Abstract
Objectives:
To assess the position of the temporomandibular joint (TMJ) disc in patients with TMJ pain and compare it with equivalent published data of asymptomatic volunteers.
Methods:
The oblique coronal closed- and open-jaw MR images from 66 patients with TMJ pain were evaluated. Clinical examination followed the research diagnostic criteria for temporomandibular disorders. In all coronal images, the transverse condylar axis and the medial and lateral edges of the disc were determined using special software. Inter-rater agreement was calculated [two raters; inter-rater correlation coefficient (ICC)]. The presence of osteoarthrosis (OA) was determined by two independent raters. The influence of OA was estimated in patients (generalized estimation equation model). The results were compared with those of healthy volunteers (t-test). Differences between closed and open jaw in patients were analysed with the Wilcoxon matched-pair test.
Results:
The ICC was good for the transverse condylar axis (0.987) and the medial edge of the disc (0.799) and fair for the lateral edge (0.355). On average, the disc projected 5.5% to the medial side; laterally, the condyle was partially uncovered by the disc (−16.6%). In the open-jaw position, both the medial and the lateral edges shifted medially (to 17.6% vs −23.6%, Wilcoxon matched-pair test, p < 0.001). OA had no significant influence (generalized estimation equation model, p = 0.952). The disc position differed significantly from asymptomatic individuals (t-test, p < 0.001) who showed a medial disc position and full coverage of the condyle.
Conclusions:
In patients with TMJ pain, the disc seems to be smaller and located less medially than in healthy volunteers. The extent of the medial shift on opening was similar.
Keywords: temporomandibular joint, temporomandibular joint disorders, temporomandibular joint disc, magnetic resonance imaging, osteoarthritis
Introduction
The sagittal and coronal MR images have become a reference standard for the diagnosis of internal derangement of the temporomandibular joint (TMJ). Among different imaging modalities,1 MRI showed adequate agreement between the clinical examination and the imaging findings.2–4 Although oblique coronal MRI is routinely performed as part of the standard imaging procedure, there is little agreement as to its contribution to the evaluation of the transverse disc position. Coronal imaging was introduced by Katzberg et al,2 who stated that it might provide additional information and help to avoid false-negative diagnoses.3 In another study, medial or lateral disc displacement was found in 11% of cases, which had not been identified on sagittal imaging.4 The method of coronal imaging was improved by the implementation of the oblique coronal imaging plane.5,6 Nevertheless, different conventions concerning the disc position have been adopted in studies by Katzberg,7 Kurita et al8 and Tasaki et al,9 but without being validated. These conventions are based on the assumption that any shift “beyond the polar regions” of the condyle equals a disc displacement,7 a criterion that is also used in TMJ arthrography.8 Tasaki et al9 have proposed a descriptive classification for disc displacements, which is based on a study of symptom-free subjects as well as of patients with temporomandibular disorders (TMDs).
A statistical approach for a comparison of disc positions was attempted in a pilot study by Schmitter et al,10 who measured the position of the disc in oblique coronal MR images in both open- and closed-jaw positions of asymptomatic volunteers and observed a medially displaced disc in one-fifth of all healthy volunteers in the most posterior slice on coronal MRI and a medial movement of the disc when the jaw was opened.10 This result might indicate that a slightly medial position of the disc as well as the medial shift can be considered physiological. The aim of the current study was to retrospectively analyse the disc position of patients with TMDs using a validated method aligned to previous studies.
Materials and methods
Patients
This study was approved by the ethics commission of the University of Heidelberg, Germany (no. 244/2002).
We included TMD patients of the Department of Prosthodontics at the University Clinic of Heidelberg from 2002 to 2009 in this study. The criterion for inclusion in our study was the presence of TMJ pain. A joint was considered to be painful if the patient referred to pain in the history or during functional movements in the examination or if the patient had pain on palpation. Pain was attributed to the TMJ by the treating clinician as described in the research diagnostic criteria for TMDs (RDC/TMD).11
All patients underwent a functional screening, including patient history (“Do you have pain in the jaw or the facial area?” and “Have you ever experienced a limited mouth opening?”), joint noises and measurement of the maximal vertical mouth opening. If the patient answered positively to either question or displayed a mouth opening of less than 35 mm or any joint sounds, further diagnostics according to the research diagnostic criteria for TMD and, if indicated, MRI of the TMJ was performed.
After MR image acquisition, patients presenting with an anterior disc displacement, joint effusions, condylar fractures or neoplasms were excluded.
Controls
The obtained data were compared with data from 30 non-matched healthy volunteers (published data10). The process of data acquisition, imaging and image interpretation was identical for this group.
MRI
A 1.5 T MRI scanner (Symphony; Siemens, Erlangen, Germany) with TMJ surface coils was used to acquire bilateral sagittal oblique and coronal oblique images (hereafter referred to as sagittal and coronal images) of the subjects in open- or closed-jaw positions. To adjust the sagittal MR image, we obtained transverse scout images of the TMJs. Subsequently, five sagittal intermediate-weighted fast low-angle shot sections {208/10.2 [repetition time (ms)/echo time (ms)], 120 × 120 mm field of view, 256 × 256 matrix, 3 mm section thickness, 5.3 min acquisition time} were obtained: one at the lateral edge of the condyle, one at the medial edge of the condyle and three in between. All sagittal sections were oriented perpendicular to the long axis of the condyle in the transverse plane. These sagittal images were used as localizer images for coronal MRI.6 Five coronal intermediate-weighted fast low-angle shot sections (208/10.2, 120 × 120 mm field of view, 256 × 256 matrix, 3 mm section thickness, 3.5 min acquisition time) perpendicular to the axis of the TMJ disc were obtained: one through the posterior 3 mm of the disc (as the section thickness was 3 mm), one behind and three anterior to that point. To reduce image blurring owing to mandibular motion, a mechanical mouth opener (Burnett BiDirectional TMJ device; Medrad, Pittsburgh, PA) was used. All MRI examinations were performed in the Department of Neuroradiology at the University of Heidelberg.
Interpretation of MR images with respect to the disc position
Sagittal MR images were appraised by two raters (MS and LE) using the criteria described by Orsini et al.12 The intermediate zone criterion demands that the intermediate zone of the disc is located in the middle of or above a line between the centres of two circles approximating the condyle and the articular eminence, and the 11 o’clock criterion describes the position of the posterior band with respect to the condyle.
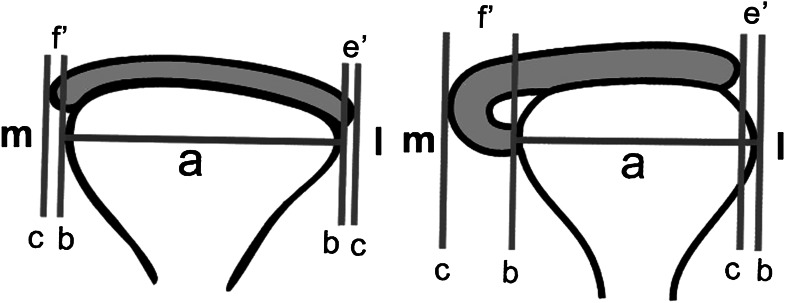
Coronal images were imported into a MathLab-based program (MathLab v. 5.3.0; The MathWorks Inc., Natick, MA) and evaluated by a standardized assessment protocol described by Schmitter et al10 (Figure 1).
Figure 1.
Schematic illustrations of left temporomandibular joint measurements in closed-jaw (left) and open-jaw positions (right). a, Longest mediolateral distance (transversal coronal axis) of the condyle; b, line perpendicular to a and tangential to the condyle; c, line parallel to b and tangential to the disc; e′, distance between b and c at the lateral aspect of the joint; f′, distance between b and c at the medial aspect of the joint; l, lateral; m, medial
Interpretation of MR images with respect to osteoarthrosis
Both the sagittal and the coronal images were evaluated for the presence of signs of osteoarthrosis (OA) by two independent raters (MS and LE). The imaging diagnosis of OA was defined as the presence of flattening, subchondral sclerosis, surface irregularities, erosion of the condyle, condylar deformities, cyst formation and osteophytes.13 Differences were resolved by consensus.
Inter-rater agreement
20 coronal images were randomly selected from all patients’ images and analysed by two raters with 1 year and 3 years of experience (LE and NNG). Both raters were blinded to the clinical findings and the sagittal image evaluation results. They independently performed the computer program-supported measurements of the coronal disc dimension. For the diagnosis of OA, 45 images were randomly chosen from non-patient images and evaluated by two independent raters with respect to the presence of OA (LE and MS).
Statistics
Inter-rater agreement was calculated as the inter-rater correlation coefficient (ICC; two-way mixed) and Cronbach’s α and was assessed.14 The comparison between open- and closed-jaw positions was evaluated with the Wilcoxon matched-pair test and Spearman’s correlation coefficient. A generalized estimation equation model was estimated for patients only to account for the effect of OA. It included again the medial disc edge as a dependent variable and an open or closed mouth, gender, right or left side and the presence or absence of OA as factors.
For the comparison with healthy volunteers (historical control group), the t-test for independent samples was used. Patients and volunteers were compared separately in the open-jaw and closed-jaw positions. All data were analysed with SPSS® v. 16.0 (SPSS Inc., Chicago, IL).
Results
Patients
A total number of 249 patients underwent MRI. 74 patients were excluded because of bilateral anterior disc displacement. Of the remaining 175 patients, 101 were excluded because of the absence of TMJ pain, 5 patients because of their age (younger than 18 years) and 3 patients because of missing data (2 MR images, 1 RDC/TMD diagnostic finding). No patients were excluded because of fractures or neoplasms.
Thus, 66 patients (44 female, 22 male) or 87 joints were included in our study because in 21 patients both joints were measured, in 29 only the right joint was measured and in 16 only the left joint was measured.
Patients had a mean age of 40.71 years (median 40.50 years, range 18–80 years).
The distribution of research diagnostic criteria for TMD diagnostic subgroups is depicted in Figure 2. Four patients had no diagnosis, but merely reported pain (N = 3) or pain on palpation (N = 1).
Figure 2.
Venn diagram of the distribution of diagnoses according to the research diagnostic criteria for temporomandibular disorders
Inter-rater agreement
The inter-rater agreement was excellent for both the transverse condylar axis (ICC = 0.987; α = 0.993) and f′ (ICC = 0.810; α = 0.888) and fair for e′ (ICC = 0.360; α = 0.524) (Figure 1). The presence or absence of OA was diagnosed with substantial agreement (ICC = 0.730).
Disc position in patients
The disc position in patients with TMD pain can be viewed in Table 1. There were significant differences between the position of the lateral rim of the disc in closed- and open-mouth positions (p = 0.032, Wilcoxon matched-pair test) as well as in the position of the medial rim of the disc in closed- and open-mouth positions (p < 0.001, Wilcoxon matched-pair test). The correlation between the disc position in closed- and open-mouth positions was r = 0.228 (p < 0.05) for the lateral and r = 0.151 (p < 0.05) for the medial rim of the disc (Spearman’s correlation coefficient).
Table 1.
Disc position in patients and volunteers. All values are in relation to the transverse condylar axis in the oblique coronal plane. Positive values indicate that the temporomandibular joint disc projects beyond the condylar poles
| Disc position | Patients |
Volunteers |
||||||
| Min | Max | Mean | SD | Min | Max | Mean | SD | |
| Closed jaw, medial distance f′ | −0.178 | 0.200 | 0.055 | 0.087 | −0.100 | 0.250 | 0.107 | 0.067 |
| Closed jaw, lateral distance e′ | −0.642 | 0.187 | −0.166 | 0.191 | −0.500 | 0.230 | 0.022 | 0.146 |
| Open jaw, medial distance f′ | −0.114 | 0.502 | 0.176 | 0.110 | 0.110 | 0.380 | 0.245 | 0.074 |
| Open jaw, lateral distance e′ | −0.858 | 0.077 | −0.237 | 0.197 | −0.310 | 0.340 | 0.092 | 0.143 |
Max, maximum; Min, minimum; SD, standard deviation.
Influence of osteoarthrosis
Imaging signs of OA were found in 22 of 87 joints. The disc position did not differ significantly in individuals with OA according to the generalized estimation equation model (p = 0.952; Table 2).
Table 2.
Influence of different parameters on the position of the medial (f′) disc margin according to the generalized estimation equation model
| p-values |
||||
| Closed vs open jaw | Osteoarthrosis (MRI) | Right or left side | Gender | |
| f′ | <0.001 | 0.952 | 0.283 | 0.620 |
Disc position in comparison with volunteers
In comparison with symptom-free volunteers, the disc position was less medial. The disc projected to the medial side with a magnitude of f′ = 5.5% as opposed to f′ = 10.7% in volunteers and 16.6% of the lateral condylar surface remained uncovered by the disc, whereas, in volunteers, the disc projected e′ = 2.2% to the lateral side (Table 1).
In the open-jaw position, the disc projected further to the medial side and a greater proportion of the lateral pole of the condyle (23.6%) was uncovered. In open-jaw images, the medial overlap f′ was not as pronounced (17.6%) as in volunteers (24.5%); laterally, however, almost one-quarter (23.6%) of the lateral aspect of the condyle was uncovered compared with 9.2% in volunteers (Table 1 and Figure 3).
Figure 3.
Two-dimensional coronal oblique intermediate fast low-angle shot MRI (208/10.2, 120 × 120 field of view, 256 × 256 matrix, 3 mm section thickness, acquisition time of 3.5 min) of the same temporomandibular joint (TMJ) in a patient with TMJ pain and schematic depiction of the mean disc position in symptom-free volunteers (arrows) and patients with TMJ pain (arrowheads) in (a) the closed-jaw position and (b) the open-mouth position
Statistically significant differences were found between the disc positions in symptom-free volunteers and those in patients with TMJ pain in the closed-jaw as well as the open-jaw positions (t-test, p < 0.001; Table 3).
Table 3.
p-values for the comparison of disc position in patients and volunteers (t-test)
| Closed jaw |
Open jaw |
|||
| Medial distance f′ | Lateral distance e′ | Medial distance f′ | Lateral distance e′ | |
| Patient vs volunteer | <0.001 | <0.001 | <0.001 | <0.001 |
There was a weak but significant correlation between the medial distance f′ and lateral distance e′ in both the closed-jaw (r = 0.32, p < 0.05) and open-jaw positions (r = 0.285, p < 0.05), whereas there was no such correlation between the disc position in the closed- and open-jaw positions (Spearman’s correlation coefficient, p < 0.05).
Discussion
The motivation for this study was to contribute to a norm of evaluation of the TMJ disc position on coronal MRI. Although there are conventions regarding the coronal disc position, there is no standard by which it can be assessed. Coronal MRI was first used to prevent false-negative diagnoses.2 Descriptive classifications categorized superior, anterior, anteromedial, anterolateral, medial and lateral positions.12 All disc positions except the superior position were considered as abnormal;7 however, it has not been shown that this assumption is correct. The study by Tasaki et al,9 based on 600 MR images of 243 patients and 57 volunteers, suggests that there is a strong association between patients and disc displacement and between volunteers and the superior disc position: disc displacements of differing extents were found in 80% of the patients, but in only 30% of the volunteers. Among them, there was an anterolateral disc displacement in 23% of patients and 9% of volunteers. However, there was no statistical evaluation of differences according to the proposed nine types of displacement and no metric comparison of disc positions between the respective groups.
A consecutive study with a similar design by Larheim and Westesson1 showed a much higher proportion of complete anterior and anterolateral disc displacements in patients with TMD than in healthy controls. Medial and lateral displacements seemed to be as common in patients as in volunteers, although this conclusion is limited by the sample size. Nevertheless, these results raise the question whether, for instance, lateral disc displacements are of pathological relevance and should be termed as displacements at all.
The problem posed is the analogous disc position on sagittal MRI, where the first and foremost central (12 o’clock) position was considered to be physiological.15 Later, it was shown that the disc position in healthy subjects varies within a physiological range,12 proving the model of the superior disc position to be too simplified.
The same can be assumed for the coronal plane, as presented by Schmitter et al,10 who seldom found a central disc position in healthy volunteers but, rather, a medial position in about one-fifth. This is in line with the findings in symptom-free patients before and after receiving orthodontic treatment,16 30% of whom showed a “medial” or “anteromedial” disc position according to the abovementioned nomenclature.12
Alterations in the position of the disc may be accompanied by joint sounds, joint pain and/or restricted mouth opening. The reason that our study focused on joint pain alone was that the diagnosis of joint sounds has no good reliability among many raters17–19 and that the sample size for patients with limited mouth opening would have been small. Additionally, there is little evidence for joint sounds in transverse disc displacements.
To draw conclusions about the possible associations between disc position and joint pain, patients with diagnoses already known to provoke joint pain, such as joint effusion, condylar fractures or neoplasms,20 were excluded.
The current study shows that the disc position in pain patients differs significantly from healthy subjects, in both closed- and open-jaw positions. As no three-dimensional information was obtained, different mechanisms could account for this fact. In particular, no conclusions on the origin of the medial “shift” of the disc on mouth opening can be drawn; translational movement, rotation or deformation of the disc can be taken into consideration.21 The position of the lateral rim of the disc has to be interpreted with caution, as the inter-rater agreement was fair. Reasons for the fair inter-rater agreement can be seen in the anatomic structures themselves: the thickness of the lateral ligament is very variable.17 The joint capsule appears to be much stronger at the lateral aspects than in other parts and, hence, is difficult to distinguish from the disc.18 Even in the evaluation of healthy volunteers, the agreement was far worse than on the medial side.10 The image quality also tends to be worse in patients; for instance, slight motion artefacts may occur owing to pain. A study on inter-rater agreement in the evaluation of MR images presented mean kappa values of less than 0.40 over the five diagnostic criteria “disc position open mouth”, “disc position closed mouth”, “direction of displacement”, “shape of the condyle” and “shape of the disc” when images of moderate to poor quality were included, but mean kappa values of 0.55 if only high-quality images were analysed.19
The reduced disc dimensions could be explained by differences in the adjustment of the MRI slices, by rotational movement or by the assumption of degenerative processes. The last may be supported by a study involving patients with anterior disc displacement, usually exhibiting reduced disc dimensions.22 However, we did not measure the thickness of the disc.
The correlation between joint pain and disc position may have multiple causes.23–25 One could argue that, because of the limited covering of the condyle by the disc, lateral joint palpation might impose direct pressure on the vulnerable exposed periosteum or the reduced covering might result in grinding of the osseous articular surfaces or pressure on the joint capsule. However, this approach has been rejected concerning disc displacements in the sagittal plane by MRI studies in healthy volunteers,26 autopsy studies27,28 and based on arthroscopic evidence.28
Disc displacement alone is unlikely to be the primary cause of pain.29 Rather, it is assumed that it is a predisposing factor increasing the risk of signs and symptoms.30,31 The altered disc position accompanies further degenerative changes that necessitate the presence of pain mediators.32 Whether changes of disc position in the coronal plane are a risk factor or a causative factor of TMJ pain or an epiphenomenon cannot be decided from this study.
One-third of the subjects in the present study presented with signs of OA. However, a statistically significant correlation to the disc position was not found except for the lateral side in the closed-mouth position. This should be viewed as a tendency only because of the fair inter-rater-agreement and p = 0.049. The assumption that OA might be the primary cause of pain cannot be supported by our study, in line with previous studies on the relationship between TMJ pain and anatomic changes in the TMJ33 and on OA in elderly people, in whom joints exhibiting OA were largely asymptomatic.34
In the absence of abnormalities on MRI, such as anterior disc displacement, joint effusion, condylar fractures or neoplasms, TMJ pain can be connected with an altered disc position in the MRI oblique coronal plane. In painful TMJs, the disc appears to be reduced in its transverse dimensions and less medially located than in healthy subjects. It seems to shift to the medial side on mouth opening to almost the same degree as in symptom-free volunteers, though. It remains to be further investigated based on larger sample sizes which diagnostic conclusions can be drawn from these observations.
Acknowledgments
The authors would like to thank Dipl.-Ing. Stefan Rues for programming the special software used in this study.
References
- 1.Larheim TA, Westesson P. TMJ imaging. In: Laskin DM, Greene CS, Hylander WL, eds. TMDs: an evidence-based approach to diagnosis and treatment. Chicago, IL: Quintessence Publishing Co, Inc; 2006 [Google Scholar]
- 2.Katzberg RW, Bessette RW, Tallents RH, Plewes DB, Manzione JV, Schenck JF, et al. Normal and abnormal temporomandibular joint: MR imaging with surface coil. Radiology 1986; 158: 183–189 [DOI] [PubMed] [Google Scholar]
- 3.Tasaki MM, Westesson PL, Kurita K, Mohl N. Magnetic resonance imaging of the temporomandibular joint. Value of axial images. Oral Surg Oral Med Oral Pathol 1993; 75: 528–531 [DOI] [PubMed] [Google Scholar]
- 4.Brooks SL, Westesson PL. Temporomandibular joint: value of coronal MR images. Radiology 1993; 188: 317–321 [DOI] [PubMed] [Google Scholar]
- 5.Musgrave MT, Westesson PL, Tallents RH, Manzione JV, Katzberg RW. Improved magnetic resonance imaging of the temporomandibular joint by oblique scanning planes. Oral Surg Oral Med Oral Pathol 1991; 71: 525–528 [DOI] [PubMed] [Google Scholar]
- 6.Hollender L, Barclay P, Maravilla K, Terry V. A new coronal imaging plane for magnetic resonance imaging of the temporomandibular joint disc. Dentomaxillofac Radiol 1998; 27: 48–50 doi: 10.1038/sj.dmfr.4600309 [DOI] [PubMed] [Google Scholar]
- 7.Katzberg RW. Temporomandibular joint imaging. Radiology 1989; 170: 297–307 [DOI] [PubMed] [Google Scholar]
- 8.Kurita K, Westesson PL, Tasaki M, Liedberg J. Temporomandibular joint: diagnosis of medial and lateral disk displacement with anteroposterior arthrography. Correlation with cryosections. Oral Surg Oral Med Oral Pathol 1992; 73: 364–368 [DOI] [PubMed] [Google Scholar]
- 9.Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop 1996; 109: 249–262 [DOI] [PubMed] [Google Scholar]
- 10.Schmitter M, Kress B, Ludwig C, Koob A, Gabbert O, Rammelsberg P. Temporomandibular joint disk position assessed at coronal MR imaging in asymptomatic volunteers. Radiology 2005; 236: 559–564 doi: 10.1148/radiol.2361040223 [DOI] [PubMed] [Google Scholar]
- 11.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6: 301–355 [PubMed] [Google Scholar]
- 12.Orsini MG, Kuboki T, Terada S, Matsuka Y, Yamashita A, Clark GT. Diagnostic value of 4 criteria to interpret temporomandibular joint normal disk position on magnetic resonance images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86: 489–497 [DOI] [PubMed] [Google Scholar]
- 13.de Leeuw R, Boering G, Stegenga B, de Bont LG. Radiographic signs of temporomandibular joint osteoarthrosis and internal derangement 30 years after nonsurgical treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 79: 382–392 [DOI] [PubMed] [Google Scholar]
- 14.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174 [PubMed] [Google Scholar]
- 15.Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology 1990; 177: 67–71 [DOI] [PubMed] [Google Scholar]
- 16.Arat FE, Arat ZM, Tompson B, Tanju S. Muscular and condylar response to rapid maxillary expansion. Part 3. Magnetic resonance assessment of condyle-disc relationship. Am J Orthod Dentofacial Orthop 2008; 133: 830–836 [DOI] [PubMed] [Google Scholar]
- 17.Ben Amor F, Carpentier P, Foucart JM, Meunier A. Anatomic and mechanical properties of the lateral disc attachment of the temporomandibular joint. J Oral Maxillofac Surg 1998; 56: 1164–1167; discussion 1168–1169 [DOI] [PubMed] [Google Scholar]
- 18.Schmolke C, Hugger A. The human temporomandibular joint region in different positions of the mandible. Ann Anat 1999; 181: 61–64 doi: 10.1016/S0940-9602(99)80091-0 [DOI] [PubMed] [Google Scholar]
- 19.Schmitter M, Kress B, Hähnel S, Rammelsberg P. The effect of quality of temporomandibular joint MR images on interrater agreement. Dentomaxillofac Radiol 2004; 33: 253–258 doi: 10.1259/dmfr/60552229 [DOI] [PubMed] [Google Scholar]
- 20.Koh KJ, List T, Petersson A, Rohlin M. Relationship between clinical and magnetic resonance imaging diagnoses and findings in degenerative and inflammatory temporomandibular joint diseases: a systematic literature review. J Orofac Pain 2009; 23: 123–139 [PubMed] [Google Scholar]
- 21.Schwaighofer BW, Tanaka TT, Klein MV, Sartoris DJ, Resnick D. MR imaging of the temporomandibular joint: a cadaver study of the value of coronal images. AJR Am J Roentgenol 1990; 154: 1245–1249 doi: 10.2214/ajr.154.6.2110737 [DOI] [PubMed] [Google Scholar]
- 22.Lemke AJ, Griethe M, Peroz I, Lange KP, Felix R. Morphometric analysis of the temporomandibular joint with MRI in 320 joints. Rofo 2005; 177: 217–228 doi: 10.1055/s-2004-813871 [DOI] [PubMed] [Google Scholar]
- 23.Emshoff R, Innerhofer K, Rudisch A, Bertram S. The biological concept of “internal derangement and osteoarthrosis”: a diagnostic approach in patients with temporomandibular joint pain? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 39–44 [DOI] [PubMed] [Google Scholar]
- 24.Emshoff R, Brandlmaier I, Gerhard S, Strobl H, Bertram S, Rudisch A. Magnetic resonance imaging predictors of temporomandibular joint pain. J Am Dent Assoc 2003; 134: 705–714 [DOI] [PubMed] [Google Scholar]
- 25.Milano V, Desiate A, Bellino R, Garofalo T. Magnetic resonance imaging of temporomandibular disorders: classification, prevalence and interpretation of disc displacement and deformation. Dentomaxillofac Radiol 2000; 29: 352–361 doi: 10.1038/sj/dmfr/4600555 [DOI] [PubMed] [Google Scholar]
- 26.Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg 1996; 54: 147–153; discussion 53–55 doi: 10.1016/j.vaccine.2012.12.045 [DOI] [PubMed] [Google Scholar]
- 27.Pereira FJ, Jr, Lundh H, Westesson PL, Carlsson LE. Clinical findings related to morphologic changes in TMJ autopsy specimens. Oral Surg Oral Med Oral Pathol 1994; 78: 288–295 [DOI] [PubMed] [Google Scholar]
- 28.Montgomery MT, Gordon SM, Van Sickels JE, Harms SE. Changes in signs and symptoms following temporomandibular joint disc repositioning surgery. J Oral Maxillofac Surg 1992; 50: 320–328 [DOI] [PubMed] [Google Scholar]
- 29.Cairns Pathophysiology of TMD pain—basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil 2010; 37: 391–410 doi: 10.1111/j.1365-2842.2010.02074.x [DOI] [PubMed] [Google Scholar]
- 30.Emshoff R, Puffer P, Rudisch A, Gassner R. Temporomandibular joint pain: relationship to internal derangement type, osteoarthrosis, and synovial fluid mediator level of tumor necrosis factor-alpha. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 442–449 doi: 10.1067/moe.2000.108801 [DOI] [PubMed] [Google Scholar]
- 31.Tallents RH, Katzberg RW, Murphy W, Proskin H. Magnetic resonance imaging findings in asymptomatic volunteers and symptomatic patients with temporomandibular disorders. J Prosthet Dent 1996; 75: 529–533 [DOI] [PubMed] [Google Scholar]
- 32.de Bont LG, Stegenga B. Pathology of temporomandibular joint internal derangement and osteoarthrosis. Int J Oral Maxillofac Surg 1993; 22: 71–74 [DOI] [PubMed] [Google Scholar]
- 33.Ohlmann B, Rammelsberg P, Henschel V, Kress B, Gabbert O, Schmitter M. Prediction of TMJ arthralgia according to clinical diagnosis and MRI findings. Int J Prosthodont 2006; 19: 333–338 [PubMed] [Google Scholar]
- 34.Schmitter M, Essig M, Seneadza V, Balke Z, Schroder J, Rammelsberg P. Prevalence of clinical and radiographic signs of osteoarthrosis of the temporomandibular joint in an older persons community. Dentomaxillofac Radiol 2010; 39: 231–234 doi: 10.1259/dmfr/16270943 [DOI] [PMC free article] [PubMed] [Google Scholar]