Abstract
Background:
Sleep disturbances and decline in the physical functionality are common conditions associated with aging. Pharmacological treatment of sleep disturbances can be associated with various adverse effects. Short term trials of Yoga on sleep have shown beneficial effects.
Objectives:
To evaluate the effect of long-term Yoga exercises on sleep quality and quality of life (QOL) in the elderly.
Materials and Methods:
This was a cross-sectional study in which data were collected from elderly people aged 60 years or more living in Nagpur city. We employed two types of survey questionnaires: Pittsburgh sleep quality index (PSQI) and QOL Leiden-Padua (LEIPAD) Questionnaire. A total of 65 elderly men and women who signed an informed consent and completed questionnaires were included in the study. Sleep quality score PSQI and QOL (LEIPAD Questionnaire) score of the study group were evaluated and compared with the control group using Mann-Whitney U test.
Results:
Total PSQI score in Yoga group was lower than that of the control group. Also various QOL scores of the Yoga groups were higher than the control group.
Conclusion:
Addition of regular Yoga exercises in the daily routine of elderly people can help to achieve good sleep quality as well as improve the QOL.
Keywords: Asana, cognition, pranayama, quality of life, sleep, Yoga
INTRODUCTION
Sleep disturbances increase with aging and it is estimated that nearly 67% of the elderly people have at least one sleep-related complaint.[1] Various sleep-related problems identified in elderly people include long time to fall asleep, disturbed sleep at night, and decreased daytime alertness etc.[2,3] Researchers have observed direct correlation between poor sleep quality and increased physical and psychiatric morbidity, decline in cognitive function, and impaired quality of life (QOL).[4,5] Most common factors cited for sleep disturbances are lack of sufficient physical activity, poor sleep-related hygiene, and excessive daytime napping.[6] Although sleep-related problems in older people put extra burden on healthcare services and consume valuable economic resources, many physicians ignore this problem and consider them as a part of a normal aging process.[7] Various drugs like benzodiazepines and non-benzodiazepines are available for the pharmacological treatment of sleep-related problems. However, all these agents are not free from side effects, especially in geriatric population. Even short-term use of these agents have been associated with number of adverse drug reactions, which include dependence (both physical as well as psychological), impairment of psychomotor performance, disturbances in rapid eye movement sleep pattern, cognitive function abnormalities, and rebound insomnia etc.[8] In this respect, adverse effects produced by sleep medications can further compromise the QOL of an elderly person. Aging is also associated with reduced exercise capacity due to decrease in muscle mass resulting in loss of self-sufficiency.[9,10] So any non-pharmacological therapy minimizing the decline in physical capacity or sleeping disturbances will improve the QOL of geriatric population. One such non-pharmacological intervention is Yoga. Yoga is a combination of various postures, breathing techniques, and meditation. Beneficial effects of Yoga like reduction of blood pressure, relieving of anxiety, delaying functional decline, decreasing sleep disturbances, and improvement in serum lipid profile have been observed.[11] Manjunath and Telles reported in a randomized trial that after regular Yoga exercises for 6 months in a geriatric sample,[12] there was significant reduction in time to fall asleep, decreased sleep disturbance during night time, better sleep quality, decreased use of medications for sleep when compared with control group. Similar findings were reported in a study by Chen and Tseng,[13] where improvement in different aspects of sleep and decrease in depressive symptoms was observed after Yoga intervention. However, extremely limited amount of data is available whether these benefits of Yoga are retained over long term Yoga practice. Accordingly, current study was planned to assess the effect of long term Yoga exercises on sleep quality and QOL in elderly people.
MATERIALS AND METHODS
Design
This was a cross-sectional questionnaire-based survey. Participants were asked to complete two questionnaires only once for this study. Control group consisted of community dwelling older adults not doing any kind of Yoga exercises from Nagpur city, whereas, study group participants were recruited from Patanjali Yog Centre, Nagpur.
Settings and samples
Survey samples consisted of two groups: Yoga and non-Yoga groups. In Yoga group, 35 volunteers were included whereas non-Yoga group consisted of 30 participants. Study was started only after getting the clearance from the Institutional Ethics Committee, Government Medical College, Nagpur. Participants in both these groups were community-dwelling elders with age 60 years or more from Nagpur city. Control group participants were of age 60 years or more, of either gender and those who were not doing any kind of Yoga exercises. As this study was self-reporting type, participants who were bed-ridden or requiring assistance for their daily living activities, with severe cardiovascular, neurological, musculoskeletal, pulmonary disorders, or suffering from chronic infectious disorders like tuberculosis were not included in this study. In Yoga group, participants doing daily Yoga exercises for 2 years or more were included. All these participants were regularly attending Patanjali Yog Centre of Nagpur City, doing regular Yoga exercises for at least one hour, with a certified Yoga instructor daily, from 6 a.m. to 7 a.m. Different Yoga exercises performed by these participants were physical postures (Various asanas like mountain pose [Tadasana], triangle pose [Trikonasana], revolved triangle pose [Parivrtta Trikonasana], standing forward bend [Uttanasana], Hands to feet [Pada Hastasana], tree pose [Vrksasana], lotus pose [Padmasana], half spinal twist [ArdhaMatsyendrasana], wind relieving poses [Pavanamuktasana], bow pose [Dhanurasana], locust pose [Salabhasana], fish pose [Matsyasana], cobra pose [Bhujangasana], bridge Pose [Setu Bandhasana] etc.) Bandhas (Jalandhar bandh, Mulabandha, Uddiyanbandha NadiShuddhi Pranayama or Anuloma-Viloma [Alternate nostril breathing-I], Anuloma-Viloma [Alternate Nostril Breathing-II], Surya Bhedan [Right Nostril Breathing], Ujjayi, Bhramari, Pranayama from Hatha Yoga [Surya Bhedan, Bhasrika, Ujjayi, Shitali, Sitkari, Bhramari, Murchha, and Plavini Pranayama]). Prior to survey, participants were given complete information about the study procedure and all doubts regarding this study were clarified. Written informed consent was obtained from each participant.
Data collection
Data collection was done by visiting each participant at his/her home and administering two commonly used instruments, Pittsburgh sleep quality index (PSQI) and QOL Leiden-Padua (LEIPAD) Questionnaire. For better understanding of these questionnaires by participants, we translated each questionnaire into Hindi (national language) and Marathi (regional language) and as per request of the participant, suitable versions were administered to them.
PSQI is an effective instrument useful for measuring subjective sleep quality and sleep disturbances in older people. PSQI contains 19 self-rated questions and five questions rated by the bed partner or room-mate (if available). Responses from room partner or room-mate were not included in the scoring system. Nineteen questions were designed to measure seven aspects of sleep having scoring range of 0-3 each where a score of zero indicated no sleep disturbance, whereas a score of three indicated significant sleep disturbance. The scores from all these seven domains were then added to calculate PSQI, which had a scoring range of 0-21, where a score of zero meant no disturbance in sleep or good sleep quality whereas higher scores indicated poor or worse sleep quality. A score of five and above indicated clinically significant sleep disturbances. The seven aspects of sleep used in this instrument were total duration of sleep, sleep disturbances during the past month, time taken to fall asleep or sleep latency, daytime dysfunction due to somnolence, habitual sleep efficiency, overall sleep quality, and use of medicines for sleep.[14]
Other instrument we used in this study was LEIPAD questionnaire, which is a useful tool to measure QOL of older people. This popular instrument consists of 49 items, which measure six domains: Cognitive functioning (CF), depression/anxiety (DA), life satisfaction (LS), physical functioning (PF), self-care (SC), and social functioning (SF). Score of all items are combined to yield a global score from 0 to 81, where score of 81 indicates maximum impairment of QOL.[15]
Graph-pad prism version 5.01 (Graphpad Software, Inc., USA) was used to analyze data. Descriptive statistics such as mean and percentage were used to describe demographics of each group. Mann-Whitney U test was used to compare the QOL and sleep quality of Yoga and non-Yoga groups and P value less than 0.05 was considered statistically significant.
RESULTS
Yoga group comprised 35 participants out of which percentage of men and women were 65% and 35%, respectively, whereas in case of non-Yoga group, percentage of men and women was 66% and 34%, respectively. Average age of participant in Yoga group was 63.7 years whereas that of non-Yoga group participants was 62.8 years. Yoga group participants were doing Yoga exercises regularly and the average duration was 5.26 years.
Table 1 shows comparison of various sub-scales of PSQI between Yoga and non-Yoga group. Participants in the Yoga group had a mean total sleep quality score of 3.771 ± 0.3623. Participants in the non-Yoga group had a mean total sleep quality score of 8 ± 0.4315. The total PSQI score in Yoga group was below the cut off level of five and differed significantly (P < 0.0001) from the total PSQI score of non-Yoga group participants. Though the average sleep duration score was less in Yoga group participants, the difference was not statistically significant between the two groups. Yoga group participants had significantly less (P < 0.0001) sleeping disturbances, shorter sleep latency, and decreased use (P < 0.05) of sleep medications. Furthermore, subjective sleep quality and habitual sleep efficiency scores were significantly better (P < 0.0001) in Yoga group than non-Yoga group participants. No difference was observed in daytime dysfunction scores.
Table 1.
Scores of various domains of Pittsburgh sleep quality index in Yoga and non-Yoga group participants
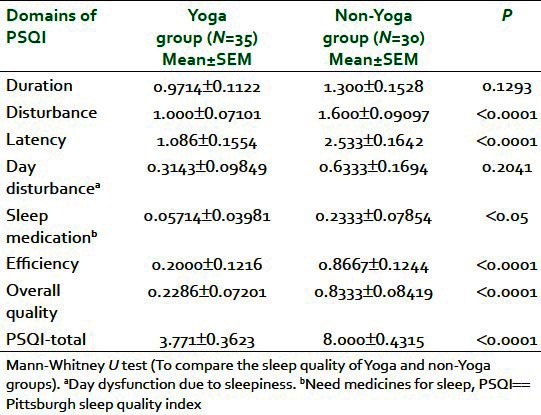
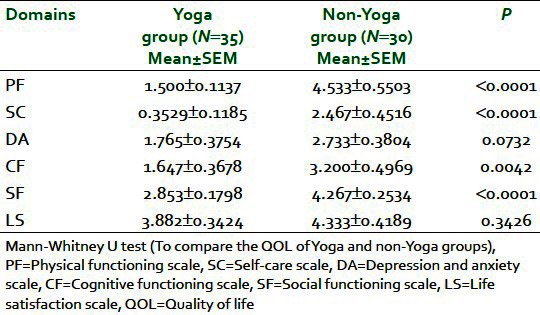
Table 2 shows comparison of scores between two groups for various items of LEIPAD questionnaire. Yoga group participants had significantly better (P < 0.0001) PF, SC functioning, and SF scores than non-Yoga group participants. CF score was significantly better (P < 0.05) in Yoga group. Although average scores of LS scale and DA scale were lower in Yoga group, no statistical difference was observed between the two groups.
Table 2.
Scores of various domains of quality of life Leiden-Padua quality of life in Yoga and non-Yoga group participants
DISCUSSION
Results of our study indicate that older adults practicing Yoga regularly had better overall sleep quality, less episodes of disturbed sleep, took less time to fall asleep, less day time dysfunction, less use of sleep medications and also felt more rested and energetic in the morning. These results were in accordance to previous studies where effect of 6 months Yoga intervention on elder people was studied and found that Yoga group participants had better sleep quality and less sleeping disturbances when compared with the control group.
One possible reason explained for better sleep quality in Yoga practitioners is that Yoga exercises involve stretching and relaxing of muscles causing significant physical and mental exertion resulting in less sleep latency, more deep sleep, less sleep disturbances, and better sleep efficiency.[16–18] As average duration of Yoga practices of participants was 5.26 years, we can say that benefits of Yoga were retained even after long-term Yoga practice in Yoga group of our study. However, exact relationship between Yoga and better sleep quality still remains to be elucidated.
Similarly, in a study reported by Dam et al., association between poor sleep quality and low wake time oxygen saturation (less than 90%) resulting in poor physical performance in the form of decreased grip strength and walking speed was observed.[19] Soni et al., concluded that Yogic breathing exercises can improve strength of the respiratory muscles which resulted in better tissue perfusion and improved oxygen saturation. Considering the fact that sleep apnea is associated with decreased oxygen saturation, improved oxygen saturation due to Yoga exercies might be another possible explanation for less sleep disturbances in Yoga group of our study.[20]
Snoring increases the chances of sleep disturbances two fold and this has been attributed to the weakened upper airway muscles, narrowing of the respiratory passage that causes snoring. Regular Yogic breathing exercises might have beneficial effect by strengthening upper airway muscles resulting in less sleep disturbances observed in this population.[21,22]
Previous studies of Yoga on health volunteers have shown that after short term Yoga exercises, there is significant increase in the vagal tone, decrease of sympathetic discharge in the form of significantly decreased heart rate response on standing as well as decreased catecholamine levels in plasma. This decreased physiological arousal effect of Yoga has been cited as one of the reasons for less sleep disturbances.[23,24]
Earlier studies have demonstrated association of poor quality of sleep with a poor physical function score; however, the exact mechanism behind this association is still not known.[19] Aging is associated with decreased muscular strength and muscle mass which results in decreased exercise capacity. Functional abilities are reduced, and hence restrictions in performing daily activities and loss of self-sufficiency can occur. Yoga exercises improve joint flexibility, prevent decline in the physical function, and improve the QOL of elderly people.[25] Our results also suggest similar findings in the form of improved PF and SC scores of LEIPAD QOL questionnaire. Similar results have been obtained in a study by Goncalves et al., in which data were collected from 83 elderly Yoga practitioners aged 60 years and above. Researchers found that joint flexibility measured using goniometry was significantly more than the control group, also significant reductions in activity execution timings were noted in Latin-American development to the maturity Group (LADEG) autonomy protocol.[26] In a systematic review, Woodyard has inferred that Yoga exercises involve stretching of the joints and long-term practice might be causing “gradual loosening of the muscles and connective tissues surrounding the bones and joints.” Regular stress on joints in Yoga exercises prevents the dystrophy of the cartilage thereby maintaining the joint function.[27] Thus, it is suggested that Yoga exercises are associated with less sleep disturbances (low PSQI score), which in turn are associated with better PF; consequently, elderly people can confidently live self-sufficient life with no dependency, which is reflected in better SF score in our study.
Better cognitive function scores in our research are consistent with previous studies where Yoga has shown to improve cognition. Though the exact mechanism of how Yoga improves cognition is not known, two hypotheses have been put forward including the role of Yoga in improving the mood and relieving the stress as chronic stress can lead to down-regulation of 5HT1A (5-hydroxytryptamine 1A) receptors with subsequent apoptosis of hippocampal neurons. Second mechanism suggested is the improvement of attention and alertness abilities as Yoga exercises involve concentrating on breathing or any specific part of the body.[28,29] Earlier studies have reported that disturbed sleep causes impaired psychomotor alertness, which can lead to decline in cognitive function known to be associated with prefrontal cortex.[30] With the advancing age, there is decrease in blood flow to the brain. Regular practice of Yoga might decrease autonomic over-activity and increase in parasympathetic activity with reduction of oxygen consumption and metabolic rate of prefrontal cortex cells. Thus, preventing the neuronal loss which might have the beneficial effect in arresting the decline in cognitive function.[31]
Study limitations
We collected this data by administering a questionnaire only. Incorporation of other qualitative methods like interviews or focus group discussions could have been more helpful in better understanding of factors related to reduced QOL in elderly such as, effects of social and lifestyle changes like death of spouse, chronic disorders associated with aging, depression, etc. This study was just a cross-sectional survey with small sample size, so findings in this study reflect only preliminary data regarding the impact of long-term practice of Yoga on sleep quality and QOL.
As aging is a continuous process, addition of non-pharmacological intervention like regular practice of Yoga in daily routine can improve sleep qualities, which in turn will improve physical function and cognitive function, thereby improving the QOL of elderly.
CONCLUSION
Long-term practice of Yoga exercises by elderly people is associated with less sleep disturbances and good sleep quality and these results are in accordance with many studies involving Yoga intervention for 6 month duration only. Considering the limited sample size and subjective data of our study, further studies are required to substantiate the findings in this study.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult-a mini-review. Gerontology. 2010;56:181–9. doi: 10.1159/000236900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 1.Sleep disorders commonly found in older people. CMAJ. 2007;176:1299–304. doi: 10.1503/cmaj.060792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lo CM, Lee PH. Prevalence and impacts of poor sleep on quality of life and associated factors of good sleepers in a sample of older Chinese adults. Health Qual Life Outcomes. 2012;10:72. doi: 10.1186/1477-7525-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrington JJ, Lee-Chiong T., Jr Sleep and older patients. Clin Chest Med. 2007;28:673–84. doi: 10.1016/j.ccm.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Ancoli-Israel S. Sleep and aging: Prevalence of disturbed sleep and treatment considerations in older adults. J Clin Psychiatry. 2005;66:24–30. [PubMed] [Google Scholar]
- 7.McCall WV. Sleep in the elderly: Burden, diagnosis, and treatment. Prim Care Companion J Clin Psychiatry. 2004;6:9–20. doi: 10.4088/pcc.v06n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenberg RP. Sleep maintenance insomnia: Strengths and weaknesses of current pharmacologic therapies. Ann Clin Psychiatry. 2006;18:49–56. doi: 10.1080/10401230500464711. [DOI] [PubMed] [Google Scholar]
- 9.Buechel HM, Popovic J, Searcy JL, Porter NM, Thibault O, Blalock EM. Deep sleep and parietal cortex gene expression changes are related to cognitive deficits with age. PLoS One. 2011;6:e18387. doi: 10.1371/journal.pone.0018387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vale RG, de Oliveira RD, Pernambuco CS, de Meneses YP, Novaes Jda S, de Andrade Ade F. Effects of muscle strength and aerobic training on basal serum levels of IGF-1 and cortisol in elderly women. Arch Gerontol Geriatr. 2009;49:343–7. doi: 10.1016/j.archger.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Sengupta P. Health Impacts of Yoga and Pranayama: A State-of-the-Art Review. Int J Prev Med. 2012;3:444–58. [PMC free article] [PubMed] [Google Scholar]
- 12.Manjunath NK, Telles S. Influence of Yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J Med Res. 2005;121:683–90. [PubMed] [Google Scholar]
- 13.Chen KM, Tseng WS. Pilot-testing the effects of a newly-developed silver yoga exercise program for female seniors. J Nurs Res. 2008;16:37–46. doi: 10.1097/01.jnr.0000387288.76430.bb. [DOI] [PubMed] [Google Scholar]
- 14.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 15.De Leo D, Diekstra RF, Lonnqvist J, Trabucchi M, Cleiren MH, Frisoni GB, et al. LEIPAD, an internationally applicable instrument to assess quality of life in the elderly. Behav Med. 1998;24:17–27. doi: 10.1080/08964289809596377. [DOI] [PubMed] [Google Scholar]
- 16.Chen KM, Chen MH, Chao HC, Hung HM, Lin HS, Li CH. Sleep quality, depression state, and health status of older adults after silver yoga exercises: Cluster randomized trial. Int J Nurs Stud. 2009;46:154–63. doi: 10.1016/j.ijnurstu.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 17.Cohen L, Warneke C, Fouladi RT, Rodriguez MA, Chaoul-Reich A. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253–60. doi: 10.1002/cncr.20236. [DOI] [PubMed] [Google Scholar]
- 18.Chen KM, Chen MH, Lin MH, Fan JT, Lin HS, Li CH. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J Nurs Res. 2010;18:53–61. doi: 10.1097/JNR.0b013e3181ce5189. [DOI] [PubMed] [Google Scholar]
- 19.Dam TT, Ewing S, Ancoli-Israel S, Ensrud K, Redline S, Stone K, et al. Association between sleep and physical function in older men: The osteoporotic fractures in men sleep study. J Am Geriatr Soc. 2008;56:1665–73. doi: 10.1111/j.1532-5415.2008.01846.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soni R, Munish K, Singh K, Singh S. Study of the effect of yoga training on diffusion capacity in chronic obstructive pulmonary disease patients: A controlled trial. Int J Yoga. 2012;5:123–7. doi: 10.4103/0973-6131.98230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobsen JH, Shi L, Mokhlesi B. Factors associated with excessive daytime sleepiness in patients with severe obstructive sleep apnea. Sleep Breath. 2012 doi: 10.1007/s11325-012-0733-z. [In press] [DOI] [PubMed] [Google Scholar]
- 22.Mehra R, Stone KL, Blackwell T, Ancoli Israel S, Dam TT, Stefanick ML, et al. Prevalence and correlates of sleep-disordered breathing in older men: Osteoporotic fractures in men sleep study. J Am Geriatr Soc. 2007;55:1356–64. doi: 10.1111/j.1532-5415.2007.01290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Veerabhadrappa SG, Baljoshi VS, Khanapure S, Herur A, Patil S, Ankad RB, et al. Effect of yogic bellows on cardiovascular autonomic reactivity. J Cardiovasc Dis Res. 2011;2:223–7. doi: 10.4103/0975-3583.89806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pal GK, Velkumary S, Madanmohan Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- 25.Ebnezar J, Nagarathna R, Bali Y, Nagendra HR. Effect of an integrated approach of yoga therapy on quality of life in osteoarthritis of the knee joint: A randomized control study. Int J Yoga. 2011;4:55–63. doi: 10.4103/0973-6131.85486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gonçalves LC, Vale RG, Barata NJ, Varejão RV, Dantas EH. Flexibility, functional autonomy and quality of life (QoL) in elderly yoga practitioners. Arch Gerontol Geriatr. 2011;53:158–62. doi: 10.1016/j.archger.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 27.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, Haas M, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–7. [PMC free article] [PubMed] [Google Scholar]
- 29.Bangalore NG, Varambally S. Yoga therapy for Schizophrenia. Int J Yoga. 2012;5:85–91. doi: 10.4103/0973-6131.98212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kyizom T, Singh S, Singh KP, Tandon OP, Kumar R. Effect of pranayama and yoga-asana on cognitive brain functions in type 2 diabetes-P3 event related evoked potential (ERP) Indian J Med Res. 2010;131:636–40. [PubMed] [Google Scholar]
- 31.Blatter K, Cajochen C. Circadian rhythms in cognitive performance: Methodological constraints, protocols, theoretical underpinnings. Physiol Behav. 2007;90:196–208. doi: 10.1016/j.physbeh.2006.09.009. [DOI] [PubMed] [Google Scholar]


