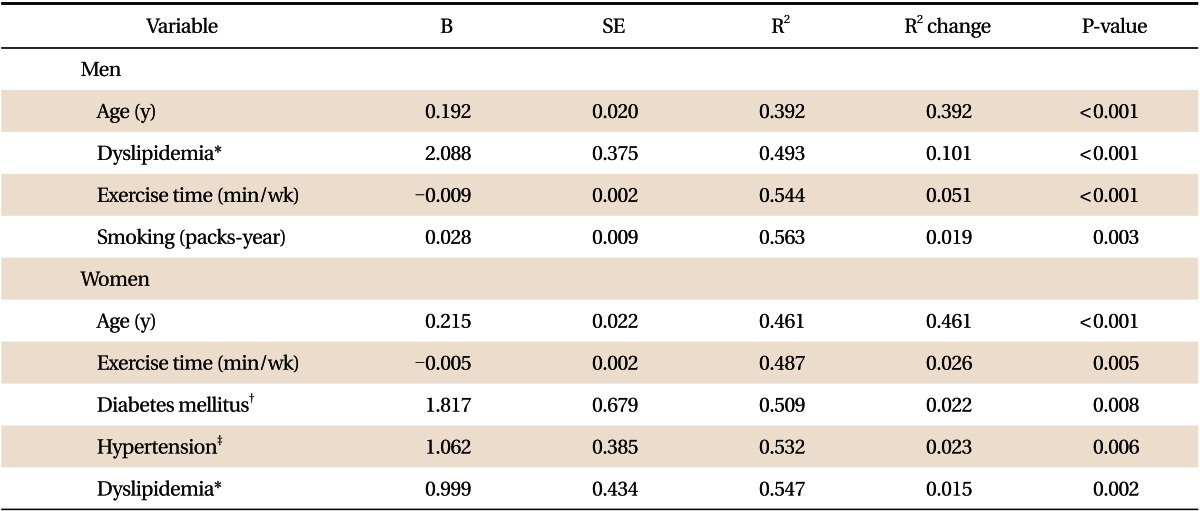
B: unstandardized regression coefficient, R2: explanatory power of variables on abdominal aortic calcification score, R2 change: explanatory power of a single variable on abdominal aortic calcification score.
*Dyslipidemia was defined as total cholesterol level ≥ 240 mg/dL or triglyceride level ≥ 200 mg/dL or use of anti-dyslipidemia medication. †Diabetes mellitus was defined as fasting blood sugar level ≥ 126 mg/dL or use of anti-diabetic medication. †Hypertension was defined as systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90 mm Hg or use of anti-hypertensive medication.
DISCUSSION
The present study investigated the association of the AAC score with lifestyle factors such as exercise, obesity, smoking and drinking, general subject characteristics, and the risk factors of cardiovascular disease. Both in the male and female subject groups, the age, dyslipidemia, and weekly exercise time showed an association with the AAC score. In addition, an association of the AAC score with smoking amount was confirmed in the male subjects, and with diabetes and hypertension, in the female subjects.
The association of blood vessel calcification with age shown in the current study was consistent with the results of previous studies.7,16) As with the results of such studies, AAC was most associated with age in the middle-age group. Also the finding that dyslipidemia was related to the AAC score in the present study correspond well with that of the study of Allison et al.,17) and support earlier studies which reported that dyslipidemia-induced atherosclerosis causes blood vessel calcification.1,2)
According to Blair et al.,18) exercise could reduce the risk of cardiovascular disease. Also, in our study, a negative correlation between the AAC score and weekly exercise time was suggested. Exercise has been known to increase the HDL level, decrease low density lipoprotein (LDL) level, reduce triglycerides level, and inhibit the hazardous effects of catecholamine in the cardiac muscle.19) To our knowledge, no previous studies exist on the association between exercise and AAC. However, considering the merits of exercise, its negative correlation with the AAC score seems to be something that can be taken for granted.
In smokers, cardiovascular disease has been known to develop four times more often than in non-smokers, and the risk of coronary artery disease is three times higher.20) In this study, however, the smoking amount in the female group did not show a positive correlation with the AAC score. According to the study of Jee et al.,21) the smoking rates of Koreans are as follows: in males, 23.0% are former smokers and 56.9% are current smokers; and in females, 2.5% are former smokers and 5.4% are current smokers. Also, in the present study, the smoking rates of females (7.0% former smokers and 11.1% current smokers) are very low as compared to the rates of males (23.0% former smokers and 32.0% current smokers). These findings mean that the smoking rates in the female subjects were too low to show any association between smoking amounts with their AAC score. However, the results of our study seems to be similar to those of a previous study which reported that, among Chinese people who had a low smoking rate, smoking was not associated with AAC, unlike in other ethnic groups.16) The findings of the present study that the male smoking amount was associated with the AAC score corresponds well with that of earlier studies.7,16,22)
According to this study, diabetes and hypertension in female subjects were associated with their AAC scores. These results are consistent with those of previous studies.7,16,22,23) In the male subjects, however, no such association was observed. It may be a result of the measurement deviations: diabetes and hypertension were defined in this study through only one blood test and blood pressure measurement, or based on histories of the diseases. In addition, 21.5% of male subjects were recognized as diabetic and 47.8%, as hypertensive, which is higher than average among Korean males. In previous studies, diabetes was associated with AAC, and hypertension was associated with AAC when systolic blood pressure was high.23) In the present study, the association between AAC and systolic or diastolic blood pressure was not analyzed in detail, so comparison of the current study with the previous studies in this regard would be inappropriate.
What, then, is the clinical implication of AAC? When atherosclerosis occurs due to any cause, atheroma is formed on the blood vessel wall and then detaches from it, blocking the blood vessel, which results in the development of cardiocerebrovascular disease. In the beginning, only atheroma is formed; but with the passage of time, most of the atheroma is calcified, and the calcified lesion can easily be detected with plain radiography.24) Once abdominal aorta calcification develops, extensive atherosclerosis is observed in other areas of the blood vessels, as confirmed in many autopsy studies.25) Blood vessels tend to be easily calcified if there is a large amount of fat mass with poor fat-free mass, though the cause of such a phenomenon is unknown.25,26) A study reported that a reduced lumbar bone density is associated with calcified atherosclerosis,27) and another study suggested that oxidized LDL cholesterol inhibits the differentiation of osteoblasts and promotes the calcification of smooth muscle cells in the blood vessels.28) These results support the association of AAC with cardiovascular disease. According to a recent meta-analysis, AAC increases the risk of all cardiovascular disease by 1.6 times.29) These results also describe the clinical implications of AAC.
The limitations of the present study are as follows. First, this study is a cross-sectional study that suggests the association of the AAC with lifestyle and the risk factors of cardiovascular disease, but not their causal relationship. Second, the AAC scores in the male and female groups differed, but this difference could not be clarified due to the lack of history taking for menopause or measurement for hormone level. A further study on female hormone and blood vessel calcification may be needed. Third, the subjects' eating habits were not evaluated. Fourth, though many studies have reported the association of AAC with atherosclerosis,23-29) the level of abdominal aortic atherosclerosis was not directly measured in our study and instead, only the AAC findings. Fifth, the exercise time investigated in the present study was determined from the self-administered questionnaire, without subcategories such as the exercise types and strengths. Accordingly, it is difficult to know what and how the exercise contributed to the AAC reduction.
Despite these limitations, our study is still meaningful because it suggests that the AAC score, which is an independent risk factor for cardiac and cerebrovascular diseases, was associated with age, presence of dyslipidemia, and weekly exercise time in both the male and female groups, with the smoking amount in the male group, and with the presence of diabetes and hypertension in the female group.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Bolick LE, Blankenhorn DH. A quantitative study of coronary arterial calcification. Am J Pathol. 1961;39:511–519. [PMC free article] [PubMed] [Google Scholar]
- 2.Wexler L, Brundage B, Crouse J, Detrano R, Fuster V, Maddahi J, et al. Writing Group. Coronary artery calcification: pathophysiology, epidemiology, imaging methods, and clinical implications: a statement for health professionals from the American Heart Association. Circulation. 1996;94:1175–1192. doi: 10.1161/01.cir.94.5.1175. [DOI] [PubMed] [Google Scholar]
- 3.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation. 1995;92:2157–2162. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 4.Simon A, Giral P, Levenson J. Extracoronary atherosclerotic plaque at multiple sites and total coronary calcification deposit in asymptomatic men: association with coronary risk profile. Circulation. 1995;92:1414–1421. doi: 10.1161/01.cir.92.6.1414. [DOI] [PubMed] [Google Scholar]
- 5.Stamler J, Neaton JD. The Multiple Risk Factor Intervention Trial (MRFIT): importance then and now. JAMA. 2008;300:1343–1345. doi: 10.1001/jama.300.11.1343. [DOI] [PubMed] [Google Scholar]
- 6.Iribarren C, Sidney S, Sternfeld B, Browner WS. Calcification of the aortic arch: risk factors and association with coronary heart disease, stroke, and peripheral vascular disease. JAMA. 2000;283:2810–2815. doi: 10.1001/jama.283.21.2810. [DOI] [PubMed] [Google Scholar]
- 7.Oei HH, Vliegenthart R, Hofman A, Oudkerk M, Witteman JC. Risk factors for coronary calcification in older subjects. The Rotterdam Coronary Calcification Study. Eur Heart J. 2004;25:48–55. doi: 10.1016/j.ehj.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Wilson PW, Kauppila LI, O'Donnell CJ, Kiel DP, Hannan M, Polak JM, et al. Abdominal aortic calcific deposits are an important predictor of vascular morbidity and mortality. Circulation. 2001;103:1529–1534. doi: 10.1161/01.cir.103.11.1529. [DOI] [PubMed] [Google Scholar]
- 9.Sun WY, Jang LC. Calcification in the abdominal aorta and common iliac artery. J Korean Soc Vasc Surg. 2008;24:94–100. [Google Scholar]
- 10.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 13.Park H. Cut-off values of waist circumference for abdominal obesity among Koreans. J Korean Med Assoc. 2005;48:1165–1172. [Google Scholar]
- 14.Park HS, Cho SI, Song YM, Sung J. Multiple metabolic risk factors and total and cardiovascular mortality in men with low prevalence of obesity. Atherosclerosis. 2006;187:123–130. doi: 10.1016/j.atherosclerosis.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 15.Lockhart ME, Robbin ML, McNamara MM, Allon M. Association of pelvic arterial calcification with arteriovenous thigh graft failure in haemodialysis patients. Nephrol Dial Transplant. 2004;19:2564–2569. doi: 10.1093/ndt/gfh414. [DOI] [PubMed] [Google Scholar]
- 16.Allison MA, Budoff MJ, Nasir K, Wong ND, Detrano R, Kronmal R, et al. Ethnic-specific risks for atherosclerotic calcification of the thoracic and abdominal aorta (from the Multi-Ethnic Study of Atherosclerosis) Am J Cardiol. 2009;104:812–817. doi: 10.1016/j.amjcard.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allison MA, Criqui MH, Wright CM. Patterns and risk factors for systemic calcified atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24:331–336. doi: 10.1161/01.ATV.0000110786.02097.0c. [DOI] [PubMed] [Google Scholar]
- 18.Blair SN, Kohl HW, 3rd, Barlow CE, Paffenbarger RS, Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. JAMA. 1995;273:1093–1098. [PubMed] [Google Scholar]
- 19.Fox CS, Hwang SJ, Massaro JM, Lieb K, Vasan RS, O'Donnell CJ, et al. Relation of subcutaneous and visceral adipose tissue to coronary and abdominal aortic calcium (from the Framingham Heart Study) Am J Cardiol. 2009;104:543–547. doi: 10.1016/j.amjcard.2009.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tolley HD, Crane L, Shipley N National Cancer Institute, editors. Strategies to control tobacco use in the United States: a blueprint for public health action in the 1990's [Internet] Bethesda: National Institutes of Health, National Cancer Institute; 1991. [cited 2012 Aug 16]. Smoking prevalence and lung cancer death rates. Available from: http://cancercontrol.cancer.gov/tcrb/monographs/1/index.html. [Google Scholar]
- 21.Jee SH, Samet JM, Ohrr H, Kim JH, Kim IS. Smoking and cancer risk in Korean men and women. Cancer Causes Control. 2004;15:341–348. doi: 10.1023/B:CACO.0000027481.48153.97. [DOI] [PubMed] [Google Scholar]
- 22.Wong ND, Lopez VA, Allison M, Detrano RC, Blumenthal RS, Folsom AR, et al. Abdominal aortic calcium and multisite atherosclerosis: the Multiethnic Study of Atherosclerosis. Atherosclerosis. 2011;214:436–441. doi: 10.1016/j.atherosclerosis.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jensky NE, Criqui MH, Wright MC, Wassel CL, Brody SA, Allison MA. Blood pressure and vascular calcification. Hypertension. 2010;55:990–997. doi: 10.1161/HYPERTENSIONAHA.109.147520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW. New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis. 1997;132:245–250. doi: 10.1016/s0021-9150(97)00106-8. [DOI] [PubMed] [Google Scholar]
- 25.Solberg LA, Strong JP. Risk factors and atherosclerotic lesions: a review of autopsy studies. Arteriosclerosis. 1983;3:187–198. doi: 10.1161/01.atv.3.3.187. [DOI] [PubMed] [Google Scholar]
- 26.Jensky NE, Criqui MH, Wright CM, Wassel CL, Alcaraz JE, Allison MA. The association between abdominal body composition and vascular calcification. Obesity (Silver Spring) 2011;19:2418–2424. doi: 10.1038/oby.2011.70. [DOI] [PubMed] [Google Scholar]
- 27.Hyder JA, Allison MA, Criqui MH, Wright CM. Association between systemic calcified atherosclerosis and bone density. Calcif Tissue Int. 2007;80:301–306. doi: 10.1007/s00223-007-9004-6. [DOI] [PubMed] [Google Scholar]
- 28.Parhami F, Morrow AD, Balucan J, Leitinger N, Watson AD, Tintut Y, et al. Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation: a possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol. 1997;17:680–687. doi: 10.1161/01.atv.17.4.680. [DOI] [PubMed] [Google Scholar]
- 29.Bastos Goncalves F, Voute MT, Hoeks SE, Chonchol MB, Boersma EE, Stolker RJ, et al. Calcification of the abdominal aorta as an independent predictor of cardiovascular events: a meta-analysis. Heart. 2012;98:988–994. doi: 10.1136/heartjnl-2011-301464. [DOI] [PubMed] [Google Scholar]


