Abstract
Personalized therapy is directed at obtaining maximal therapeutic effect on diseased tissue with minimal off-target side effects. Many classes of therapeutics have attempted to reach this ideal, only to fall well short. Therapeutic vaccines represent a novel class of therapies that can induce a dynamic immune response that, in theory, can continue to adapt and expand following initiation of vaccination. This adaptability, through epitope spreading or antigen cascade, can continuously refine a therapeutic immune response, making it more relevant to the patient’s tumor. This active, dynamic, iterative process can continue long after the vaccine course has been completed. Recent clinical trials have provided further insight into the clinical activity of therapeutic vaccines, and offer guidance on clinical expectations following vaccine. The ongoing active sculpting of the immune response, along with the lack of significant side effects, uniquely positions therapeutic vaccines as perhaps the ultimate in personalized therapy.
Keywords: antigen cascade, antigen spreading, cancer vaccine, epitope spreading, immunotherapy, individualized therapy, personalized medicine, precision medicine
Introduction
The ideal medical intervention aims to correct an underlying disorder or condition with minimal or no negative impact on health. Initial systemic anticancer regimens employed chemotherapy agents that were able to kill cancer cells but in many cases did not lead to cures. Unfortunately, these agents have harsh side effects with very narrow therapeutic indices. Recently, attention has shifted substantially to “personalized medicine” or “precision therapy,” with a rapid surge in the number of agents that target specific pathways involved in oncogene addiction. Unfortunately, current treatment strategies under the rubric of personalized therapy frequently fall far short of the ideal goal of targeting only diseased tissues without side effects on normal tissues. Furthermore, there are often numerous driver mutations within a cancer cell, with new mutations coming into play over time, requiring that multiple pathways be blocked concurrently and sequentially. Thus, with few exceptions, this form of targeted therapy has not led to dramatic improvements in patient outcomes.
While therapeutic vaccines have only recently demonstrated the potential to improve patient outcomes, as a class they have the potential to become the ultimate in personalized medicine. Although therapeutic vaccines for tumor specific antigens (e.g., mutated ras or idiotypic vaccines) may intuitively be thought of as personalized therapy, vaccines against widely shared tumor associated antigens (e.g., PSA, MUC-1 or CEA) may also give rise to a personalized therapeutic response. These therapeutic vaccines, which have few if any side effects, can initiate a therapeutic response that the resilient, adaptable immune system can further expand into an ongoing, dynamic immune response—arguable the optimal personalized therapy.
Understanding the “New Kid”
Therapeutic vaccines have a completely different mechanism of action compared with previously approved cancer therapeutics. First, vaccines do not directly target the tumor or its microenvironment, but instead directly target the immune system, which subsequently initiates or expands attacks on the tumor. Furthermore, a cytotoxic therapy does not initiate a memory response, whereas such a response is an important goal of an effective therapeutic vaccine. Thus, the kinetics of a clinical response following treatment with a therapeutic vaccine are predictably different from the kinetics of a cytotoxic agent.1-4 Indeed, because of their very different mechanisms of action, therapeutic vaccines initiate an ongoing, dynamic response that may result initially in subtle changes to the tumor growth rate; over time, however, if these changes are maintained or expanded, improvements in outcome may be substantial. In other words, the immune response may start slowly, but over time it may grow deeper, broader, and more clinically active, and may persist long after initial administration of the vaccine. Underscoring this important point, definitive clinical trials with two immunotherapies, ipilimumab5 and sipuleucel-T,6 have demonstrated no improvement in median progression-free survival, but have shown substantial improvement in overall survival.
The Winning Strategy
Multiple preclinical studies have suggested that CD8+ T cells are key players in the antitumor response following therapeutic vaccines. CD8 depletion studies demonstrate complete abrogation of the therapeutic effect of vaccines. Thus, many studies have focused on increasing the number of CD8+ T cells following vaccination. However, focusing on the absolute number of vaccine-specific T cells misses other critical factors, such as the quality of the T-cell response and the effectiveness of the cancer patient’s own immunosuppressive entities.
Many immunosuppressive factors and cells within the tumor microenvironment can significantly affect the success of a therapeutic vaccine.7 This is one reason that many studies have suggested that immunotherapy should ideally be used earlier in the disease course in patients with lower tumor burdens.8,9 Other studies have suggested combining vaccine with standard therapies in a manner designed to minimize or neutralize the immunosuppressive factors elaborated by or harbored within the tumor.10-12 (The myriad important features of the tumor microenvironment, and their negative impact on the function of antitumor T cells, is beyond the scope of this brief commentary.)
The quality of a T-cell response may arguably be divided into two aspects. The first is the avidity of the T-cell response. The avidity of a T cell can be defined by the concentration of antigen required to elicit a response. Thus, higher-avidity T cells can become activated to kill tumor cells with much lower concentrations of antigen.13 This is important because only high-avidity T cells can efficiently kill tumor cells. Therefore, therapeutic vaccine strategies designed to augment antitumor avidity may prove to be more clinical active. Unfortunately, most conventional T-cell assays, such as the ELISPOT or tetramer, do not measure this important factor.
The second qualitative aspect of a T-cell response is its breadth, or the expansion of a T-cell response to epitopes not found in the vaccine. This concept, known as epitope spreading, antigen spreading or antigen cascade,14 has been associated with both MHC class I- and II-restricted responses and reflects cross-presentation of tumor antigens. Thus, if a tumor-specific T cell can lyse tumor cells, the dead or dying tumor cells can be taken up by antigen-presenting cells, with the result that multiple, perhaps even more immunogenic, tumor antigens can be presented to immune cells, initiating a broader immune response (Fig. 1).
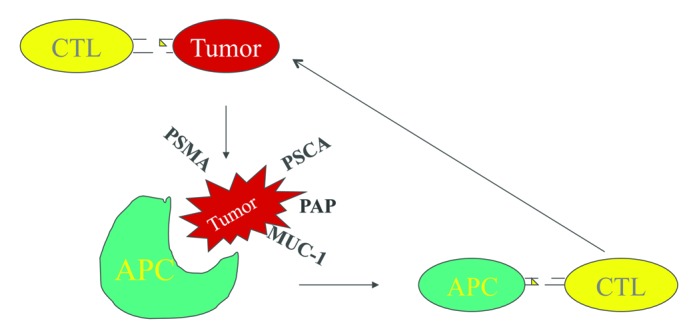
Figure 1. Antigen cascade: An initial immune response (e.g., a PSA-specific cytotoxic T lymphocyte [CTL] following vaccination with a PSA specific vaccine) may encounter a PSA expressing tumor cell. If that CTL can kill the tumor cell in an immunologically relevant manner, as that tumor cell is dying it can be taken up by antigen-presenting cells (APCs). There, other tumor-associated antigens (depicted by prostate-specific membrane antigen [PSMA], prostate stem cell antigen [PSCA], prostatic acid phosphatase [PAP] and mucin-1 [MUC-1]) can be processed and presented via cross-presentation to other CTLs, a process that can activate these CTLs specific for these other antigens. Thus, while the initial vaccine may target one antigen, a broader antitumor immune response may ensue, and this dynamic response may continue to broaden and adapt to subsequent mutations.
This phenomenon has been described by many investigators, but a recently published preclinical study by Hodge et al. highlights the impact of antigen cascade.15 In this study, mice implanted in the flank with a CEA-expressing tumor were vaccinated subcutaneously with a CEA-based vaccine. In the opposite flank, a parental tumor that did not contain CEA was implanted. Thus, an immune response to the CEA antigen in the vaccine could not directly affect the growth of the CEA– tumor. In this experiment, vaccinated mice had a substantial decrease in tumor size in both the CEA+ and CEA– tumors compared with nonvaccinated mice. In fact, the antitumor immune response appeared to be due to T cells specific for GP70, an endogenous murine retroviral antigen present in the tumors implanted in both flanks, but not included in the vaccine. Indeed, in vaccinated mice, the IFN-γ response to GP70 was about 15 times greater than the response to the CEA present in the vaccine, suggesting that this cascade response was critical to the activity of the vaccine in this model.
In humans, it is possible that the same vaccine may induce completely different immune responses, in terms of antigen cascade, in different patients with the same type of cancer. Furthermore, as suggested in the murine model described above, the immune response to antigens not present in the vaccine may be much more clinically relevant for a given patient than the initial immune response to the epitope in the vaccine. However, while antigen cascade may be a significant factor in a clinically relevant antitumor immune response,14 using conventional T-cell assays to determine a priori which antigen-specific T cells are most likely to be activated, and which of those is clinically significant, is akin to finding the proverbial needle in a haystack.
An expanding, cascading immune response may continue over time, eventually broadening into an immune response that could be even more clinically relevant than the initial immune response to vaccine. Many clinical trials of therapeutic vaccines in cancer patients have reported multiple examples of T-cell antigen cascade.16-20 Some studies have also suggested improved clinical outcomes for patients who demonstrated a broadened immune response to epitopes not found in the vaccine.19,20
Implications for Personalized Therapy
The phenomenon of antigen cascade means that a patient treated with a therapeutic vaccine could potentially generate an immune response tailor-made to his or her individual tumor—a response that may be more clinically relevant than the response to the epitope found in the vaccine. Furthermore, unlike with traditional therapies, an ongoing, dynamic immune response can adapt to subsequent mutations within the tumor, continuing or expanding a therapeutic response. The built-in ability of an immune response to adjust to changes within the tumor, to target mutations (which may be much more immunogenic than tumor-associated antigens), and to develop higher-avidity T-cell responses over time, may very well provide the best opportunity for personalized medicine. A lack of significant side effects, along with our growing understanding of when to use this modality and what clinical outcomes to look for, indicate a bright future for therapeutic vaccines in our increasingly more sophisticated and from a patient standpoint, better tolerated fight against cancer.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/22106
References
- 1.Stein WD, Gulley JL, Schlom J, Madan RA, Dahut W, Figg WD, et al. Tumor regression and growth rates determined in five intramural NCI prostate cancer trials: the growth rate constant as an indicator of therapeutic efficacy. Clin Cancer Res. 2011;17:907–17. doi: 10.1158/1078-0432.CCR-10-1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Madan RA, Gulley JL, Fojo T, Dahut WL. Therapeutic cancer vaccines in prostate cancer: the paradox of improved survival without changes in time to progression. Oncologist. 2010;15:969–75. doi: 10.1634/theoncologist.2010-0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlom J, Arlen PM, Gulley JL. Cancer vaccines: moving beyond current paradigms. Clin Cancer Res. 2007;13:3776–82. doi: 10.1158/1078-0432.CCR-07-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bilusic M, Gulley JL. Endpoints, patient selection, and biomarkers in the design of clinical trials for cancer vaccines. Cancer Immunol Immunother. 2012;61:109–17. doi: 10.1007/s00262-011-1141-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. IMPACT Study Investigators Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 7.Gajewski TF. Failure at the effector phase: immune barriers at the level of the melanoma tumor microenvironment. Clin Cancer Res. 2007;13:5256–61. doi: 10.1158/1078-0432.CCR-07-0892. [DOI] [PubMed] [Google Scholar]
- 8.Hale DF, Clifton GT, Sears AK, Vreeland TJ, Shumway N, Peoples GE, et al. Cancer vaccines: should we be targeting patients with less aggressive disease? Expert Rev Vaccines. 2012;11:721–31. doi: 10.1586/erv.12.39. [DOI] [PubMed] [Google Scholar]
- 9.Gulley JL, Madan RA, Schlom J. Impact of tumour volume on the potential efficacy of therapeutic vaccines. Curr Oncol. 2011;18:e150–7. doi: 10.3747/co.v18i3.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gulley JL, Drake CG. Immunotherapy for prostate cancer: recent advances, lessons learned, and areas for further research. Clin Cancer Res. 2011;17:3884–91. doi: 10.1158/1078-0432.CCR-10-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rotow J, Gameiro SR, Madan RA, Gulley JL, Schlom J, Hodge JW. Vaccines as monotherapy and in combination therapy for prostate cancer. Clin Transl Sci. 2010;3:116–22. doi: 10.1111/j.1752-8062.2010.00186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hodge JW, Guha C, Neefjes J, Gulley JL. Synergizing radiation therapy and immunotherapy for curing incurable cancers. Opportunities and challenges. Oncology. 2008;22:1064–70. [PMC free article] [PubMed] [Google Scholar]
- 13.Brandmaier AG, Leitner WW, Ha SP, Sidney J, Restifo NP, Touloukian CE. High-avidity autoreactive CD4+ T cells induce host CTL, overcome T(regs) and mediate tumor destruction. J Immunother. 2009;32:677–88. doi: 10.1097/CJI.0b013e3181ab1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kudo-Saito C, Schlom J, Hodge JW. Induction of an antigen cascade by diversified subcutaneous/intratumoral vaccination is associated with antitumor responses. Clin Cancer Res. 2005;11:2416–26. doi: 10.1158/1078-0432.CCR-04-1380. [DOI] [PubMed] [Google Scholar]
- 15.Hodge JW, Sharp HJ, Gameiro SR. Abscopal regression of antigen disparate tumors by antigen cascade after systemic tumor vaccination in combination with local tumor radiation. Cancer Biother Radiopharm. 2012;27:12–22. doi: 10.1089/cbr.2012.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gulley JL, Arlen PM, Bastian A, Morin S, Marte J, Beetham P, et al. Combining a recombinant cancer vaccine with standard definitive radiotherapy in patients with localized prostate cancer. Clin Cancer Res. 2005;11:3353–62. doi: 10.1158/1078-0432.CCR-04-2062. [DOI] [PubMed] [Google Scholar]
- 17.Lechleider RJ, Arlen PM, Tsang KY, Steinberg SM, Yokokawa J, Cereda V, et al. Safety and immunologic response of a viral vaccine to prostate-specific antigen in combination with radiation therapy when metronomic-dose interleukin 2 is used as an adjuvant. Clin Cancer Res. 2008;14:5284–91. doi: 10.1158/1078-0432.CCR-07-5162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madan RA, Mohebtash M, Arlen PM, Vergati M, Rauckhorst M, Steinberg SM, et al. Ipilimumab and a poxviral vaccine targeting prostate-specific antigen in metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13:501–8. doi: 10.1016/S1470-2045(12)70006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Disis ML, Wallace DR, Gooley TA, Dang Y, Slota M, Lu H, et al. Concurrent trastuzumab and HER2/neu-specific vaccination in patients with metastatic breast cancer. J Clin Oncol. 2009;27:4685–92. doi: 10.1200/JCO.2008.20.6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hardwick N, Chain B. Epitope spreading contributes to effective immunotherapy in metastatic melanoma patients. Immunotherapy. 2011;3:731–3. doi: 10.2217/imt.11.62. [DOI] [PubMed] [Google Scholar]


