Abstract
Several dental implant studies have reported that radiographic evaluation of bone quality can aid in reducing implant failure. Bone quality is assessed in terms of its quantity, density, trabecular characteristics and cells. Current imaging modalities vary widely in their efficiency in assessing trabecular structures, especially in a clinical setting. Most are very costly, require an extensive scanning procedure coupled with a high radiation dose and are only partially suitable for patient use. This review examines the current literature regarding diagnostic imaging assessment of trabecular microstructure prior to oral implant placement and suggests cone beam CT as a method of choice for evaluating trabecular bone microstructure.
Keywords: dental implants, cone beam CT, microstructure
Introduction
The term “bone quality” has been extensively used in the literature to describe different aspects of bone characteristics with variable definitions depending on the context. Among inseparable factors that influence bone quality is the trabecular bone.1–4 The trabeculae or “trabecular” bone is the primary anatomical and functional unit of cancellous bone. Cortical bone helps to attain primary implant stability, but the role of cancellous bone is also remarkable. This is because cancellous bone has a higher bone turnover rate than cortical bone5 and has direct contact with the majority of the implant surface.6 Accordingly, it influences the healing and osseointegration process at the implant–bone surface.7
Bone strength has a significant role in determining implant success. To improve prediction of bone strength, the measurements of trabecular density and trabecular microstructure should be combined.8 This is because those measurements do not always denote each other. For instance, high bone density does not always correspond to high trabecular parameters such as trabecular number (Tb.N) and trabecular thickness (Tb.Th).9 Therefore, estimating implant success by assessing trabecular density alone is no longer suggested.10
Precise clinical assessment of bone structural and mechanical properties is essential in planning dental implant treatment and implant thread design.11 The task can be performed on two-dimensional (2D) plain radiographs (e.g. intraoral radiograph) by calculating fractal dimensions of trabecular bone.12 In three-dimensional (3D) imaging modalities [e.g. high-resolution peripheral quantitative CT (HR-pQCT)], high-resolution images are analysed using dedicated imaging software [e.g. CT Analyser (CTAn); Skyscan®, Kontich, Belgium]. Computational techniques such as finite element methods13,14 are also utilized in analysing 3D images to simulate the status of implant surface and the bone adjacent to the implant.11
To date, bone quality assessments in oral implant studies have largely focused on trabecular bone density.15–18 What follows is a review of the imaging techniques used in oral implant studies for assessing trabecular microstructure as evidenced in the literature. Articles that reported on trabecular microstructural imaging methods were searched in the PubMed electronic database. Titles and abstracts of the related articles were reviewed based on keywords that had initially been set as inclusion criteria: bone quality, imaging, trabecular microstructure, cone beam CT (CBCT) and dental or oral implant.
Dental radiographs
Periapical (PA) and panoramic radiographs are the first-choice diagnostic clinical instruments in dentistry. PA radiographs with superior resolution and sharpness provide valuable information for evaluating the amount and pattern of trabecular bone structure.19,20 Trabecular visibility was reported to be high on PA radiographs,21 thus enhancing its potential in trabecular imaging studies.22–27
Bone classification systems are used to study bone quality on PA images. Of the Lekholm and Zarb, Trisi and Rao, and Misch systems, the first is largely adopted in oral implant studies on trabecular bone assessment.22–25 A visual index was proposed in 1996 to simplify trabecular classification on PA radiographs.23 This index categorizes trabecular patterns according to the intertrabecular spaces (small or large) and the degree of trabeculation (sparse or dense).25–27 However, these subjective techniques remain partially validated.22
On the other hand, panoramic radiographs have also been used to assess trabecular structure.28,29 However, this technique applies the rotational principles that structures not centred in the focal trough are not sharply imaged. The formation of geometrical distortion, magnification and loss of information are thus commonly observed artefacts on panoramic radiographs. Moreover, the reduced resolution of panoramic images degrades their ability in identifying fine trabeculae.30 Therefore their application in trabecular assessments is less favourable than PA radiographs.27
Undeniably, utilizing dental radiographs for assessing trabecular microstructure is a rapid, relatively safe and convenient method to apply in the jaws. Although the nature of the 2D image could never provide information in the buccolingual direction,31 dental radiographs are still largely employed in many countries for pre-implant assessment because of availability and cost.32
The complex shapes and structure of trabecular bone can be calculated by performing fractal dimension (FD) analysis on 2D images such as PA and panoramic radiographs.30 Current studies on 2D FD analysis of trabecular microarchitecture parameters (porosity, connectivity and anisotropy) are reported to be adequately comparable to that of the 3D FD method.33
FD analyses and calculations of trabecular structures require several complex steps.25 Nowadays, FD applications are simplified by using personal computers and simple Java software (Oracle®, Los Angeles, CA). However, the overall reproducibility of the projection techniques remains a contentious issue that requires further investigation.34
MRI
MRI is a non-invasive, non-ionizing system which applies high magnetic fields, transmission of radiofrequency waves and detection of radiofrequency signals from excited hydrogen protons. Trabecular bone is filled with bone marrow that contains free protons and generates a strong MR signal.35,36 Fat and water protons in the marrow tissue are depicted as negative images. Because the trabecular structure cannot directly be visualized, this technique employs image processing to invert the negative image.37,38 Using this technique, values for implant loading and bone healing time for trabecular alveolar bone were proposed to improve implant success.39 Despite improving trabecular structure assessment, the quality of the acquired MR images is largely influenced by the field strength, pulse sequence, echo time and signal-to-noise ratio. Additionally, the measurements are affected by the selected threshold values, image-processing algorithms, complex analysis and interpretation of the images.39–41 Moreover, the availability and accessibility of MRI machines for dental practitioners remains limited.
CT
CT techniques are being progressively developed to meet the clinical needs in assessing the bone microstructure. Structural analysis of trabecular bone requires scanners with contiguous isotropic pixel resolution of less than 300 μm.42 High-resolution CT systems that are commonly employed for trabecular microstructural assessment in oral implant studies are discussed below.
Multidetector CT
The latest generation of multidetector CT (MDCT) systems has improved the resolution to 150–300 μm in plane and 300–500 μm in slice thickness.43 Trabecular microstructure parameters such as Tb.N, Tb.Th and trabecular separation (Tb.Sp) were measured using MDCT and compared with HR-pQCT.42 Although the resolution is still beyond trabecular dimensions (50–200 μm), the measurements from both techniques were highly correlated. In a human cadaver study, trabecular microstructure parameters were compared among MDCT and micro-CT and micro-CT finite element modelling.44 The study concluded that trabecular bone structure assessment using MDCT is overall feasible, although still limited by its spatial resolution. These studies were conducted using a high-resolution mode, which is not routinely used in clinical settings protocols.42,43 Consequently, although MDCT is largely employed in oral implant studies, its applicability remains mostly confined to bone density measurements.45–47
High-resolution peripheral quantitative CT
With a spatial resolution of 82 μm, this device is used for trabecular microstructural imaging. The measurements of microstructural parameters are reported to be similar to those of micro-CT (voxel size of 25 μm).48 The technology has a higher spatial resolution than MDCT; however, scanning sites are limited to the peripheral skeletal region (e.g. wrist and tibia) and accessibility is currently limited.43 Unlike MRI, microstructural assessment using high-resolution CT permits direct visualization of trabecular bone. However, the latter technique involves a relatively high radiation dose which is beyond the recommended clinical setting.38 Moreover, the results are also affected by the selected threshold, image analysis and processing techniques.49 Thus its application in oral implant imaging studies remains restricted.
Micro-CT
2D histomorphometric analysis was previously considered the gold standard for assessing trabecular size, shape, connectivity and orientation. As it is time-consuming and costly, micro-CT is now routinely employed for structural 2D or 3D evaluations of the trabecular microstructure.43,50 This non-destructive high-resolution (approaching 10 μm) method depicts the trabecular network in different grey levels according to its mineral content. It has been reported that trabecular parameters quantified by micro-CT are similar to traditional 2D histomorphometric values.35,36 As it permits high-resolution scans, in 2004 micro-CT was recommended as a gold standard imaging for ex vivo bone studies at implant sites.50 However, only studies with small-sized jaw specimens have been conducted to observe trabecular microstructure in oral implant research.6,9,18,51
Cone beam CT
CBCT systems were developed in the 1990s. In 2001, CBCT was introduced as a 3D imaging modality. Since then it has largely replaced both single- and multislice CT for diagnostic imaging in oral implants.52 Owing to the wide availability of the machines, rapid scan and processing times, high-resolution images and relatively reduced scan radiation dose and costs, the demand for CBCT images preceding implant placement has increased exponentially.53–57 Although many studies have been conducted on CBCT, the literature on its suitability in measuring trabecular bone microstructural parameters at oral implant sites remains scarce. This may be due to the insufficient resolution of past generations of CBCT systems to depict bone microstructure. The applications of CBCT in evaluating bone quality are still restricted for bone density assessment.45–47 Recently, however, a study on assessing bone microstructure described CBCT as a promising modality for analysing trabecular bone.57 Bone parameters (Tb.Th, Tb.N and Tb.Sp) at the mandibular condyle were also successfully evaluated by CBCT at a resolution of 125 μm coupled with image processing.58
The visibility of small anatomical structures with CBCT is largely influenced by the field of view (FOV) and scan setting selection.59 Visibility of trabecular microstructure is mainly determined by the chosen voxel size and signal-to-noise ratio plus image artefacts.60 In CBCT, voxel size, slice thickness, and spatial and contrast resolutions vary with respect to machine type, FOV and scan settings.59,60 Additionally, several image artefacts specific to CBCT technology could influence the effective system resolution, which could be less than the nominal system resolution expressed in voxel size alone. It has been previously stated that the accuracy of 3D measurement of anisotropic trabecular structures can be improved by performing in vivo rather than in vitro investigation.4,8 In this respect, the use of CBCT could prove appealing. As the need to evaluate the implant insertion sites prior to surgical placement has dramatically increased, CBCT should be validated as a non-invasive procedure for assessing bone microstructure.
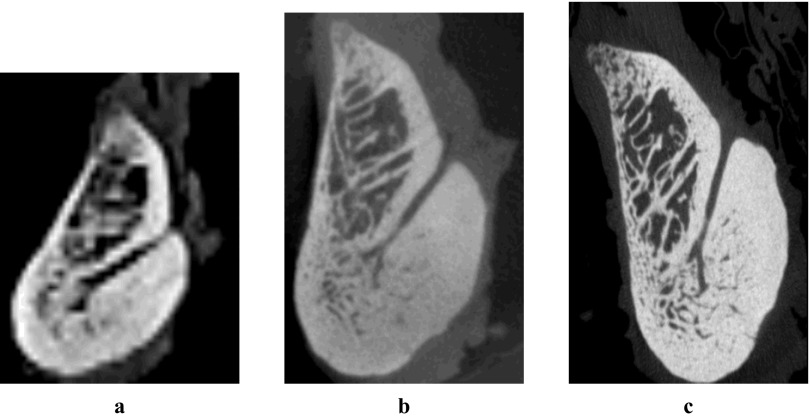
Müller et al61 have described that a CT scanner with a resolution up to 60 μm can present morphometric information similar to that of 10 μm. Using the latest CBCT system, the appearance of trabecular structures was observed using a 4 × 4 cm FOV at a nominal resolution of 80 μm. The resultant image was compared with images derived from MDCT and micro-CT (Figure 1). It is expected that this system could be useful in measuring trabecular microstructure. However, thorough investigation and validation are required prior to applying this technique in clinical practice.
Figure 1.
Sagittal images of trabecular structure at the lingual foramen region derived from (a) multidetector CT (650 μm), (b) cone beam CT (80 μm) and (c) micro-CT (35 μm)
Conclusions
Although there is rapid progress in advanced bone imaging modalities, their routine clinical employment remains limited due to the technical features, cost and complex procedures. The current review recommends studies to validate CBCT as a clinical imaging modality to evaluate trabecular microstructure at oral implant sites. More research is required to assess the influence of CBCT FOV, scan settings and image artefacts on the visibility of the trabecular microstructure.
References
- 1.Sievänen H, Kannus P, Järvinen TLN. Bone quality: an empty term. PLoS Med 2007; 4: e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Compston J. Bone quality: What is it and how is it measured? Arq Bras Endocrinol Metab 2006; 50: 579–585 [DOI] [PubMed] [Google Scholar]
- 3.Licata A. Bone density vs bone quality: What's a clinician to do? Cleve Clin J Med 2009; 76: 331–336 [DOI] [PubMed] [Google Scholar]
- 4.Fyhrie DP. Summary—measuring “bone quality”. J Musculoskelet Neuronal Interact 2005; 5: 318–320 [PubMed] [Google Scholar]
- 5.Sakka S, Coulthard P. Bone quality: a reality for the process of osseointegration. Implant Dent 2009; 18: 480–485 [DOI] [PubMed] [Google Scholar]
- 6.Fanuscu MI, Chang TL. Three-dimensional morphometric analysis of human cadaver bone: microstructural data from maxilla and mandible. Clin Oral Impl Res 2004; 15: 213–218 [DOI] [PubMed] [Google Scholar]
- 7.Minkin C, Marinho VC. Role of the osteoclast at the bone-implant interface. Adv Dent Res 1999; 13: 49–56 [DOI] [PubMed] [Google Scholar]
- 8.Müller R. Bone microarchitecture assessment: current and future trends. Osteoporos Int 2003; 14Suppl. 5: S89–S95 [DOI] [PubMed] [Google Scholar]
- 9.Gomes de Oliveira RC, Leles CR, Lindh C, Ribeiro-Rotta RF. Bone tissue microarchitectural characteristics at dental implant sites. Part 1: Identification of clinical-related parameters. Clin Oral Implants Res 2012; 23: 981–986 [DOI] [PubMed] [Google Scholar]
- 10.Wirth AJ, Goldhahn J, Flaig C, Arbenz P, Müller R, van Lenthe GH. Implant stability is affected by local bone microstructural quality. Bone 2011; 49: 473–478 [DOI] [PubMed] [Google Scholar]
- 11.DeTolla DH, Andreana S, Patra A, Buhite R, Comella B. Role of the finite element model in dental implants. J Oral Implantol 2000; 26: 77–81 [DOI] [PubMed] [Google Scholar]
- 12.Yi WJ, Heo MS, Lee SS, Choi SC, Huh KH. Comparison of trabecular bone anisotropies based on fractal dimensions and mean intercept length determined by principal axes of inertia. Med Biol Eng Comput 2007; 45: 357–364 [DOI] [PubMed] [Google Scholar]
- 13.Krug R, Burghardt AJ, Majumdar S, Link TM. High-resolution imaging techniques for the assessment of osteoporosis. Radiol Clin North Am 2010; 48: 601–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müller R, van Lenthe GH. Trabecular bone failure at the microstructural level. Curr Osteoporos Rep 2006; 4: 80–86 [DOI] [PubMed] [Google Scholar]
- 15.Turkyilmaz I, McGlumphy EA. Influence of bone density on implant stability parameters and implant success: a retrospective clinical study. BMC Oral Health 2008; 8: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turkyilmaz I, Sennerby L, McGlumphy EA, Tözüm TF. Biomechanical aspects of primary implant stability: a human cadaver study. Clin Implant Dent Relat Res 2009; 11: 113–119 [DOI] [PubMed] [Google Scholar]
- 17.Molly L. Bone density and primary stability in implant therapy. Clin Oral Implants Res 2006; 17: 124–135 [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez-Garcia R, Monje F. The reliability of cone-beam computed tomography to assess bone density at dental implant recipient sites: a histomorphometric analysis by micro-CT. Clin Oral Implants Res. 2012 Jan 17. doi: 10.1111/j.1600-0501.2011.02390.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 19.White SC, Pharoah MJ. Oral radiology: principles and interpretation. 5th edn. St Louis: Mosby; 2004 [Google Scholar]
- 20.Whaites E. Essentials of dental radiography and radiology. 3rd edn. London: Churchill Livingstone; 2007 [Google Scholar]
- 21.Couture RA, Whiting BR, Hildebolt CF, Dixon DA. Visibility of trabecular structures in oral radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 764–771 [DOI] [PubMed] [Google Scholar]
- 22.Ribeiro-Rotta RF, Lindh C, Pereira AC, Rohlin M. Ambiguity in bone tissue characteristics as presented in studies on dental implant planning and placement: a systematic review. Clin Oral Implants Res 2011; 22: 789–801 [DOI] [PubMed] [Google Scholar]
- 23.Lindh C, Petersson A, Rohlin M. Assessment of the trabecular pattern before endosseous implant treatment: diagnostic outcome of periapical radiography in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82: 335–343 [DOI] [PubMed] [Google Scholar]
- 24.Aalam AA, Nowzari H, Krivitsky A. Functional restoration of implants on the day of surgical placement in the fully edentulous mandible: a case series. Clin Implant Dent Relat Res 2005; 7: 10–16 [DOI] [PubMed] [Google Scholar]
- 25.Jonasson G, Jonasson G, Jonasson L, Kiliaridis S. Skeletal bone mineral density in relation to thickness, bone mass, and structure of the mandibular alveolar process in dentate men and women. Eur J Oral Sci 2007; 115: 117–123 [DOI] [PubMed] [Google Scholar]
- 26.Lindh C, Horner K, Jonasson G, Olsson P, Rohlin M, Jacobs R, et al. The use of visual assessment of dental radiographs for identifying women at risk of having osteoporosis: the OSTEODENT project. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 285–293 [DOI] [PubMed] [Google Scholar]
- 27.Pham D, Jonasson G, Kiliaridis S. Assessment of trabecular pattern on periapical and panoramic radiographs: A pilot study. Acta Odontol Scand 2010; 68: 91–97 [DOI] [PubMed] [Google Scholar]
- 28.Taguchi A, Suei Y, Ohtsuka M, Otani K, Tanimoto K, Ohtaki M. Usefulness of panoramic radiography in the diagnosis of postmenopausal osteoporosis in women. Width and morphology of inferior cortex of the mandible. Dentomaxillofac Radiol 1996; 25: 263–267 [DOI] [PubMed] [Google Scholar]
- 29.Watanabe PCA, Oliveira TM, Monteiro SAC, Iyomasa MM, Regalo SCH, Siessere S. Morphodigital study of the mandibular trabecular bone in panoramic radiographs. Int J Morphol 2007; 25: 875–880 [Google Scholar]
- 30.Bollen AM, Taguchi A, Hujoel PP, Hollender LG. Fractal dimension on dental radiographs. Dentomaxillofac Radiol 2001; 30: 270–275 [DOI] [PubMed] [Google Scholar]
- 31.Lofthag-Hansen S, Gröndahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res 2009; 11: 246–255 [DOI] [PubMed] [Google Scholar]
- 32.Sakakura CE, Morais JA, Loffredo LC, Scaf G. A survey of radiographic prescription in dental implant assessment. Dentomaxillofac Radiol 2003; 32: 397–400 [DOI] [PubMed] [Google Scholar]
- 33.Pothuaud L, Benhamou CL, Porion P, Lespessailles E, Harba R, Levitz P. Fractal dimension of trabecular bone projection texture is related to three-dimensional microarchitecture. J Bone Miner Res 2000; 15: 691–699 [DOI] [PubMed] [Google Scholar]
- 34.Sánchez I, Uzcátegui G. Fractals in dentistry. J Dent 2011; 39: 273–292 [DOI] [PubMed] [Google Scholar]
- 35.Genant HK, Jiang Y. Advanced imaging assessment of bone quality. Ann NY Acad Sci 2006; 1068: 410–428 [DOI] [PubMed] [Google Scholar]
- 36.Lespessailles E, Chappard C, Bonnet N, Benhamou CL. Imaging techniques for evaluating bone microarchitecture. Joint Bone Spine 2006; 73: 254–261 [DOI] [PubMed] [Google Scholar]
- 37.Jiang Y, Zhao J, White DL, Genant HK. Micro CT and Micro MR imaging of 3D architecture of animal skeleton. J Musculoskelet Neuronal Interact 2000; 1: 45–51 [PubMed] [Google Scholar]
- 38.Ito M. Recent progression in assessment of bone microstructure. Nihon Rinsho 2011;691233–691238 [PubMed] [Google Scholar]
- 39.Choël L, Last D, Duboeuf F, Seurin MJ, Lissac M, Briquet A, et al. Trabecular alveolar bone microarchitecture in the human mandible using high resolution magnetic resonance imaging. Dentomaxillofac Radiol 2004; 33: 77–182 [DOI] [PubMed] [Google Scholar]
- 40.Sell CA, Masi JN, Burghardt A, Newitt D, Link TM, Majumdar S. Quantification of trabecular bone structure using magnetic resonance imaging at 3 Tesla-calibration studies using microcomputed tomography as a standard of reference. Calcif Tissue Int 2005; 76: 355–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Celenk P, Celenk C. Evaluation by quantitative magnetic resonance imaging of trabecular bone quality in mandible and cervical vertebrae. Clin Oral Implants Res 2010; 21: 409–413 [DOI] [PubMed] [Google Scholar]
- 42.Issever AS, Link TM, Kentenich M, Rogalla P, Burghardt AJ, Kazakia GJ, et al. Assessment of trabecular bone structure using MDCT: comparison of 64- and 320-slice CT using HR-pQCT as the reference standard. Eur Radiol 2010; 20: 458–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burghardt AJ, Link TM, Majumdar S. High-resolution computed tomography for clinical imaging of bone microarchitecture. Clin Orthop Relat Res 2011; 469: 2179–2193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Issever AS, Link TM, Kentenich M, Rogalla P, Schwieger K, Huber MB, et al. Trabecular bone structure analysis in the osteoporotic spine using a clinical in vivo setup for 64-slice MDCT imaging: comparison to micro CT imaging and micro FE modelling. J Bone Miner Res 2009; 24: 1628–1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naitoh M, Aimiya H, Hirukawa A, Ariji E. Morphometric analysis of mandibular trabecular bone using cone beam computed tomography: an in vitro study. Int J Oral Maxillofac Implants 2010; 25: 1093–1098 [PubMed] [Google Scholar]
- 46.Naitoh M, Hirukawa A, Katsumata A, Ariji E. Prospective study to estimate mandibular cancellous bone density using large-volume cone-beam computed tomography. Clin Oral Implants Res 2010; 21: 1309–1313 [DOI] [PubMed] [Google Scholar]
- 47.Araki K, Okano T. The effect of surrounding conditions on pixel value of cone beam computed tomography. Clin Oral Impl Res. 2011 November 17. doi: 10.1111/j.1600-0501.2011.02373.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 48.Liu XS, Zhang XH, Sekhon KK, Adams MF, McMahon DJ, Bilezikian JP, et al. High-Resolution peripheral quantitative computed tomography can assess microstructural and mechanical properties of human distal tibial bone. J Bone Miner Res 2010; 25: 746–756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacNeil JA, Boyd SL. Accuracy of high-resolution peripheral quantitative computed tomography for measurement of bone quality. Med Eng Phys 2007; 29: 1096–1105 [DOI] [PubMed] [Google Scholar]
- 50.Yip G, Schneider P, Roberts EW. Micro-computed tomography: high resolution imaging of bone and implants in three dimensions. Semin Orthod 2004; 10: 174–187 [Google Scholar]
- 51.Swain MV, Xue J. State of the art of micro CT applications in dental research. Int J Oral Sci 2009; 1: 177–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hatcher DC. Operational principles for cone-beam computed tomography. J Am Dent Assoc 2010; 141Suppl. 3:3S–6S [DOI] [PubMed] [Google Scholar]
- 53.Al-Rawi B, Hassan B, Vandenberge B, Jacobs R. Accuracy assessment of three-dimensional surface reconstructions of teeth from cone beam computed tomography scans. J Oral Rehabil 2010; 37: 352–358 [DOI] [PubMed] [Google Scholar]
- 54.Kau CH, Bozic M, English J, Lee R, Bussa H, Ellis RK. Cone-beam computed tomography of the maxillofacial region - an update. Int J Med Robot 2009; 5: 366–380 [DOI] [PubMed] [Google Scholar]
- 55.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT) Part I. on subjective image quality. Eur J Radiol 2010; 75: 265–269 [DOI] [PubMed] [Google Scholar]
- 56.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral and Maxillofac Surg 2009; 38: 609–625 [DOI] [PubMed] [Google Scholar]
- 57.Corpas LS, Jacobs R, Quirynen M, Huang Y, Naert I, Duyck J. Peri-implant bone tissue assessment by comparing the outcome of intra-oral radiograph and cone beam computed tomography analyses to the histological standard. Clin Oral Impl Res 2011; 22: 492–499 [DOI] [PubMed] [Google Scholar]
- 58.Liu SM, Zhang ZY, Li JP, Liu DG, Ma XC. A study of trabecular bone structure in the mandibular condyle of healthy young people by cone beam computed tomography. Zhonghua Kou Qiang Yi Xue Za Zhi 2007; 42: 357–360 [PubMed] [Google Scholar]
- 59.Loubele M, Jacobs R, Maes F, Denis K, White S, Coudyzer W, et al. Image quality vs radiation dose of four cone beam computed tomography scanners. Dentomaxillofac Radiol 2008; 37: 309–318 [DOI] [PubMed] [Google Scholar]
- 60.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol 2011; 40: 265–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Müller R, Koller B, Hildebrand T, Laib A, Gianolini S, Rüegsegger P. Resolution dependency of microstructural properties of cancellous bone based on three-dimensional μ-tomography. Technol Health Care 1996; 4: 113–119 [PubMed] [Google Scholar]