Abstract
Granuloma annulare (GA) is a disease characterized by granulomatous inflammation of the dermis. A variant form of the disease, generalized granuloma annulare (GGA), can be observed in 15% of affected patients. Localized GA is likely to resolve spontaneously within months or a few years, whereas GGA can persist for decades. There are various therapies for treating GGA. Monthly combination therapy of rifampicin 600 mg, ofloxacin 400 mg, and minocycline 100 mg (ROM) is used for treating paucibacillary leprosy which shares both clinical and histopathologic similarities with GA. Therefore, we decided to evaluate the possible efficacy of monthly ROM in a patient with GGA.
Keywords: Granuloma annulare, monthly ROM for granuloma annulare, treatment of granuloma annulare
Introduction
What was known?
Association of GGA with diabetes mellitus.
Granuloma annulare (GA) is a benign, usually self-limited dermatosis of unknown cause, characterized by necrobiotic dermal papules that often assume an annular configuration. Although localized GA is most common, the generalized variant of the disease accounts for 15% of all cases. In generalized granuloma annulare (GGA), hundreds or even thousands of individual 1-2 mm, usually skin-colored papules arise on the cutaneous surface and may form small annular plaques. In contrast to the other forms, GGA usually involves the trunk, and lesions are especially common on the neck, forearms, legs, and extensor surfaces of the elbows. Diabetes has been reported to occur in up to 20% of cases. GGA differs from the localized form by a later age of onset, protracted course with only rare spontaneous resolution, poor response to therapy,[1] and increased prevalence of HLA Bw 35.[2]
Case Report
A 52-year-old woman presented with complaints of multiple asymptomatic skin-colored raised lesions on the trunk and extremities of 6 months duration, which were insidious in onset and progressive in nature, with the last lesion appearing 1 month back. Patient was a diagnosed case of Type 2 diabetes mellitus (DM) and rheumatoid arthritis (RA) since 2008, for which she was on regular treatment with tablet metformin 500 mg TDS, tablet glimipride 1 mg daily, tablet hydroxychloroquine 200 mg BD, tablet methotrexate 5-7.5 mg per week (total cumulative dose of methotrexate till now being 1300 mg), and tablet folic acid 5 mg taken daily except on the days of taking methotrexate. There was no history of photosensitivity.
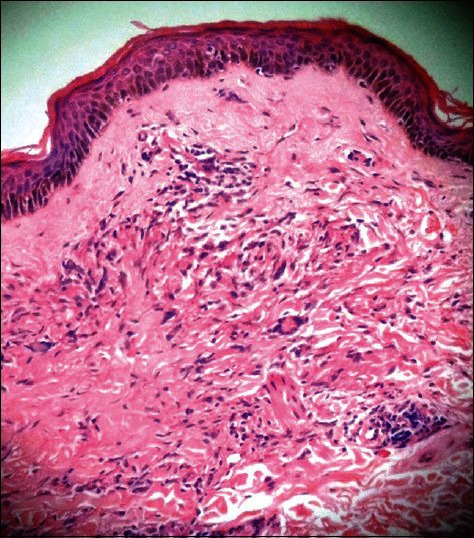
Dermatological examination revealed the presence of multiple well-defined skin-colored to slightly erythematous papules coalescing to form well-defined plaques, few being annular in configuration, present on the flexor aspect of right forearm near the elbow joint, flexor and extensor aspects of left forearm near the elbow joint [Figure 1], left upper arm, chest, and abdomen. The individual papules forming the plaques had elevated borders with depressed centers. The lesions were normoasthetic on examination. Rest of the general and systemic examinations were within normal limits.
Figure 1.

Multiple skin-colored to erythematous papules on extensor surface of left forearm
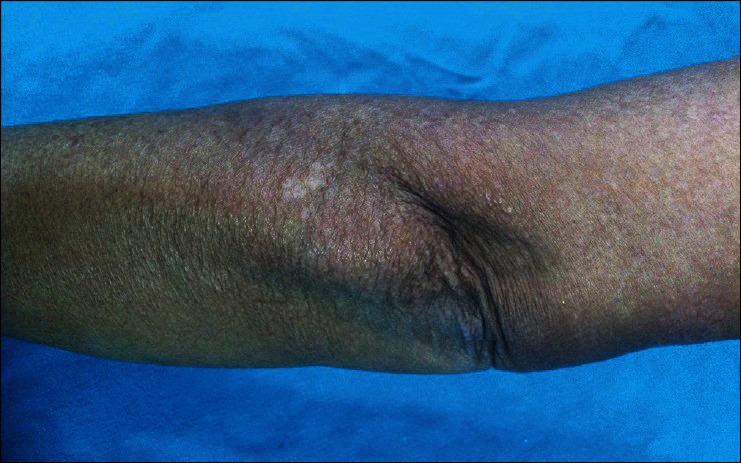
The results of her complete blood count, erythrocyte sedimentation rate, liver and kidney function tests were within normal limits. Fasting blood sugar was 95 mg/dl and postprandial blood sugar was 124 mg/dl, which were essentially within normal limits. Histopathologic examination was suggestive of GA. There was mild thinning of the epidermis with dermis showing histiocytes arranged in interstitial pattern, presence of multinucleate giant cells, and mild perivascular lymphocytic infiltrate with no collagen necrosis [Figure 2].
Figure 2.
Dermis shows histiocytes arranged in interstitial pattern, presence of multinucleate giant cells, and mild perivascular lymphocytic infiltrate (Staining: H and E stain ×10)
Based on the dermatological examination and histopathologic findings, the diagnosis of GA was made. The patient was treated with single dose of rifampicin 600 mg, ofloxacin 400 mg, and minocycline 100 mg (ROM) given once a month for 5 months. Patient tolerated the combination therapy well with no side effects. All the lesions subsided after 5 months of monthly ROM, leaving behind slight epidermal atrophy of skin at few sites [Figure 3]. There was no recurrence at 3 months of follow-up.
Figure 3.
Lesions on extensor surface of left forearm have healed, leaving behind epidermal atrophy
Discussion
GGA affects mostly women past their middle age. Diabetes has been reported to occur in up to 20% of cases. It presents as a diffuse papular eruption. Lesions are found in the nape of the neck, upper trunk, and proximal upper extremities. The face and genital area are usually spared. In some cases, sun exposure seems to be a trigger. GGA differs from the localized form by a later age of onset, protracted course with only rare spontaneous resolution, poor response to therapy,[1] and increased prevalence of HLA Bw 35.[2]
There are various treatment modalities for treating GA, including topical and systemic steroids, psoralen UV-A, isotretinoin, dapsone, pentoxifylline, hydroxychloroquine, cyclosporine, interferon gamma, chlorambucil, potassium iodide, nicotinamide, niacinamide, salicylic acid, chlorpropamide, thyroxine, dipyridamole,[3] methyl aminolevulinate photodynamic therapy,[4] fumaric esters,[5] etarnacept, infliximab, adalimumab,[6] and efalizumab.
Marcus et al. reported six patients with GA refractory to standard modality of treatment. The patients were treated with monthly ROM for 3 months. Three to five months after the initiation of treatment, the plaques cleared completely.[7]
The rationale for using monthly ROM therapy for treating GA is based on the similarities between GA and paucibacillary leprosy. The granulomatous appearance in histopathologic examination and the annular clinical appearance are common to both GA and paucibacillary leprosy. In addition, both the conditions respond to dapsone therapy and to prolonged antibiotic use.[8–10] Infections are postulated as one of the possible etiological factors for GA. Shelley reported successful treatment of GA by treating the underlying infections with antibiotics such as cefaclor, cefixime, penicillin, amoxicillin, ciprofloxacin, erythromycin, clarithromycin, and trimethoprim–sulfamethoxazole.[3]
Our patient, a known case of Type 2 DM and RA and on regular treatment, presented with GGA which was confirmed histopathologically. None of the drugs which the patient was taking for DM or RA were known to cause GA. Owing to the generalized nature of her presentation, she was treated with monthly ROM therapy for 5 months to which she responded well with complete clearance of lesions without experiencing any side effects. Considering the complete response to this modality of treatment, its safety profile, and cost-effectiveness, without the inconvenience of daily application of topical treatment, daily oral drugs, or prolonged therapy, monthly ROM seems to be a good option for treating GGA, and further studies are needed to establish the role of monthly ROM in treating GGA.
What is new?
Monthly ROM as a modality of treatment for GGA.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Dicken CH, Carrington SG, Winkelmann RK. Genearalized granuloma annulare. Arch Dermatol. 1969;99:556–63. [PubMed] [Google Scholar]
- 2.Friedman-Birnbaum R, Haim S, Gideone O, Barzilai A. Histocompatibility antigens in granuloma annulare: Comparative study of generalized and localized types. Br J Dermatol. 1978;98:425–8. [PubMed] [Google Scholar]
- 3.Shelley ED. Granuloma annulare. In: Shelley ED, Shelley WB, editors. Advanced Dermatologic Therapy. Vol. 2. Philadelphia, PA: WB Saunders Ltd; 2001. pp. 491–8. [Google Scholar]
- 4.Piaserico S, Zattra E, Linder D, Peserico A. Generalized granuloma annulare treated with methyl aminolevulinate photodynamic therapy. Dermatology. 2009;218:282–4. doi: 10.1159/000195675. [DOI] [PubMed] [Google Scholar]
- 5.Weber HO, Borelli C, Rocken M, Schaller M. Treatment of disseminated granuloma annulare with low-dose fumaric acid. Acta Derm Venereol. 2009;89:295–8. doi: 10.2340/00015555-0647. [DOI] [PubMed] [Google Scholar]
- 6.Rosmarin D, LaRaia A, Schlauder S, Gottlieb AB. Successful treatment of disseminated granuloma annulare with adalimumab. J Drugs Dermatol. 2009;8:169–71. [PubMed] [Google Scholar]
- 7.Marcus DV, Mahmoud BH, Hamzavi IH. Granuloma annular treated with rifampicin, ofloxacin, and minocycline combination therapy. Arch Dermatol. 2009;145:787–9. doi: 10.1001/archdermatol.2009.55. [DOI] [PubMed] [Google Scholar]
- 8.Steiner A, Pehamberger H, Wolff K. Sulphone treatment of granuloma annulare. J Am Acad Dermatol. 1985;13:1004–8. doi: 10.1016/s0190-9622(85)70253-8. [DOI] [PubMed] [Google Scholar]
- 9.Villahermosa LG, Fajardo TT, Jr, Abalos RM, Cellona RV, Balagon MV, Dela Cruz EC, et al. Parallel assessment of 24 monthly doses of rifampicin, ofloxicin, and minocycline versus two years of World Health Organization multi-drug therapy for multi-bacillary leprosy. Am J Trop Med Hyg. 2004;70:197–200. [PubMed] [Google Scholar]
- 10.Duarte AF, Mota A, Pereira MA, Baudrier T, Azevedo F. Generalized granuloma annulare-response to doxycycline. J Eur Acad Dermatol Venereol. 2008;23:84–5. doi: 10.1111/j.1468-3083.2008.02707.x. [DOI] [PubMed] [Google Scholar]


