Abstract
Objectives:
This study aims to demonstrate the effectiveness of leaded glasses in reducing the lens of eye dose and of lead thyroid collars in reducing the dose to the thyroid gland of an adult female from dental cone beam CT (CBCT). The effect of collimation on the radiation dose in head organs is also examined.
Methods:
Dose measurements were conducted by placing optically stimulated luminescent dosemeters in an anthropomorphic female phantom. Eye lens dose was measured by placing a dosemeter on the anterior surface of the phantom eye location. All exposures were performed on one commercially available dental CBCT machine, using selected collimation and exposure techniques. Each scan technique was performed without any lead shielding and then repeated with lead shielding in place. To calculate the percent reduction from lead shielding, the dose measured with lead shielding was divided by the dose measured without lead shielding. The percent reduction from collimation was calculated by comparing the dose measured with collimation to the dose measured without collimation.
Results:
The dose to the internal eye for one of the scans without leaded glasses or thyroid shield was 0.450 cGy and with glasses and thyroid shield was 0.116 cGy (a 74% reduction). The reduction to the lens of the eye was from 0.396 cGy to 0.153 cGy (a 61% reduction). Without glasses or thyroid shield, the thyroid dose was 0.158 cGy; and when both glasses and shield were used, the thyroid dose was reduced to 0.091 cGy (a 42% reduction).
Conclusions:
Collimation alone reduced the dose to the brain by up to 91%, with a similar reduction in other organs. Based on these data, leaded glasses, thyroid collars and collimation minimize the dose to organs outside the field of view.
Keywords: Leaded glasses, thyroid shielding, CBCT dosimetry, dose reduction, eye lens dose
Introduction
In a previous paper,1 we reported that the use of leaded glasses reduced the radiation dose to the eye from an Iluma® dental cone beam CT (CBCT) system (Imtec, Ardmore, OK) by approximately 62% for a full field of view scan and 36% for a collimated scan. This dose reduction applies for the one specific machine studied, as other investigators2–5 have reported that no two CBCT machines produce the same amount of radiation at similar settings. Here, we are studying the radiation sparing effect of eye and thyroid shielding for an adult female anthropomorphic phantom on an i-CAT (Imaging Sciences International, Inc., Hatfield, PA) Platinum CBCT system. The International Commission on Radiological Protection (ICRP) has reviewed recent epidemiological evidence suggesting that, for the lens of the eye, the threshold in the absorbed dose for cataractogenesis is now considered to be as low as 0.5 Gy.6 Additionally, ionizing radiation can cause chromosomal mutations that are non-repairable, and some studies have suggested that the effects are cumulative.7 Several large pooled research evaluation reports have suggested that such stochastic effects are believed to have no threshold radiation dose below which they will not occur.8–10 In the last three decades, incidence of thyroid cancer has increased worldwide.11–13 In fact, the thyroid gland, especially in children, is among the most sensitive organs to radiation-induced tumours, both benign and malignant.14 There is a strong inverse relationship between the risk of thyroid cancer and the age at the time of exposure for ages under 20 years, with a small risk over the age of 20 years.9,15 Although it was initially assumed that the relative risk of radiation-induced thyroid cancer for women was twice the relative risk for men,9 additional studies have shown that the risk is equal in both women and men.15 Although doses and risks from dental radiology are considered to be small, a number of epidemiological studies have provided some limited evidence of an increased risk of thyroid tumours resulting from dental radiography.9,12,16,17 However, there are weaknesses in these studies in that they rely on patient’s recall of treatment and there are neither records of the number of images taken over the years nor any data on the dose each patient received. Nonetheless, since radiation doses used in dentistry have the potential to cause biological damage,18 it is appropriate to optimize dental imaging such that we reduce radiation exposure through appropriate methods of dose reduction commensurate with the diagnostic requirements.19 Such optimization methods include collimation and thyroid shielding for dental applications.20–23 Although the benefit of lead shielding to radiosensitive organs has been recognized,24 even with optimum techniques, the primary dental X-ray beam may still pass near and occasionally through the gland. In the absence of a thyroid shield, children have a larger fraction of neck structure exposed to radiation than adults.25 Indeed, the National Council on Radiation Protection and Measurements (NCRP) recommends that thyroid shielding shall be provided for children and should be provided for adults when it will not interfere with the examination.14 Care is needed in positioning so that repeat exposures are not required.9 There has been little published with regard to the CBCT patient dose measured using optically stimulated luminescence (OSL) dosemeters. The potential dose reduction gained by wearing a thyroid shield during CBCT has not been extensively investigated.
Prins et al1 reported that the wearing of leaded glasses during various CBCT procedures reduced the absorbed dose to the eye for a full scan by more than 60% and by 38% for a collimated scan. Both the ICRP and the NCRP consider radiation-induced lens opacification to be a deterministic event, and the ICRP has noted that newer studies have suggested that it may occur at doses less than previously thought.10 The recent evidence for a lower threshold for eye lens opacification than was previously thought was recently acknowledged by the ICRP by citing their intent to recommend reducing the annual eye lens equivalent dose from 150 mSv to 20 mSv.10 There are limited studies on the effectiveness of lead shielding to reduce the dose to both thyroid and the eye using different scanning protocols and next-generation scanners. Therefore, we investigated the impact of wearing leaded glasses and a thyroid shield on doses to the lens of the eye and thyroid using an anthropomorphic female phantom and a commercially available dental CBCT scanner using five various exposure settings. We suggest the use of protective lead garments as part of an overall effort to optimize the radiation exposure from dental radiography.
Materials and methods
An adult female anthropomorphic phantom [model 702; Computerized Reference Imaging System (CIRS), Norfolk, VA] representing an average woman who is 160 cm in height and 55 kg in weight was used for all exposures. This full-bodied phantom is manufactured to ICRP 23 and International Commission on Radiation Units and Measurements (ICRU) 48 specifications and consists of 25-mm contiguous sections containing 21 specific inner organs.26 We utilized only the head and neck sections (12 sections). OSL dosemeters (NanoDot; Landauer, Glenwood, IL) were used to assess the radiation dose to ten key head and neck organs, including eye and thyroid. Dosemeters were also placed on the surface of each phantom eye to measure the lens dose. All scans were performed using an i-CAT Platinum CBCT machine in the State University of New York, Stony Brook Radiology Clinic, NY, USA. The five different scans consisted of different exposure techniques employed and are distinguished by collimation and resolution (voxel size). Table 1 summarises the scan types and parameters. The “full scan” was performed with no collimation (full field of view, approximately 17 cm height × 23 cm depth) at a resolution of 0.3 mm. The maxilla scan required that the field of view be, as much as possible, collimated to view only the maxilla, and it was performed at both 0.2 mm and 0.4 mm voxel sizes. Likewise, the field of view for the mandibular scan was limited to only the mandible, and the scan was performed with 0.2 mm and 0.4 mm voxel size. All exposures were performed at 120 kVp and 5 mA, and the exposure times were preset in the image acquisition software (i-CAT vision 1.9.3.13). Three exposures were performed for each type of scan, each consisting of a scout and volume acquisition. The scout scan was performed at a lower tube current and served to verify the accuracy of the position of the field of view. Each of the five types of scans were performed without leaded glasses (LG-600 Rayshield; Aadco Medical, Randolph, VT. 0.75 mm lead equivalent lenses, 0.25 lead side shields) or thyroid shield (Max Pro, 0.5 mm lead equivalent, Maxant Technologies Inc. Niles, IL), then repeated with lead glasses only, then repeated with thyroid shielding only and, finally, repeated with both thyroid shield and leaded glasses (Figure 1). After the completion of three exposures for each scan type, the dosemeters were removed from the phantom and placed into a storage container. Unexposed dosemeters were then placed in the same locations in the phantom, and the next exposure technique was performed. Care was taken to always place the dosemeter in the same orientation for each type of scan. Exposed dosemeters were transported with unexposed dosemeters to serve as negative controls (background readings). When applicable, the total organ dose was calculated by summing up the individual readings per location within an organ and dividing by the number of locations.
Table 1.
Scan types and parameters
| Scan type | Resolution (mm) | Time (s) |
| Full head | 0.3 | 8.9 |
| Mandible | 0.2 | 26.9 |
| Mandible | 0.4 | 8.9 |
| Maxilla | 0.2 | 26.9 |
| Maxilla | 0.4 | 8.9 |
Scanner: Platinum i-CAT (120 kVp, 5 mA); Imaging Sciences International, Inc., Hatfield, PA.
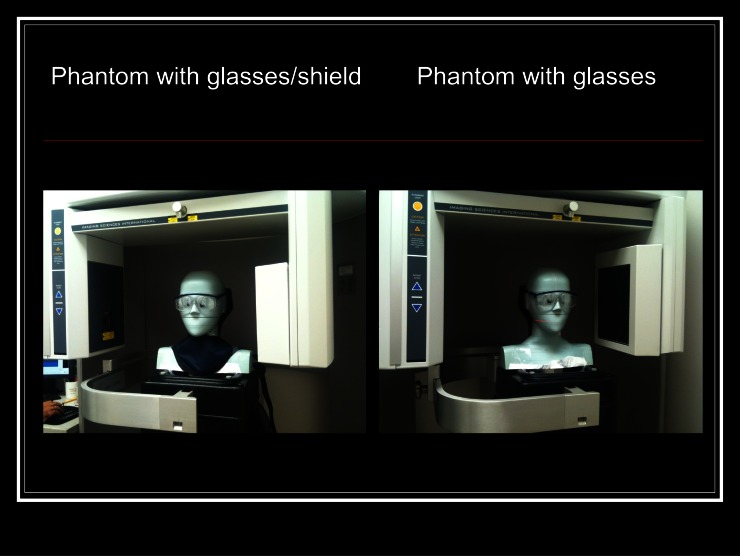
Figure 1.
Phantom with glasses and thyroid shield and glasses and no thyroid shield
Mean and standard deviation were calculated using Excel (Microsoft Corp., Redmond, WA). OSL dosemeters were analysed according to the manufacturer’s specifications and calibrated with a manufacturer-provided calibration set. All dosemeters were read three times and background readings were subtracted from the averaged readings. Individual readings of absorbed dose (cGy) from one scout plus one scan were obtained by dividing the averaged net reading minus background by three.
Results
Absorbed dose to key organs and structures were assessed for a full scan with and without leaded glasses, with and without a lead thyroid shield and with and without a combination of the two shielding devices and are presented in Tables 2–5. For all scans, the combination of leaded glasses and thyroid shield yielded the greatest dose reduction for most organs. In the full scan, leaded glasses and thyroid shield reduced the dose to the eye by 74% and to the lens of the eye by 62%. The dose to the thyroid was reduced by 26%. The five other key head and neck structures and organs (brain, cranium, cervical spine, mandible and parotid) yielded similar dose reductions (Tables 6 and 7). When machine collimation was used to obtain the mandibular scans (0.2 mm and 0.4 mm resolution; Table 8), it had the greatest radiation savings effect to organs of the midface (eyes, eye lens and brain) compared with the full scan. Radiation doses to the thyroid were significantly reduced (70%) by machine collimation alone in the maxillary scan. In both cases, radiation doses to most organs were further reduced by the thyroid shield and eye glasses to levels that are considerably lower than in a full head scan (Table 9). In the mandibular scan, leaded glasses and thyroid shield reduced the dose to the eye by 4%, 13% to the lens of the eye and by 33% to the thyroid. For the maxillary scans, 0.2 mm resolution, leaded glasses and thyroid shield used together reduced the dose to the eye by 24%, to the lens of the eye by 22% and by 40% to the thyroid. For the 0.4 mm resolution maxillary scan, the dose reduction to the eye was 48%, 38% for the lens of the eye and 92% for the thyroid. Noteworthy, in the absence of shielding devices, the dose to the eye and eye lens was roughly five times greater than in the mandibular scan.
Table 2.
Adult female full head scan, glasses and thyroid shield
| Organ | cGy | SD | Weight (ICRP103) | µSv |
| Brain | 0.231 | 0.005 | 0.01 | 23.1 |
| Cranium | 0.151 | 0.004 | 0.01 | 15.1 |
| Cervical spine | 0.510 | 0.005 | 0.01 | 51.0 |
| Eye L | 0.116 | 0.001 | ||
| Eye lens L | 0.153 | 0.002 | ||
| Eye lens R | 0.132 | 0.001 | ||
| Eye R | 0.171 | 0.001 | ||
| Mandible | 0.318 | 0.009 | 0.01 | 31.8 |
| Parotid | 0.416 | 0.005 | 0.01 | 41.6 |
| Thyroid | 0.090 | 0.005 | 0.04 | 36.0 |
ICRP, International Commission on Radiological Protection; L, left; R, right; SD, standard deviation.
Scanner: i-CAT (Imaging Sciences International, Inc., Hatfield, PA); phantom: adult female, glasses and thyroid shield; field of view and time: full scan, 8.9 s.
Table 5.
Summary of the dose to the eye and lens of the eye
| Organ | GL/TS | GL/NTS | NG/TS | NG/NTS |
| Eye L (cGy) | 0.116 | 0.186 | 0.464 | 0.450 |
| Eye lens L (cGy) | 0.153 | 0.188 | 0.422 | 0.396 |
| Eye lens R (cGy) | 0.132 | 0.186 | 0.462 | 0.469 |
| Eye R (cGy) | 0.171 | 0.280 | 0.521 | 0.478 |
GL, glasses; L, left; NG, no glasses; NTS, no thyroid shield; R, right; TS, thyroid shield.
Scanner: i-CAT (Imaging Sciences International, Inc., Hatfield, PA); phantom: adult female; field of view and time: full scan, 8.9 s.
Table 6.
Comparison of results of full head scan with glasses and thyroid shield vs no glasses and no thyroid shield
| Organ | cGy | SD | Weight (ICRP103) | µSv |
| Brain | 0.386 | 0.006 | 0.01 | 38.6 |
| Cranium | 0.250 | 0.006 | 0.01 | 25.0 |
| Cervical spine | 0.744 | 0.004 | 0.01 | 74.4 |
| Eye L | 0.450 | 0.002 | ||
| Eye lens L | 0.396 | 0.004 | ||
| Eye lens R | 0.469 | 0.008 | ||
| Eye R | 0.478 | 0.003 | ||
| Mandible | 0.506 | 0.006 | 0.01 | 50.6 |
| Parotid | 0.646 | 0.004 | 0.01 | 64.6 |
| Thyroid | 0.158 | 0.002 | 0.04 | 63.2 |
ICRP, International Commission on Radiological Protection; L, left; R, right; SD, standard deviation.
Scanner: i-CAT (Imaging Sciences International, Inc., Hatfield, PA); phantom: adult female, no glasses, no thyroid shield; field of view and time: full scan, 8.9 s.
Table 7.
Comparison of leaded glasses + thyroid shield vs no glasses, no thyroid shield. Summary of the dose to eye and lens of eye during a full head scan
| Organ | GL (cGy) | TS (µSv) | NG (cGy) | NTS (µSv) |
| Brain | 0.231 | 23.1 | 0.386 | 38.6 |
| Cranium | 0.151 | 15.1 | 0.250 | 25.0 |
| Cervical spine | 0.510 | 51.0 | 0.744 | 74.4 |
| Eye L | 0.116 | 0.450 | ||
| Eye lens L | 0.153 | 0.396 | ||
| Eye lens R | 0.132 | 0.469 | ||
| Eye R | 0.171 | 0.478 | ||
| Mandible | 0.318 | 31.8 | 0.506 | 50.6 |
| Parotid | 0.416 | 41.6 | 0.646 | 64.6 |
| Thyroid | 0.900 | 36.0 | 0.158 | 63.2 |
GL, glasses; L, left; NG, no glasses; NTS, no thyroid shield; R, right; TS, thyroid shield.
Scanner: i-CAT (Imaging Sciences International, Inc., Hatfield, PA); phantom: adult female; field of view and time: full scan, 8.9 s.
Table 8.
Collimated mandibular scans (0.2 mm and 0.4 mm resolution) to the head and neck organs
| Mandible: 0.2 mm, 26.9 s |
Mandible: 0.4 mm, 8.9 s |
|||||||
| Organ | GL/TS | GL/NTS | NG/TS | NG/NTS | GL/TS | GL/NTS | NG/TS | NG/NTS |
| Brain | 0.035 | 0.030 | 0.034 | 0.032 | 0.020 | No data | 0.019 | 0.019 |
| Cranium | 0.009 | 0.008 | 0.010 | |||||
| Maxilla | 0.413 | No data | 0.415 | |||||
| Cervical spine | 0.795 | 0.795 | 0.802 | |||||
| Clavicle | 0.013 | No data | 0.006 | |||||
| Mandible | 0.825 | 0.825 | 0.683 | 0.852 | 0.344 | No data | 0.335 | 0.336 |
| Parotid | 0.741 | 0.741 | 0.805 | |||||
| Thyroid | 0.119 | 0.195 | 0.096 | 0.178 | 0.032 | No data | 0.043 | 0.110 |
| Eye L | 0.047 | 0.042 | 0.051 | 0.025 | 0.032 | No data | 0.024 | 0.038 |
| Eye lens L | 0.038 | 0.036 | 0.052 | 0.043 | 0.020 | No data | 0.025 | 0.060 |
| Eye lens R | 0.036 | 0.039 | 0.049 | 0.042 | 0.025 | No data | 0.033 | 0.080 |
| Eye R | 0.045 | 0.039 | 0.044 | 0.047 | 0.024 | No data | 0.027 | 0.084 |
GL, glasses; TS, thyroid shield; NG, no glasses; NTS, no thyroid shield.
Scan results in cGy.
Table 9.
Collimated maxillary scans (0.2 mm and 0.4 mm resolution) to head and neck organs in cGy
| Maxilla: 0.2 mm, 26.9 s |
Maxilla: 0.4 mm, 8.9 s |
|||||||
| Organ | GL/TS | GL/NTS | NG/TS | NG/NTS | GL/TS | GL/NTS | NG/TS | NG/NTS |
| Brain | 0.112 | 0.110 | 0.164 | 0.121 | 0.098 | No data | 0.071 | 0.378 |
| Cranium | 0.068 | 0.074 | ||||||
| Maxilla | 0.231 | 0.158 | 0.052 | No data | 0.070 | |||
| Cervical spine | 0.182 | 0.186 | ||||||
| Clavicle | 0.006 | 0.012 | 0.005 | No data | 0.004 | |||
| Mandible | 0.188 | 0.171 | 0.184 | 0.170 | 0.180 | No data | 0.218 | 0.126 |
| Parotid | 0.766 | 0.804 | ||||||
| Thyroid | 0.028 | 0.059 | 0.037 | 0.047 | 0.014 | No data | 0.017 | 0.181 |
| Eye L | 0.195 | 0.178 | 0.266 | 0.277 | 0.149 | No data | 0.232 | 0.329 |
| Eye lens L | 0.287 | 0.269 | 0.338 | 0.314 | 0.265 | No data | 0.228 | 0.321 |
| Eye lens R | 0.141 | 0.126 | 0.284 | 0.262 | 0.121 | No data | 0.116 | 0.290 |
| Eye R | 0.202 | 0.185 | 0.239 | 0.245 | 0.195 | No data | 0.165 | 0.328 |
GL, glasses; L, left; NG, no glasses; TS, thyroid shield; NTS, no thyroid shield; R, right.
Table 3.
Adult female full head scan, glasses and no thyroid shield
| Organ | cGy | SD | Weight (ICRP103) | µSv |
| Brain | 0.348 | 0.004 | 0.01 | 34.8 |
| Cranium | 0.187 | 0.002 | 0.01 | 18.7 |
| Cervical spine | 0.614 | 0.011 | 0.01 | 61.4 |
| Eye L | 0.186 | 0.008 | ||
| Eye lens L | 0.188 | 0.003 | ||
| Eye lens R | 0.186 | 0.006 | ||
| Eye R | 0.280 | 0.004 | ||
| Mandible | 0.488 | 0.003 | 0.01 | 48.8 |
| Parotid | 0.652 | 0.008 | 0.01 | 65.2 |
| Thyroid | 0.157 | 0.002 | 0.04 | 62.8 |
ICRP, International Commission on Radiological Protection; L, left; R, right; SD, standard deviation.
Scanner: i-CAT (Imaging Sciences International, Inc., Hatfield, PA); phantom: adult female, glasses and no thyroid shield; field of view and time: full scan, 8.9 s.
Table 4.
Adult female full head scan, no glasses and thyroid shield
| Organ | cGy | SD | Weight (ICRP103) | µSv |
| Brain | 0.371 | 0.004 | 0.01 | 37.1 |
| Cranium | 0.206 | 0.003 | 0.01 | 20.6 |
| Cervical spine | 0.239 | 0.003 | 0.01 | 23.9 |
| Eye L | 0.464 | 0.005 | ||
| Eye lens L | 0.422 | 0.004 | ||
| Eye lens R | 0.462 | 0.005 | ||
| Eye R | 0.521 | 0.004 | ||
| Mandible | 0.496 | 0.004 | 0.01 | 49.6 |
| Parotid | 0.676 | 0.005 | 0.01 | 67.6 |
| Thyroid | 0.120 | 0.005 | 0.04 | 48.0 |
ICRP, International Commission on Radiological Protection; L, left; R, right; SD, standard deviation.
Scanner: i-CAT (Imaging Sciences International, Inc., Hatfield, PA); phantom: adult female, no glasses and thyroid shield, present field of view and time: full scan, 8.9 s.
The shielding devices further reduced radiation doses to most organs. At axial levels above the thyroid shield and below the eyeglasses, no perceived changes in image sharpness, distortion or intensity of artefacts were noted. On axial images at the level of the shielding devices, a slight decrease in image definition and increased streak artefacts were noted. However, they had no significant impact on the ability to identify and evaluate major anatomic landmarks, with the exception of the lacrimal duct, which was obscured by streak artefacts when leaded glasses were used.
Discussion
In a previous study, we discussed the fact that leaded glasses can be used to reduce the amount of energy absorbed in the eye during CBCT scans and they should be worn by patients to limit the dose to the lens of the eye and reduce the risk of radiation cataract development.1 Since the lens is sensitive to radiation and the threshold for cataractogenesis is lower than previously thought, practitioners must make sure that exposures, both singular and cumulative over time, are as low as possible. Dental practitioners should consider that the size of the leaded glasses could interfere with the identification of the lacrimal duct for orthodontic tracings and decrease the image quality at axial levels between the maxillary sinus floor and the orbit.27 Smaller leaded glasses may solve the problem. A multitude of studies28–34 have shown that thyroid shielding can reduce the patient dose to the radiosensitive organs outside of the primary beam without impacting on image quality. Additionally, unshielded radiation doses to the thyroid (scatter radiation) can vary depending on the scanning technique used. With all five scanning techniques, the lead thyroid shield in conjunction with leaded glasses significantly reduced the dose to the thyroid and eye. The greatest reduction to the eye was achieved with the maxillary 0.4 mm resolution scan. For the lens of the eye, the full lead scan achieved the greatest dose reduction using both methods of shielding. The smallest dose reduction was to the eye during the mandibular 0.2 mm resolution scan. Although dental X-ray examinations are an important component of dental care, they should be taken only after a thorough clinical examination and consideration of the dental history, preferably including the study of any previous dental radiographs.17 In addition, adequate education and practical training in radiological protection should be provided for all who work with radiation in dentistry, and this is especially important in CBCT dental radiography. The basic principles recommended by the NCRP for radiation protection in dentistry15 as well as the European CBCT radiation protection guidelines9 represent important starting points for developing a comprehensive radiation protection policy with regard to CBCT utilization. The American Dental Association Council on Scientific Affairs recognized the importance of radiation protection in CBCT exams when they issued an advisory statement to notify the community that they developed collaborative guidance regarding the use of CBCT in dentistry.35 Recently, the American Thyroid Association (ATA)36 issued new guidelines on minimizing unnecessary exposure to radiation from medical and dental imaging procedures, such as the use of thyroid collars for dental X-rays. With more than 56 000 cases of thyroid cancer likely to be diagnosed in the USA in 2012, the incidence of thyroid cancer is increasing faster than any other cancer, the ATA noted. Although it is unlikely that radiation exposure is the predominant contributor to this trend, an increase in the use of diagnostic X-rays, particularly CBCT, is widespread and necessitates the protection of the thyroid gland when possible to diminish thyroid cancer risk.
In a 2005 brochure about thyroid cancer, the ATA stated that “routine X-ray exposure (e.g. dental X-rays, chest X-rays, and mammograms) does not cause thyroid cancer.”36 Although scientific knowledge at the time supported this language for the one-time use of the modalities cited, the statement did not take into account repeated exposure through diagnostic X-rays over a patient’s lifetime or the increasing use of alternative procedures, such as CT and CBCT, in which doses to the thyroid are generally much larger. This could initiate a review of radiation as a cause of thyroid cancer, with the aim of establishing a policy that would state its view on how the exposure of the thyroid to radiation should be minimized.36 Among many conclusions and recommendations, the ATA recommended in this review that “thyroid-protective collars should be used for all dental X-rays when they do not interfere with the examination”.
In our previous paper, we discussed how machine collimation significantly reduces the dose to other areas of the head and neck. Here, we also show that the use of leaded glasses in conjunction with a leaded thyroid shield reduces CBCT scan exposure to the radiosensitive eye and thyroid tissue, thereby reducing the possible risk of radiation cataract development and reducing the risks associated with radiation exposure of the thyroid gland.
Conclusions
Our data indicate that, for adult females, for five CBCT scanning techniques the use of leaded glasses and lead thyroid shielding will significantly reduce patient dose to the lens of the eye and the thyroid. As a result, the risk of developing cataracts in the eye and developing thyroid cancer is reduced. Optimization in CBCT imaging is an essential principle that should be rigorously evaluated and implemented, especially with regard to reducing radiation exposures to radiosensitive organs.
References
- 1.Prins R, Dauer LT, Colosi DC, Quinn B, Kleiman NJ, Bohle GC, et al. Significant reduction in dental cone beam computed tomography (CBCT) eye dose through the use of leaded glasses. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 112: 502–507 doi: 10.1016/j.tripleo.2011.04.041 [DOI] [PubMed] [Google Scholar]
- 2.Smith A, Shah GA, Kron T. Variation of patient dose in head CT. Br J Radiol 1998; 71: 1296–1301 [DOI] [PubMed] [Google Scholar]
- 3.Williams L, Adams C. Computed tomography of the head: an experimental study to investigate the effectiveness of lead shielding during three scanning protocols. Radiography 2006; 12: 143–152 [Google Scholar]
- 4.Shah R, Gupta AK, Rehani MM, Pandey AK, Mukhopadhyay S. Effects of reduction in tube current on reader confidence in paediatric computed tomography. Clin Radiol 2005; 60: 224–231 doi: 10.1016/j.crad.2004.08.011 [DOI] [PubMed] [Google Scholar]
- 5.Brooks S. Radiation doses of common dental radiographic examinations: a review. Acta Stomat Croat 2008; 42: 207–217 [Google Scholar]
- 6.International Commission on Radiological Protection ICRP publication 118. ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organ threshold doses for tissue reactions in a radiation protection context. Ann ICRP 2012; 41: 1–322 [DOI] [PubMed] [Google Scholar]
- 7.Friedberg EC, Walker GC, Siede W, Wood RD, Schultz RA, Ellenberger T. DNA repair and mutagenesis, part 3. 2nd edn Washington, DC: ASM Press; 2006 [Google Scholar]
- 8.SEDENTEXT Radiation protection: cone beam CT for dental and maxillofacial radiology. Evidence based guidelines. Luxembourg: European Commission, Directorate-General for Energy; Radiation Protection No. 172. ISSN; 2012. pp. 1681–6803 [Google Scholar]
- 9.BEIR VII Health risks from exposure to low levels of ionizing radiation; BEIR VII, Phase 2, Committee to Assess Health Risks From Exposure to Low Levels of Ionizing Radiation. Board of Radiation Effects, Research Division on Earth and Life Studies, National Research Council of the National Academies, National Academy of Sciences. Washington, DC: National Academies Press; 2006 [Google Scholar]
- 10.International Commission on Radiological Protection The 2007 recommendations of the International Commission on Radiolgical Protection. ICRP publication No. 103. Ann ICRP 2007; 37: 1–332 [DOI] [PubMed] [Google Scholar]
- 11.Schonfeld SJ, Lee C, Berrington de Gonzalez A. Medical exposure to radiation and thyroid cancer. Clin Oncol (R Coll Radiol) 2011; 23: 244–250 doi: 10.1016/j.clon.2011.01.159 [DOI] [PubMed] [Google Scholar]
- 12.Memon A, Godward S, Williams D, Siddique I, Al-Saleh K. Dental X-rays and the risk of thyroid cancer: a case-control study. Acta Oncol 2010; 49: 244–250 doi: 10.3109/02841861003705778 [DOI] [PubMed] [Google Scholar]
- 13.Holm LE. Radiation-induced thyroid neoplasia. Soz Praventivmed 1991; 36: 266–275 [DOI] [PubMed] [Google Scholar]
- 14.NCRP Radiation protection in dentistry. NCRP Report No. 145 Bethesda, MD: National Council on Radiation Protection and Measurements; 2004 [Google Scholar]
- 15.NCRP Risk to thyroid from ionizing radiation. NCRP Report No. 159 Bethesda, MD: Nation Council on Radiation Protection and Measurements; 2008 [Google Scholar]
- 16.Hallquist A, Hartell L, Degerman A, Wingren G, Boquist L. Medical diagnostic and therapeutic ionizing radiation and risk for thyroid cancer: a case-control study. Eur J Cancer Prev 1994; 3: 259–267 [DOI] [PubMed] [Google Scholar]
- 17.Wingren G, Hallquist A, Hartell L. Diagnostic X-ray exposure and female papillary thyroid cancer: a pooled analysis of two Swedish studies. Eur J Cancer Prev 1997; 6: 550–556 [DOI] [PubMed] [Google Scholar]
- 18.Lam EWN. Considerations for the use of ionizing radiation in dentistry. Dispatch Magazine 2011; 25: 1–12 [Google Scholar]
- 19.ICRP Radiological protection of the worker in medicine and dentistry. ICRP Publication no. 57 Ann ICRP 1990; 20 [PubMed] [Google Scholar]
- 20.Tsikiakis K, Donta C, Gavala S, Karayianni K, Kamenopoulou V, Hourdakis CJ. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol. 2005; 56: 413–417 doi: 10.1016/j.ejrad.2005.05.011 [DOI] [PubMed] [Google Scholar]
- 21.Qu XM, Li G, Sanderink GCH, Zhang ZY, Ma XC. Dose reduction of cone beam CT scanning for the entire oral and maxillofacial regions with thyroid collars. Dentomaxillofacial Radiol 2012; 41: 373–378 doi: 10.1259/dmfr/30200901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee YH, Park E, Cho PK, Sec HS, Je BK, Suh S, et al. Comparative analysis of radiation dose and image quality between thyroid shielding and unshielding during CT examination of the neck. AJR Am J Roentgenol 2011; 196: 611–615 doi: 10.2214/AJR.10.4955 [DOI] [PubMed] [Google Scholar]
- 23.Sikorski PA, Taylor KW. The effectiveness of the thyroid shield in dental radiology. Oral Surg Oral Med Oral Pathol 1984; 58: 225–236 [DOI] [PubMed] [Google Scholar]
- 24.McLaughlin DJ, Mooney RB. Dose reduction to radiosensitive tissues in CT. Do commercially available shields meet the user’s needs? Clin Radiol 2004; 59: 446–450 doi: 10.1016/j.crad.2003.10.016 [DOI] [PubMed] [Google Scholar]
- 25.Hujoel P. Thyroid shields and nck exposures in cephalometric radiography. BMC Med Imag 2006; 6: 6 Available from: http://www.biomedcentral.com/1471-2342/6/6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.CIRS Dosimetry verification phantoms, CT X-ray phantoms. 2009. [accessed 28 July 2009]. Available from: http://www.cirsinc.com/700_ct_xray.html
- 27.Colosi DC, Faber RD, Al-Najjar A, Prins R, Dauer LT, Quinn B, et al. Effect of thyroid and eye shielding on CBCT image quality.In: Proceedings of 62nd Annual Meeting American Academy of Oral and Maxillofacial Radiology; 7–10 December 2011; Chicago, IL. Chicago, IL: AAOMR; 2011 [Google Scholar]
- 28.Whitcher BL, Gratt BM, Sickles EA. Leaded shields for thyroid dose reduction in intraoral dental radiography. Oral Surg Oral Med Oral Pathol 1979; 48: 567–570 [DOI] [PubMed] [Google Scholar]
- 29.Whitcher BL, Gratt BM, Sickles EA. A leaded apron for use in panoramic dental radiography. Oral Surg Oral Med Oral Pathol 1980; 49: 467–470 [DOI] [PubMed] [Google Scholar]
- 30.Siskonen T, Tapiovaara M, Kosunen A, Lehtinen M, Variainen M. Monte Carlo simulations of occupational doses in interventional radiology. Br J Radiol 2007; 80: 460–468 doi: 10.1259/bjr/26692771 [DOI] [PubMed] [Google Scholar]
- 31.Mazonakis M, Tzedakis A, Damilaks J, Varveris H, Kachris S, Gourtsoyiannis N. Scattered dose to thyroid from prophylactic cranial irradiation during childhood: a Monte Carlo study. Phys Med Biol 2006; 51: N139–N145 doi: 10.1088/0031-9155/51/8/N01 [DOI] [PubMed] [Google Scholar]
- 32.Shortt CP, Fanning NF, Malone L, Thornton J, Brennan P, Lee MJ. Thyroid dose during neurointerventional procedures: does lead shielding reduce the dose? Cardiovasc Intervent Radiol 2007; 30: 922–927 doi: 10.1007/s00270-007-9093-7 [DOI] [PubMed] [Google Scholar]
- 33.Gunn ML, Kanal KL, Kolokythas O, Anzai Y. Radiation dose to the thyroid gland and breast from multidetector computed tomography of the cervical spine: does bismouth shielding with and without a cervical collar reduce dose? J Comp Assist Tomogr 2009; 33: 987–990 doi: 10.1097/RCT.0b013e3181a776ff [DOI] [PubMed] [Google Scholar]
- 34.Beaconsfield T, Nicholson R, Thornton A, Al-Kutoubi A. Would thyroid and breast shielding be beneficial in CT of the head? Eur Radiol 1998; 8: 664–667 [DOI] [PubMed] [Google Scholar]
- 35.The American Dental Association Council on Scientific Affairs The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2012; 143: 899–902 [DOI] [PubMed] [Google Scholar]
- 36.American Thyroid Association. 2012. Policy statement on thyroid shielding during diagnostic medical and dental radiology. [cited April 2012]. Available from: http://www.thyroid.org. [Google Scholar]