Abstract
Context:
It is often difficult to find an adenoma in patients with Cushing's disease (CD) whose preoperative magnetic resonance imaging (MRI) is normal. Better localizing modalities are needed.
Objective:
The aim of this study was to determine the accuracy of inferior petrosal sinus sampling (IPSS) in predicting adenoma lateralization.
Design and Setting:
We conducted a prospective observational study at a tertiary care clinical research center.
Patients:
A total of 501 consecutive patients (363 female) with confirmed ACTH adenomas and IPSS were included.
Main Outcome Measure:
We measured the accuracy of IPSS to predict the intrasellar location of an adenoma.
Results:
IPSS confirmed a pituitary source of ACTH secretion in 491 patients (98%). All 10 patients with false-negative results had peak IPSS ACTH concentrations (before or after CRH) of < 400 pg/ml. Interpetrosal (side-to-side) ratios were ≥ 1.4 in 491 patients (98%). This ratio correctly predicted lateralization in 273 of 396 patients (positive predictive value = 69%) with a lateral adenoma. Left-sided IPSS lateralization (P = .008) and consistent lateralization before and after CRH administration (P = .02) were associated with enhanced accuracy. When positive, preoperative MRI correlated with adenoma location in 171 of 201 patients (positive predictive value = 86%).
Conclusions:
Potential false-negative results, the most common type of diagnostic error with IPSS for the differential diagnosis of CS, can be identified by peak IPSS ACTH values < 400 pg/ml. When MRI is normal, IPSS can be used to guide surgical exploration in patients with negative preoperative imaging. However, because of the limited accuracy of lateralization, thorough exploration of the pituitary gland is required when an adenoma is not readily discovered based on predicted location.
Bilateral simultaneous inferior petrosal sinus sampling (IPSS) is used: 1) as an aid in the differential diagnosis of Cushing's syndrome; and 2) to indicate which side of the pituitary contains an adenoma in patients with Cushing's disease (CD). It is a standard part of the diagnostic paradigm in patients with presumed CD who have either inconclusive biochemical testing or negative magnetic resonance (MR) imaging (MRI) of the pituitary gland (1–3). IPSS is performed with bilateral simultaneous samples drawn from each inferior petrosal sinus, which permits direct comparison of ACTH concentrations from the left and right petrosal sinuses. Although the test occasionally yields diagnostic errors, almost all the errors have been false-negative results—the absence of a diagnostic inferior petrosal sinus to peripheral ACTH gradient (IPS:P) in a patient with CD.
Previous data suggest that side-to-side contemporaneous differences in ACTH concentration during venous sampling may be used to predict the location of the adenoma within the pituitary (the side of the gland containing a microadenoma) and can be used to guide surgical treatment in MR-negative cases. Prior studies report that an IPS:P ACTH gradient of at least 1.4 between the inferior petrosal sinuses can be used to predict lateralization of a microadenoma in patients with CD (1, 4–9). However, these studies have not defined precisely the lateralization accuracy of IPSS because most comprised a small series of patients, and some series included patients without immunohistochemical confirmation of an adenoma (6, 8). To determine the intrapituitary lateralization accuracy of IPSS, we prospectively studied CD patients with immunohistochemically confirmed ACTH-secreting adenomas from a single center.
Patients and Methods
Patient inclusion
In this prospective observational study, consecutive pediatric and adult CD patients who underwent IPSS and transsphenoidal surgery and who had immunohistological confirmation of an ACTH-secreting adenoma at the National Institutes of Health (NIH) were included. All patients, or their legal guardians, signed informed consent for evaluation and treatment under institutional review board-approved protocols.
Imaging evaluation
The imaging techniques used to identify a pituitary tumor changed during the study. Contrast-enhanced computed tomography imaging was used from 1982 to 1986. MRI with and without gadolinium contrast enhancement with standard spin echo sequences was used from 1983 to the present. From 1997, spoiled gradient recalled acquisition sequences were added (10). The MR study was considered negative if no adenoma was visible and was classified as positive if a discrete lesion was evident on preoperative review by either the neurosurgeon or the neuroradiologist.
Laboratory evaluation
Patients underwent routine preoperative endocrinological testing to: 1) establish the presence of hypercortisolism; 2) define the hypercortisolism as ACTH-dependent; and 3) localize ACTH secretion to a pituitary source (2, 3). After an initial investigation of the diagnostic accuracy of IPSS (1), patients underwent IPSS if they had negative pituitary imaging or if the results of noninvasive endocrinological evaluation were inconclusive (conflicting results from the overnight high-dose dexamethasone suppression test and the CRH stimulation test).
ACTH was originally assayed by RIA at the Hazleton/Covance Laboratories (Vienna, Virginia). Subsequently, the method was revised to use Nichols IRMA ACTH assay kit (Nichols Institute, San Clemente, California) at the Hazleton/Covance Laboratories. After January 2000, ACTH was measured at the NIH Clinical Center, initially by Nichols Advantage chemiluminescent kit (Nichols Institute) as previously described (11). After September 2005, ACTH was measured by a chemiluminescence immunoassay on Siemens Immulite 2500 analyzer (Siemens Healthcare Diagnostics, Inc., Tarrytown, New York). A systematic comparison of values of ACTH measured with these different assays indicated close correlation between them, although the immunoradiometric and immunochemiluminometric assays yielded slightly lower concentrations than RIA (11). No attempt was made to normalize the results for the calculations in the current report.
IPSS procedure
IPSS was performed as previously described (12). Briefly, the bilateral femoral veins were cannulated, and catheters were advanced into the inferior petrosal sinuses bilaterally. Retrograde venography was performed to assess for anatomic anomaly and catheter positioning. Simultaneous samples were obtained from the right petrosal sinus, left petrosal sinus, and peripheral venous blood at 2 time points before and at 3, 5, and 10 minutes after ovine CRH (1 μg/kg up to 100 μg maximal dose) was administered iv. Samples were assayed for ACTH concentration.
IPSS analysis
Diagnosis
ACTH ratios of the left and right inferior petrosal sinus sample to the peripheral venous blood sample were calculated (IPS:P) at each time point. IPSS was considered diagnostic for a pituitary source of ACTH production if the peak basal ratio (peak ratio before CRH administration) was greater than 2.0 or if the peak ratio after CRH administration was greater than 3.0 (1).
Adenoma lateralization
The interpetrosal gradient ratios were calculated between the 2 petrosal sinus samples at each available time point. This ratio was considered predictive of lateralization if it was at least 1.4 (1, 4). Nondiagnostic results for CD occurred in 10 patients, and these patients were included for interpetrosal sinus gradient analysis if their gradient was ≥ 1.4.
Surgical procedure
Patients underwent a transsphenoidal approach to the pituitary gland, as previously described (13). When possible, adenomas were removed using the histological pseudocapsule as a surgical capsule. Identified adenomas were characterized intraoperatively based on the location of the epicenter of the adenoma (on the midline or to 1 side of the midline). For the purposes of determining lateralization of an adenoma, a tumor was considered right- or left-sided if its epicenter at surgery was off the midline; it was considered midline if its epicenter was directly on the midline. Larger adenomas that occupied both sides of the pituitary gland were considered bilateral. If no adenoma was identified after thorough inspection of the gland, a partial hypophysectomy was performed, and the location of the resected tissue was recorded. The decision of where to perform a partial hypophysectomy was made by a combination of intraoperative findings, preoperative imaging findings, and an IPSS lateralization gradient, when present. If multiple tissue specimens were resected, their locations were recorded, and each specimen was individually assessed for an ACTH-positive adenoma. Thus, adenoma location could be correlated with the location of the resected tissue. Surgical findings were recorded in a diagram immediately after every case.
Histological analysis
Resected specimens including adenoma or hypophysectomy pituitary tissue were analyzed using routine hematoxylin and eosin staining, as well as reticulin and ACTH immunohistochemistry.
Statistical analysis
Statistical analysis was performed using SPSS Statistics 19 software (IBM Corporation, Somers, New York). Variables were analyzed for impact on test accuracy using binary logistic regression for each individual variable. Measureable variable means were compared with the Mann-Whitney test. For all statistical tests, a P value less than .05 was considered significant.
The positive predictive value (PPV) for the interpetrosal gradient and MRI was calculated as follows: number of true positive results for test/[number of true positive + false-positive results for the test].
Results
Patient characteristics
A total of 501 consecutive patients treated at the NIH between 1982 and 2011 who underwent IPSS and who had immunohistochemical confirmation of an ACTH-secreting adenoma after resection were included. A total of 363 patients (72%) were female, 138 patients (28%) were male; 392 patients (78%) were adults (age greater than 21 y at time of surgery), and 109 (22%) were pediatric patients. These pediatric patients represent the immunohistochemically confirmed subset of those undergoing IPSS that are reported in our published pediatric CD series (14). Seventy-two patients (14%) had undergone prior transsphenoidal surgery at an outside institution, and 429 patients (86%) had their initial surgery at the NIH. Mean age at the time of IPSS was 34.4 ± 14.4 (range, 5.8 to 77.2) years. Mean interval between IPSS and surgery was 1.9 ± 3.0 months (range, 1 d to 42.8 mo). MRI was performed on 473 patients (94%) and demonstrated an adenoma in 201 patients (42%).
IPSS results
Venographic findings
Although bilateral catheterization of the inferior petrosal sinuses was successful in 496 patients (99%), 5 patients (1%) had sampling performed in the more proximal venous system, including the jugular vein just inferior to the petrosal sinus, when a very small petrosal sinus did not accommodate a catheter or plexiform venous anatomy could not be traversed to reach the petrosal sinus. Detailed reports of venography and catheter positioning were available in 443 patients (88%). Of these patients, 59 (13%) demonstrated abnormal anatomy such as a hypoplastic or grossly asymmetric size between the inferior petrosal sinuses.
Samples were obtained before and after CRH administration in 498 patients (99%), whereas 2 patients did not receive CRH, and in 1 patient only the results of samples taken after CRH were available. A total of 365 patients (73%) had samples taken at all 5 time points—2 at baseline, followed by samples at 3, 5, and 10 minutes after CRH stimulation. A total of 123 patients (25%) had results from 3 sample sets taken (because of the cost of the ACTH assays, as experience increased, the 5- and 10-min samples were drawn but were not assayed if the first 3 sets of samples provided a diagnosis), 2 at baseline followed by 1 sample at 3 minutes after CRH stimulation. Ten patients (2%) studied early in the series had additional sample sets taken at 20 and/or 30 minutes after stimulation.
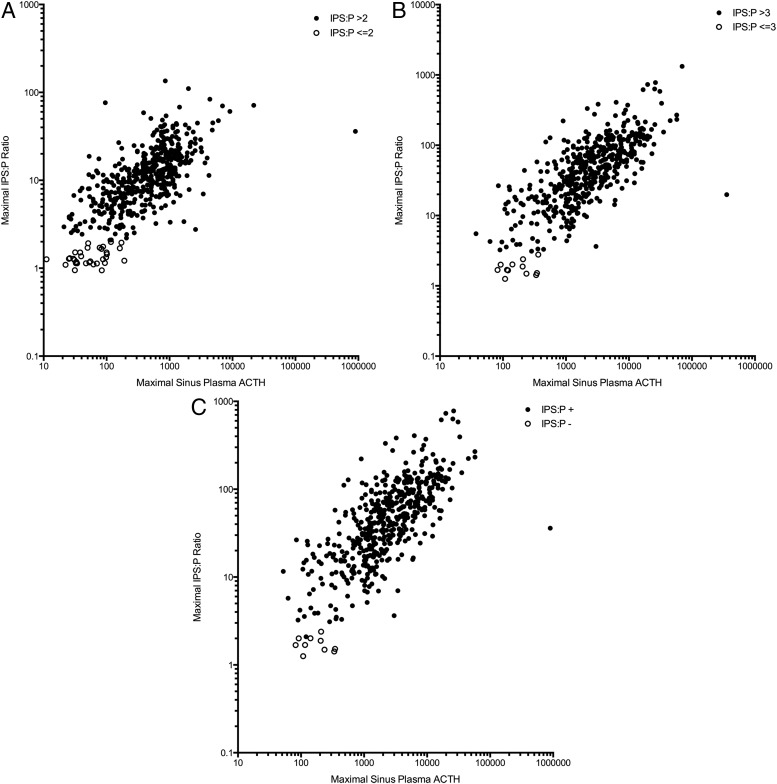
Endocrinological findings
IPSS confirmed a pituitary source of ACTH production in 491 patients (98%), including in 467 patients (93%) before CRH stimulation and in 487 patients (97%) after CRH stimulation. All 10 patients with false-negative results had peak IPSS ACTH concentrations (before or after CRH) of < 400 pg/ml, which suggests that the results of IPSS in patients who have no diagnostic IPS:P gradient for CD and peak IPS ACTH concentrations < 400 pg/ml should be interpreted with suspicion for false-negative results (Figure 1).
Figure 1.
A. Peak basal IPS:P ACTH ratio in relation to peak petrosal sinus ACTH concentration. B, Peak IPS:P ACTH ratio in relation to peak petrosal sinus ACTH concentration after CRH stimulation. C, Peak IPS:P ACTH ratio in relation to peak petrosal sinus ACTH concentration before or after CRH stimulation. Filled circles represent patients where IPSS was diagnostic for pituitary source of ACTH production, whereas empty circles represent false-negative IPSS results. All false-negative IPSS results occurred in cases where peak petrosal sinus ACTH concentrations were less than 400 pg/ml.
Interpetrosal ACTH ratios were calculated at all time points, and 6 patterns were observed: 1) consistent lateralization to 1 side before and after CRH stimulation; 2) lateralization only after CRH stimulation; 3) lateralization before CRH stimulation that disappeared after stimulation; 4) lateralization that changed to the contralateral side after CRH stimulation; 5) lateralization that oscillated between sides independent of CRH stimulation; and 6) lateralization that developed at only 1 time point during multiple time point sampling (Table 1). In cases of lateralization that changed between sides, the highest interpetrosal gradient was used for prediction of adenoma lateralization.
Table 1.
Patterns of Response to CRH Stimulation
| Response pattern to CRH stimulation | Patients, n (%) |
|---|---|
| Consistent lateralization (≥ 1.4:1) to 1 side before and after CRH administration | 381 (76) |
| Lateralization only after CRH administration | 31 (6) |
| Lateralization in basal (pre-CRH) samples only | 10 (2) |
| Lateralization that changed to the contralateral side after CRH administration | 20 (4) |
| Lateralization that changed between sides independent of CRH administration | 30 (6) |
| Lateralization that developed at only 1 time point during multi-point sampling | 16 (3) |
| No lateralization at any time point | 10 (2) |
Data are based on 498 patients (2 patients did not receive CRH stimulation, 1 patient only had values after stimulation).
Surgical results
A discrete adenoma was found within the pituitary gland in 482 patients (96%), in the pituitary stalk in 2 patients (0.4%), and in the sphenoid sinus mucosa in 1 patient (0.2%). In 16 patients (3%), no adenoma was discovered and a partial hypophysectomy (removal of 40 to 90% of the pituitary gland) was performed and contained an ACTH-adenoma at pathological analysis.
Among the 498 patients that had a solitary adenoma within the pituitary gland, the adenoma was in the right side of the gland in 189 patients (38%), in the left side in 216 patients (43%), and in the midline in 75 patients (15%). Eighteen patients (4%) had large tumors that involved the pituitary gland bilaterally and were not classified as right, left, or midline. Mean adenoma size, as measured at surgery, was 6.4 ± 3.6 (range, 1.0 to 25.0) mm. Eleven patients (2%) had a macroadenoma that was qualified as such but not measured at surgery, which combined with measured tumors with a diameter of at least 10 mm gives a total of 90 patients (18%) with a macroadenoma. Cavernous sinus invasion was identified at surgery in 131 patients (26%).
Correlation of IPSS lateralization with tumor location
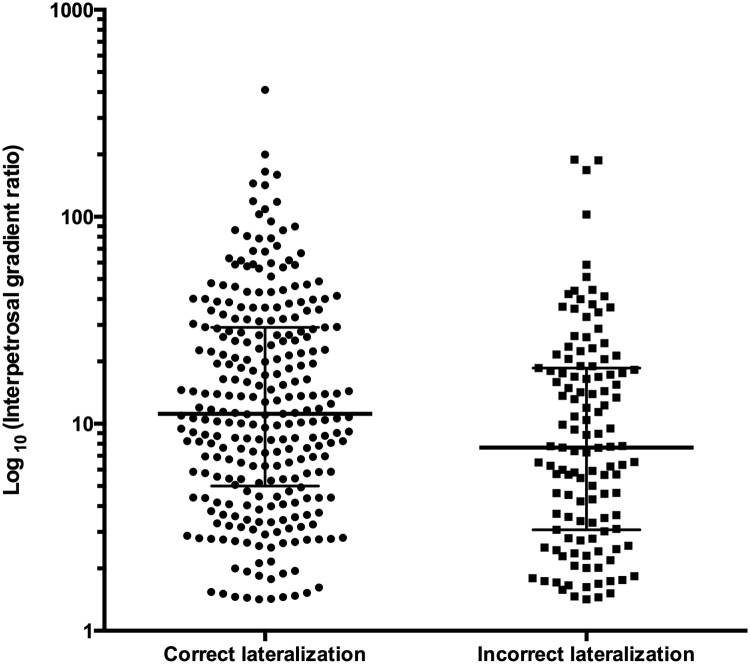
Peak interpetrosal gradient was ≥ 1.4 in 491 patients (98%). Lateralization was predicted to the right side in 285 patients (58%) and to the left side in the 206 patients (42%). In 396 patients with a lateral adenoma (an adenoma with its epicenter off the midline) and an interpetrosal gradient ≥ 1.4, IPSS correctly predicted the side of the pituitary gland that contained the tumor (PPV) in 273 patients (69%), whereas the tumor was located contralaterally in 123 patients (31%). The median peak interpetrosal ratio (side-to-side) for correctly predicted patients (11.2; interquartile range [IQR], 24.1) was significantly different (Mann-Whitney test; P = .0035) compared to incorrectly predicted patients (median, 7.7; IQR, 15.3) (Figure 2).
Figure 2.
Scatter-plot graph demonstrating distribution of interpetrosal gradient ratios in correct and incorrectly predicted lateralization. Horizontal bars represent median gradient and IQR.
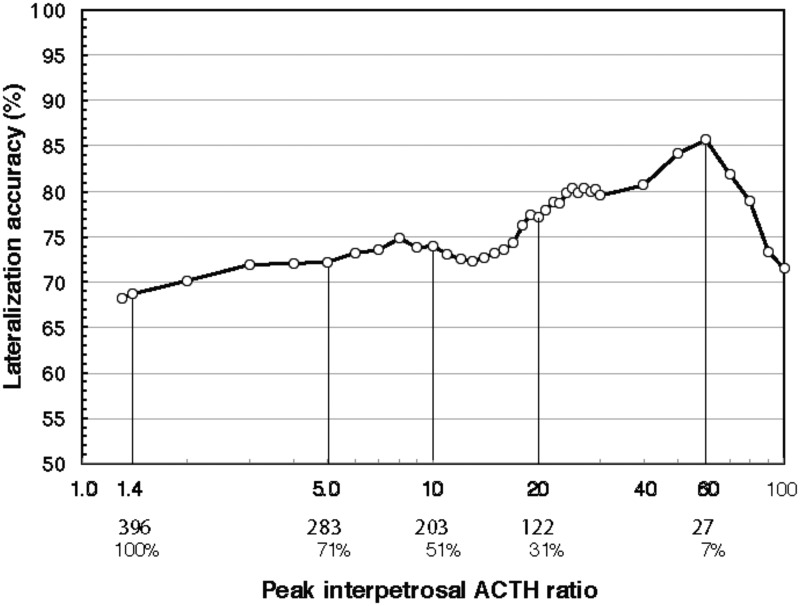
Calculation of the PPV of lateralization for predicting the side of the gland containing an ACTH-staining adenoma was performed over the range of ACTH ratios between the IPSSs (Figure 3). This demonstrates that the PPV peaks at 86% with an ACTH concentration ratio between the IPSSs of 60:1. However, the usefulness of that data is limited because only 7% of the 396 patients with a lateral adenoma reached that ratio level.
Figure 3.
Graph demonstrating the lateralization accuracy (PPV) of IPSS for predicting the side of the pituitary containing a microadenoma over the range of ratios of the ACTH concentrations between the IPSSs. Beneath the abscissa are the number and percentage of patients whose values exceeded certain ratios. Note that the best PPV occurred with ratios exceeding 60:1; however, only 7% of the patients had a ratio that high.
Subset analysis of the 10 patients that had IPS:P gradients that were not diagnostic for CD was performed for assessment of lateralization. Only 5 of these patients (50%) had an interpetrosal gradient of ≥ 1.4, and in only 2 of these 5 patients (40%) did the results of IPSS correctly predict tumor lateralization.
The results of 10 patients that had interpetrosal gradients less than 1.4 (thus not predicting lateralization) were also analyzed. One patient had a macroadenoma, with overall mean adenoma size of 6.4 ± 4.5 (range, 2.5–18.0) mm. Five adenomas were encountered in the left half of the gland, 2 on the right, 2 on the midline, with 1 adenoma in the sphenoid sinus mucosa. One patient had an adenoma with cavernous sinus invasion, and the remainder did not. Five of these patients (50%) had IPSS gradients that were not diagnostic for CD, with another 3 patients having IPSS gradients diagnostic for CD but peak IPSS ACTH concentrations of < 400 pg/ml. This further supports the conclusion that both diagnostic and lateralization results are of little value in patients with very low peak petrosal ACTH concentrations.
Factors associated with the accuracy of IPSS lateralization
Potential variables associated with IPSS lateralization accuracy were evaluated using binary logistic regression analysis (Table 2). IPSS ACTH lateralization to the left was associated with greater accuracy of predicting the side of the pituitary containing an adenoma (binary logistic regression analysis; P = .008). The accuracy of predicted lateralization was calculated for each pattern of response to CRH stimulation (Table 3). The highest accuracy was observed in patients with consistent lateralization before and after CRH stimulation (PPV = 72%). This association was statistically significant (binary logistic regression analysis; P = .02), whereas other patterns of response to CRH were not. Patient and tumor variables were also evaluated using binary logistic regression analysis for association with accurate prediction of lateralization, including patient age (both numeric as well as pediatric [<21 y old] vs adult patient status), MR-visible status on preoperative MRI assessment, adenoma size (both numeric as well as microadenoma vs macroadenoma), the presence of normal anatomy and correct catheter position, and the presence of cavernous sinus invasion, none of which was significant (Table 4).
Table 2.
IPSS Variables Associated With Accurate Lateralization Prediction
| Variable | PPV When Present | PPV When Absent | Univariate P value |
|---|---|---|---|
| Symmetric inferior petrosal sinuses and optimal catheter placement | 67% | 77% | .2 |
| Left-sided lateralization ratio | 76% | 64% | .008 |
| Median (IQR) when correct | Median (IQR) when incorrect | ||
| Peak interpetrosal gradient ratio | 11.2 (24.1) | 7.7 (15.3) | .0035 |
| Peak ACTH concentration | 2450 (5320) | 2060 (3440) | .4 |
Table 3.
PPVs of Predicted Lateralization in Patterns of Response to CRH Stimulation
| Response Pattern to CRH Stimulation | PPV, % |
|---|---|
| Consistent lateralization to 1 side before and after CRH administration | 72 |
| Lateralization only after CRH administration | 57 |
| Lateralization in basal (pre-CRH) samples only | 63 |
| Lateralization that changed to the contralateral side after CRH administration | 50 |
| Lateralization that changed between sides independent of CRH administration | 61 |
| Lateralization that developed at only 1 time point during multi-point sampling | 50 |
Table 4.
Patient Variables Associated With Lateralization Prediction
| Variable | PPV When Present, % | PPV When Absent, % | Univariate P value |
|---|---|---|---|
| Adult patient | 71 | 61 | .1 |
| MRI positivity | 73 | 65 | .1 |
| Cavernous sinus invasion | 66 | 70 | .4 |
| Lack of prior surgery | 69 | 67 | .7 |
| Adenoma size | Not applicable | Not applicable | .5 |
| Macroadenoma | 64 | 70 | .5 |
Analysis of MR-negative patients
A total of 272 patients (58%) had negative preoperative MRI. IPSS predicted lateralization (with a side-to-side gradient of at least 1.4) in 269 patients (99%). Within this patient subset, 212 patients (78%) had an adenoma with its epicenter off the midline. IPSS correctly predicted a laterally situated adenoma in 137 patients (PPV = 65%), whereas the adenoma was located in the opposite side of the pituitary gland in 75 patients (35%).
Analysis of MR-positive patients
A total of 201 patients (42%) had positive preoperative MRI. When positive, preoperative MRI correlated with adenoma location in 171 patients (PPV = 86%). Among patients with positive preoperative MRI, 160 patients (80%) had an adenoma with its epicenter off the midline. IPSS correctly predicted a laterally situated adenoma in 117 patients (PPV = 73%), whereas the adenoma was located in the opposite side of the pituitary gland in 43 patients (27%).
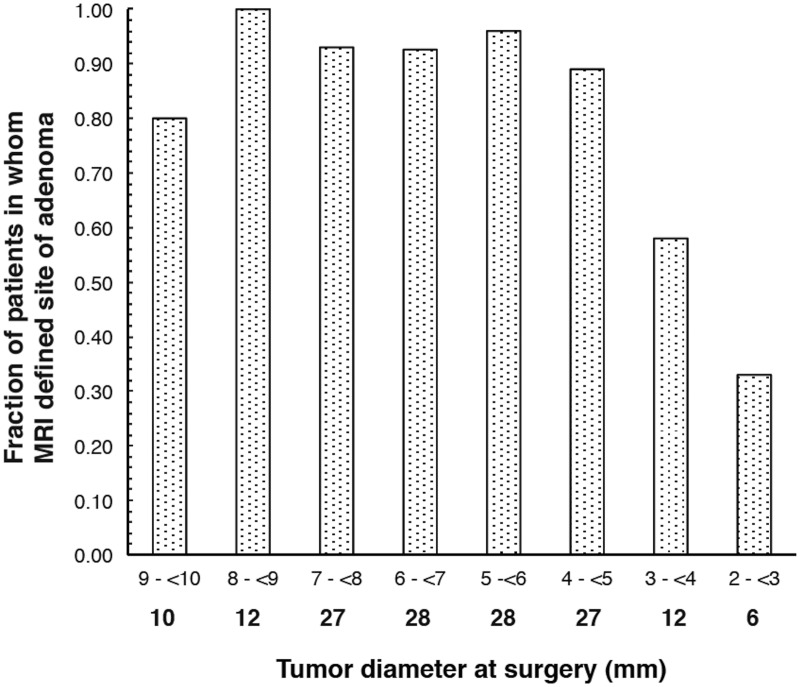
A total of 150 patients had MRIs interpreted as positive and lesions identified at surgery that were microadenomas (<10 mm maximum diameter). In the 132 patients with lesions ≥ 4 mm in diameter, the MRI was accurate in defining the site of the adenoma in 122 (92.4%). Furthermore, a positive MRI was accurate in identifying 7 of 12 lesions (58%) that were ≥ 3 to <4 mm in diameter but was accurate in only 2 of the 6 lesions < 3 mm in diameter with MRIs that were considered positive (Figure 4). Thus, MRI, when positive, was accurate in defining the site of a microadenoma in 87.3% of lesions that were < 10 mm in maximum diameter but was more accurate with adenomas 4 mm or greater in size.
Figure 4.
Column graph demonstrating the accuracy of MRI for prediction of the site of a microadenoma at surgery for microadenomas of various sizes. The numbers below the abscissa indicate the number of tumors of each size.
Discussion
Previous studies
Previous studies describe a wide range of accuracy when IPSS is used to predict lateralization of adenomas in CD (1, 4–9). Some of these studies include small patient numbers, whereas others consider lateralization to be accurate if a patient underwent remission of CD despite negative immunohistochemical analysis (6, 8). These inclusion criteria impart uncertainty to conclusions regarding the accuracy of tumor lateralization using IPSS because biochemical remission in a patient with negative immunohistochemical analysis could be due to infarction of an adenoma within remaining pituitary tissue, regardless of the accuracy of lateralization of a small microadenoma. To define the accuracy of IPSS for tumor lateralization, we analyzed a large consecutive series of CD patients with ACTH-confirmed adenomas at a single institution.
Clinical implications
False-negative results in patients with CD
The IPS:P ACTH ratio increases with peak inferior petrosal sinus ACTH concentrations, and this occurs before and after CRH, as previously observed (1). In the current study, all patients with CD and false-negative results had peak inferior petrosal sinus concentrations of ACTH that were below certain threshold values (<200 pg/ml before CRH, <400 pg/ml before or after CRH), whereas all patients diagnosed as having CD with IPSS had diagnostic peak IPS:P ratios regardless of peak IPSS concentrations of CRH. The importance of this observation is that it permits identification of patients who may have CD and a false-negative result because all of them in this set of 501 patients (10 patients [2%]) had peak inferior petrosal sinus ACTH concentrations below the thresholds indicated above.
The addition of simultaneous prolactin measurement in the samples obtained during venous sampling has been used to identify the basis of false-negative results in patients with CD (15–19). In 1 of the 10 patients with false-negative results included in the current report, prolactin concentrations were determined and the ACTH IPS:P ratios were diagnostic for CD after normalization using the prolactin concentrations (19).
Prediction of lateralization
Among patients with an interpetrosal gradient of at least 1.4:1, IPSS had a PPV for correctly identifying the side of the tumor of 69%. In comparison with MRI (when positive), IPSS was less accurate in predicting intrapituitary tumor location. MRI was positive for an adenoma in 42% of patients in this series. When MRI identified an adenoma, the imaging location of adenoma agreed with intraoperative findings in 86% of patients. The lower accuracy of IPSS compared with MRI (when positive) supports that IPSS should be reserved for cases of negative imaging or in cases of inconclusive endocrine testing. The accuracy of a positive MRI indicating the site of an adenoma identified at surgery (86%) in this series is lower than expected. This seems likely to be a reflection of the selection criteria for IPSS because patients with very small lesions on MRI, several with uncertain findings, were strongly represented in this series compared to general series of patients with CD.
Factors associated with lateralization accuracy
Multiple factors associated with IPSS have been postulated as potential sources of error in predicting tumor lateralization, including asymmetric or hypoplastic petrosal sinus anatomy (5, 6, 20) and catheter positioning (5). Analysis of the results of the current series does not demonstrate decreased lateralization accuracy in patients with asymmetric or anomalous inferior petrosal sinus anatomy at venography. The peak petrosal ACTH concentrations were not significantly associated with higher lateralization accuracy. Although a significantly higher peak interpetrosal ratio (side-to-side) occurred in correctly predicted patients compared to incorrectly predicted patients, the PPV was not high.
These limitations of lateralization, even with high peak ACTH concentrations, with high peak interpetrosal gradients, and without a clear explanation of failure based on abnormal venographic anatomy, require other explanations for why IPSS ACTH results do not provide consistently accurate lateralization. Other mechanisms such as intercavernous venous mixing or dominance in venous drainage patterns that are not evident from the anatomy displayed on venography may contribute to false-positive results.
This series demonstrates a higher rate of lateralization to the right petrosal sinus and statistically significant higher accuracy with left-sided lateralization (P = .008). This was previously evident in patients with CD (1). Prior evaluation in normal healthy patients also demonstrated asymmetric ACTH concentrations between the IPSSs, before and after CRH stimulation (21). Thus, right-sided dominance of petrosal drainage patterns may influence IPSS ACTH lateralization whether or not asymmetric anatomy is visible by venography. The higher frequency of right-sided predicted lateralization and the higher accuracy in left-sided predicted lateralization that occurred in the current study may simply be a factor of more frequent right-sided dominance of venous drainage from the pituitary.
The use of measurement of other hormones in the samples obtained during IPSS to normalize the side-to-side gradient of ACTH and improve adenoma lateralization has been examined in several studies, but the results have been inconsistent (15, 18, 22).
There has been limited analysis of the response pattern of ACTH levels and interpetrosal gradient ratios to CRH stimulation. Inconsistent lateralization to 1 side between the basal samples and in response to CRH have been previously reported (23), and those patients are also included in this series. We observed multiple response patterns to CRH stimulation; a consistent unilateral interpetrosal gradient both before and after CRH stimulation was associated with the highest accuracy of lateralization of the adenoma. Although this pattern was significantly associated with correct lateralization prediction compared to other response patterns, it reached only 72% PPV.
We analyzed the impact of multiple patient factors on lateralization accuracy. None of these factors achieved a statistically significant association with accurate lateralization prediction, including patient age or prior transsphenoidal surgery. Surprisingly, anatomic factors such as invasion of the cavernous sinus, which would place the adenoma in intimate relationship with the venous drainage system on 1 side of the pituitary, did not demonstrate increased rates of accurate lateralization prediction.
Implications for surgery
The data from this IPSS series provide critical insights into the use of IPSS lateralization to predict intrapituitary lateralization in CD patients undergoing surgical treatment. When MRI is positive, it is superior to IPSS in determining the intrapituitary location of an adenoma. Second, lateralization to 1 side from IPSS can be used to guide the initial pituitary gland exploration if the MRI is negative, but if an adenoma is not discovered, the entire pituitary gland must be thoroughly explored, as has been emphasized repeatedly in the past. Thus, lateralization of ACTH to 1 side cannot be used to guide hemihypophysectomy unless a thorough exploration of the entire gland is done because this series demonstrates that 31% of patients would harbor an untreated ACTH-secreting adenoma within the remaining gland if it were left unexplored.
Acknowledgments
We posthumously acknowledge John L. Doppman, MD, for his invaluable contributions to the development, validation, and application of inferior petrosal sinus sampling in many of these patients.
This research was supported by the Intramural Research Programs of the National Institute of Neurologic Disorders and Stroke and the Eunice Kennedy Shriver National Institute of Child Health and Development at the National Institutes of Health.
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- CD
- Cushing's disease
- IPS:P
- inferior petrosal sinus to peripheral ACTH gradient
- IPSS
- inferior petrosal sinus sampling
- IQR
- interquartile range
- MR
- magnetic resonance
- MRI
- MR imaging
- PPV
- positive predictive value.
References
- 1. Oldfield EH, Doppman JL, Nieman LK, et al. Petrosal sinus sampling with and without corticotropin-releasing hormone for the differential diagnosis of Cushing's syndrome. N Engl J Med. 1991;325:897–905 [DOI] [PubMed] [Google Scholar]
- 2. Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing's syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008;93:1526–1540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Newell-Price J, Bertagna X, Grossman AB, Nieman LK. Cushing's syndrome. Lancet. 2006;367:1605–1617 [DOI] [PubMed] [Google Scholar]
- 4. Oldfield EH, Chrousos GP, Schulte HM, et al. Preoperative lateralization of ACTH-secreting pituitary microadenomas by bilateral and simultaneous inferior petrosal venous sinus sampling. N Engl J Med. 1985;312:100–103 [DOI] [PubMed] [Google Scholar]
- 5. Lefournier V, Martinie M, Vasdev A, et al. Accuracy of bilateral inferior petrosal or cavernous sinuses sampling in predicting the lateralization of Cushing's disease pituitary microadenoma: influence of catheter position and anatomy of venous drainage. J Clin Endocrinol Metab. 2003;88:196–203 [DOI] [PubMed] [Google Scholar]
- 6. Mamelak AN, Dowd CF, Tyrrell JB, McDonald JF, Wilson CB. Venous angiography is needed to interpret inferior petrosal sinus and cavernous sinus sampling data for lateralizing adrenocorticotropin-secreting adenomas. J Clin Endocrinol Metab. 1996;81:475–481 [DOI] [PubMed] [Google Scholar]
- 7. Booth GL, Redelmeier DA, Grosman H, Kovacs K, Smyth HS, Ezzat S. Improved diagnostic accuracy of inferior petrosal sinus sampling over imaging for localizing pituitary pathology in patients with Cushing's disease. J Clin Endocrinol Metab. 1998;83:2291–2295 [DOI] [PubMed] [Google Scholar]
- 8. Liu C, Lo JC, Dowd CF, et al. Cavernous and inferior petrosal sinus sampling in the evaluation of ACTH-dependent Cushing's syndrome. Clin Endocrinol (Oxf). 2004;61:478–486 [DOI] [PubMed] [Google Scholar]
- 9. Colao A, Faggiano A, Pivonello R, Pecori Giraldi F, Cavagnini F, Lombardi G. Inferior petrosal sinus sampling in the differential diagnosis of Cushing's syndrome: results of an Italian multicenter study. Eur J Endocrinol. 2001;144:499–507 [DOI] [PubMed] [Google Scholar]
- 10. Patronas N, Bulakbasi N, Stratakis CA, et al. Spoiled gradient recalled acquisition in the steady state technique is superior to conventional postcontrast spin echo technique for magnetic resonance imaging detection of adrenocorticotropin-secreting pituitary tumors. J Clin Endocrinol Metab. 2003;88:1565–1569 [DOI] [PubMed] [Google Scholar]
- 11. Lindsay JR, Shanmugam VK, Oldfield EH, Remaley AT, Nieman LK. A comparison of immunometric and radioimmunoassay measurement of ACTH for the differential diagnosis of Cushing's syndrome. J Endocrinol Invest. 2006;29:983–988 [DOI] [PubMed] [Google Scholar]
- 12. Doppman JL, Oldfield E, Krudy AG, et al. Petrosal sinus sampling for Cushing syndrome: anatomical and technical considerations. Work in progress. Radiology. 1984;150:99–103 [DOI] [PubMed] [Google Scholar]
- 13. Oldfield EH, Vortmeyer AO. Development of a histological pseudocapsule and its use as a surgical capsule in the excision of pituitary tumors. J Neurosurg. 2006;104:7–19 [DOI] [PubMed] [Google Scholar]
- 14. Lonser RR, Wind JJ, Nieman LK, Weil RJ, Devroom HL, Oldfield EH. Outcome of surgical treatment of 200 children with Cushing's disease. J Clin Endocrinol Metab. 2013;98(3):892–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Daousi C, Nixon T, Javadpour M, Hayden K, MacFarlane IA. Inferior petrosal sinus ACTH and prolactin responses to CRH in ACTH-dependent Cushing's syndrome: a single centre experience from the United Kingdom. Pituitary. 2010;13:95–104 [DOI] [PubMed] [Google Scholar]
- 16. Findling JW, Kehoe ME, Raff H. Identification of patients with Cushing's disease with negative pituitary adrenocorticotropin gradients during inferior petrosal sinus sampling: prolactin as an index of pituitary venous effluent. J Clin Endocrinol Metab. 2004;89:6005–6009 [DOI] [PubMed] [Google Scholar]
- 17. Grant P, Dworakowska D, Carroll P. Maximizing the accuracy of inferior petrosal sinus sampling: validation of the use of prolactin as a marker of pituitary venous effluent in the diagnosis of Cushing's disease. Clin Endocrinol (Oxf). 2012;76:555–559 [DOI] [PubMed] [Google Scholar]
- 18. Mulligan GB, Faiman C, Gupta M, et al. Prolactin measurement during inferior petrosal sinus sampling improves the localization of pituitary adenomas in Cushing's disease. Clin Endocrinol (Oxf). 2012;77:268–274 [DOI] [PubMed] [Google Scholar]
- 19. Sharma ST, Raff H, Nieman LK. Prolactin as a marker of successful catheterization during IPSS in patients with ACTH-dependent Cushing's syndrome. J Clin Endocrinol Metab. 2011;96:3687–3694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Doppman JL, Chang R, Oldfield EH, Chrousos G, Stratakis CA, Nieman LK. The hypoplastic inferior petrosal sinus: a potential source of false-negative results in petrosal sampling for Cushing's disease. J Clin Endocrinol Metab. 1999;84:533–540 [DOI] [PubMed] [Google Scholar]
- 21. Yanovski JA, Nieman LK, Doppman JL, et al. Plasma levels of corticotropin-releasing hormone in the inferior petrosal sinuses of healthy volunteers, patients with Cushing's syndrome, and patients with pseudo-Cushing states. J Clin Endocrinol Metab. 1998;83:1485–1488 [DOI] [PubMed] [Google Scholar]
- 22. Zovickian J, Oldfield EH, Doppman JL, Cutler GB, Jr, Loriaux DL. Usefulness of inferior petrosal sinus venous endocrine markers in Cushing's disease. J Neurosurg. 1988;68:205–210 [DOI] [PubMed] [Google Scholar]
- 23. Miller DL, Doppman JL, Nieman LK, et al. Petrosal sinus sampling: discordant lateralization of ACTH-secreting pituitary microadenomas before and after stimulation with corticotropin-releasing hormone. Radiology. 1990;176:429–431 [DOI] [PubMed] [Google Scholar]