Abstract
Rates of vaccinations of healthcare workers with recommended vaccines are generally low in the developed countries. Our goals were to identify attitudes associated with self-reported vaccinations against pertussis and seasonal influenza among Israeli nurses in Mother and Child Healthcare Centers (MCHC) in the Haifa District. Over 100 nurses answered a self-administered questionnaire. Forty two percent of the nurses reported receiving the pertussis vaccine in the last five years and 44% reported receiving the influenza vaccine during the previous year. Attitudes toward the importance of vaccinating nurses, trust in the public health authorities and demand for autonomy were associated with receiving the pertussis vaccine. Attitudes toward the importance of vaccinating nurses and trust were associated with receiving the influenza vaccine in a bivariant analysis. However, in the logistic regression models only attitudes toward the importance of vaccinating nurses were associated with vaccinations [odds ratio (OR)- 3.66, 95% confidence interval (CI)- 1.4–9.6 for pertussis and OR- 4.53, CI-1.6–13.0 for influenza]. Jewish nurses reported more often receiving the influenza vaccine compared with the Arab nurses, whereas there was no difference between them in receiving the pertussis vaccine. Low levels of positive attitudes toward the importance of vaccinating nurses may inhibit nurses in MCHC from receiving vaccines. The demand for autonomy and low levels of trust may, in part, form these low levels of positive attitudes toward the importance of vaccinating nurses.
Keywords: attitudes, trust, autonomy, pertussis, influenza, vaccinations, nurses
Introduction
Vaccine preventable diseases among healthcare workers (HCW) such as pertussis and influenza can cause both further transmission of the diseases to vulnerable populations and absenteeism.1,2 Vaccination of HCW has been shown to benefit their patients.3 Therefore, health authorities in the developed countries formulated recommendations for vaccination of HCW.4-7 Pertussis vaccines have been in routine pediatric use for more than 50 y and a drastic decrease in the incidence of the disease has been achieved.8 However, the disease is still endemic in western countries despite the high rates of coverage achieved in infants.9 Levels of immunity decrease with time after both vaccination and natural infection, if no booster is given (waning of immunity). Therefore, adults and adolescents are the source of infection for infants who are at greatest risk for morbidity and mortality.10-12 In 2005, an adult pertussis vaccine was approved and guidelines for adult and HCW vaccinations were published with strong recommendations for HCW to get vaccinated. This is imperative so HCW do not transmit the disease to non-immunized infants.13 However, compliance with the pertussis vaccination is still low among HCW.14
Low compliance with recommended vaccinations for HCW is also reported for other vaccines. Many studies have looked at the low compliance with the seasonal influenza vaccine in the general population15 and among HCW.16-21 Levels of compliance among nurses were low. However, among physicians there are studies that reported higher levels of influenza vaccine coverage.20-22
Lately, Aguilar-Diaz et al.21 reviewed studies on influenza vaccines in HCW and found that the most common reasons for not receiving the vaccine were fear of adverse events, doubt regarding efficacy, not feeling belonging to a high risk group and believing that influenza is not a serious disease. Hollmeyer et al.23 reviewed studies on attitudes and predictors of influenza vaccination among HCWs in hospitals and found two major reasons for not receiving the vaccine. Respondents reported: (1) a wide range of misconceptions and lack of knowledge regarding influenza and the vaccine and (2) problems with access to receiving the vaccine. They also reported low perceived susceptibility to influenza, low perceived severity of influenza, low perceived efficacy of the vaccine, fear of adverse reactions to the vaccine and others. In a recent meta-analysis on predictors of seasonal influenza vaccination in HCW in hospitals, similar predictors were found, such as knowing that the vaccine is effective, being willing to prevent influenza transmission and believing that influenza is highly contagious.24
Negative attitudes toward vaccines have existed since the first development of vaccines two hundred years ago, relentlessly influencing the acceptance of vaccines. Lately, Poland and Jacobson25,26 highlighted the struggle against the antivaccinationists. It seems that the A(H1N1) influenza pandemic revealed a strong fear of vaccinations backed by the antivaccinationists, and these authors believe that the antivaccinationist have done much harm to public health.
In Haifa, Israel, a study from 2000 reported that only 11% of hospital employees had received the influenza vaccine27 and in 2004–5 the rates were not much higher (16.4%).28 Dubnov et al. (2010) reported that in 2009 after a large campaign in an Arab hospital in Nazareth, Israel, the rate of flu vaccination increased from 16% to 50%.
In a qualitative study we performed among Israeli nurses in Mother and Child Healthcare Centers (MCHC) we identified reasons for the low rate of compliance with vaccines. The nurses expressed mistrust in the public health authorities, and a demand for autonomy in making the decision regarding vaccinating themselves. They expressed negative feelings toward the vaccines such as fear of a new vaccine, fear of the side effects and more.29 In addition, it seemed that the A(H1N1) influenza scare had an effect on the nurses' attitudes toward pertussis and other vaccines.
The aim of this study was to assess, in a quantitative study, if and to what degree there is an association between attitudes toward the importance of vaccinating nurses, the nurse's trust in public health authorities, perceived need for autonomy and receiving pertussis and seasonal influenza vaccines. It was possible to study these aspects without the interference of the access to the vaccines because these nurses were given direct access to the vaccines.
Results
A hundred and seven nurses (47% response rate), all of them female, responded to the questionnaire, of these 77 were Jewish and 30 were Arab. More than half of them had academic degrees in addition to professional nursing training (Table 1). This serves as a representative sample of the population as in the total population (230 nurses) 35% of nurses are Arab and a similar percent have higher education as in the sample.
Table 1. Characteristics of nurses in the mother and child centers that participated in the study.
| Characteristics | Percent | Number | |
|---|---|---|---|
|
Total |
|
100 |
107 |
|
Population group |
Jews |
71.1 |
77 |
| Arabs |
28.0 |
30 |
|
| |
Missing |
0.9 |
1 |
|
Education |
Non academic professional nursing education |
42.0 |
45 |
| Undergraduate academic degree |
44.0 |
47 |
|
| Graduate academic degree |
14.0 |
15 |
|
|
Age |
Mean SD |
45.5 |
SD 9.3 |
|
Received pertussis vaccine in the last five years |
Yes |
42.0 |
45 |
| No |
56.1 |
60 |
|
| Missing |
1.9 |
2 |
|
| Received seasonal influenza vaccine for the last season | Yes |
43.9 |
47 |
| No |
55.1 |
59 |
|
| Missing | 0.9 | 1 |
About 44% of nurses reported receiving an influenza vaccine during the previous season and 42% reported receiving the pertussis vaccine during the previous five years (Table 1). Although the rate of receiving the vaccine was similar for both vaccines, only 27 nurses reported receiving both vaccines, 18 nurses reported receiving the pertussis vaccine but not the influenza vaccine and another 18 nurses reported receiving the influenza vaccine but not the pertussis vaccine (data not presented).
Between 64% and 41% agreed (agreed and strongly agreed) with the items describing autonomy (Table 2). For example, 64% of nurses agreed that “public health nurses should be given full independence to decide if to receive the recommended vaccines for healthcare workers,” and 60% agreed with the item “I trust only myself when I decide to get vaccinated.”
Table 2. Items included in the questionnaire depicting the variables.
| Item | Percent of nurses agreeing* with items | Item reversed | |
|---|---|---|---|
|
Autonomy |
|
|
|
| 1. |
Public health nurses should be given full independence to decide if to receive the recommended vaccines for healthcare workers |
63.8% |
+ |
| 2. |
The public should be given the freedom to decide about vaccinations |
41.3% |
+ |
| 3. |
I trust only myself when I decide to get vaccinated |
59.6% |
+ |
|
Trust in the public health authorities |
|
|
|
| 1. |
The healthcare system, to some degree, is using the nurses as guinea pigs for new vaccines |
12.9% |
+ |
| 2. |
The healthcare system is trying to “push” too many vaccines for healthcare workers |
21.9% |
+ |
| 3. |
The vaccine against influenza does not prevent influenza |
24.8% |
+ |
| 4. |
The healthcare system defends vaccines too strongly |
46.6% |
+ |
| 5. |
The healthcare system is attentive to opinions of public health nurses regarding vaccines |
53.8% |
|
| 6. |
I trust the information the Ministry of Health provides regarding vaccines |
88.3% |
|
| 7. |
Today, the healthcare system exaggerates in its reaction toward outbreaks of vaccine preventable diseases 0 |
19.6% |
+ |
| 8. |
The healthcare system provides public health nurses with the needed information to convince them that the recommended vaccines are important |
69.9% |
|
| 9 |
I don’t trust information the Ministry of Health provides regarding a new epidemic |
3.8% |
+ |
| 10 |
If there was a concern regarding a vaccine, it would not have been recommended |
70.8% |
|
|
Attitudes regarding the importance of vaccinating nurses |
|
|
|
| 1. |
As most people are immune, it is not that important if I do not get vaccinated |
4.7% |
+ |
| 2. |
It is very important that public health nurses get all the recommended vaccines |
64.8 |
|
| 3. |
A public health nurse that does not get vaccinated is putting others at risk |
59.4% |
|
| 4. |
Today there are too many demands from healthcare workers to vaccinate themselves |
40.6% |
+ |
| 5. |
Adult vaccinations are given without enough testing |
23.6% |
+ |
| 6 | I am willing to be among the first to accept a vaccine | 16.0% | |
Agree and strongly agree.
Levels of agreement with the items depicting trust in the public health authorities were high, 87% of nurses do not think the nurses are being used as guinea pigs for new vaccines and 88% of nurses trust information the MOH provides, however, over 10% do not report high trust.
Nurses’ attitudes regarding the importance of vaccinating nurses varied between 64.8% that thought it is very important that nurses get all recommended vaccines to 16% that were willing to be the first to accept a vaccine (Table 2).
Table 3 presents the association between the combined variables depicting the three types of attitudes and self-reported vaccinations. Attitudes regarding the importance of vaccinating nurses were significantly associated with receiving the vaccines; the mean score was 3.51 (ranging from 1 to 5) for nurses who received the pertussis vaccine and 3.00 for those who did not. Trust in the public health authorities was also significantly associated with receiving the vaccines; the mean score was 3.70 for nurses who received the pertussis vaccine and 3.46 for those who did not. Autonomy was significantly associated only with receiving the pertussis vaccine but not with receiving the influenza vaccine, this may be due to the small difference and not a large enough sample.
Table 3. Mean levels of attitudes by self-reported vaccination (ANOVA), mean and (SD).
| Attitudes | Pertussis vaccination | Influenza vaccination | ||
|---|---|---|---|---|
| Yes |
No |
Yes |
No |
|
|
Attitudes regarding the importance of vaccinating nurses |
3.51 (0.66) |
3.00 (0.57) |
3.49 (0.64) |
3.00 (0.58) |
| p |
< 0.0001 |
< 0.0001 |
||
|
Trust in the public health authorities |
3.70 (0.49) |
3.46 (0.50) |
3.73 (0.51) |
3.43 (0.46) |
| p |
0.016 |
0.002 |
||
|
Autonomy for nurses regarding vaccinations |
2.82 (0.83) |
2.45 (0.76) |
2.72 (0.82) |
2.50 (0.79) |
| p | 0.019 | 0.17 | ||
The three types of attitudes were significantly correlated with each other. Pearson correlation coefficient for attitudes regarding the importance of vaccinating nurses and autonomy was 0.55, and for trust and attitudes regarding the importance of vaccinating nurses was 0.60. The coefficient for the correlation between autonomy and trust was lower: 0.32. In a linear regression with attitudes regarding the importance of vaccinating nurses as the dependant variable, autonomy and trust explain 50% of the variance. In addition, autonomy explained 10.3% of the variance in trust in a linear regression analysis.
Age and level of education were not associated with self-reported vaccination with any of the vaccines, nor with the three attitude variables. However, Jewish nurses reported more often receiving the influenza vaccine, but not the pertussis vaccine compared with Arab nurses. There was no difference in the levels of the three types of attitudes among Jewish and Arab nurses.
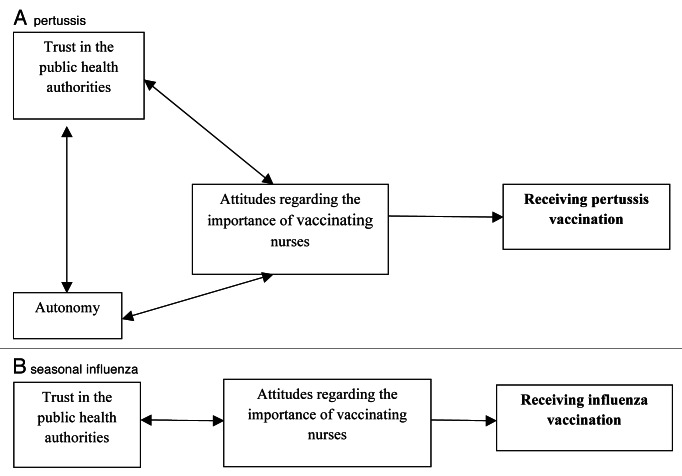
Logistic regression models were run to identify the attitudes associated with receiving each vaccine, after adjusting for population group. In each step another attitude was added to the regression. In the results presented in Table 4, the dependent variable is self-reported pertussis vaccination. Attitudes regarding autonomy were associated with reported vaccination [odds ratio (OR) = 1.8, 95% confidence interval (CI) = 1.09–3.00], however after adding attitudes regarding trust in the public health authorities the association was non-significant and attitudes regarding trust were only marginally significantly associated with reported vaccination (OR = 2.4, CI = 0.98–5.92). Attitudes regarding the importance of vaccinating nurses were strongly associated with reported pertussis vaccination and eliminated the marginal association with the other attitudes (OR = 3.66, CI = 1.40–9.59). This suggests the possibility that attitudes regarding the importance of vaccinating nurses serve as a mediator for the trust and autonomy variables (Fig. 1A).
Table 4. Factors associated with self reported receiving the Pertussis vaccine in the past 5 y, logistic regression models odds ratio (OR), confidence interval (CI) and p value. n = 104.
| Independent variables | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
OR |
CI |
p |
OR |
CI |
p |
OR |
CI |
p |
OR |
CI |
p |
| Population group* |
1.47 |
0.63–3.44 |
0.33 |
1.47 |
0.61–3.54 |
0.39 |
1.55 |
0.64–3.80 |
0.33 |
1.60 |
0.62–4.16 |
0.33 |
|
Attitudes |
|
|
|
|
|
|
|
|
|
|
|
|
| Autonomy |
- |
- |
- |
1.80 |
1.09–3.00 |
0.036 |
1.55 |
0.91–2.63 |
0.11 |
1.10 |
0.60–2.04 |
0.76 |
| Trust in public health authorities |
- |
- |
- |
- |
- |
- |
2.41 |
0.98–5.92 |
0.05 |
0.97 |
0.33–2.83 |
0.96 |
| Attitudes regarding the importance of vaccinating nurses | - | - | - | - | - | - | - | - | - | 3.66 | 1.40–9.59 | 0.008 |
Jews-1 Arabs 2.
Figure 1. Suggested models explaining the attitudes associated with vaccinations.
In the regression models presented in Table 5 the dependent variable was reported seasonal influenza vaccination during the previous year. Attitudes toward autonomy were not associated with receiving this vaccine, however, trust in the public health authorities was (OR = 3.75, CI = 1.44–9.77). This association was non-significant after adding the attitudes regarding the importance of vaccinating nurses into the regression. The OR of nurses with positive attitudes regarding the importance of vaccinating nurses compared with nurses with negative attitudes was 4.5 (CI = 1.58–13.00). This again suggests that attitudes regarding the importance of vaccinating nurses mediate the association between trust and reported influenza vaccination. The interaction between population group and attitudes and influenza vaccine was not significant. The suggested model describing the attitudes that affect the decision of receiving this vaccine is depicted in Figure 1B.
Table 5. Factors associated with self reported receiving the seasonal influenza vaccine last year, logistic regression models odds ratio (OR), confidence interval (CI) and p value. n = 105.
| Independent variables | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
OR |
CI |
p |
OR |
CI |
p |
OR |
CI |
p |
OR |
CI |
p |
| Population group* |
0.21 |
0.08–0.57 |
0.002 |
0.20 |
0.07–0.54 |
0.002 |
0.19 |
0.07–0.54 |
0.002 |
0.15 |
0.05–0.46 |
0.001 |
|
Attitudes |
|
|
|
|
|
|
|
|
|
|
|
|
| Autonomy |
- |
- |
- |
1.52 |
0.90–2.57 |
0.15 |
1.22 |
0.68–2.16 |
0.44 |
0.74 |
0.37–1.50 |
0.51 |
| Trust in public health authorities |
- |
- |
- |
- |
- |
- |
3.75 |
1.44–9.77 |
0.007 |
1.77 |
0.59–5.32 |
0.31 |
| Attitudes regarding the importance of vaccinating nurses | - | - | - | - | - | - | - | - | - | 4.53 | 1.58–13.00 | 0.005 |
Jews-1 Arabs 2.
Discussion
This study was intended to go beyond the frequently reported attitudes based on the Health Belief Model such as perceived susceptibility to disease, perceived severity of the disease, perceived efficacy of the vaccine, fear of adverse reactions to the vaccine and other problems such as access to receiving the vaccine.21,23,24
In this study, nurses who care for healthy infants were interviewed about their attitudes and behaviors regarding vaccinations. These nurses' main occupation is to vaccinate infants and toddlers. Attitudes identified in a previous qualitative study with a similar population of nurses were developed into a quantitative questionnaire.29 These attitudes included lack of trust in the information and recommendations that the health authorities published, especially during the A(H1N1) influenza pandemic. In the qualitative study, these feelings of lack of trust were strongly expressed; however, in this quantitative study less than 20% expressed them. It is not possible to compare the results of the two studies due to methodological differences, however, the present study was performed about two years after the A(H1N1) influenza scare and the feeling of mistrust may have faded a little.
An additional theme identified in the qualitative study was the nurses' demand for autonomy. Nurses did not want to be told they have to receive vaccinations, they wanted to be able to decide for themselves if to accept the vaccine or not. In this quantitative study, more than half of the nurses thought they should be given the autonomy to decide on personal vaccinations. In addition, the nurses were also asked about their general attitudes regarding the importance of vaccines for nurses. The results indicate that the importance nurses give to vaccinating nurses is the strongest factor associated with the acceptance of both the influenza and the pertussis vaccines. Nurses who think vaccines are important for nurses are more inclined to get vaccinated.
The trust nurses have in the authorities and the autonomy they demand explain a high percentage of the variance in the importance nurses give to vaccinating nurses. Nurses that have less trust in the authorities and demand more autonomy may see less importance in vaccinations for nurses and therefore may receive the pertussis vaccine less often. Regarding influenza, the importance nurses give to vaccinating nurses seems to be associated only with the trust they have in the authorities, the higher the trust the higher the importance they give to vaccinating nurses and receiving the influenza vaccine. Autonomy was not found to be a factor in the decision making regarding receiving the influenza vaccine. This may be due to the small numbers of nurses in the study and the weak association examined.
It seems that autonomy and trust are not attitudes that directly influence receiving the vaccines. Their effect may be mediated through attitudes regarding the importance of vaccinating nurses. In addition, the decision regarding receiving vaccinations may not be a general process of making a decision for all vaccines, but a separate decision for each specific vaccine. This idea is backed by the fact that a third of all the nurses made a different decision for each vaccine, i.e., receiving one but not the other. This again provides evidence that the nurses want to have autonomy in deciding on receiving vaccinations, and that the factors affecting the decision differ for each specific vaccine.
It seems that nurses, just like lay people, are not willing to blindly accept the recommendations of health care experts. They try to form their own opinions and act by them. Velan et al.31 suggested that nowadays more people use reflexive risk/benefit assessment to make decisions about vaccination and a large part of them use rational assessment before deciding if to receive a vaccine. This study supports this assumption as a large part of the nurses chose to receive one vaccine but not the other. This suggests reflexive thinking, where each nurse makes a personal decision regarding each specific vaccine.
Evidence regarding past low rates of influenza vaccinations among HCW in other countries16-21 emphasizes the importance of understanding the barriers to influenza vaccination. HCW may have lost trust in the public health authorities during the A(H1N1) influenza pandemic, and this trust needs to be regenerated before high levels of vaccination can be achieved among HCWs. There is evidence that levels of trust in health authorities decreased after the A(H1N1) influenza scare30 and other studies have also identified trust to be an important factor in acceptance of vaccines such as the acceptance of the Human Papilloma Virus (HPV) vaccine among mothers of 8–14 y old girls.31 In our qualitative study29 there were nurses that expressed strong feelings against the demand to be vaccinated generally, and especially against A(H1N1). Some of them felt the authorities did not know what they were doing and were not consistent in the information they gave, and therefore could not be trusted. The next vaccine they were asked to get happened to be against pertussis, therefore their lack of trust was turned toward it.29 In a survey of HCW and medical students in a German university hospital during an influenza vaccination campaign, 16.4% of the 1,645 respondents reported that the A(H1N1) pandemic had influenced their attitudes toward vaccinations in general.32 Velan et al.30 identified distrust as a key element in the attitudes of their survey respondents. They suggested that the increased loss of trust in health authorities worldwide could explain the low rates of A(H1N1) influenza vaccination coverage. In the present study we could not directly associate between the A(H1N1) pandemic and trust, however it seems that trust is a major factor influencing attitudes regarding the importance of vaccinating nurses, which in turn influences acceptance of the vaccines, both influenza and pertussis.
Distrust and fear are not new phenomena in the world of vaccines and it has been reported in the general population previously. These feelings have been expressed since the development of vaccines and specifically every time a new vaccine has been introduced and people invited to receive it. We need to develop ways to tackle the issues causing mistrust and to increase trust. Poland and Jacobson (2011) claim that “antivaccinationists tend towards complete mistrust of government and manufacturers, conspiratorial thinking, denialism, low cognitive complexity in thinking patterns, reasoning flaws and a habit of substituting emotional anecdotes for data.”25,26 Up till now, this was not considered a major problem among HCW compared with the general population. The recent reviews on barriers to HCW vaccination emphasize the Health Belief Model components as barriers and not low levels of trust.21,23,24 However, it seems that nurses are not different from lay persons that increasingly question the need for each vaccine.
These results indicate that in addition to increasing levels of knowledge regarding the vaccines and the ethical aspects of vaccinating HCW, it is important also to restore and increase levels of trust in the public health authorities among HCW.
Communication of the importance of vaccinations should not only be developed for the lay public but also for HCW, as they too have misconceptions regarding vaccinations. Providing the public and HCW with information regarding the epidemiology of the disease and information regarding the vaccine itself, its efficacy and safety, may reduce levels of mistrust and uncertainty. In addition, it is important to be very consistent in the information given, so no changes are made in the messages, and if messages are changed in-depth explanations should be given so as not to promote mistrust. Obviously it is very important to pay attention to the needs of HCW and to try to avoid mandatory vaccination policies as they may cause unrest and increased mistrust in times of an epidemic. However, this may not be possible or ethical.
The nurses' reflexive decisions regarding these two vaccines may incorporate the difference between them. The pertussis vaccine is a vaccine they routinely vaccinate infants with, and the health district implemented a yearlong intervention to increase compliance with the vaccine, whereas the influenza vaccine is not a routine vaccine they work with.
Nurses may need to justify their demand for autonomy therefore may adopt perceptions that the vaccines are “not so important for nurses” and therefore they can decide for themselves. This may be due to low cognitive complexity in thinking patterns as Poland and Jacobson (2011) suggested. The nurses' logic may lead them to believe they have all the information needed to make an independent decision. Hakim et al.33 studied HCW and non-HCW in a large hospital with a high compliance rate of influenza vaccinations. Within this context the most frequent reason for opposing vaccination was violation of freedom of choice and personal autonomy. In addition, even among the HCW who voluntarily received the influenza vaccine, a third of the employees objected to mandatory immunization as an official policy citing precisely these concerns of personal choice and autonomy.
HCW, and especially nurses that vaccinate infants, can and should serve as role models for the lay public. How can we expect the general public to have trust in vaccines if a large percent of the HCW do not vaccinate themselves? Nurses need to understand that the public expects them to be vaccinated, and if not, the trust in the health system will be tarnished. The importance of nurses as role models should be presented to the nurses and generally to all HCW.
Recently, policy makers have been advocating for the adoption of mandating vaccinations or providing incentives and sanctions to increase HCW compliance with vaccines.2,34,35 Ethical issues back the demand for mandatory policies for HCW.1 Mandatory vaccination for HCW contradicts the demand for autonomy expressed by HCW in our study and others. Hakim et al. report that a significant minority have unfavorable views toward mandating vaccinations among HCW. In Israel, in 2011 the MOH published a program that included mandatory vaccinations against certain diseases for specific groups of HCW performing specific activities.36 By the first of January 2014 MCHC nurses will not be allowed to work with infants if they are not vaccinated against pertussis. In other developed countries implementation of these mandatory vaccination programs faced resistance. For example, Virginia Mason Medical Center faced litigation from nurses; however the court favored the mandatory program.37 A major campaign among HCW will be needed if mandatory policies are implemented and should start before.
In this study education and age were not associated with receiving the vaccinations. Velan et al.30 also found that education was not associated with receiving the A(H1N1) influenza vaccine in lay persons although older people were more inclined to be vaccinated for A(H1N1). The attitudes studied in this questionnaire are not dependent on age or education and therefore were not found to be factors predicting vaccinations.
Arab nurses reported less often receiving the influenza vaccine compared with Jewish nurses, but no difference was observed for the pertussis vaccine. Generally, there is a higher rate of childhood vaccine coverage within the Arab community, however there is evidence than among adults levels of vaccinations and specifically seasonal and A(H1N1) influenza were lower than among Jew. Though this was among the general population, it is an indication of the community's response to the vaccines, and Arab nurses are a part of the Arab community and seem to behave in accordance with it.30,38
The major limitations of this study are the small sample, low response rate and non-diverse group of nurses. However, MCHC nurses are a very important group of HCW as vaccinations are their routine job and they have daily contact with unvaccinated infants. It is very important that they have positive attitudes toward vaccinations as they are the healthcare systems' agents that represent vaccines and have to convince parents to vaccinate their children. More importantly, these nurses could infect infants and toddlers if not immunized.
Other limitations include the cross-sectional design of the study that could limit the ability to draw conclusions about a causal relationship and selection and information biases. Self-reported vaccination may be biased due to recall bias and social desirability, as the nurses know they were expected to be vaccinated. In addition, their ratings of the attitudes may also be biased toward the “expected” positive attitudes concerning vaccines. In future studies objective information regarding vaccinations would be preferable, however ethically this is not always possible.
Materials and Methods
In January 2011 a letter from the two Subdistrict Health Officers was sent out asking every nurse working at the MCHC to immunize herself with a dose of Tdap. During this year nurses were also given an e-learning tutorial about pertussis vaccination, including the importance of vaccinating HCW. Every nurse was asked to order a dose of Tdap from the Subdistrict Health Office, free of charge, for herself and the other nurses in the clinic as part of her monthly routine order of vaccines for the infants she treats at the clinic. At the beginning of December 2011 a personal letter from the head nurse of the Haifa District of the Ministry of Health (MOH) was sent via email to all nurses in the MCHCs asking the nurses to answer the attached questionnaire (230 nurses). Each clinic has a MOH email address and in each clinic there are between 2 to 4 nurses. The nurses were asked to print out the questionnaire, answer it and send it back to the district health office with no identifying information. One hundred and seven nurses answered the questionnaires giving a response rate of 47%.
The questionnaire was in Hebrew and included information on age, professional education, population group (Arab or Jewish), influenza and pertussis vaccinations received in the past and receiving guidance regarding the pertussis vaccine during the last month. A list of items depicting different attitudes was included in the questionnaire: (1) Attitudes toward the importance of vaccinating nurses, (2) Trust in the public health authorities and (3) Autonomy regarding vaccinations. The list was compiled based on our qualitative study29 and on another study.39 A pretest was performed in a large city (outside the Haifa District) and in another MOH district. The present items were chosen after factor analysis and Cronbach's α calculations.
Dependent variables were defined as self-reported pertussis vaccination during the last five years and self-reported influenza vaccination during the previous season of 2010–2011. Receiving the vaccine was coded as 1 and not receiving the vaccine was coded as 0.
Independent variables
A list of 19 items (see Table 2) were presented to the nurses, for each item the respondent was asked to choose a response from a Likert scale ranging from 5-agree very much, to 1-do not agree at all. The items consisted of three types of attitudes: (1) Autonomy regarding vaccinations- included three items with a Cronbach's α of 0.64. The higher the score the lower the demand for autonomy. (2) Trust in the public health authorities- included ten items with a Cronbach's α of 0.75. The higher the score the higher the trust. (3) Attitudes regarding the importance of vaccinating nurses- included six items with a Cronbach's α of 0.77. The higher the score the more positive the attitudes toward the importance of vaccines. The combined scores for each of the variables autonomy, trust and importance of vaccinating nurses were calculated using the mean response rate. Age was treated as a continuous variable and education as a categorical variable as appears in Table 1.
Statistical analysis
Spearman's correlations were applied to assess the crude associations between the three types of attitudes. The ANOVA test was applied to measure the association between the mean levels of the attitudes and receiving or not receiving a vaccine. Multivariable logistic regression analysis was performed for each vaccine separately (the dependent variable). Only variables associated with receiving at least one of the vaccines in the bivariable analysis were added to the regressions, therefore age and education were not added to the model. The first model included only the population group variable, then, in each model one additional attitude was added to assess the association of each attitude over and above the other attitudes. The odds ratio (OR), 95% confidence interval (CI) and p-value are presented in the tables. Statistical significance was set at a p value of 0.05. SPSS version 17.0 was used for the analysis.
Conclusions
This study presents evidence on the importance of trust and autonomy in the process of decision making of the MCHC nurses about receiving vaccines. Although the effects of trust and autonomy were mediated through attitudes regarding the importance of vaccinating nurses, they are important in influencing the adoption of vaccines by MCHC nurses. Interventions to increase trust and explain the importance of HCW immunity is imperative in order to achieve higher levels of vaccination among HCW. This may increase their feeling of autonomy prior to implementing the mandatory policies to vaccinate them.
Glossary
Abbreviations:
- HCW
healthcare workers
- MCHC
Mother and Child Health Care Centers
- OR
odds ratio
- CI
confidence interval
- MOH
Ministry of Health
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/22503
References
- 1.Anikeeva O, Braunack-Mayer A, Rogers W. Requiring influenza vaccination for health care workers. Am J Public Health. 2009;99:24–9. doi: 10.2105/AJPH.2008.136440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ottenberg AL, Wu JT, Poland GA, Jacobson RM, Koenig BA, Tilburt JC. Vaccinating health care workers against influenza: the ethical and legal rationale for a mandate. Am J Public Health. 2011;101:212–6. doi: 10.2105/AJPH.2009.190751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bénet T, Régis C, Voirin N, Robert O, Lina B, Cronenberger S, et al. Influenza vaccination of healthcare workers in acute-care hospitals: a case-control study of its effect on hospital-acquired influenza among patients. BMC Infect Dis. 2012;12:30. doi: 10.1186/1471-2334-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiore AE, Shay DK, Broder K, Iskander JK, Uyeki TM, Mootrey G, et al. Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2008. MMWR Recomm Rep. 2008;57(RR-7):1–60. [PubMed] [Google Scholar]
- 5.Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med. 2007;357:1373–81. doi: 10.1056/NEJMoa070844. [DOI] [PubMed] [Google Scholar]
- 6.Burls A, Jordan R, Barton P, Olowokure B, Wake B, Albon E, et al. Vaccinating healthcare workers against influenza to protect the vulnerable--is it a good use of healthcare resources? A systematic review of the evidence and an economic evaluation. Vaccine. 2006;24:4212–21. doi: 10.1016/j.vaccine.2005.12.043. [DOI] [PubMed] [Google Scholar]
- 7.Ministry of Health. Influenza vaccinations. Jerusalem, Israel 2009. (Hebrew) [Google Scholar]
- 8.Edwards KM, Decker MD, Mortimer EA Jr. Pertussis vaccine. In: Plotkin SA, Orenstein WA, eds. Vaccines. 3rd ed. Philadelphia: W.B. Saunders, 1999:293–344. [Google Scholar]
- 9.Raguckas SE, VandenBussche HL, Jacobs C, Klepser ME. Pertussis resurgence: diagnosis, treatment, prevention, and beyond. Pharmacotherapy. 2007;27:41–52. doi: 10.1592/phco.27.1.41. [DOI] [PubMed] [Google Scholar]
- 10.He Q, Viljanen MK, Nikkari S, Lyytikäinen R, Mertsola J. Outcomes of Bordetella pertussis infection in different age groups of an immunized population. J Infect Dis. 1994;170:873–7. doi: 10.1093/infdis/170.4.873. [DOI] [PubMed] [Google Scholar]
- 11.Wirsing von König CH, Postels-Multani S, Bock HL, Schmitt HJ. Pertussis in adults: frequency of transmission after household exposure. Lancet. 1995;346:1326–9. doi: 10.1016/S0140-6736(95)92343-8. [DOI] [PubMed] [Google Scholar]
- 12.Leekha S, Thompson RL, Sampathkumar P. Epidemiology and control of pertussis outbreaks in a tertiary care center and the resource consumption associated with these outbreaks. Infect Control Hosp Epidemiol. 2009;30:467–73. doi: 10.1086/596774. [DOI] [PubMed] [Google Scholar]
- 13.Greer AL, Fisman DN. Keeping vulnerable children safe from pertussis: preventing nosocomial pertussis transmission in the neonatal intensive care unit. Infect Control Hosp Epidemiol. 2009;30:1084–9. doi: 10.1086/644755. [DOI] [PubMed] [Google Scholar]
- 14.Wicker S, Rose MA. Health care workers and pertussis: an underestimated issue. Med Klin (Munich) 2010;105:882–6. doi: 10.1007/s00063-010-1153-0. [DOI] [PubMed] [Google Scholar]
- 15.Szucs TD, Müller D. Influenza vaccination coverage rates in five European countries-a population-based cross-sectional analysis of two consecutive influenza seasons. Vaccine. 2005;23:5055–63. doi: 10.1016/j.vaccine.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Seale H, Wang Q, Yang P, Dwyer DE, Wang X, Zhang Y, et al. Influenza vaccination amongst hospital health care workers in Beijing. Occup Med (Lond) 2010;60:335–9. doi: 10.1093/occmed/kqq037. [DOI] [PubMed] [Google Scholar]
- 17.Takayanagi IJ, Cardoso MR, Costa SF, Araya ME, Machado CM. Attitudes of health care workers to influenza vaccination: why are they not vaccinated? Am J Infect Control. 2007;35:56–61. doi: 10.1016/j.ajic.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Chittaro M, Turello D, Calligaris L, Farneti F, Faruzzo A, Fiappo E, et al. Impact of vaccinating HCWs on the ward and possible influence of avian flu threat. Infection. 2009;37:29–33. doi: 10.1007/s15010-008-8002-6. [DOI] [PubMed] [Google Scholar]
- 19.Vírseda S, Restrepo MA, Arranz E, Magán-Tapia P, Fernández-Ruiz M, de la Cámara AG, et al. Seasonal and Pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish University Hospital. Vaccine. 2010;28:4751–7. doi: 10.1016/j.vaccine.2010.04.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wicker S, Rabenau HF, Doerr HW, Allwinn R. Influenza vaccination compliance among health care workers in a German university hospital. Infection. 2009;37:197–202. doi: 10.1007/s15010-008-8200-2. [DOI] [PubMed] [Google Scholar]
- 21.Aguilar-Díaz FdelC, Jiménez-Corona ME, Ponce-de-León-Rosales S. Influenza vaccine and healthcare workers. Arch Med Res. 2011;42:652–7. doi: 10.1016/j.arcmed.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Cowan AE, Winston CA, Davis MM, Wortley PM, Clark SJ. Influenza vaccination status and influenza-related perspectives and practices among US physicians. Am J Infect Control. 2006;34:164–9. doi: 10.1016/j.ajic.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals--a review of studies on attitudes and predictors. Vaccine. 2009;27:3935–44. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 24.Riphagen-Dalhuisen J, Gefenaite G, Hak E. Predictors of seasonal influenza vaccination among healthcare workers in hospitals: a descriptive meta-analysis. Occup Environ Med. 2012;69:230–5. doi: 10.1136/oemed-2011-100134. [DOI] [PubMed] [Google Scholar]
- 25.Poland GA, Jacobson RM. The age-old struggle against the antivaccinationists. N Engl J Med. 2011;364:97–9. doi: 10.1056/NEJMp1010594. [DOI] [PubMed] [Google Scholar]
- 26.Poland GA, Jacobson RM. The clinician’s guide to the anti-vaccinationists’ galaxy. Hum Immunol. 2012;73:859–66. doi: 10.1016/j.humimm.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 27.Habib S, Rishpon S, Rubin L. Influenza vaccination among healthcare workers. Isr Med Assoc J. 2000;2:899–901. [PubMed] [Google Scholar]
- 28.Dubnov JK, Kassabri W, Bisharat B, Rishpon S. Influenza vaccination coverage determinants among employees of the Nazareth Hospital in Israel. Isr Med Assoc J. 2010;12:338–41. [PubMed] [Google Scholar]
- 29.Baron-Epel O, Bord S, Madjar B, Habib S, Rishpon S. What lies behind the low rates of vaccinations among nurses who treat infants? Vaccine. 2012;30:3151–4. doi: 10.1016/j.vaccine.2012.02.074. [DOI] [PubMed] [Google Scholar]
- 30.Velan B, Kaplan G, Ziv A, Boyko V, Lerner-Geva L. Major motives in non-acceptance of A/H1N1 flu vaccination: the weight of rational assessment. Vaccine. 2011;29:1173–9. doi: 10.1016/j.vaccine.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 31.Marlow LA, Waller J, Wardle J. Trust and experience as predictors of HPV vaccine acceptance. Hum Vaccin. 2007;3:171–5. doi: 10.4161/hv.3.5.4310. [DOI] [PubMed] [Google Scholar]
- 32.Brandt C, Rabenau HF, Bornmann S, Gottschalk R, Wicker S. The impact of the 2009 influenza A(H1N1) pandemic on attitudes of healthcare workers toward seasonal influenza vaccination 2010/11. Euro Surveill. 2011;16 [PubMed] [Google Scholar]
- 33.Hakim H, Gaur AH, McCullers JA. Motivating factors for high rates of influenza vaccination among healthcare workers. Vaccine. 2011;29:5963–9. doi: 10.1016/j.vaccine.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 34.Maltezou HC, Wicker S, Borg M, Heininger U, Puro V, Theodoridou M, et al. Vaccination policies for health-care workers in acute health-care facilities in Europe. Vaccine. 2011;29:9557–62. doi: 10.1016/j.vaccine.2011.09.076. [DOI] [PubMed] [Google Scholar]
- 35.Mereckiene J, Cotter S, Weber JT, Nicoll A, D’Ancona F, Lopalco PL, et al. VENICE project gatekeepers group Influenza A(H1N1)pdm09 vaccination policies and coverage in Europe. Euro Surveill. 2012;17:pii 20064. doi: 10.2807/ese.17.04.20064-en. [DOI] [PubMed] [Google Scholar]
- 36.Ministry of Health. Guidelines for health care workers. General Manager of the Ministry of Helath, 2011. Hebrew. [Google Scholar]
- 37.Rakita RM, Hagar BA, Crome P, Lammert JK. Mandatory influenza vaccination of healthcare workers: a 5-year study. Infect Control Hosp Epidemiol. 2010;31:881–8. doi: 10.1086/656210. [DOI] [PubMed] [Google Scholar]
- 38.Shahrabani S, Benzion U. The effects of socioeconomic factors on the decision to be vaccinated: the case of flu shot vaccination. Isr Med Assoc J. 2006;8:630–4. [PubMed] [Google Scholar]
- 39.Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. J Fam Pract. 2005;54:344–52. [PubMed] [Google Scholar]