Abstract
Background
Inpatients may be at risk of cardiopulmonary instability during radiologic testing. Calling the medical emergency team is one rescue intervention that brings a team of critical care providers to the unstable patient. Little is known, however, about patients’ instability and activations of the medical emergency team in the radiology department (RD-MET).
Objectives
To describe the cause of activation of the RD-MET for hospitalized patients, temporal attributes of RD-MET involvement, characteristics of RD-MET patients, and characteristics associated with good and poor outcomes after RD-MET activation.
Methods
Retrospective pilot study of RD-MET calls for 64 inpatients in a tertiary care hospital during 2009.
Results
Reasons for RD-MET activation were 39% neurological, 38% cardiac, and 22% respiratory, and nearly half (42%) occurred during a computed tomography scan. Most RD-MET calls were made between 10 AM and noon. RD-MET patients had a mean age of 61 (SD, 19) years; 52% were female, and 89% were white. Admitting diagnoses were most commonly neurological (20%), cardiovascular (16%), and abdominal (16%). The most common comorbid conditions were chronic obstructive pulmonary disease (23%) and diabetes (20%). Half of RD-MET inpatients were from a general care unit, and 56% required preexisting oxygen support. After RD-MET involvement, 61% of patients required a higher level of care; 3% died during the MET intervention, and 19% died later in hospitalization. Patients with preexisting comorbid conditions were more likely to have poor outcomes after the RD-MET intervention (P = .001).
Conclusions
RD-MET patients with comorbid conditions, from a general care unit, and at risk for neurological deterioration arrive in the radiology department with potentially underestimated support needs. Greater support in specific time frames and locations may be warranted to improve outcomes.
Hospitalized patients who require diagnostic testing and procedures in the radiology department range from “stable” patients admitted for elective surgery to highly unstable critically ill patients who require a high level of human and technological monitoring and physiological support, including mechanical ventilation and hemodynamic support. Patients may be at risk for cardiopulmonary instability while undergoing diagnostic testing, and in some, that instability may progress to cardiorespiratory collapse. When instability occurs, one rescue intervention involves activation of a medical emergency team (MET) to bring a team of critical care providers to the imaging site. Although published reports describing MET activations and outcomes on clinical units within the hospital are fairly extensive,1-3 little is known about MET activations in diagnostic testing areas such as the radiology department. More information about the precursors of such events could lead to earlier detection of cardiopulmonary instability and improved outcomes in patients who require activation of the MET in the radiology department (RD-MET), inform interventions to prevent the need for RD-MET activation, and alter systems of care in the radiology department.
Rapid response to patients’ instability has driven the establishment of METs, whose goal is to bring a cadre of critical care providers to the bedsides of patients in unstable condition outside of the intensive care unit (ICU). Once cardiopulmonary instability is recognized, the MET provides a rapidly available secondary system of ICU level support to all units throughout the hospital. MET systems usually provide hospital staff with a preset list of criteria to serve as “triggers” to initiate a MET call, and staff are both educated and encouraged to use this resource.4,5 The success of the MET is dependent on early recognition of deterioration in a patient’s condition, rapid response by the bedside providers, and aggressive intervention to stabilize and rescue patients to prevent further deterioration in their condition.1,2
The onset of cardiopulmonary instability is rarely acute, but shows a cyclic pattern of change.
Early detection of deterioration in patients’ condition is key to successful intervention and may prevent complications.6,7 The onset of cardiopulmonary instability is rarely acute, but demonstrates a cyclic pattern of change with patients’ heart rate, blood pressure, respiratory rate, and oxygen saturation moving above and below accepted parameters, sometimes for hours before deterioration in their condition is acknowledged.
Clinical antecedents to patients’ cardiopulmonary instability have been detected 6 to 8 hours before recognized cardiorespiratory collapse.8,9 Owing to the cyclic pattern of these dynamic variables, cardiopulmonary instability may be missed by the intermittent clinical evaluation that may occur in the radiology department. Additionally, research has shown that patients being cared for in areas where the direct care providers are not specifically trained for their care requirements and diagnosis may be at greater risk for unrecognized cardiopulmonary instability and the need for MET activation.3 This situation often may occur in the radiology department, when patients at various levels of acuity receive care from staff members who are not familiar with their prior care needs, stability level, or particular diagnosis.
The purpose of this pilot study was to describe the reasons for RD-MET activation for hospitalized inpatients, the temporal attributes of RD-MET involvement, the characteristics of inpatients who experience RD-MET interventions, and the characteristics associated with outcomes after RD-MET activation.
Methods
This retrospective pilot study included all RD-MET activations for patients age 18 years and older between January 1 and December 31, 2009, at the University of Pittsburgh Medical Center Presbyterian Hospital in Pittsburgh, Pennsylvania, an urban tertiary care center with a well-established MET system. Patients who experienced a MET activation while in transit to or from the radiology department were excluded from the study, as were RD-MET activations for outpatients (eg, ambulatory test). This descriptive study was conducted with the approval and oversight of the institution’s Total Quality Council as a quality improvement initiative for the radiology department. All 64 inpatients who experienced an RD-MET intervention in 2009 were reviewed. Patients’ records were identified through the Medical Emergency Response Improvement Team database, which identifies all MET events occurring in the hospital. Patients were classified as having a poor outcome after RD-MET if they required a higher level of care after RD-MET intervention or did not survive to discharge. Higher level of care was indicated by 1 or more of 4 factors: increased respiratory support, increased level of cardiac support, necessity of an emergent procedure, or transfer to a higher acuity patient care unit.
MET Trigger Criteria
The radiology department uses the same MET trigger criteria as used in the general hospital units (Table 1) to respond to patients’ cardiopulmonary instability. Any nurse, physician, patient, or visitor can call for the MET by dialing a predetermined, well-publicized number.
Table 1.
Criteria for calling the University of Pittsburgh Medical Center’s medical emergency team during the study perioda
| Respiratory
|
| Rate <8/min or >36/min |
| New onset of difficult breathing |
| New pulse oximeter reading <85% for >5 min without known chronic hypoxia |
| New oxygen requirement to keep SpO2 >85% |
|
|
| Cardiovascular
|
| Heart rate <40/min or >140/min with new symptoms or any rate >160/min |
| Blood pressure <80 mm Hg or >200 mm Hg systolic or 110 mm Hg diastolic with symptoms (neurological changes, angina, dyspnea) |
|
|
| Acute neurological change
|
| Acute loss of consciousness |
| New onset of lethargy |
| Sudden collapse |
| Seizure (outside of seizure monitor unit) |
| Sudden loss of movement or weakness in the face, arm, or leg |
|
|
| Other
|
| >1 stat page required to assemble team needed to respond to a crisis Patient complaint of chest pain (unresponsive to nitroglycerine or physician unavailable) |
| Color change (patient or extremity): pale, dusky, gray, or blue |
| Unexplained agitation of >10 min |
| Use of naloxone without immediate response |
| Suicide attempt |
| Uncontrolled bleeding |
| Bleeding into airway |
| Large acute blood loss |
| Crash cart must be used for rapid delivery of medications |
Based on data from DeVita et al.1
Data Collection and Variables of Interest
Patients’ demographics and event details for all RD-METs were extracted from the electronic medical records, which included the reason for the RD-MET call, time and day of week, patients’ characteristics before the event:
codes for the admitting diagnosis from the International Classification of Diseases, Ninth Revision (ICD-9)
Charlson comorbidity index (CCI)
unit of origin (unit from which patient was sent to radiology)
radiology technique
oxygen requirements and patients’ outcomes after the RD-MET intervention:
requiring a higher level of care
survival to discharge.
For all patients who did not survive to discharge, the date and time of death were obtained. Information to calculate CCI scores was obtained by reviewing the electronic medical records.
ICD-9 codes that were not recorded in the electronic medical record were determined by cross-checking the documented admitting diagnosis with the ICD-9 code book.10 Admitting diagnoses, obtained from the physician’s admission clinical note, were considered primary or secondary according to the order they appeared in the patient’s record. All charts were reviewed by the first author (L.K.O.).
Statistics
Statistical analysis was done by using SPSS version 17 (SPSS Inc, Chicago, Illinois). Missing data fields were not replaced. Continuous variables were reported as mean with standard deviation, and comparisons were made by using a Student t test or Mann Whitney test as appropriate. The same conclusions were drawn from the Student t test and Mann Whitney test; therefore the results of the Student t test were reported. Categorical variables were reported as frequencies with percentages, and comparisons were made by using χ2 tests and the Fisher exact test. Age was calculated as the patient’s age when the RD-MET was activated. Admitting ICD-9 codes were categorized into 11 related categories representing primary diagnosis. CCI scores were reported as individual item scores and a total score.
Units of origin were categorized as general care units, step-down units, and ICUs. Reasons for RD-MET activation were categorized as neurological, cardiac, or respiratory. Time of day was categorized by 2-hour increments for analysis. All tests were 2-sided, and P values less than .05 were considered statistically significant.
Results
The RD-MET was activated 65 times from January 1 through December 31, 2009, involving 64 different patients. One patient experienced 2 RD-MET calls on the same day for the same reason; therefore this patient was included in the analysis once, resulting in a study sample of 64 patients. Hospitalized patients had the RD-MET activated for the following reasons: neurological (39%), cardiac (38%), and respiratory (22%). Temporally, RD-MET calls were most likely to occur between 10 AM and noon (see Figure, part A). RD-MET calls were more likely to be made on Wednesday (25%), followed by Friday (16%) and Tuesday (14%; see Figure, part B).
Figure.
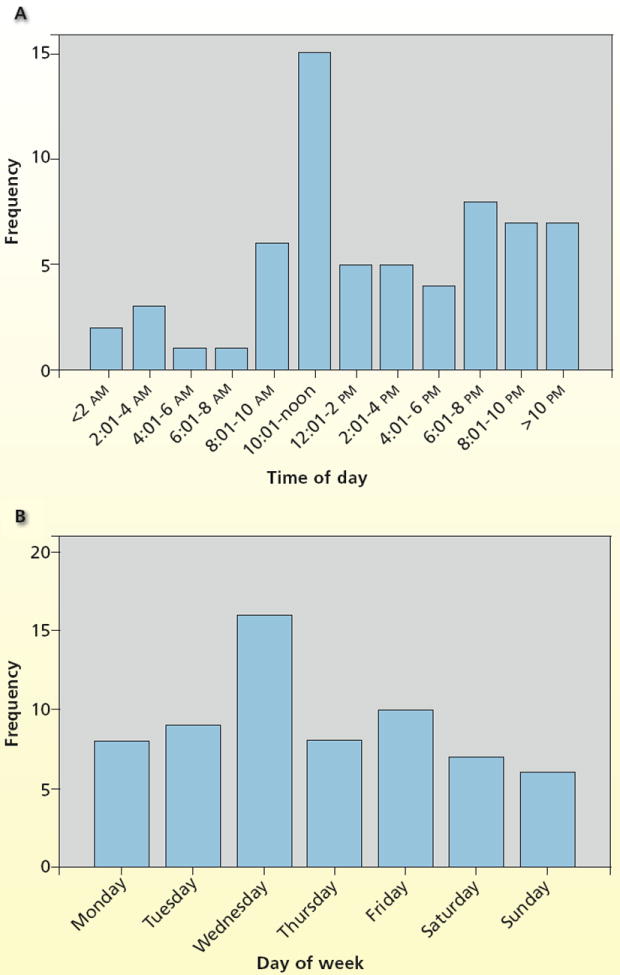
Temporal relationship between activations of the medical emergency team in the radiology department and time of day (A) and day of week (B) when team was activated.
Overall, the inpatients who experienced RD-MET had a mean age of 61 years (Table 2) and were white (the percentage of white patients in the sample was consistent with local population demographics). The most common admitting diagnoses were neurological (20%), cardiovascular (16%), abdominal (16%), and respiratory (14%). The total CCI score had a mean of 4.6 (SD, 2.8) with a range of 0 to 11. The most common comorbid conditions were chronic obstructive pulmonary disease (23%), diabetes mellitus without complications (20%), and congestive heart failure (19%).
Table 2.
Characteristics of 64 inpatients who required activation of the medical emergency team in the radiology department
| Characteristic | Valuea |
|---|---|
| Age, y | |
| Mean (SD) | 61 (19) |
| Median | 62.2 |
| Range | 18.12-87.44 |
|
| |
| Female sex | 33 (52) |
|
| |
| White race | 57 (89) |
|
| |
| Primary admitting diagnosis | |
| Neurological problem | 13 (20) |
| Abdominal problem | 10 (16) |
| Cardiovascular problem | 10 (16) |
| Respiratory problem | 9 (14) |
| Infection | 5 (8) |
| Peripheral vascular problem | 5 (8) |
| Trauma | 4 (6) |
| Cancer | 3 (5) |
| Diabetes | 2 (3) |
| Psychiatric problem | 2 (3) |
| Skeletomuscular problem | 1 (2) |
|
| |
| Charlson Comorbidity Index | |
| Mean (SD) | 4.6 (2.8) |
| Median | 4.5 |
| Range | 0-11 |
| Total score | |
| 0 | 6 (9) |
| 1 | 4 (6) |
| 2 | 6 (9) |
| 3 | 6 (9) |
| 4 | 10 (15.6) |
| ≥5 | 32 (50) |
|
| |
| Radiology technique used | |
| Computed tomography | 27 (42) |
| Magnetic resonance imaging | 16 (25) |
| Interventional radiology | 9 (14) |
| General radiography | 9 (9) |
| Nuclear medicine | 3 (5) |
| Peripheral vascular | 1 (2) |
| Fluoroscopy | 1 (2) |
| Ultrasound | 1 (2) |
|
| |
| Respiratory support before team called | 36 (56) |
| Nasal cannula | 21 (33) |
| Oxygen mask | 9 (14) |
| Mechanical ventilation | 6 (9) |
Values are No. (%) of patients unless otherwise indicated.
RD-MET calls were most likely to occur during computed tomography (CT), followed by magnetic resonance imaging and interventional radiology. The most common units of origin for patients experiencing an RD-MET intervention were the general care units followed by the ICU and the step-down units. Most patients required respiratory support before the RD-MET was called; nasal cannula was the most common oxygen delivery system.
After the RD-MET intervention, almost two-thirds of patients required a higher level of care; increased respiratory support was the most common reason (Table 3). Although only 2 patients (3%) died during the RD-MET intervention, nearly one-quarter (22%) of the RD-MET patients did not survive to discharge.
Table 3.
Outcomes of 64 inpatients after activation of the medical emergency team in the radiology department
| Outcome | No. (%) |
|---|---|
| Higher level of care | 39 (61) |
| Respiratory support | 23 (36) |
| Immediate transfer to higher care unit | 18 (28) |
| Cardiac support | 14 (22) |
| Procedure | 13 (20) |
|
| |
| Died during or after team activated during hospitalization | 14 (22) |
| Died during medical emergency team episode | 2 (3) |
Two-thirds (67%) of RD-MET patients (n = 43) experienced a poor outcome (Table 4). Patients with good versus poor outcomes did not differ significantly in age, sex, admitting diagnosis, radiology technique used, unit of origin, prior oxygen support, or the reason that the RD-MET was activated. However, patients who experienced poor outcomes were more likely to have pre-existing comorbid conditions, according to the CCI total score.
Table 4.
Comparison of the characteristics of inpatients with good and poor outcomes after activation of the medical emergency team in the radiology department
| Characteristic | Outcome
|
P | Odds ratiob | 95% Confidence interval | |
|---|---|---|---|---|---|
| Good (n = 21, 33%) | Poora (n = 43, 67%) | ||||
| Age, mean (SD), y | 56 (20) | 63 (18) | .17 | 1.02 | 0.99-1.05 |
|
| |||||
| Sex | .29 | 0.56 | 0.18-1.55 | ||
| Female | 13 (39)c | 20 (61) | |||
| Male | 8 (26) | 23 (74) | |||
|
| |||||
| Primary admitting diagnosis | |||||
| Cardiovascular problem | 1 (10) | 9 (90) | .15 | 5.29 | 0.62-44.93 |
| Respiratory problem | 3 (33) | 6 (67) | >.99 | 0.97 | 0.22-4.34 |
| Neurological problem | 4 (31) | 9 (69) | >.99 | 1.13 | 0.30-4.19 |
| Peripheral vascular problem | 3 (60) | 2 (40) | .32 | 0.29 | 0.05-1.91 |
| Trauma | 2 (75) | 1 (25) | .10 | 0.14 | 0.04-1.47 |
| Psychiatric problem | 2 (100) | 0 (0) | .10 | 0.31 | 0.21-0.45 |
| Skeletomuscular problem | 1 (100) | 0 (0) | .33 | 0.32 | 0.22-0.46 |
| Diabetes | 0 (0) | 2 (100) | >.99 | 0.66 | 0.55-0.80 |
| Infection | 1 (20) | 4 (80) | >.99 | 0.21 | 0.26-19.6 |
| Abdominal problem | 3 (30) | 7 (70) | >.99 | 1.17 | 0.27-5.05 |
| Cancer | 0 (0) | 3 (100) | .55 | 0.66 | 0.55-0.79 |
|
| |||||
| Charlson Comorbidity Index, mean (SD) | 3.0 (2.3) | 5.4 (2.8) | .001 | 1.44 | 1.13-1.83 |
|
| |||||
| Radiology technique | |||||
| Magnetic resonance imaging | 8 (50) | 8 (50) | .13 | 0.37 | 0.12-1.20 |
| Computed tomography | 7 (26) | 20 (74) | .42 | 1.74 | 0.60-5.16 |
| Interventional radiology | 1 (11) | 8 (89) | .16 | 4.60 | 0.53-39.3 |
| Otherd | 5 (42) | 7 (58) | .51 | 0.62 | 0.17-2.26 |
|
| |||||
| Unit of origin | |||||
| General care unit | 13 (41) | 19 (59) | .29 | 0.49 | 0.17-1.42 |
| Step-down unit | 1 (11) | 8 (89) | .25 | 4.57 | 0.53-39.25 |
| Intensive care unit | 7 (30) | 16 (70) | >.99 | 1.19 | 0.40-3.55 |
|
| |||||
| Respiratory support before team activated | |||||
| None | 10 (36) | 18 (64) | .79 | 0.79 | 0.28-2.26 |
| Nasal cannula | 5 (24) | 16 (76) | .39 | 1.90 | 0.58-6.17 |
| Oxygen mask | 3 (33) | 6 (67) | >.99 | 0.97 | 0.22-4.34 |
| Mechanical ventilation | 3 (50) | 3 (50) | .39 | 0.45 | 0.10-2.45 |
|
| |||||
| Reason why team activated | |||||
| Neurological | 10 (40) | 15 (60) | .42 | 0.60 | 0.20-1.70 |
| Cardiovascular | 6 (25) | 18 (75) | .41 | 1.80 | 0.60-5.54 |
| Respiratory | 4 (29) | 10 (71) | >.99 | 1.29 | 0.35-4.72 |
Poor outcome equals higher level of care and/or death. Values are No. (%) of patients unless otherwise indicated.
Unadjusted crude odds ratio.
Row percentages were reported to illuminate possible clinically relevant associations.
Peripheral vascular, nuclear medicine, fluoroscopy, general radiography, ultrasound.
Discussion
Inpatients sometimes experience instability that requires MET activation when away from their hospital units. Studies to date of METs and the patients experiencing cardiopulmonary instability who require MET intervention have been conducted on medical and surgical inpatients.2,3 We are the first to describe cardiopulmonary instability among patients in the radiology department, and interestingly RD-MET activations vary in some ways from MET activations on inpatient care units.
The most important finding of our pilot study is that the reasons for deterioration in a patient’s condition that warrants an RD-MET activation are most commonly of a neurological origin, including changes in level of consciousness and seizures. This finding is in contrast to reports of hypoxia and respiratory symptoms as the most common causes of instability on inpatient units.11,12 Perhaps patients in the radiology department are at greater risk for neurological deterioration, and as Downey et al13 suggest, clinicians may be less astute at recognizing acute changes in consciousness than they are at recognizing changes in other physiological parameters. We also found that 60% of the patients with a neurological reason for RD-MET activation experienced a poor outcome. We did not collect data on procedural sedation or the documentation of level of consciousness before transport to the radiology department, but gathering this more detailed information in the future may be helpful in explaining this finding.
The third most common reason for RD-MET activation was respiratory problems (22%), and 71% of these patients experienced poor outcomes. Given that more than half (56%) of patients arrive in the radiology department with supplemental oxygen support, and 23% have chronic obstructive pulmonary disease as a pre-existing comorbid condition, it is not surprising that respiratory deterioration occurs this often. Again, gathering information on sedation before the procedure may lend insight into this finding.
The CCI was chosen to measure comorbidity burden in the sample because the CCI has demonstrated excellent discrimination of in-hospital mortality with an area under the receiver operating characteristic curve of 0.86 to 0.87.14 The CCI has been validated in various populations of patients15,16 and across different hospital systems internationally14-17; CCI score is a consistent predictor of 1-year mortality and in-hospital mortality. The CCI total scores for this RD-MET sample are high (50% of CCI scores ≥5) compared with CCI total scores reported in other instability studies that featured patients in general care areas (Hravnak et al,9 8.9% CI ≥4; Capelastegui et al,18 12.5% CCI ≥3; Chin et al,19 20% CCI ≥4). CCI total scores of 5 of higher have been associated with high mortality and complications related to comorbid conditions in hospitalized patients.19,20
This information, along with the high prevalence of oxygen support required by our RD-MET patients, suggests that these patients are compromised at baseline and may require more frequent or sensitive neurological and respiratory assessment and monitoring than may be the current standard of care in the radiology department. Further inquiry is needed to examine the assessment of patients before transfer to the radiology department and the decision making involved in determining staffing needs for surveillance of patients while in the radiology department.
Another interesting finding is that the RD-MET was activated most commonly in the middle of the week and during the late morning hours. In the inpatient setting, temporal patterns of recognition of patients’ instability peak during the times of increased patient care activity and encounters with caregivers,3,9 such as during morning/evening care and the early shift assessment between 6 AM and 8 AM. One reason for this may be that caregivers tend to be more likely to recognize instability when they are in a face-to-face encounter with the patient during prescheduled bedside visits. Our finding of peak RD-MET activity between 10 AM and noon may suggest that those patients recognized as unstable earlier in the morning on the general care unit are being sent for diagnostic testing several hours later. Another possible explanation is that the midmorning hours represent peak volume for both inpatient and outpatient evaluation in the radiology department, and perhaps fewer staff are available for surveillance of patients. The increase in RD-MET activity again in the evening hours may reflect a similar pattern of recognition of instability in the general care unit followed by diagnostic testing later, and lower off-shift staffing patterns in the radiology department.
Because RD-MET activation occurred most during computed tomography, nurses should consider increasing vigilance during this time.
Interestingly, most RD-MET events occurred in patients who were sent from the general care unit (50%), and not from the ICU (36%) or from step-down units (14%). This may suggest that patients from ICUs and step-down units are expected to be unstable and are therefore accompanied to the radiology department by a nurse and, if undergoing mechanical ventilation, a respiratory therapist as well. “Stable” patients in the general care unit whose condition is not expected to deteriorate may not be observed as closely in the radiology department. Although 1-to-1 nurse-to-patient ratios for all patients in the radiology department is not feasible, further study is needed to develop models to predict which of these “stable” patients are at higher risk of development of instability in the radiology department and warrant closer human and technological observation.
Sixty-one percent of RD-MET patients required some higher level of care after the RD-MET intervention, suggesting that patients may be transferred to the radiology department without a sufficient needs assessment before transfer, leading to further deterioration in their condition while they are away from their units. Further study is needed to evaluate in more detail the characteristics of patients before transfer to the radiology department, the level of monitoring and nursing surveillance provided for patients while in the radiology department, and how these factors may affect patients’ outcomes.
RD-MET activation occurred most often during CT scanning (42%), with most of those patients (74%) having poor outcomes. This finding might be due to the use of CT as a diagnostic tool for evaluation of unstable inpatients, in particular those undergoing neurological imaging. Of the 2 patients who died during the RD-MET intervention, both were undergoing CT. CT scanning—a study that is noninvasive and of relatively short duration—is the diagnostic option of choice for unstable patients with suspected pulmonary emboli and stroke.21-25 Nevertheless, the CT procedure requires moving patients to the scanner table, the potential for dislodging catheters and tubes as the scanner table moves during the procedure, and compromise of ventilation because the patient remains supine (often with arms overhead). Additionally, staff remain outside the room during the test. Depending on the layout of the scanning suite, which can vary between institutions, visibility of the patient may also be limited during scanning. Although further study is needed to determine why MET calls occurred more often for patients during CT scanning, nurses should consider increasing vigilance for patients undergoing CT.
Although RD-MET occurred less often in patients undergoing interventional radiology (14%), poor outcomes for these patients were common (89%). Although the nurse to patient ratio is usually 1-to-1 during the procedure, the invasive nature of the interventional radiology procedures and the high acuity of these patients may explain this finding.
RD-MET patients experienced an overall mortality rate after RD-MET intervention (22%) that is higher than that reported in prior studies of MET activations.3,26 This finding may reflect the higher acuity of patients in the radiology department and increased risk for patients outside of their usual care area. This further suggests the need for improved assessment of patients’ needs before transferring patients to the radiology department to ensure the proper continuity of care while patients are away from their units of origin.
Limitations
This pilot study had several limitations. Performing the study at only 1 urban tertiary care center that has a well-established MET system may limit the generalizability of these findings to the inpatient populations seen by other radiology departments. The 1-year review has a limited sample size, and a larger sample may provide different findings. Physiological parameters and the details of patient care provided before transfer of the patient to the radiology department and during the visit to the radiology department (with the exception of supplemental oxygen support) were not collected. The retrospective nature of the pilot study required collection of data from a variety of existing data sources. We recognize that clinical data sources, such as the medical record, are not designed for research purposes, and missing or inconsistently recorded data may introduce threats to validity. Nevertheless, such pilot work is necessary in order to justify prospective studies in this area. Finally, more information about the level of surveillance and nursing characteristics would provide more insight into the reason that the RD-MET was activated.
Conclusion
RD-MET patients arrive in the radiology department with potentially underestimated support needs. Inpatients who are at risk for neurological, cardiovascular, and respiratory deterioration and experience an RD-MET intervention are likely to require a higher level of care. This pilot study provides information supporting the need for further study to increase understanding of the reasons for deterioration in patients’ condition while in the radiology department, and how systems of care might be improved to improve detection and support of patients in unstable condition before a MET call, including but not limited to the education, experience, training, and availability of staff in the radiology department.27
Acknowledgments
FINANCIAL DISCLOSURES
Dr Ott was supported by Research in Chronic and Critical Illness (T32 NR 008857). Dr Clark was supported by grant number KL2 RR024154 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Contributor Information
Lora K. Ott, was a doctoral candidate in the School of Nursing at the University of Pittsburgh, Pennsylvania when this study was done. She is now an adjunct faculty member at the University of Pittsburgh and an assistant professor at Indiana University of Pennsylvania.
Marilyn Hravnak, is a professor in the Department of Acute and Tertiary Care at the School of Nursing, University of Pittsburgh.
Sunday Clark, is an assistant professor in the Division of General Internal Medicine of the School of Medicine and the Department of Epidemiology in the Graduate School of Public Health at the University of Pittsburgh.
Nikhil B. Amesur, is an associate professor and patient safety officer in the Department of Radiology at UPMC Presbyterian Hospital in Pittsburgh, Pennsylvania.
References
- 1.DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons R. Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13:251–254. doi: 10.1136/qshc.2003.006585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of the effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004;32:916–921. doi: 10.1097/01.ccm.0000119428.02968.9e. [DOI] [PubMed] [Google Scholar]
- 3.Schmid-Mazzoccoli A, Hoffman L, Wolf G, Happ M, DeVita M. The use of medical emergency teams in medical and surgical patients: impact of patient, nurse and organisational characteristics. Qual Saf Health Care. 2008;17:377–381. doi: 10.1136/qshc.2006.020438. [DOI] [PubMed] [Google Scholar]
- 4.Winters B, Pham J, Hunt E, Guallar E, Berenholtz S, Pronovost P. Rapid response systems: a systematic review. Crit Care Med. 2007;35:1238–1243. doi: 10.1097/01.CCM.0000262388.85669.68. [DOI] [PubMed] [Google Scholar]
- 5.DeVita M, Bellomo R, Hillman K, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006;34(9):2463–2478. doi: 10.1097/01.CCM.0000235743.38172.6E. [DOI] [PubMed] [Google Scholar]
- 6.Hillman KM, Bristow PJ, Chey T, et al. et al. Antecedents to hospital deaths. Intern Med J. 2001;31:343–348. doi: 10.1046/j.1445-5994.2001.00077.x. [DOI] [PubMed] [Google Scholar]
- 7.Hillman KM, Bristow PJ, Chey T, et al. Duration of life-threatening antecedents prior to intensive care admission. Intensive Care Med. 2002;28:1629–1634. doi: 10.1007/s00134-002-1496-y. [DOI] [PubMed] [Google Scholar]
- 8.Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98:1388–1392. doi: 10.1378/chest.98.6.1388. [DOI] [PubMed] [Google Scholar]
- 9.Hravnak M, DeVita M, Edwards L, et al. Defining the incidence of cardio-respiratory instability in step-down unit patients using an electronic integrated monitoring system. Arch Intern Med. 2008;168:1300–1308. doi: 10.1001/archinte.168.12.1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Generic ICD-9-CM. Reno, NV: Channel Publishing, Ltd; 2010. [Google Scholar]
- 11.Hodgetts T, Kenward G, Vlachonikolis I, et al. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation. 2002;54:125–131. doi: 10.1016/s0300-9572(02)00100-4. [DOI] [PubMed] [Google Scholar]
- 12.Jones D, Duke G, Green J, et al. Medical emergency team syndromes and an approach to their management. Crit Care. 2006;10:R30. doi: 10.1186/cc4821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Downey A, Quach J, Haase M, et al. Characteristics and outcomes of patients receiving a medical emergency team review for acute change in conscious state or arrhythmias. Crit Care Med. 2008;36(2):477–481. doi: 10.1097/01.CCM.0000300277.41113.46. [DOI] [PubMed] [Google Scholar]
- 14.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali W. New ICD-10 version of the Charlson Comorbidity Index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 15.Needham D, Scales D, Laupacis A, Pronovost P. A systematic review of the Charlson comorbidity index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005;20:12–19. doi: 10.1016/j.jcrc.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 16.Hall W, Ramachandran R, Narayan S, Jani A, Vijayakumar S. An electronic application for rapidly calculating Charlson comorbidity score. BioMed Central Cancer. 2004;4:94. doi: 10.1186/1471-2407-4-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quan H, Parsons G, Ghali W. Validity of information on comorbidity derived from ICD-9-CCM administrative data. Med Care. 2002;40:675–685. doi: 10.1097/00005650-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Capelastegui A, Espana P, Bilbao A, et al. Pneumonia: Criteria for patient instability on hospital discharge. Chest. 2008;134:595–600. doi: 10.1378/chest.07-3039. [DOI] [PubMed] [Google Scholar]
- 19.Chin M, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol. 1997;79:1640–1644. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- 20.Charlson M, Pompei K, Ales K, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Anderson D, Barnes D. Computerized tomographic pulmonary angiography versus ventilation perfusion lung scanning for the diagnosis of pulmonary embolism. Curr Opin Pulm Med. 2009;15:425–429. doi: 10.1097/MCP.0b013e32832d6b98. [DOI] [PubMed] [Google Scholar]
- 22.Tapson V. Acute pulmonary embolism. N Engl J Med. 2008;358(10):1037–1052. doi: 10.1056/NEJMra072753. [DOI] [PubMed] [Google Scholar]
- 23.Ragni M. Pulmonary embolism and spiral computerized tomographic scans. Curr Opin Pulm Med. 2009;15:430–438. doi: 10.1097/MCP.0b013e32832d860d. [DOI] [PubMed] [Google Scholar]
- 24.Geerts W, Graham F, Pineo J, et al. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126:338S–400S. doi: 10.1378/chest.126.3_suppl.338S. [DOI] [PubMed] [Google Scholar]
- 25.Nyquist P. Management of acute intracranial and intraventricular hemorrhage. Crit Care Med. 2010;38(3):946–953. doi: 10.1097/CCM.0b013e3181d16a04. [DOI] [PubMed] [Google Scholar]
- 26.Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on post-operative morbidity and mortality rates. Crit Care Med. 2004;32(4):916–921. doi: 10.1097/01.ccm.0000119428.02968.9e. [DOI] [PubMed] [Google Scholar]
- 27.DeVita M, Smith G, Adam S, et al. Identifying the hospitalized patient in crisis: a consensus conference on the afferent limb of rapid response systems. Resuscitation. 2010;81:375–382. doi: 10.1016/j.resuscitation.2009.12.008. [DOI] [PubMed] [Google Scholar]


