Abstract
The presence of a single first-rank auditory hallucination (FRAH) or bizarre delusion (BD) is sufficient to satisfy the symptom criterion for a DSM-IV-TR diagnosis of schizophrenia. We queried two independent databases to investigate how prevalent FRAH and BD are in schizophrenia spectrum disorders and whether the diagnosis depends on them. FRAH was common in both datasets (42.2% and 55.2%) and BD was present in the majority of patients (62.5% and 69.7%). However, FRAH and BD rarely determined the diagnosis. In the first database, we found only seven cases among 325 patients (2.1%) and in the second database we found only one case among 201 patients (0.5%) who were diagnosed based on FRAH or BD alone. Among patients with FRAH, 96% had delusions, 14–42% had negative symptoms, 15–21% had disorganized or catatonic behavior, and 20–23% had disorganized speech. Among patients with BD, 88–99% had hallucinations, 17–49% had negative symptoms, 20–27% had disorganized or catatonic behavior, and 21–25% had disorganized speech. We conclude that FRAH and BD are common features of schizophrenia spectrum disorders, typically occur in the context of other psychotic symptoms, and very rarely constitute the sole symptom criterion for a DSM-IV-TR diagnosis of schizophrenia.
Keywords: Schneider, first-rank symptoms, running commentary, voices conversing, diagnosis, DSM-5
1. Introduction
In the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), the diagnosis of schizophrenia can be made with just one criterion A symptom if that symptom is auditory hallucinations characterized by running commentary (RC) or voices conversing (VC), or bizarre delusions (BD) (APA, 2000). RC and VC are first-rank symptoms (FRS), proposed to distinguish schizophrenia from other psychoses (Schneider, 1959), and we will use the term first-rank auditory hallucinations (FRAH) to refer to these. BD, according to the DSM-IV-TR, are delusions that are “clearly implausible and not understandable and not derived from ordinary life experiences.” Some bizarre delusions involve the delusion of control by others, including the control of the person’s thought (thought insertion, thought withdrawal, and thought broadcasting). These delusions are also referred to as alien control or passivity phenomena. FRAH and BD were thought to be particularly characteristic of schizophrenia and were thus accorded special diagnostic significance in the DSM, beginning with the DSM-III-R (APA, 1987).
There are problems, however, with rating FRAH and BD. The inter-rater reliability for BD is variable, with kappa coefficients ranging from 0.28 to 0.92 (Flaum et al., 1991; Goldman et al., 1992; Kendler et al., 1983; Mojtabai and Nicholson, 1995; Nakaya et al., 2002; Spitzer et al., 1993; Tanenberg-Karant et al., 1995). The definition of BD is ambiguous, particularly regarding whether emphasis should be placed on form vs. content, and the validity of BD as currently operationalized in the DSM has been questioned (Cermolacce et al., 2010; Mullen, 2003). Inter-rater reliability for FRAH is higher: Peralta and Cuesta (1999) report kappa values of 0.63 for RC and 0.70 for VC; Carpenter and Strauss (1974) report r=0.76 for RC and for VC; and in the International Pilot Study of Schizophrenia (IPSS), the mean reliability for examiners within a study center was high (r=0.87) for VC (Wing and Nixon, 1975). However, reliability between study centers was still highly variable (r=0.37 to 0.95) (Wing and Nixon, 1975). Determining the prevalence of FRAH in schizophrenia has also been problematic, with estimates ranging from 10–40% for RC, 0–34% for VC, and 22–48% for cases with at least one FRAH (Ahmed and Naeem, 1984; Bland and Orn, 1980; Carpenter and Strauss, 1974; Chandrasena and Rodrigo, 1979; Gureje and Bamgboye, 1987; Lewine et al., 1982; Malik et al., 1990; Marneros, 1984; Mellor, 1970; Peralta and Cuesta, 1999; Salleh, 1992; Shinn et al., 2011; Thorup et al., 2007; Zarrouk, 1978). The variations in FRAH estimates may reflect different clinical and cultural contexts (Chandrasena, 1987), but also may be due to the variable use of narrow or wide interpretations of FRAH (Koehler, 1979; O’Grady, 1990), as well as the use of different diagnostic criteria for schizophrenia when determining FRAH base rates (Nordgaard et al., 2008). Furthermore, neither FRAH (Shinn et al., 2011) nor BD (Carpenter et al., 1973; Goldman et al., 1992) are pathognomonic of schizophrenia. Finally, FRS and BD hold little prognostic value (Brockington et al., 1978; Carpenter et al., 1973; Goldman et al., 1992; Hawk et al., 1975; Kendell et al., 1979; Nordgaard et al., 2008; Stephens et al., 1982; Strauss and Carpenter, 1972; Thorup et al., 2007).
The DSM-5 Psychotic Disorders Work Group has proposed to remove the special status of FRAH and BD from the diagnostic criteria for schizophrenia (Tandon, 2012; Tandon and Carpenter, 2012). This prompted us to ask whether this affects the “caseness” of schizophrenia. Specifically, how many cases would no longer be diagnosed with schizophrenia if special treatment of FRAH or BD were eliminated? Two studies previously answered this question in relation to BD using the DSM-III-R. Goldman et al. (1992) studied 214 consecutively admitted inpatients with psychosis and found that of the 152 broad-spectrum schizophrenia cases (schizophrenia, schizoaffective disorder, and schizophreniform disorder), 4.6% were diagnosed on the basis of BD alone. Tanenberg-Karant et al. (1995) studied 196 first-admission patients with psychosis and found that of the 96 cases with schizophrenia spectrum disorders, 7.5% were due to the sufficiency of BD. These rates have not been estimated using subsequent versions of the DSM, and the prevalence of cases diagnosed solely on the basis of FRAH has never been examined. Here, we investigated the prevalence of cases diagnosed with FRAH or BD as the solitary psychotic symptom using the DSM-IV-TR.
2. Methods
We recently published data on auditory hallucinations from a database of 569 patients with schizophrenia (n=172), schizoaffective disorder (n=153), and bipolar psychosis (n=244) (Shinn et al., 2011) at McLean Hospital. Patients were men and women, ages 18–65 years old, originally recruited for a genotype-phenotype study of psychotic and mood disorders. Individuals with disorders attributable to a general medical condition, a neurologic illness, or substance intoxication or withdrawal were excluded. We included schizoaffective disorder in addition to schizophrenia in this analysis because the special treatment of FRAH and BD pertains to the diagnostic algorithm for both of these disorders; this subset of patients (n=325; 41.5% female) had a mean age of 38.3 ± 12.2 years, mean age at psychosis onset of 21.2 ± 6.7 years, and mean duration of illness of 16.7 ± 11.9 years.
We recently published the initial results from a genotype-phenotype study of psychotic and mood disorders at Vanderbilt University (Woodward et al., 2012). For this study, we selected a sample of 201 patients with schizophrenia (n=109), schizophreniform disorder (n=57) and schizoaffective disorder (n=35), which was 34.3% female and had a mean age of 34.7 ± 12.8 years.
In both the McLean and Vanderbilt studies, participants underwent a comprehensive clinical research evaluation, including the Structured Clinical Interview for DSM-IV-TR (SCID) (First et al., 1995). In coding SCID items for running commentary (B17), two or more voices conversing (B18), and BD (B15), only scores of 3 (threshold/true) were regarded affirmatively; scores of 1 (absent/false), 2 (subthreshold), or 4 (inadequate information) were coded as negative. For each of the three symptoms, we identified cases in which the SCID item of interest was rated 3 and all other symptoms in the SCID psychosis module were rated absent. Given the frequency with which patients experience both RC and VC, we also identified cases in which B17 and B18 were both rated 3 with all other psychotic symptoms rated absent.
We assessed the presence of BD in two ways. We counted all delusion items B1-B14 that were judged to be bizarre (SCID item B15=3). As described, however, the operationalization of BD in the SCID for DSM-IV-TR is ambiguous and BD can be difficult to judge. According to the DSM-IV-TR (p. 299), “Delusions that express a loss of control over mind or body are generally considered to be bizarre; these include a person’s belief that his or her thoughts have been taken away by some outside force (“thought withdrawal”), that alien thoughts have been put into his or her mind (“thought insertion”), or that his or her body or actions are being acted on or manipulated by some outside force (“delusions of control”). Thus, in addition to item B15, we counted all unequivocal delusions of control (DC; B11), thought insertion (TI; B12), thought withdrawal (TW; B13), or thought broadcasting (TB; B14) as BD. This allowed us to combine all SCID items B11-15 scored as present into a total count of all BD cases.
In addition, to assess how common FRAH and BD are, even if accompanied by other criterion A symptoms, we calculated prevalence rates for RC, VC, and BD. To determine the association between FRAH and BD with other criterion A symptoms, we calculated the percent overlap of FRAH and BD with other criterion A symptoms. Finally, we looked at the number of criterion A symptoms that are present to meet a diagnosis of a schizophrenia spectrum disorder. As the McLean and Vanderbilt datasets were collected under different study protocols, we performed these analyses separately for the two datasets rather than combine them.
For both McLean and Vanderbilt datasets, patients were assessed by trained research staff. The 325 SCID assessments in the McLean dataset were completed by a total of 18 raters (9 psychiatrists, 2 PhD psychologists, 6 research assistants, and 1 psychiatric nurse); seven of these raters (3 psychiatrists, 1 psychologist, and 3 research assistants) completed 259 (79.7%) of all ratings. The majority (n=199, 61.2%) of the assessments were completed by raters with MD’s or PhD’s. At McLean, we carried out monthly reliability exercises where a study subject was interviewed in the presence of the research team. Each rater assessed the subject independently. Reliability was measured by the fraction of raters who showed agreement on a specific measure. Rates of agreement were perfect (1.0) for SCID diagnoses, near perfect for current mood episodes (1.0 for major depression, 0.93 for mania), and excellent for specific psychotic symptoms (0.80 for persecutory delusions, 0.85 for AH). The 201 SCID assessments in the Vanderbilt dataset were completed by a total of 11 trained research assistants, of which 2 completed 148 (73.6%) and 4 completed 172 (85.6%) of all ratings. For the Vanderbilt data, one experienced psychiatrist (S.H.) reviewed the SCID interviews, compared them with available medical records and made all final diagnoses.
3. Results
In the McLean data, we found one case (0.3%) of schizophrenia diagnosed with FRAH as the only criterion A symptom (Table 1). This patient scored 3 for both SCID items B17 and B18. This individual had no significant mood episodes. Thus, without special diagnostic weighting of FRAH, this individual would be diagnosed with psychotic disorder not otherwise specified (NOS) with isolated auditory hallucinations. We found six patients (1.8%) who received diagnoses of either schizophrenia (n=1) or schizoaffective disorder (n=5) due to BD as the sole criterion A symptom. Without special weighting, the schizophrenia patient would be diagnosed with delusional disorder. The five schizoaffective disorder patients, who in addition to BD reported mood episodes for a substantial portion of the illness duration, would be diagnosed with psychotic disorder NOS. In the Vanderbilt data, we found only one case (0.5%) of schizophrenia diagnosed with FRAH as the only criterion A symptom. Without special treatment of FRAH, this case would be diagnosed with psychotic disorder NOS with isolated auditory hallucinations. There were no cases diagnosed on the basis of BD alone in the Vanderbilt data.
Table 1.
Prevalence of Schizophrenia Cases Diagnosed on the Sole Presence of First-Rank Auditory Hallucinations (FRAH) or Bizarre Delusions (BD)
| Study | DSM Version | Sample Characteristics | Sample Size (Total) | Sample Size (Schizophrenia Spectrum Disorders) | Patients in whom FRAH was sufficient for Diagnosis | Patients in whom BD was sufficient for Diagnosis |
|---|---|---|---|---|---|---|
| Goldman et al. (1992) | DSM-III-R | Inpatients | 214 | 152 | N/A | 7 (4.6%) |
| Tanenberg-Karant et al. (1995) | DSM-III-R | First-admission inpatients | 196 | 96 | N/A | 7 (7.5%) |
| McLean Data | DSM-IV-TR | Inpatients and outpatients | 569 | 325 | 1 (0.3%) | 6 (1.8%) |
| Vanderbilt Data | DSM-IV-TR | Inpatients and outpatients | 260 | 201 | 1 (0.5%) | 0 (0.0%) |
The majority of patients had two (46.8% in the McLean data; 59.2% in the Vanderbilt data) or three (32.0% McLean; 25.4% Vanderbilt) criterion A symptoms (Figure 1). While there were only a few cases in which FRAH or BD was sufficient for diagnosis, FRAH was present in 42.2% and 55.2% of patients with schizophrenia spectrum disorders at McLean and Vanderbilt, respectively, and BD was present in 62.5% and 69.7% (Table 2). We found a large degree of overlap between FRAH or BD and other criterion A symptoms (Table 3). Most strikingly, approximately 96% of patients with FRAH also have delusions, while 88.2–98.6% of patients with BD also have hallucinations.
Figure 1.
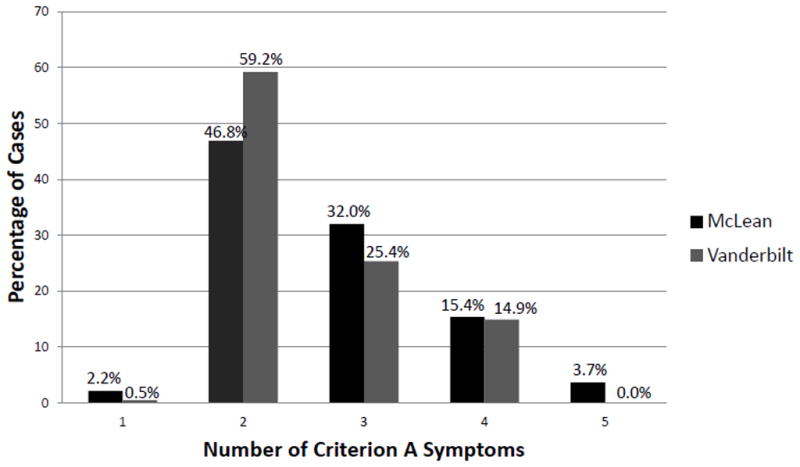
Number of Criterion A Symptoms Met to Diagnose Schizophrenia Spectrum Disorders
Table 2.
Prevalence of First-Rank Auditory Hallucinations (FRAH) and Bizarre Delusions (BD)
| SCID item = 3 | McLean Data (n=325) | Vanderbilt Data (n=201) | |
|---|---|---|---|
| FIRST-RANK AUDITORY HALLUCINATIONS | |||
| Running Commentary (RC) | B17 | 106 (32.6%) | 96 (47.8%) |
| Voices Conversing (VC) | B18 | 85 (26.2%) | 69 (34.3%) |
| RC or VC | B17 or B18 | 137 (42.2%) | 111 (55.2%) |
| BIZARRE DELUSIONS | |||
| Delusions of Control (DC) | B11 | 106 (32.6%) | 96 (47.8%) |
| Thought insertion (TI) | B12 | 88 (27.1%) | 66 (32.8%) |
| Thought withdrawal (TW) | B13 | 30 (9.2%) | 19 (9.5%) |
| Thought broadcasting (TB) | B14 | 124 (38.2%) | 99 (49%) |
| Bizarre Delusions (BD) | B15 | 57 (17.5%) | 36 (17.9 %) |
| TI/TW/TB | B12 or B13 or B14 | 165 (50.8%) | 119 (59.2%) |
| DC/TI/TW/TB | B11 or B12 or B13 or B14 | 185 (56.9%) | 132 (65.7%) |
| TI/TW/TB/BD | B12 or B13 or B14 or B15 | 187 (57.5%) | 129 (64.2%) |
| DC/TI/TW/TB/BD | B11 or B12 or B13 or B14 or B15 | 203 (62.5%) | 140 (69.7%) |
Table 3.
Overlap Between FRAH or BD and Other Criterion A Symptoms
| FRAH | BD | |||
|---|---|---|---|---|
| McLean (n=137) | Vanderbilt (n=111) | McLean (n=203) | Vanderbilt (n=140) | |
| Hallucinations | - | - | 165 (88.2%) | 138 (98.6%) |
| Delusions | 131 (95.6%) | 107 (96.4%) | - | - |
| Disorganized/Catatonic Behavior | 29 (21.2%) | 17 (15.3%) | 51 (27.3%) | 28 (20.0%) |
| Disorganized Speech | 28 (20.4%) | 25 (22.5%) | 47 (25.1%) | 30 (21.4%) |
| Negative Symptoms | 57 (41.6%) | 15 (13.5%) | 91 (48.7%) | 24 (17.1%) |
4. Conclusion
FRS, which reflect experiences of disturbed self-demarcation, and BD, as originally conceptualized (Jaspers, 1963), are common and represent important phenomenological features pertaining to self-disturbances in schizophrenia. However, as our data show, cases diagnosed on the basis of either FRAH or BD alone are exceedingly rare. We provide evidence of this from two independent datasets. The majority of patients with schizophrenia spectrum disorders have 2–3 criterion A symptoms. The vast majority of patients with FRAH have other criterion A symptoms, especially delusions and negative symptoms. Similarly, almost all patients with BD also have hallucinations, and up to a half have negative symptoms. These findings are also consistent with our previous report, which showed strong associations between auditory hallucinations and BD as well as several other schizophrenia criterion A symptoms (Shinn et al., 2011). One of the biometric principles guiding the selection of items for inclusion in diagnostic criteria is an adequate base rate (Andreasen and Flaum, 1991). Given the exceptionally low base rate of schizophrenia cases diagnosed on the sole presence of FRAH or BD, the utility of their special weighting in the diagnostic criteria for schizophrenia is questionable.
Our case estimates are lower than those reported by Goldman et al. (1992) and Tanenberg-Karant et al. (1995) (Table 1). This may be related, in part, to differences in the patient samples studied. Our study included a broad range of patients—both in- and outpatients, and chronic as well as early-stage patients. Goldman et al. (1992) included only inpatients, and Tanenberg-Karant et al. (1995), who studied only first-admission patients, found the highest prevalence. It may be more common to find patients who present with a single criterion A symptom earlier in the course of illness, and that as the disease unfolds more symptoms emerge and/or are detected. The discrepancy in estimates may also reflect changes in the definition of BD from the DSM-III-R (APA, 1987)—“involving a phenomenon that the person’s culture would regard as totally implausible”—to the DSM-IV (APA, 1994) and DSM-IV-TR (APA, 2000)—“clearly implausible and not understandable and not derived from ordinary life experiences.” While both definitions require subjective judgment, the latter DSM-IV/DSM-IV-TR definition is narrower, requiring that a delusion be un-understandable and not derived from ordinary life experiences in addition to being implausible in order to qualify as bizarre.
The ambiguous definition of BD is further complicated by the design of the SCID, which lists specific types of BD (i.e., DC, TI, TW, and TB) and then separately asks whether any delusions are bizarre (SCID item B15). In both the McLean and Vanderbilt datasets, we found that item B15 did not always reflect the presence of DC, TI, TW, or TB, even though the DSM-IV-TR gives these as examples of BD. Therefore we determined BD prevalence in our sample with item B15 only, as well as all forms of BD in the SCID.
An additional problem with SCID item B15 [which prompts the rater to assess, “IF DELUSIONAL: How do you explain (CONTENT OF DELUSION)?”] is that it takes into account only the content of BD, or what the belief is about, and ignores the form of BD, which relates to the way a belief is experienced. In the case of the latter, a delusion can be bizarre if a belief represents a significant departure from what is known about an individual’s history, values, and beliefs, even if that belief is not objectively or culturally bizarre (Mullen, 2003). The concept of bizarreness stems in large part from Jaspers’ notion of un-understandability (Jaspers, 1963). As described by Cermolacce et al. (2010), Jaspers contrasted true delusions, which lack a sense of intersubjective reality in being “non-understandable from our normal empathic stance,” from delusion-like ideas, which are often seen in mood disorders and can more readily be understood as originating from experiences or affects existing prior to the delusional manifestation. The DSM-IV’s emphasis on bizarreness of content over form has been criticized as conceptually invalid (Cermolacce et al., 2010; Mullen, 2003). Since both the McLean and Vanderbilt datasets were collected using the SCID for the DSM-IV, the form of BD was not specifically examined, and this is a limitation of the current study.
Another potential limitation of this study is that we did not examine systematically each of Schneider’s eleven FRS. We made the a priori decision to analyze only those FRS that have achieved special status in DSM. Running commentary and voices conversing are FRS that are explicitly given special weight in criterion A of DSM-IV and DSM-IV-TR; thus we included these two FRS in our analyses. How bizarre delusions relate to FRS in the DSM is less straightforward. While bizarre delusions are not FRS per se, bizarre delusions and most FRS have in common abnormal self experiences (especially relating to loss of ego-boundaries), un-understandability, and physical impossibility (Cermolacce et al., 2010), and the FRS of delusions of control, thought insertion, thought withdrawal, and thought broadcasting are given as examples of bizarre delusions in the DSM. Yet another issue is that Schneider’s FRS do not map easily onto individual items in the SCID. While “delusions of control” was not among Schneider’s eleven FRS, this symptom as operationalized in the DSM (“feelings, impulses, thoughts, or actions are experienced as being under the control of some external force”) is presented as an aggregate of Schneider’s concepts of somatic passivity, ‘made’ feelings, ‘made’ impulses, and ‘made’ volitional acts (Mellor, 1970). As such, we did not assess somatic passivity and each of the ‘made” phenomena individually. Lastly, we did not address the FRS of audible thoughts and delusional perception in this study. Since these two FRS are not included either explicitly or implicitly in criterion A for schizophrenia and are not explored sufficiently during a SCID interview, we did not include them in our analysis. The objective of the study, however, was not to examine all FRS. In spite of the limitations of the SCID, we were able to answer a very specific question—whether eliminating special treatment of FRAH and BD in the DSM affects the caseness of schizophrenia.
In conclusion, our data suggest that while FRAH and BD are common in schizophrenia, patients diagnosed on the basis of solitary FRAH or BD are rare. These symptoms have variable reliability, inconsistent frequency, lack of specificity, and poor prognostic value. In addition, the rarity of schizophrenia cases diagnosed due to RC, VC, and/or BD alone suggests that the elimination of the special Criterion A provision for these symptoms in the DSM-5 would not significantly alter the practice of diagnosing schizophrenia.
Acknowledgments
We are grateful to the patients who participated in the McLean and Vanderbilt genotype-phenotype studies. We thank Kristan Armstrong, who kindly assisted with the preparation of the Vanderbilt dataset.
FUNDING SOURCES
Collection of the McLean dataset was supported by the Shervert Frazier Research Institute and NIMH (K23MH079982 and R01MH094594) to DO. Collection of the Vanderbilt dataset was supported by NIMH grant R01-MH70560 (SH), the Vanderbilt Psychiatric Genotype/Phenotype Project, and the Vanderbilt Institute for Clinical and Translational Research (through grant 1-UL-1-RR024975 from the National Center for Research Resources/NIH).
Footnotes
CONTRIBUTORS
All three authors were involved in data collection. AKS performed the literature searches. AKS and SH analyzed the data. AKS wrote the first draft of the manuscript. All three authors contributed to the manuscript and approved the final draft.
CONFLICTS OF INTEREST
All three authors report no conflicts of interest relevant to this manuscript. Collection of the McLean dataset was supported by the Shervert Frazier Research Institute and NIMH (K23MH079982 and R01MH094594) to DO. Collection of the Vanderbilt dataset was supported by NIMH grant R01-MH70560 (SH), the Vanderbilt Psychiatric Genotype/Phenotype Project, and the Vanderbilt Institute for Clinical and Translational Research (through grant 1-UL-1-RR024975 from the National Center for Research Resources/NIH). DO is a principal investigator in a research contract with Rules Based Medicine, Inc.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmed SH, Naeem S. First rank symptoms and diagnosis of schizophrenia in developing countries. Psychopathology. 1984;17(5–6):275–279. doi: 10.1159/000284062. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Flaum M. Schizophrenia: the characteristic symptoms. Schizophr Bull. 1991;17(1):27–49. doi: 10.1093/schbul/17.1.27. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic Statistical Manual of Mental Disorders. 3. American Psychiatric Press; Washington, D.C: 1987. Revised. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Press; Washington, DC: 1994. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Press; Washington, DC: 2000. Text Revision. [Google Scholar]
- Bland RC, Orn H. Schizophrenia: Schneider’s first-rank symptoms and outcome. Br J Psychiatry. 1980;137:63–68. doi: 10.1192/bjp.137.1.63. [DOI] [PubMed] [Google Scholar]
- Brockington IF, Kendell RE, Leff JP. Definitions of schizophrenia: concordance and prediction of outcome. Psychol Med. 1978;8(3):387–398. doi: 10.1017/s0033291700016068. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Jr, Strauss JS. Cross-cultural evaluation of Schneider’s first-rank symptoms of schizophrenia: a report from the International Pilot Study of Schizophrenia. Am J Psychiatry. 1974;131(6):682–687. doi: 10.1176/ajp.131.6.682. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Jr, Strauss JS, Muleh S. Are there pathognomonic symptoms in schizophrenia? An empiric investigation of Schneider’s first-rank symptoms. Arch Gen Psychiatry. 1973;28(6):847–852. doi: 10.1001/archpsyc.1973.01750360069010. [DOI] [PubMed] [Google Scholar]
- Cermolacce M, Sass L, Parnas J. What is bizarre in bizarre delusions? A critical review. Schizophr Bull. 2010;36(4):667–679. doi: 10.1093/schbul/sbq001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasena R. Schneider’s First Rank Symptoms: an international and interethnic comparative study. Acta Psychiatr Scand. 1987;76(5):574–578. doi: 10.1111/j.1600-0447.1987.tb02921.x. [DOI] [PubMed] [Google Scholar]
- Chandrasena R, Rodrigo A. Schneider’s First Rank Symptoms: their prevalence and diagnostic implications in an Asian population. Br J Psychiatry. 1979;135:348–351. doi: 10.1192/bjp.135.4.348. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders. New York State Psychiatric Institute, Biometrics Research; New York: 1995. [Google Scholar]
- Flaum M, Arndt S, Andreasen NC. The reliability of “bizarre” delusions. Compr Psychiatry. 1991;32(1):59–65. doi: 10.1016/0010-440x(91)90070-s. [DOI] [PubMed] [Google Scholar]
- Goldman D, Hien DA, Haas GL, Sweeney JA, Frances AJ. Bizarre delusions and DSM-III-R schizophrenia. Am J Psychiatry. 1992;149(4):494–499. doi: 10.1176/ajp.149.4.494. [DOI] [PubMed] [Google Scholar]
- Gureje O, Bamgboye EA. A study of Schneider’s first-rank symptoms of schizophrenia in Nigerian patients. Br J Psychiatry. 1987;150:867–869. doi: 10.1192/bjp.150.6.867. [DOI] [PubMed] [Google Scholar]
- Hawk AB, Carpenter WT, Jr, Strauss JS. Diagnostic criteria and five-year outcome in schizophrenia. A report from the International Pilot Study of schizophrenia. Arch Gen Psychiatry. 1975;32(3):343–347. doi: 10.1001/archpsyc.1975.01760210077005. [DOI] [PubMed] [Google Scholar]
- Jaspers K. General Psychopathology. The University of Chicago Press; Chicago: 1963. [Google Scholar]
- Kendell RE, Brockington IF, Leff JP. Prognostic implications of six alternative definitions of schizophrenia. Arch Gen Psychiatry. 1979;36(1):25–31. doi: 10.1001/archpsyc.1979.01780010031002. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Glazer WM, Morgenstern H. Dimensions of delusional experience. Am J Psychiatry. 1983;140(4):466–469. doi: 10.1176/ajp.140.4.466. [DOI] [PubMed] [Google Scholar]
- Koehler K. First rank symptoms of schizophrenia: questions concerning clinical boundaries. British Journal of Psychiatry. 1979;134:236–248. doi: 10.1192/bjp.134.3.236. [DOI] [PubMed] [Google Scholar]
- Lewine R, Renders R, Kirchhofer M, Monsour A, Watt N. The empirical heterogeneity of first rank symptoms in schizophrenia. Br J Psychiatry. 1982;140:498–502. doi: 10.1192/bjp.140.5.498. [DOI] [PubMed] [Google Scholar]
- Malik SB, Ahmed M, Bashir A, Choudhry TM. Schneider’s first-rank symptoms of schizophrenia: prevalence and diagnostic use. A study from Pakistan. Br J Psychiatry. 1990;156:109–111. doi: 10.1192/bjp.156.1.109. [DOI] [PubMed] [Google Scholar]
- Marneros A. Frequency of occurrence of Schneider’s first rank symptoms in Schizophrenia. Eur Arch Psychiatry Neurol Sci. 1984;234(1):78–82. doi: 10.1007/BF00432888. [DOI] [PubMed] [Google Scholar]
- Mellor CS. First rank symptoms of schizophrenia. I. The frequency in schizophrenics on admission to hospital. II. Differences between individual first rank symptoms. Br J Psychiatry. 1970;117(536):15–23. [PubMed] [Google Scholar]
- Mojtabai R, Nicholson RA. Interrater reliability of ratings of delusions and bizarre delusions. Am J Psychiatry. 1995;152(12):1804–1806. doi: 10.1176/ajp.152.12.1804. [DOI] [PubMed] [Google Scholar]
- Mullen R. The problem of bizarre delusions. J Nerv Ment Dis. 2003;191(8):546–548. doi: 10.1097/01.nmd.0000082184.39788.de. [DOI] [PubMed] [Google Scholar]
- Nakaya M, Kusumoto K, Okada T, Ohmori K. Bizarre delusions and DSM-IV schizophrenia. Psychiatry Clin Neurosci. 2002;56(4):391–395. doi: 10.1046/j.1440-1819.2002.01027.x. [DOI] [PubMed] [Google Scholar]
- Nordgaard J, Arnfred SM, Handest P, Parnas J. The diagnostic status of first-rank symptoms. Schizophr Bull. 2008;34(1):137–154. doi: 10.1093/schbul/sbm044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Grady JC. The prevalence and diagnostic significance of Schneiderian first-rank symptoms in a random sample of acute psychiatric in-patients. Br J Psychiatry. 1990;156:496–500. doi: 10.1192/bjp.156.4.496. [DOI] [PubMed] [Google Scholar]
- Peralta V, Cuesta MJ. Diagnostic significance of Schneider’s first-rank symptoms in schizophrenia. Comparative study between schizophrenic and non-schizophrenic psychotic disorders. Br J Psychiatry. 1999;174:243–248. doi: 10.1192/bjp.174.3.243. [DOI] [PubMed] [Google Scholar]
- Salleh MR. Specificity of Schneider’s first rank symptoms for schizophrenia in Malay patients. Psychopathology. 1992;25(4):199–203. doi: 10.1159/000284772. [DOI] [PubMed] [Google Scholar]
- Schneider K. Clinical psychopathology. Grune & Stratton; New York: 1959. [Google Scholar]
- Shinn AK, Pfaff D, Young S, Lewandowski KE, Cohen BM, Ongur D. Auditory hallucinations in a cross-diagnostic sample of psychotic disorder patients: a descriptive, cross-sectional study. Compr Psychiatry. 2011 doi: 10.1016/j.comppsych.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, First MB, Kendler KS, Stein DJ. The reliability of three definitions of bizarre delusions. Am J Psychiatry. 1993;150(6):880–884. doi: 10.1176/ajp.150.6.880. [DOI] [PubMed] [Google Scholar]
- Stephens JH, Astrup C, Carpenter WT, Jr, Shaffer JW, Goldberg J. A comparison of nine systems to diagnose schizophrenia. Psychiatry Res. 1982;6(2):127–143. doi: 10.1016/0165-1781(82)90001-4. [DOI] [PubMed] [Google Scholar]
- Strauss JS, Carpenter WT., Jr The prediction of outcome in schizophrenia. I. Characteristics of outcome. Arch Gen Psychiatry. 1972;27(6):739–746. doi: 10.1001/archpsyc.1972.01750300011002. [DOI] [PubMed] [Google Scholar]
- Tandon R. The nosology of schizophrenia: toward DSM-5 and ICD-11. Psychiatr Clin North Am. 2012;35(3):557–569. doi: 10.1016/j.psc.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Tandon R, Carpenter WT., Jr DSM-5 status of psychotic disorders: 1 year prepublication. Schizophr Bull. 2012;38(3):369–370. doi: 10.1093/schbul/sbs048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanenberg-Karant M, Fennig S, Ram R, Krishna J, Jandorf L, Bromet EJ. Bizarre delusions and first-rank symptoms in a first-admission sample: a preliminary analysis of prevalence and correlates. Compr Psychiatry. 1995;36(6):428–434. doi: 10.1016/s0010-440x(95)90250-3. [DOI] [PubMed] [Google Scholar]
- Thorup A, Petersen L, Jeppesen P, Nordentoft M. Frequency and predictive values of first rank symptoms at baseline among 362 young adult patients with first-episode schizophrenia Results from the Danish OPUS study. Schizophr Res. 2007;97(1–3):60–67. doi: 10.1016/j.schres.2007.06.018. [DOI] [PubMed] [Google Scholar]
- Wing J, Nixon J. Discriminating symptoms in schizophrenia. A report from the international pilot study of schizophrenia. Arch Gen Psychiatry. 1975;32(7):853–859. doi: 10.1001/archpsyc.1975.01760250045004. [DOI] [PubMed] [Google Scholar]
- Woodward ND, Karbasforoushan H, Heckers S. Thalamocortical dysconnectivity in schizophrenia. Am J Psychiatry. 2012;169(10):1092–1099. doi: 10.1176/appi.ajp.2012.12010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarrouk ET. The usefulness of first-rank symptoms in the diagnosis of schizophrenia in a Saudi Arabian population. Br J Psychiatry. 1978;132:571–573. doi: 10.1192/bjp.132.6.571. [DOI] [PubMed] [Google Scholar]


