Abstract
The most significant and debilitating complication of herpes zoster (HZ) is herpetic neuralgia that accompanies and may persist in 10-15% of all zoster patients, particularly those over 60 years of age. The described 3 cases had an uncommon complication of spontaneous tooth exfoliation after trigeminal HZ that rarely finds mention in dermatology literature.
Keywords: Post-herpetic complications, post-herpetic neuralgia, toothache, varicella zoster virus infection
Introduction
What was known?
The most significant and debilitating complication of herpes zoster is herpetic neuralgia that accompanies and may persist in 10-15% of all zoster patients, particularly those over 60 years of age.
Herpes zoster (HZ), a sporadic infection with an estimated lifetime risk of 10-20%, occurs in all age groups, especially among individuals who have had varicella any time in the past, but its prevalence almost doubles in each decade past the age of 50 years.[1] Individuals with immunosuppression are also more prone to it. The most significant and debilitating complication of HZ is herpetic neuralgia that accompanies and may persist in 10-15% of all zoster patients, particularly those over 60 years of age.[2] Cranial and peripheral nerve palsies, encephalitis, pneumonitis, acute retinal necrosis, encephalitis, myelitis, and secondary bacterial infection are other well-known complications of HZ. The described cases had an uncommon complication of spontaneous tooth exfoliation after trigeminal HZ, of which only about 30 cases have been reported before 2006 in the English literature.[1,3–8]
Case Reports
Case 1
This 80-year-old HIV-negative male had spontaneous loss of teeth from right upper jaw about 10 days after severe tooth pain, gingival swelling/ulceration, and cutaneous vesicular eruptions over right cheek, suggestive of HZ, for which he took analgesics only. He had few loose or missing teeth previously but not in the right upper quadrant. The skin and gingival lesions had healed in about 2 weeks, but he still had paresthesia over the right cheek. Oro-cutaneous examination [Figure 1a and b] showed hyperesthesia, scarring, and milia over right facial skin innervated by maxillary division of right trigeminal nerve, slight deviation of upper lip, and edentulous right upper alveolar ridge due total loss of teeth. There was minimal periodontitis and few missing teeth in lower jaw, but no oral lesions, gingival ulceration/necrosis, blood, purulent exudates, granulation or loose teeth were noted. X-ray of the jaw and orthopantograph (OPG) showed complete loss of teeth in right upper quadrant and no necrosis or other abnormality of the alveolar bone [Figure 1c and d]. Systemic examination, complete blood counts, serum biochemistry, urinalysis, and chest X-ray were essentially normal, and he had no other predisposing factors for immune suppression. The oral prophylaxis performed, and the patient was provided with artificial removable dentures later.
Figure 1.
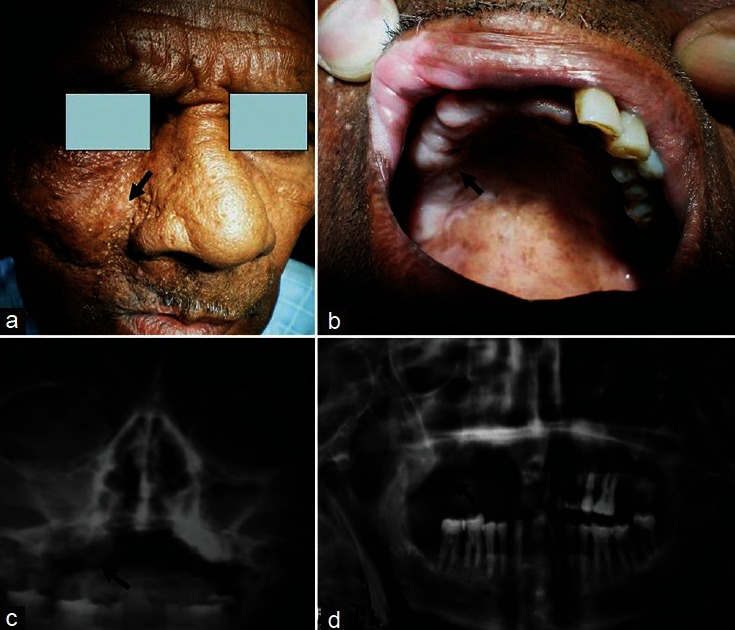
(a) Post-herpes zoster scarring and milia formation over the skin innervated by maxillary branch of right trigeminal nerve. (b) Unilateral exfoliated right upper incisors, canine, premolar, and molar teeth leaving him edentulous in right upper quadrant. (c and d) X-ray and orthopantograph show loss of teeth. No alveolar bone necrosis is noted
Case 2
This 55-year-old HIV-negative female was hospitalized for painful vesicular lesions over right cheek, right half of tongue and buccal mucosa innervated by right mandibular nerve, and corresponding gingival swelling. Although she had toothache 2 days prior to onset of skin lesions, there was no blood, purulent exudates, granulation, or loose teeth. She had mild generalized periodontitis and few missing teeth, but teeth in right lower quadrant were intact. Systemic examination, complete blood counts, serum biochemistry, urinalysis, and chest X-ray showed no abnormality, and there were no predisposing factors for immune suppression. Clinical diagnosis of HZ was made, and she was treated with intravenous acyclovir (500 mg 8 hourly/d) for initial 2 days, followed by oral acyclovir (800 mg × 5 times/d) for the next 1 week and was sent home. Oro-cutaneous examination on return visit 2 weeks later showed hyperesthesia and hyperpigmentation of facial skin over right mandibular area, slight hypo-/hyperpigmentation of lower lip, and edentulous right lower alveolar ridge due total loss of teeth [Figure 2a and b]. Orthopantograph showed complete loss of teeth in right lower quadrant and no necrosis or other abnormality of the alveolar bone [Figure 2c]. The oral prophylaxis performed. She did not return for further follow-up.
Figure 2.

(a) Post-herpes zoster hypopigmentation and hyperpigmentation over the skin innervated by mandibular branch of right trigeminal nerve. (b) Edentulous alveolus showing healing after exfoliation of all teeth in right lower quadrant. Few teeth left in left lower jaw show periodontitis and no loose teeth. (c) Orthopantograph shows total loss of right mandibular teeth but no alveolar bone necrosis
Case 3
This 45-year-old HIV-negative male presented with spontaneous loss of few teeth from right lower jaw about 3 weeks after severe gingival/tooth pain and vesiculo-ulcerative eruptions over tongue and skin over right mandibular region, suggestive of HZ. He had no loose teeth previously. The skin and gingival lesions had healed in about 2 weeks, but he still felt abnormal sensations over the healed skin eruption area. There was hyperpigmentation and hyperesthesia over right facial skin innervated by mandibular division of right trigeminal nerve, loss of right lower incisors, canine, premolar teeth, exposed portions of the empty tooth sockets in the alveolar bone, and root surfaces of the exfoliated teeth, but no loose teeth were found [Figure 3]. X-ray of the jaw showed empty sockets corresponding to lost teeth and no necrosis or other abnormality of the alveolar bone. Systemic examination, laboratory work-up, and chest X-ray were essentially normal, and there were no predisposing factors for immune suppression. The patient declined for OPG and biopsy. The exposed bone was trimmed, and oral prophylaxis performed. He did not follow-up further.
Figure 3.
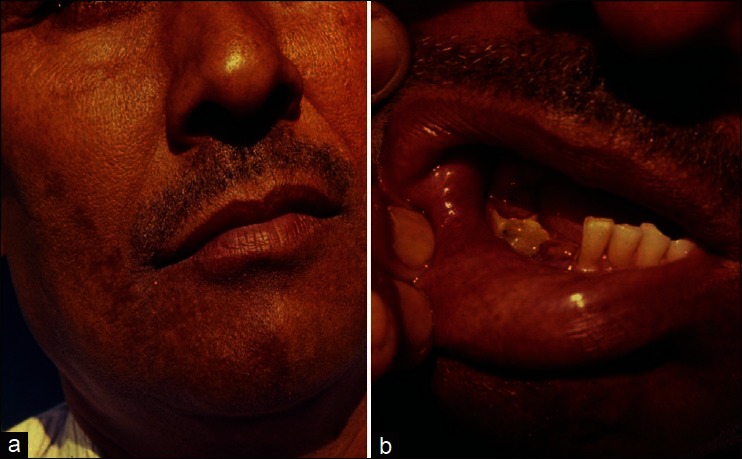
(a) Post-herpes zoster hyperpigmentation ending abruptly in the midline over the skin innervated by mandibular branch of right trigeminal nerve. (b) Unilateral empty tooth sockets from the exfoliated right lower incisors, canine, and premolar teeth ending abruptly in the midline are clearly visible. No necrosis of alveolar bone is noted.
Discussion
HZ of trigeminal nerve manifests as painful vesicular eruptions of the skin and mucosa innervated by the affected nerve division. Its major complications vary from temporary prodromal odontalgia to permanent tooth nerve damage, devitalized teeth, abnormal development of permanent teeth, root resorption, muscle paralysis, multiple ocular and ear complications, prolonged neuralgia, trigeminal trophic syndrome, and occasionally encephalitis.[3] The pain of trigeminal zoster frequently simulates toothache, not uncommonly leading to tooth extraction. Other oral complications like exfoliation of teeth and alveolar bone necrosis or osteomyelitis of maxilla or mandible have been rarely described in dermatology literature. Osteonecrosis following HZ often presents as painless exfoliation of teeth in the involved area approximately 6 weeks after the vesicular eruptions when the acute phase has subsided. The precise pathomechanism(s) of these oral complications eventually leading to tooth loss and necrosis of the alveolar bone, periodontal tissue membrane, nerve supply, and adjacent gingival tissue remain largely uncertain. The pre-existing local periodontal disease does not appear to influence the tooth loss.[4] Although the majority of the described cases are aged over 50 years, had severe HZ, were suffering from lymphoproliferative or other malignancies, HIV infection, receiving corticosteroids or chemo-/radiotherapy, the conditions well-known for increased incidence and severity of HZ, few of the reported cases have been young, immunocompetent, and otherwise healthy individuals suggesting that factors like old age, pre-existing systemic illnesses too seem not to precipitate this rare complication. It has been also postulated that it could result from intense vasoconstriction, endarteritis, or vasculitis with ischemia of the blood supply that may be caused by the virus migrating along the trigeminal neurovascular bundle. It is possible that the varicella zoster virus invades the sympathetic nerves that accompanying the blood vessels to the alveolar bone causing vasoconstriction and hampered blood supply[1] or that systemic viral infection perhaps injures odontoblasts and cause degenerative tissue changes/pulp necrosis.[3] Another plausible explanation is that by direct extension of neural inflammation and edema, the adjacent alveolar artery may get compressed in the narrow bony channels and resultant poor tissue perfusion.[5] The postulation of local vasculitis caused by varicella zoster virus leading to infarction and ischemia of the periodontal tissue and alveolar bone has limited evidence despite well-documented vascular damage it causes in the central nervous system.[3,5,7] Interestingly, early anti-viral medication too does not appear to prevent this complication as is evident in our case-2. Our patients were immunocompetent, never used tobacco, and had only minimal pre-existing local periodontal disease, suggesting that the HZ infection perhaps remains the primary determinant for exfoliation of teeth/bone necrosis. We feel that the described cases will make dermatologists aware of this rather unusual trigeminal HZ complication described mainly in the literature on oro-dental diseases.
What is new?
Spontaneous tooth exfoliation after trigeminal herpes zoster is a rare complication that rarely finds mention in dermatology literature.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.van Heerden WF, McEachen SE, Boy SC. Alveolar bone necrosis and tooth exfoliation secondary to herpes zoster in the setting of HIV/AIDS. AIDS. 2005;19:2183–4. doi: 10.1097/01.aids.0000194803.89540.a8. [DOI] [PubMed] [Google Scholar]
- 2.Araújo LQ, Macintyre CR, Vujacich C. Epidemiology and burden of herpes zoster and post-herpetic neuralgia in Australia, Asia and South America. Herpes. 2007;14:40–4. [PubMed] [Google Scholar]
- 3.Mintz SM, Anavi Y. Maxillary osteomyelitis and spontaneous tooth exfoliation after herpes zoster. Oral Surg Oral Med Oral Pathol. 1992;73:664–6. doi: 10.1016/0030-4220(92)90005-b. [DOI] [PubMed] [Google Scholar]
- 4.Wright WE, Davis ML, Geffen DB, Martin SE, Nelson MJ, Straus SE. Alveolar bone necrosis and tooth loss. A rare complication associated with herpes zoster infection of the fifth cranial nerve. Oral Surg Oral Med Oral Pathol. 1983;56:39–46. doi: 10.1016/0030-4220(83)90053-1. [DOI] [PubMed] [Google Scholar]
- 5.Arikawa J, Mizushima J, Higaki Y, Hoshino J, Kawashima M. Mandibular alveolar bone necrosis after trigeminal herpes zoster. Int J Dermatol. 2004;43:136–7. doi: 10.1111/j.1365-4632.2004.01837.x. [DOI] [PubMed] [Google Scholar]
- 6.Mendieta C, Miranda J, Brunet LI, Gargallo J, Berini L. Alveolar bone necrosis and tooth exfoliation following herpes zoster infection: A review of the literature and case report. J Periodontol. 2005;76:148–53. doi: 10.1902/jop.2005.76.1.148. [DOI] [PubMed] [Google Scholar]
- 7.Chindia ML. HIV-associated fulminating herpes zoster infection with alveolar necrosis and tooth exfoliation: A case report. Dent Update. 1997;24:126–8. [PubMed] [Google Scholar]
- 8.Siwamogstham P, Kuansuwan C, Reichart PA. Herpes zoster in HIV infection with osteonecrosis of the jaw and tooth exfoliation. Oral Dis. 2006;12:500–5. doi: 10.1111/j.1601-0825.2006.01230.x. [DOI] [PubMed] [Google Scholar]


