Abstract
Objectives:
The purpose of this study was to evaluate the optimal upper threshold levels of a number of individuals and determine the most suitable upper threshold.
Methods:
A phantom model and ten patients were used in this study. The phantom was made of acrylic resin and urethane resin and had nine pillar-shaped air spaces. The subjects were ten female patients with jaw deformities who were not affected by respiratory disease. The optimal threshold levels were determined using the “calculation of CT value disparities” (CCTD) technique, which we devised. In other words, the mean CT values along two lines (air space and soft tissue) were calculated and the optimal threshold level was determined as the level that produced the maximum difference between the CT values measured inside and outside of the air-space border.
Results:
The optimal upper threshold levels of the nine phantom holes calculated using the CCTD technique in the front-on standing position and side-on standing position were −434 HU and −456 HU, respectively. The optimal upper threshold level of the ten patients calculated using the CCTD technique was −472 HU. The true threshold level of each patient was defined as the optimal threshold level calculated using the CCTD technique. The mean threshold level was defined as −472 HU. The absolute differences between the volume measurements obtained with these two measures were considered. Therefore, the no error values were −460 HU and −470 HU.
Conclusions:
We consider that the most suitable upper threshold level for extracting the airway is from −460 HU to −470 HU.
Keywords: obstructive sleep apnoea syndrome, CT, optimal upper threshold level
Introduction
Obstructive sleep apnoea syndrome (OSAS) has attracted attention as a cause of traffic accidents due to excessive daytime sleepiness and cognitive dysfunction, and stricture of the airway is thought to be one of the causes of OSAS. Thus, the importance of evaluations of airway morphology has been recognized. In recent years, airway morphology has been evaluated by CT, MRI and endoscopy. Among them, CT scans have been used most extensively, even though they involve irradiation, because they only involve brief X-ray exposure and are highly reproducible,1–3 and the introduction of helical (spiral) CT has dramatically changed our ability to image the hypopharynx, larynx and upper airway.4,5
Prior to the development of helical CT, conventional CT had several limitations since standard scanners require a 2–4 s scan time and a 6 s delay to return to their initial position between images. In addition, patient motion, such as breathing or swallowing, often causes blurring.6 Conversely, helical CT can scan the entire neck within a single breath-hold (30 s) in most patients because it has the ability to acquire consecutive scans.4,5 In addition, thick-section images can be obtained with helical CT. Therefore, helical CT is now widely used for evaluations of the airway.
There are many commercially available software applications for the three-dimensional (3D) modelling of CT data. 3D modelling software employing the region-growing technique requires the user to input upper and lower threshold values. For the airway, the lower threshold level is generally set at approximately −1000 HU, although this varies slightly among applications. In contrast, the upper threshold level has been given a wide variety of values by previous researchers. There are few reports about the optimal upper threshold level for extracting the airway from CT images. Zeiberg et al7 reported an optimal upper threshold level for use with the region-growing technique that was capable of measuring the true volume of the airway. However, in humans it is conceivable that there are interindividual differences in the most suitable upper threshold level because of differences in the soft tissue surrounding the airway, and the above-mentioned threshold value does not take account of these differences.
We devised a new technique, the “calculation of CT value disparities” (CCTD) technique, for determining the optimal upper threshold level. The CCTD technique has not been previously reported. In addition, this technique can be applied to humans. The purpose of this study was to devise and validate a CCTD technique and then use it to determine the most suitable upper threshold level.
Materials and methods
Materials
A phantom model and ten patients were used in this study. The phantom was made of acrylic resin and urethane resin and had nine pillar-shaped air spaces. The nine pillar-shaped air spaces were 13 mm in diameter, 50 mm in height and 26 533 mm3 in volume. The subjects were ten female patients with jaw deformities who were not affected by respiratory disease. The purpose of undertaking CT was careful examination of jaw. Their mean age was 23.1 years (range 17–38 years).
The study was approved by the ethics committee of Yamaguchi University Hospital, and all participants signed informed consent forms.
Methods
A multislice helical CT system (SOMATOM Definition; Siemens, Erlangen, Germany) was used in this study. The slice thickness of the reconstructed images was 0.6 mm.
The optimal threshold levels were determined using the CCTD technique, which we devised. The threshold level was determined using the following process: (1) regions of interest along the airway were selected on the CT images; (2) the airway was then extracted by the region-growing technique; (3) isolated points along the airway were removed by closing, erosion and dilation processes; (4) the border of the air space was outlined; (5) lines were then drawn at 1 pixel outside and inside the border of the air space; and (6) the mean CT values along these lines were calculated. The optimal threshold level was determined as the level that produced the maximum difference between the CT values measured inside and outside of the air-space border (Figures 1 and 2).
Figure 1.
The algorithm for our novel technique. The algorithm used in the calculation of CT value disparities technique is as follows: (1) the analyst selects regions of interest along the airway on three-dimensional CT images; (2) the airway is extracted via the region-growing technique; (3) isolated points along the airway are removed using closing processing; (4) the mean CT values of the regions just outside and inside of the airway are calculated; (5) the difference between the mean CT values of the two regions is calculated; (6) the threshold value associated with the greatest difference between the mean CT values of the two regions is chosen as the optimal threshold value
Figure 2.

The use of the calculation of CT value disparities technique with a phantom model. The phantom model had nine pillar-shaped air spaces. First, extract the air space (dotted area). Second, mark the border of the air space (arrow). Third, mark the line located 1 pixel inside and outside of this border (arrowhead). The difference between the mean CT values along the inside and outside of this border was measured for various threshold values
Determination of the upper threshold level using the conventional phantom technique
The differences between the true volumes of the nine phantom holes and the volumes calculated by the region-growing technique were measured at 50 HU intervals between −200 HU and −600 HU. The optimal upper threshold level was defined as the threshold that produced the smallest difference between the calculated and true volume values.
Determination of the upper threshold level using the CCTD technique in a phantom and ten patients
Using the CCTD technique, the upper threshold levels for the phantom and patients were calculated at 10 HU intervals between −800 HU and 100 HU in the front-on and side-on standing positions. The optimal upper threshold was defined as the threshold that produced the greatest difference between the mean CT values of the lines drawn 1 pixel outside and inside the air-space border.
Evaluation of the utility of the mean threshold level of the ten patients
The differences between the volume measurements calculated using each patient's true threshold level, i.e. those determined by the CCTD technique, and the volume measurements calculated using the mean threshold level of the ten patients were investigated.
Results
Determination of the upper threshold level using the conventional phantom technique
The differences between the volume estimates obtained using the conventional technique and the true volume were smallest when an upper threshold of −500 HU was used (Figure 3).
Figure 3.
Determination of the optimal upper threshold value from comparisons of the volume measurements of nine phantom holes. The differences between the true volume and the volume measurements obtained with the region-growing technique were measured. The y-axis marks the difference between measured and true volume. As a result, we found that the smallest differences between the two volume measurements were detected when a threshold value of −500 HU was used
Determination of the upper threshold level using the CCTD technique in a phantom and ten patients
The average of optimal upper threshold levels of the nine phantom holes calculated using the CCTD method in the front-on standing position was −434 HU (Figure 4). The standard deviation was −12 HU. The optimal upper threshold levels of the nine phantom holes calculated using the CCTD method in the side-on standing position was −456 HU (Figure 5). The standard deviation was −10 HU.
Figure 4.
The relationship between the upper threshold value and the difference between the mean external and internal CT values in a phantom (front-on standing position). The highest Ext. AV–Int. AV (outside the border of the air space–inside the border of the air space) values obtained for the nine phantom holes in the front-on standing position were associated with threshold values ranging from −420 HU to −450 HU. The mean threshold value was −434 HU
Figure 5.
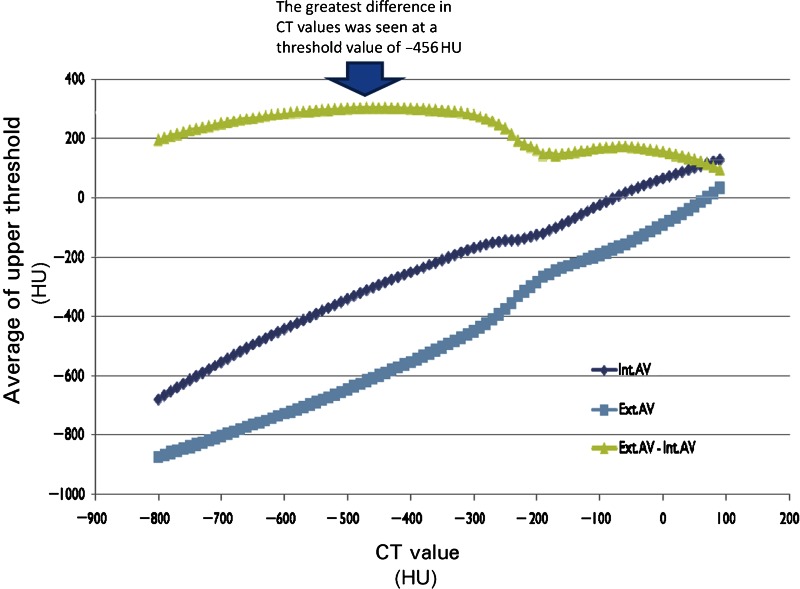
The relationship between the upper threshold value and the difference between the mean external and internal CT values in a phantom (side-on standing position). The highest Ext. AV–Int. AV (outside the border of the air space–inside the border of the air space) values obtained for the nine phantom holes in the side-on standing position were associated with threshold values ranging from −440 HU to 470 HU. The mean threshold value was −456 HU
The optimal upper threshold level of the ten patients calculated using the CCTD technique was −472 HU (Figure 6). The standard deviation was −22 HU.
Figure 6.
The relationship between the upper threshold value and the difference between the mean external and internal CT values in ten patients. The highest Ext. AV–Int. AV (outside the border of the air space–inside the border of the air space) values obtained for the ten patients were associated with threshold values ranging from −440 HU to −500 HU. The mean threshold value was −472 HU
Evaluation of the utility of the mean threshold level of the ten patients
The true threshold level of each patient was defined as the optimal threshold level calculated using the CCTD technique. The mean threshold level was defined as −472 HU. The percentage difference values were 0.0–1.1%. The mean percentage difference was 0.5% (Table 1).
Table 1.
The differences between the volume measurements obtained with the true threshold level and the mean threshold level
| Patient number | Threshold level calculated using the CCTD technique (HU) | True volume (mm3) | Volume obtained with CCTD technique (mm3) | Absolute error (mm3) | Percentage error |
| 1 | −460 | 26342.0 | 26342.0 | 0.0 | 0.0% |
| 2 | −460 | 23483.5 | 23483.5 | 0.0 | 0.0% |
| 3 | −500 | 10626.5 | 10742.5 | 116.1 | 1.1% |
| 4 | −470 | 17569.4 | 17569.4 | 0.0 | 0.0% |
| 5 | −440 | 16277.1 | 16456.9 | 179.8 | 1.1% |
| 6 | −500 | 11629.3 | 11716.4 | 87.2 | 0.7% |
| 7 | −500 | 6104.3 | 6172.1 | 67.8 | 1.1% |
| 8 | −480 | 12367.2 | 12418.0 | 50.8 | 0.4% |
| 9 | −460 | 6907.9 | 6907.9 | 0.0 | 0.0% |
| 10 | −450 | 8059.2 | 8021.9 | 37.3 | 0.5% |
| Mean | −472 | 0.5% |
The true threshold level of each patient was defined as the optimal threshold level using the calculation of CT value disparities technique. The mean threshold level was defined as −472 HU. The absolute differences between the volume measurements obtained with these two measures were 0.0 mm3, 0.0 mm3, 116.1 mm3, 0.0 mm3, 179.8 mm3, 87.2 mm3, 67.8 mm3, 50.8 mm3, 0.0 mm3 and 37.3 mm3, resulting in percentage difference values of 0.0–1.1%. The mean percentage difference was 0.5%.
Discussion
3D CT images are constructed using the region-growing technique. In this method, it is necessary to determine a range of threshold levels. The threshold level of air is defined as −1000 HU, and those of soft tissues, including muscle without fat, range from 20 to 70 HU. However, the threshold level used to extract the airway from CT images is higher than the true threshold level because the air space in the airway is influenced by partial volume effects. Therefore, defining the threshold level is extremely important when extracting the airway from CT images using the region-growing technique. 3D modelling software requires the user to input upper and lower threshold levels. Generally, the lower threshold level is set at approximately −1000 HU, but this can vary among 3D modelling software programs. Conversely, the upper threshold level has not been clearly established. Kawarai et al8 reported that the most accurate volume measurements were obtained when a threshold value within the range −1024 HU to −30 HU was used to indicate the air space. Additionally, Lan et al9 reported that the CT value of air should be set between −1024 HU and −200 HU in order to exclude fat tissue (−30 HU to −70 HU). However, the accuracy of these methods has not been examined because they use the standard threshold level for soft tissue. Zeiberg et al7 built a conical phantom for determining the optimal threshold levels so that errors in 3D models could be measured as a function of the chosen threshold levels. As a result, an upper threshold level of −500 HU was used for the patients in their study because this resulted in similar mean error values for phantoms of different sizes. We obtained similar results in a phantom study using the same method. We can examine the volumes of phantoms using the above technique, but cannot use it to examine the volumes of human organs. With regards to the airway, it is conceivable that there is a lot of interindividual variation in the optimal threshold values for humans because of differences in the soft tissue surrounding the airway. It is impossible to take account of these interindividual variations using the above-mentioned technique.
The airway contains air from the atmosphere surrounded by soft tissue including the mucosa. Thus, the airway boundary is composed of two components, air (internal) and soft tissue (external). The threshold level greatly affects the degree of contrast between the air and soft tissue within the airway on CT images. Thus, we considered that the optimal upper threshold value for extracting the airway would be the threshold value associated with the greatest difference between the CT values of the two components. Based on this idea, we devised a new technique, the CCTD technique. The main advantage of our method is that it can be used to evaluate the interindividual differences in the optimal upper thresholds of humans. As a result, we found that the optimal upper threshold ranged from −450 HU to −500 HU and that the mean value was −472 HU. Subsequently, we examined the error between the volume values obtained using each threshold level and the mean threshold level. The error was 0.5%, and zero error was detected when an upper threshold value of −460 HU or −470 HU was used. Therefore, we consider that the most suitable upper threshold level for extracting the airway ranges from −460 HU to −470 HU.
References
- 1.Li HY, Chen NH, Wang CR, Shu YH, Wang PC. Use of 3-dimensional computed tomography scan to evaluate upper airway patency for patients undergoing sleep-disordered breathing surgery. Otolaryngol Head and Neck Surg 2003; 129: 336–342 [DOI] [PubMed] [Google Scholar]
- 2.Lowe AA, Gionhaku N, Takeuchi K, Fleetham JA. Three-dimensional CT reconstructions of tongue and airway in adult subjects with obstructive sleep apnea. Am J Ortod Dentofacial Orthop 1986; 90: 364–374 [DOI] [PubMed] [Google Scholar]
- 3.Metes A, Hoffstein V, Direnfeld V, Chapnik JS, Zamel N. Three-dimensional CT reconstruction and volume measurements of the pharyngeal airway before and after maxillofacial surgery in obstructive sleep apnea. J Otolaryngol 1993; 22: 261–264 [PubMed] [Google Scholar]
- 4.Kalender WA, Polacin A, Suss C. A comparison of conventional and spiral CT: An experimental study on detection of spherical lesion. J Comput Assist Tomogr 1994; 18: 671. [DOI] [PubMed] [Google Scholar]
- 5.Polacin A, Kalender WA, Brink J, Vannier MA. Measurement of slice sensitivity profiles in spiral CT. Med Phys 1994; 21: 133–40 [DOI] [PubMed] [Google Scholar]
- 6.Silverman PM, Zeiberg AS, Sessions RB, Troost TR, Zeman RK. Three-diamensional imaging of the hypopharynx and larynx by means of helical (spiral) computed tomography. Comparison of radiological and otolaryngological evaluation. Ann Otol Rhinol Laryngol 1995; 104: 425–431 [DOI] [PubMed] [Google Scholar]
- 7.Zeiberg AS, Silverman PM, Sessions RB, Troost TR, Davros WJ, Zeman RK. Helical (Spiral) CT of the upper airway with three-dimensional imaging: technique and clinical assessment. AJR Am Roentgenol 1996; 166: 293–299 [DOI] [PubMed] [Google Scholar]
- 8.Kawarai Y, Fukushima K, Ogawa T, Nishizaki K, Gunduz M, Fujimoto M, et al. Volume quantification of healthy paranasal cavity by the three-dimensional CT imaging. Acta Otolaryngol Suppl 1999; 540: 45–49 [PubMed] [Google Scholar]
- 9.Lan Z. Evaluation of pharyngeal volume and compliance of OSAHS patients using 3D CT and volume measurement. J Kanazawa Med Univ 2004; 29: 243–251 [Google Scholar]