Abstract
This report prospectively examines the course of body dysmorphic disorder (BDD) for up to 8 years in a sample of 514 participants in the Harvard/Brown Anxiety Research Project, a naturalistic, longitudinal study of anxiety disorders. Diagnostic and Statistical Manual of Mental Disorders (4th ed.) BDD was assessed with a reliable semi-structured measure. For participants with BDD, severity of BDD symptoms was assessed with the Longitudinal Interval Follow-up Evaluation Psychiatric Status Rating scale. At the initial assessment, 17 participants (3.3%; 95% confidence interval = 1.8%–4.8%) had current BDD; 22 (4.3%; 95% confidence interval = 2.6%–6.1%) had lifetime BDD. Participants with BDD had significantly lower Global Assessment Scale scores than those without BDD, indicating poorer functioning. The probability of full recovery from BDD was 0.76, and probability of recurrence, once remitted, was 0.14 over the 8 years. In conclusion, among individuals ascertained for anxiety disorders, the probability of recovering from BDD was relatively high and probability of BDD recurrence was low.
Keywords: Body dysmorphic disorder, anxiety disorders, course, recovery, recurrence
Body dysmorphic disorder (BDD), a distressing or impairing preoccupation with an imagined or slight defect in physical appearance, is a relatively common disorder that is associated with markedly poor functioning and quality of life (Koran et al., 2008; Phillips and Diaz, 1997; Phillips et al., 2005b). Although BDD has been consistently described for more than a century, systematic research on this disorder has been done only in the past 2 decades.
One important area of investigation is course of illness. A chart-review study and 2 cross-sectional/retrospective studies suggest that the course of BDD is often chronic (Phillips and Diaz, 1997; Phillips et al., 2005a, b). To our knowledge, the only prospective, observational, longitudinal study of BDD is the BDD Longitudinal Interview Study, in which most participants had a primary diagnosis of BDD and the probability of full recovery from BDD over 1 year of follow-up was only 0.09 (Phillips et al., 2005c, 2006).
Further studies on the course of BDD are needed to more fully understand the disorder and facilitate treatment development. This study examines the course of BDD in participants in the Harvard/Brown Anxiety Research Project (HARP), a prospective, observational, longitudinal study on individuals with a Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R anxiety disorder (Massion et al., 1993). To our knowledge, this is the longest prospective assessment of the course of BDD that has been done so far.
METHOD
This study was conducted using data from the HARP, a naturalistic, longitudinal follow-up study on adults with a current or chronic DSM-III-R defined target diagnosis of panic disorder (with or without agoraphobia), agoraphobia without a history of panic disorder, generalized anxiety disorder, or social phobia. Subjects had to be at least 18 years of age, capable of participating voluntarily in the study, and able to sign a written consent form. Exclusion criteria were presence of an organic mental disorder or psychotic disorder within 6 months prior to entry into the study. Participants were recruited from psychiatry clinics of 11 hospitals in Massachusetts and Rhode Island. The study was approved by the Institutional Review Board at each site, and all subjects provided written informed consent. Study methods are described in detail elsewhere (Keller et al., 1994; Massion et al., 1993). This report presents data for the 514 participants who were assessed for DSM-IV BDD.
The initial comprehensive evaluation at the HARP study intake, conducted by trained clinical interviewers, assessed lifetime psychiatric history using the SCALUP, which included items from the reliable Structured Clinical Interview for DSM-III-R Non-Affective Disorders, Patient Version (Spitzer et al., 1990) and the Research Diagnostic Criteria Schedule for Affective Disorders-Lifetime (Endicott and Spitzer, 1978). Assessment at intake included demographic variables and the reliable Global Assessment Scale (GAS; Endicott et al., 1976), which is an earlier version of the Global Assessment of Functioning (American Psychiatric Association, 2000) scale. The GAS rates individuals’ overall psychopathology and psychosocial functioning on a 0 to 100 scale where 1 refers to the most severely ill individuals and 100 to the healthiest individuals. The presence of DSM-IV BDD was assessed with the reliable BDD Diagnostic Module, a semi-structured interview, beginning in year 5 of the HARP study (Phillips, 2005). The delusionality of BDD beliefs (e.g., “I look like a freak”) was assessed using item number 11 from the reliable and valid Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder (Phillips et al., 1997). Training in the assessment of BDD was provided by K.A.P.
For the study presented here, follow-up interviews were conducted annually, using the Longitudinal Interval Follow-Up Evaluation (LIFE), which has been shown to have good psychometric properties (Keller et al., 1987). The LIFE employs the Psychiatric Status Rating (PSR) scale to indicate the severity of DSM-defined disorders. In this study, a period of full recovery was defined prospectively as minimal or no symptoms of BDD (PSR of 1 or 2) for at least 8 consecutive weeks. This definition is the standard definition of recovery used in HARP, and it has been widely used in other studies (Keller et al., 1994). Recurrence was defined as the occurrence of symptoms at a PSR level of 5 or greater (i.e., meeting full DSM criteria) for 4 consecutive weeks after recovery.
SAS version 9.1 (SAS Institute Inc., Cary, NC) was used for analyses. Means, standard deviations, and frequencies were calculated for intake data. Differences between those with lifetime BDD versus those without a history of BDD for intake data were explored using chi square analyses for categorical variables and t tests for continuous variables. The tests were 2-tailed, and the alpha level was 0.05. Kaplan-Meier life tables were constructed for time to full recovery.
RESULTS
At the initial assessment, 17 (3.3%; 95% confidence interval = 1.8%–4.8%) participants had current DSM-IV BDD; 22 (4.3%; 95% confidence interval = 2.6%–6.1%) had lifetime BDD. Of the individuals with lifetime BDD, the mean age was 38.1 (standard deviation = 10.8), and 16 (72.7%) were females. About one-third were currently married (36.4%). Mean age at onset of BDD in this sample was 17.3 (standard deviation = 10.4). More than half of the individuals with BDD had BDD beliefs that were characterized by poor insight (45.5%) or delusional thinking (9.1%). This was a relatively educated sample (with 45.5% having completed college or a higher level of education). However, fewer than one-third of the BDD participants were working full time (27.3%).
There were no significant differences on demographic variables between participants with and without lifetime BDD (Table 1). Individuals with BDD had significantly lower scores on the GAS, t(511) = 2.03, p = 0.043. There were no significant differences found in lifetime comorbidity between the 2 groups. However, at a trend level, individuals with BDD were more likely to be diagnosed with generalized anxiety disorder (χ2 = 3.20, df = 1, p = 0.091) and less likely to be diagnosed with panic disorder with agoraphobia (χ2 = 3.69, df = 1, p = 0.073) than individuals without BDD.
TABLE 1.
Demographic and Clinical Characteristics of 514 Individuals With and Without Lifetime BDD
| Variables | With BDD (n = 22) | Without BDD (n = 492) | χ2 or t | p |
|---|---|---|---|---|
| Demographic variables | ||||
| Age (mean ± SD) | 38.1 ± 10.8 | 40.4 ± 11.7 | 0.90 | 0.369 |
| Gender (% female) | 16 (72.7%) | 339 (68.9%) | 0.14 | 0.817 |
| Marital status (currently married) | 8 (36.4%) | 268 (54.5%) | 2.77 | 0.126 |
| Education (completed college) | 10 (45.5%) | 187 (38.2%) | 0.46 | 0.509 |
| Employment (working full time) | 6 (27.3%) | 222 (45.1%) | 2.72 | 0.125 |
| Psychosocial functioning/symptom severity | ||||
| GAS score (mean ± SD) | 56.4 ± 11.8 | 61.3 ± 11.1 | 2.03 | 0.043 |
| Comorbidity (lifetime) | ||||
| Panic disorder without agoraphobia | 5 (22.7%) | 86 (17.5%) | 0.40 | 0.566 |
| Panic disorder with agoraphobia | 9 (40.9%) | 302 (61.4%) | 3.69 | 0.073 |
| Agoraphobia without history of panic disorder | 2 (9.1%) | 31 (6.3%) | 0.37 | 0.645 |
| Social phobia | 9 (40.9%) | 127 (25.8%) | 2.47 | 0.138 |
| Generalized anxiety disorder | 10 (45.5%) | 137 (27.9%) | 3.20 | 0.091 |
| Obsessive-compulsive disorder | 6 (27.3%) | 80 (16.3%) | 1.83 | 0.236 |
| Post-traumatic stress disorder | 2 (9.1%) | 43 (8.7%) | 0.003 | 1.0 |
| Specific phobia | 4 (18.2%) | 89 (18.1%) | 0.000 | 1.0 |
| Major depressive disorder | 16 (72.7%) | 273 (55.5%) | 2.54 | 0.128 |
| Alcohol dependence or abuse | 7 (31.8%) | 135 (27.4%) | 0.20 | 0.632 |
| Drug dependence or abuse | 5 (22.7%) | 77 (15.7%) | 0.79 | 0.372 |
BDD indicates body dysmorphic disorder; SD, standard deviation; GAS, Global Assessment Scale.
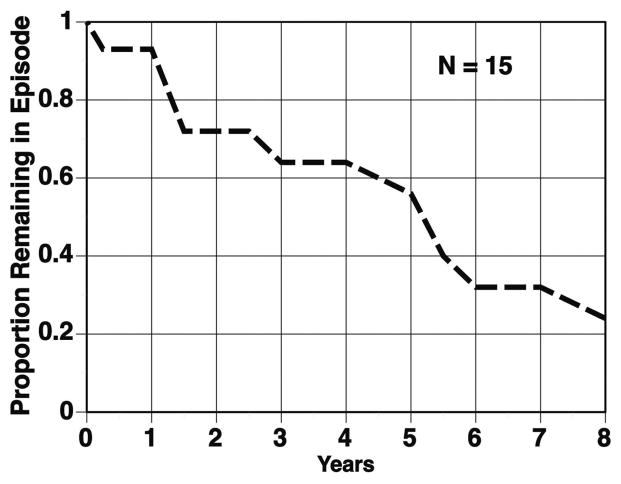
The probability of full recovery from BDD over 8 years was 0.76 (Fig. 1), allowing for censoring; 2 participants were lost to follow-up. One participant was lost to follow-up at the 1-year follow-up and the other at the 2-year follow-up. As can be seen in Figure 1, the recovery curve is steep for the first 1.5 years, then relatively stable, with another steep slope between years 5 and 6 before leveling off again. Of the 10 participants who recovered, only 1 subsequently suffered recurrence of BDD. The probability of recurrence, once recovered, was 0.14, allowing for censoring.
FIGURE 1.
Probability of full recovery from BDD in HARP.
DISCUSSION
The prevalence of BDD in this sample was higher than what has been found in the general population (Koran et al., 2008) but somewhat lower (3.3% current and 4.3% lifetime) than in 2 other studies of anxiety disorders, which reported a current prevalence of BDD of 6.7% (Wilhelm et al., 1997) and 5% (Brawman-Mintzer et al., 1995). Studies have typically found a higher prevalence of BDD among individuals who are ascertained for certain anxiety disorders, such as obsessive-compulsive disorder, where the prevalence of BDD ranges from 3% to 37%, with a mean of about 17% (Phillips and Kaye, 2007). Demographic variables examined in the present study, such as age at onset and marital status, were similar to those in past studies of BDD (Koran et al., 2008; Phillips and Diaz, 1997; Phillips et al., 2005b). In the present study, BDD subjects had significantly lower GAS scores than subjects without BDD, indicating lower overall psychosocial functioning and greater symptom severity. However, the GAS scores for BDD participants in HARP were higher than scores on the Global Assessment of Functioning (a later version of the GAS) in studies that ascertained subjects for BDD (Phillips and Diaz, 1997; Phillips et al., 2005b), suggesting that the BDD participants in HARP were not as severely symptomatic or functionally impaired as participants in the BDD studies. In the present study, individuals with BDD were more likely to be diagnosed with generalized anxiety disorder and less likely to be diagnosed with panic disorder with agoraphobia at a trend level only, which might represent chance association or insufficient statistical power to reveal significant differences in the population.
The probability of fully recovering from BDD (0.76) over 8 years of prospective follow-up was high. Although the small BDD sample size limits comparisons to other disorders, the probability of fully recovering from BDD over 8 years was in the range reported during this period of time for major depressive disorder (0.70) and panic disorder without agoraphobia (0.72) in HARP, but higher than that for panic disorder with agoraphobia (0.38), generalized anxiety disorder (0.46), and social phobia (0.29) in HARP (Keller, 2006).
After 1 year of follow-up, the probability of full recovery from BDD in HARP (0.13) (Fig. 1) was somewhat higher than after 1 year of prospective follow-up in the BDD Longitudinal Interview Study (0.09), which ascertained subjects for BDD and used nearly identical methods to those used in HARP (Phillips et al., 2005c, 2006). A possible reason for the somewhat higher BDD recovery rate in HARP is that the severity of BDD was likely to be greater in the BDD study. In the BDD Longitudinal Interview Study, greater severity of BDD symptoms at study intake predicted a lower probability of recovery from BDD (Phillips et al., 2005c). The probability of recovery from BDD in the present study was notably higher than in 2 retrospective studies of BDD. In the latter studies, in which subjects had a mean duration of illness of about 16 years, a notably low proportion of participants—only 18% to 19%—reported recovery of BDD for at least 1 month during the course of their illness (Phillips and Diaz, 1997; Phillips et al., 2005b). Possible explanations for the far lower recovery rate in these latter studies compared with HARP is that participants in the BDD studies may have been more severely ill, and the retrospective methodology that was used may not have detected all periods of recovery. However, the probability of full recovery from BDD after 4 years in HARP (0.36) was lower than that in a chart-review study of 95 outpatients with BDD who were treated in a specialty BDD setting (0.58 over 4 years) (Phillips et al., 2005a). A likely explanation for this difference is that patients in the chart-review study received treatment that specifically targeted their BDD symptoms.
Probability of recurrence after recovery from BDD in HARP was low (only 0.14). In fact, the probability of recurrence in HARP over 8 years was similar to that in the BDD Longitudinal Interview Study over only 1 year of prospective follow-up (0.15) (Phillips et al., 2006). This finding, too, may perhaps be explained by less severe BDD symptoms at intake in HARP compared with the BDD Longitudinal Interview Study. This possible explanation needs to be examined in future studies.
One limitation of this study is the relatively small number of participants with BDD, which may have increased the risk of Type II error. Furthermore, all participants were ascertained for anxiety disorders, and it is not clear whether these results can be generalized to other populations of individuals with BDD, for example, those in the community or other clinical settings, including settings that specialize in BDD. Strengths of this study include its prospective, longitudinal design, use of widely used definitions of recovery and recurrence, rigorous training of raters, use of LIFE methodology, and the longest follow-up period during which BDD has been prospectively assessed.
CONCLUSIONS
In summary, the probability of recovery from BDD over 8 years of prospective follow-up was relatively high, and probability of recurrence after recovery was fairly low. Future studies on the course of BDD are greatly needed, with larger samples and in different settings.
Acknowledgments
Supported by K23MH69595 (to R.B.W.), 5RO1MH51415-14 (to M.B.K.), and K24MH063975 (to K.A.P.).
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington (DC): American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Brawman-Mintzer O, Lydiard RB, Phillips KA, Morton A, Czepowicz V, Emmanuel N, Villareal G, Johnson M, Ballenger JC. Body dysmorphic disorder in patients with anxiety disorders and major depression: A comorbidity study. Am J Psychiatry. 1995;11:1665–1667. doi: 10.1176/ajp.152.11.1665. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: The Schedule for Affective Disorders and Schizophrenia (SADS-L) Arch Gen Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Keller MB. Social anxiety disorder clinical course and outcome: Review of Harvard/Brown anxiety research project (HARP) findings. J Clin Psychiatry. 2006;67:14–19. [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E. The Longitudinal Interval Follow-up Evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, White K, Swartz AR, Reich J, Lavori PW. Remission and relapse in subjects with panic disorder and panic with agoraphobia. J Nerv Ment Dis. 1994;182:290–296. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- Koran LM, Abujaoude E, Large MD, Serpe RT. The prevalence of body dysmorphic disorder in the United States adult population. CNS Spectr. 2008;13:316–322. doi: 10.1017/s1092852900016436. [DOI] [PubMed] [Google Scholar]
- Massion A, Warshaw M, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. Am J Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York (NY): Oxford University Press; 2005. (revised and expanded ed) [Google Scholar]
- Phillips KA, Diaz SF. Gender differences in body dysmorphic disorder. J Nerv Ment Dis. 1997;185:570–577. doi: 10.1097/00005053-199709000-00006. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Grant JE, Siniscalchi JM, Stout RL, Price LH. A retrospective follow-up study of body dysmorphic disorder. Compr Psychiatry. 2005a;46:315–321. doi: 10.1016/j.comppsych.2004.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Hollander E, Rasmussen SA, Aronowitz BR, DeCaria C, Goodman WK. A severity rating scale for body dysmorphic disorder: Development, reliability and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacol Bull. 1997;33:17–22. [PubMed] [Google Scholar]
- Phillips KA, Kaye WH. The relationship of body dysmorphic disorder and eating disorders to obsessive-compulsive disorder. CNS Spectr. 2007;12:347–358. doi: 10.1017/s1092852900021155. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Menard W, Fay C, Weisberg R. Demographic characteristics, phenomenology, comorbidity and family history in 200 individuals with body dysmorphic disorder. Psychosomatics. 2005b;46:317–326. doi: 10.1176/appi.psy.46.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Pagano ME, Menard W, Fay C, Stout RL. Predictors of remission from body dysmorphic disorder: A prospective study. J Nerv Ment Dis. 2005c;193:564–567. doi: 10.1097/01.nmd.0000172681.51661.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Pagano ME, Menard W, Stout RL. A 12-month follow-up study of the course of body dysmorphic disorder. Am J Psychiatry. 2006;163:907–912. doi: 10.1176/appi.ajp.163.5.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R. Washington (DC): American Psychiatric Press; 1990. [Google Scholar]
- Wilhelm S, Otto MW, Zucker BG, Pollack MH. Prevalence of body dysmorphic disorder in patients with anxiety disorders. J Anxiety Dis. 1997;11:499–502. doi: 10.1016/s0887-6185(97)00026-1. [DOI] [PubMed] [Google Scholar]