Abstract
Background:
There is no consensus on the most effective strategy (mammography or magnetic resonance imaging (MRI)) for screening women with BRCA1 or BRCA2 mutations. The effectiveness and cost-effectiveness of the Dutch, UK and US screening strategies, which involve mammography and MRI at different ages and intervals were evaluated in high-risk women with BRCA1 or BRCA2 mutations.
Methods:
Into a validated simulation screening model, outcomes and cost parameters were integrated from published and cancer registry data. Main outcomes were life-years gained and incremental cost-effectiveness ratios. The simulation was situated in the Netherlands as well as in the United Kingdom, comparing the Dutch, UK and US strategies with the population screening as a reference. A discount rate of 3% was applied to both costs and health benefits.
Results:
In terms of life-years gained, the strategies from least to most cost-effective were the UK, Dutch and US screening strategy, respectively. However, the differences were small. Applying the US strategy in the Netherlands, the costs were €43 800 and 68 800 for an additional life-year gained for BRCA1 and BRCA2, respectively. At a threshold of €20 000 per life-year gained, implementing the US strategy in the Netherlands has a very low probability of being cost-effective. Stepping back to the less-effective UK strategy would save relatively little in costs and results in life-years lost. When implementing the screening strategies in the United Kingdom, the Dutch, as well as the US screening strategy have a high probability of being cost-effective.
Conclusion:
From a cost-effectiveness perspective, the Dutch screening strategy is preferred for screening high-risk women in the Netherlands as well as in the United Kingdom.
Keywords: breast cancer, BRCA1 and BRCA2 genes, radiation-induced neoplasm, hereditary cancer, screening, costs/cost-effectiveness, simulation model
Women with a mutation in the BRCA1 or BRCA2 gene are at an increased lifetime breast cancer risk and they have a younger mean age at breast cancer diagnosis than that in the general population (mean age of onset: BRCA1, 53.9 years; BRCA2, 58.5 years; general population, 69.5 years) (Easton et al, 1995; Ford et al, 1998; Chen and Parmigiani 2007). These women are therefore offered mammography screening, which, in the general population, is the only screening test associated with reduced breast cancer mortality (Glasziou and Houssami 2011). However, mammography has reduced screening sensitivity in younger age groups (Yankaskas et al, 2010) and in gene mutation carriers (Warner et al, 2008). It has an increased risk of false-positive results at young age (Armstrong et al, 2007), which may cause distress and unnecessary biopsies, including surgical biopsy. It also gives an additional risk of radiation-induced tumours, which is particularly relevant in younger women (Preston et al, 2002; BEIR 7, 2006) and in those with cancer susceptibility genes (Jansen-van der Weide et al, 2010; Pijpe A et al, 2012).
The approach to overcome the above-noted limitations of mammography screening has been to use contrast-enhanced magnetic resonance imaging (MRI) to mammography for screening high-risk women, to increase the sensitivity of screening and to reduce the number of mammograms (Lord et al, 2007; Warner et al, 2008; Heijnsdijk et al, 2012). MRI has a higher sensitivity in this context than mammography and does not use ionising radiation. However, MRI has a variable sensitivity for ductal carcinoma in situ, generates higher costs and has a more limited availability and a lower specificity than mammography, which leads to more false positives in screening (Lord et al, 2007; Warner et al, 2008).
Recently, we published a validation study of the Simulation Model on Radiation Risk and breast cancer Screening (SiMRiSc), which quantified screening benefits and risks in various scenarios for women at an increased hereditary breast cancer risk (Greuter et al, 2010). The simulation model was shown to be valid and suitable for the provision of accurate benefits and risks estimates necessary for the refinement of screening guidelines in these women. The purpose of the present study is, therefore, to evaluate both the effectiveness and cost-effectiveness of existing breast cancer screening strategies in which MRI and mammography are used to screen women at an increased hereditary breast cancer risk with this simulation model.
Methods
Description of the simulation model for screening
We used the SiMRiSC model (Greuter et al, 2010; Lu et al, 2012) based on Jacobi et al (2006) and extended the model by incorporating data on the specificity of screening, on population death rates and on associated costs. In this micro-simulation model, women who had a chance of developing breast cancer and of death were followed up every year, based on probability functions. During the screening period, breast cancers were detected by mammography and/or MRI, based on the sensitivity of both modalities. In addition, during the screening period, breast cancers can develop and can clinically manifest between imaging. These are counted during the screening period as interval cancers. When a cancer is screen-detected or has become clinically manifested, costs of therapy and of hospital stay are calculated (see Description of the cost model). Women leave the simulation model when they die.
The parameters of the model
All values of the parameters that were used in the model were derived from literature (Table 1).
Table 1. Parameters of the screening model.
| Model component | Parameter | Baseline estimate | Mininum estimate | Maximum estimate | Reference |
|---|---|---|---|---|---|
| Tumour induction due to radiation risk | Dose (mSv) | 3 | 1 | 5 | Peer et al (1993) |
| |
The lifetime probability of tumour induction |
0.51 |
0.28 |
0.83 |
Preston et al (2002) |
| Preclinical tumour growth |
Mean preclinical period (years) |
|
|
|
|
| <50 years | 1.9 | 0.63 | 3.17 | Peer et al (1996); Tilanus-Linthorst et al (2007); Kriege et al (2006) | |
| 50–70 years | 3.7 | 1.23 | 6.17 | ||
| |
>70 years |
4.5 |
1.50 |
7.50 |
|
| |
s.d. (years) |
|
|
|
|
| <50 years | 0.63 | 0.21 | 1.05 | (Peer et al, 1996; Tilanus-Linthorst et al, 2007; Kriege et al, 2006) | |
| 50–70 years | 0.51 | 0.17 | 0.85 | ||
| |
>70 years |
1.06 |
0.35 |
1.77 |
|
| |
Tumour-doubling times (days) |
|
|
|
|
| <50 years | 80 | 27 | 133 | Peer et al (1996); Tilanus-Linthorst et al (2007); Kriege et al (2006)) | |
| 50–70 years | 157 | 52 | 262 | ||
| |
>70 years |
188 |
63 |
313 |
|
| Risk of developing breast during life |
BRCA1 probability function |
|
|
|
|
| Lifetime risk at age 70 years | 0.80 | 0.71 | 0.84 | Easton et al (1995); Ford et al (1998) | |
| Mean age (years) | 53.9 | 43.9 | 63.9 | ||
| |
s.d. (years) |
16.5 |
5.5 |
28 |
|
| |
BRCA2 probability function |
|
|
|
|
| Lifetime risk at age 70 years | 0.76 | 0.69 | 0.76a | Easton et al (1995); Ford et al (1998) | |
| Mean age (years) | 58.5 | 48.5 | 68.5 | ||
| |
s.d. (years) |
13.8 |
4.6 |
23 |
|
| Sensitivity | Sensitivity of mammography at age <40 years | 0.333 | 0.279 | 0.397 | Kerlikowske et al (2000) |
| Sensitivity of mammography at age 40–49 years | 0.389 | 0.326 | 0.464 | ||
| Sensitivity of mammography at age 50–54 | 0.556 | 0.466 | 0.663 | ||
| Sensitivity of mammography at age 55–59 years | 0.697 | 0.584 | 0.832 | ||
| Sensitivity of mammography at age ⩾60 years | 0.838 | 0.702 | 1 | ||
| |
Sensitivity of MRI for all age groups |
0.770 |
0.593 |
1 |
Warner et al (2008) |
| Specificity | Specificity of mammography at age <40 years | 0.961 | 0.924 | 1 | Kerlikowske et al (2000) |
| Specificity of mammography at age ⩾40 years | 0.946 | 0.909 | 0.984 | ||
| |
Specificity of MRI for all age groups |
0.863 |
0.745 |
1 |
Warner et al (2008) |
| Death rate | Average life expectancy population (years) | 79 | — | — | www.RIVM.nl |
| 5-year survival rate breast cancer patients | www.cijfersoverkanker.nl | ||||
| Tumour diameter <20 mm | 0.98 | — | — | ||
| Tumour diameter 20–50 mm | 0.86 | — | — | ||
| Tumour diameter >50 mm | 0.62 | — | — |
Minimum and maximum estimates correspond with two times the s.d. For a detailed description of the parameters, see Heijnsdijk et al (2012).
The maximum estimate is equal to the baseline estimate because the lifetime risk at the age of 100 years is 100%.
The tumour induction model consisted of the mean glandular dose for a two-view screen-film mammogram and the probability of tumour induction from radiation (BEIR 7, 2006; Zoetelief et al, 2006). The preclinical tumour growth model consisted of the mean and s.d. of the preclinical period based on the average tumour-doubling time of primary breast cancers in women younger than 50 years, in women between 50 and 70 years, and in those who were 70 years and older (Peer et al, 1993, 1996; Tilanus-Linthorst et al, 2007). The risk of developing breast cancer during life consisted of the baseline estimates for the lifetime risk of developing breast cancer for BRCA1 and BRCA2 mutation carriers (Easton et al, 1995; Ford et al, 1998). The sensitivity model consisted of mean sensitivities for film mammography and MRI; mean sensitivity of mammography was for five age groups (Kriege et al, 2006; Kerlikowske et al, 2000), whereas mean sensitivity of MRI was an overall sensitivity, as it was independent of age (Warner et al, 2008).
The specificity model consisted of the mean specificities for each of mammography and MRI; mean specificity of mammography was for women younger (or older) than 40 years of age (Kriege et al, 2006) and mean MRI specificity was an overall specificity that was independent of age (Warner et al, 2008). The population death-rate model consisted of the cumulative death rates at ages up to 100 years, based on the Dutch cohort who were born in 1970 (www.statline.cbs.nl. The breast cancer death risk consisted of the probability of death from breast cancer that was linked to the tumour volume according to the preclinical tumour growth model (www.cijfersoverkanker.nl).
Description of the cost model
Cost parameters included the direct costs of screening, diagnostics, therapy and hospital stay (Table 2). Costs of screening included that of mammography examination and/or an MRI examination. Costs of diagnostics included the costs of biopsy and of histopathological analysis. Costs of therapy included costs of surgical, chemotherapeutic endocrine and/or radiotherapeutic treatment. The costs were estimated for the Netherlands and for United Kingdom separately. For the calculation of the costs in the Netherlands, the unit prices for screening, diagnostics and therapy were based on current national tariffs and the Dutch published studies on cost prices (www.cvz.nl; Flobbe et al, 2004; LPRM and NABON, 2000; Farmacotherapeutisch Kompas, 2000/2001; Slotman et al, 2000; Oostenbrink et al, 2000). For the calculation of costs in the UK scenario, data were based on national tariffs and the UK studies on cost prices (NICE, 2006; Prescott et al, 2007). Mean treatment costs per patient were calculated by combining prices and treatment data from the Dutch regional cancer registry, stratified by tumour size (Table 3).
Table 2. Resource items for screening, diagnostics and treatment: unit prices for the Netherlands and the United Kingdom, and sources.
| Cost category | Unit price € (The Netherlands) | Source | Unit price £ (United Kingdom) | Source/HRG code |
|---|---|---|---|---|
|
Screening | ||||
| Mammography (National Breast Screening Program) | 69 | www.cvz.nl | 46 | www.whnt.nhs.uk |
| Mammography (hospital) | 92 | www.cvz.nl | 58 | NICE (2006) |
| MRI |
227 |
www.cvz.nl |
220 |
Prescott et al (2007) |
|
Diagnostics | ||||
| Pathology and evaluation |
75 |
Flobbe et al (2004) |
122 |
Prescott et al (2007) |
|
Treatment | ||||
| Breast conserving therapy | 1009 | www.cvz.nl | 808 | a |
| Mastectomy | 1856 | www.cvz.nl | 2549 | HRG J11 |
| Radiation therapy | 2891 | Flobbe et al (2004); LPRM and NABON (2000); Slotman et al (2000) | 2316 | a |
| Chemo therapy | 950 | Flobbe et al (2004); Slotman et al (2000) | 761 | a |
| Hormonal therapy | 733 | Flobbe et al (2004); Slotman et al (2000) | 587 | a |
| Specialist visits | 672 | Flobbe et al (2004) | 538 | a |
| Specialist visits (adjuvant therapy) | 1788 | Flobbe et al (2004) | 1433 | a |
| Hospital stay | 1594 | Flobbe et al (2004); Oostenbrink et al (2000) | 1277 | a |
Abbreviation: HRG=Healthcare Research Group.
If there was no HRG code, prices calculated were based on the balance between the per capita expenditures of the Netherlands vs that of the United Kingdom (0.84) (stats.oecd.org, visited online: June 2012) and the conversion rate on 1 January 2009, which is 0.96 for UK pounds (www.x-rates.com visited online: June 2012).
Table 3. Mean treatment costs per patient by tumour size.
| |
⩽2 cm |
>2 cm and ⩽5 cm |
>5 cm |
|||
|---|---|---|---|---|---|---|
| Costs € | Costs £ | Costs € | Costs £ | Costs € | Costs £ | |
| Total therapy |
4268 |
3909 |
4812 |
4105 |
5426 |
4789 |
| Hospital stay |
1589 |
1273 |
1573 |
1260 |
1580 |
1266 |
| Total | 5857 | 5182 | 6485 | 5365 | 7006 | 6055 |
Validation of the model
The SiMRiSC model was validated by comparing model-predicted outcome data with observed data from three published large screening studies of women with an increased hereditary breast cancer risk (Greuter et al, 2010). A sensitivity analysis was used to estimate the error margins of model-predicted outcome data and to analyse the sensitivity of the simulation model to each input parameter. It was shown that the model predicted the number of tumours reported to a high accuracy. The model was the most sensitive to changes in the parameters related to the lifetime breast cancer risk and the sensitivity of mammography.
Screening strategies
Three existing screening strategies were evaluated (Table 4). The Dutch strategy uses an annual MRI analysis for women aged 25–30 years, annual mammography and MRI for those aged 30–60 years and a biennial mammography-only for those aged 60–75 years (www.cbo.nl). The UK strategy uses an annual mammography and MRI analysis for women aged 30–50 years and a mammography-only for those aged 50–70 years for every 3 years (www.nice.org.uk). The US strategy includes an annual mammography and MRI analysis for women aged 25 years until the end of life, according to the American Cancer Society guidelines and the National Comprehensive Cancer Network guidelines (Saslow et al, 2007; www.NCCN.org). When the strategy in the model recommended a mammography and an MRI analysis, these techniques were performed sequentially: first, mammography was performed and, if positive, a screen-detected breast cancer was counted. If the mammography was negative, an MRI was subsequently performed.
Table 4. Evaluated screening strategies for breast cancer in women with a BRCA1/2/u mutation.
| Age (years) | Dutch strategy | UK strategy | US strategy |
|---|---|---|---|
| 25–30 |
MRI every year |
No screening |
MRI and mammography every year |
| 30–50 |
MRI and mammography every year |
MRI and mammography every year |
MRI and mammography every year |
| 50–60 |
MRI and mammography every year |
Mammography every 3 years in NBSP |
MRI and mammography every year |
| 60–70 |
Mammography every 2 years in NBSP |
Mammography every 3 years in NBSP |
MRI and mammography every year |
| 70–75 |
Mammography every 2 years in NBSP |
No screening |
MRI and mammography every year |
| Age over 75 when being in good health | No screening | No screening | MRI and mammography every year |
Abbreviation: NBSP=National Breast Cancer Screening Program.
Input population
The input population consisted of a cohort of 10 000 women followed since the age of 20 years. On the basis of the lifetime probability function for breast cancer given the woman's specific gene mutation and age (Easton et al, 1995; Ford et al, 1998), breast cancers were distributed randomly over the simulated population each year. Each year, the age of the women was increased, existing tumours were allowed to grow based on age (Peer et al, 1993, 1996; Tilanus-Linthorst et al, 2007), women died as based on a probability function (www.rivm.nl) and, during screening, growing breast cancers could be detected by mammography and/or MRI scanning based on the sensitivity of both modalities and the screening strategy of the specific country (Kerlikowske et al, 2000; Kriege et al, 2006; Yankaskas et al, 2010).
Analysis and model output
The output of the model (Tables 5a and , b) was given in terms of the absolute number of small tumours (diameter <2 cm) detected, the number of tumours detected with mammography or MRI screening, the number of interval cancers, the number of tumours diagnosed before the start of screening and those after commencing the screening, the number of mammography examinations (within the hospital and within the National Breast Cancer Screening Program), the number of MRI examinations and the number of false positives for mammography and MRI. We calculated the life-years gained by high-risk screening, the costs of this screening and the incremental cost-effectiveness rate (ICER) defined as the ratio of the additional costs per life-year gained, where the national strategy was the reference. The simulation was run for the two gene types separately. In the analyses, a discount rate of 3% per year was applied to costs and life-years from 20 years of age.
Table 5a. Comparison of the Dutch screening strategy as implemented in NL.
|
Genetic mutation |
BRCA1 |
BRCA2 |
||||
|---|---|---|---|---|---|---|
| Screening strategy | NL | UK | US | NL | UK | US |
| Small tumours detected (<2 cm) |
750±11 |
663±15 |
799±11 |
777±12 |
696±11 |
821±13 |
| Tumours detected |
791±23 |
717±22 |
838±24 |
814±17 |
749±15 |
851±18 |
| Interval cancers |
88±11 |
153±12 |
59±6 |
61±5 |
119±9 |
32±5 |
| Tumours diagnosed before start of screening |
42±6 |
73±11 |
43±7 |
16±3 |
36±5 |
17±4 |
| Tumours diagnosed after end of screening |
26±6 |
30±5 |
N.A. |
27±5 |
30±4 |
N.A. |
| Mammography examinations in hospital ( × 1000) |
18.9±0.5 |
15.2±0.4 |
24.5±0.4 |
21.1±0.3 |
16.7±0.2 |
27.4±0.3 |
| Mammography examinations in NBSP ( × 1000) |
1.0±0.1 |
3.2±0.2 |
N.A. |
1.2±0.1 |
3.9±0.1 |
N.A. |
| MRI examinations ( × 1000) |
23.2±0.5 |
15.1±0.2 |
23.9±0.3 |
25.6±0.3 |
16.6±0.1 |
26.8±0.3 |
| False-positive mammographies |
904±36 |
831±30 |
1.081±28 |
1.033±46 |
939±34 |
1.231±38 |
| False-positive MRIs |
3.139±86 |
2.033±48 |
3.231±71 |
3.448±38 |
2.249±40 |
3.624±74 |
| Years of life gained (years/woman)a |
1.614 |
1.366 |
1.620 |
1.217 |
1.077 |
1.221 |
| Additional costs ( × €1000 per woman)b |
2.292 |
1.572 |
2.555 |
2.511 |
1.743 |
2.786 |
| Additional costs per life-year gained compared with NL strategy ( × €1000 per year per woman) | — | 2.9c | 43.8 | — | 5.5c | 68.8 |
Abbreviations: MRI=magnetic resonance imaging; N.A.=not applicable; NBSP=National Breast Cancer Screening Program; NL=The Netherlands
Comparison of the Dutch screening strategy as implemented in NL, with the British (UK) and American (US) screening strategy when implemented in NL, assuming simultaneous application of the Dutch NBSP. Average values of absolute numbers±s.d. per 1000 women with a BRCA1 or BRCA2 genetic mutation.
Reference is Dutch NBSP.
Additional costs with reference to Dutch NBSP, all cost estimates based on Dutch prices.
Savings: programme is less expensive and adds less life-years gained with respect to the Dutch strategy.
Table 5b. Comparison of the UK's screening strategy as implemented in the United Kingdom.
|
Genetic mutation |
BRCA1 |
BRCA2 |
||||
|---|---|---|---|---|---|---|
| Screening strategy | NL | UK | US | NL | UK | US |
| Small tumours detected (<2 cm) |
684±12 |
552±18 |
748±11 |
670±12 |
545±15 |
755±9 |
| Tumours detected |
731±21 |
624±18 |
781±25 |
715±16 |
618±21 |
781±16 |
| Interval cancers |
144±13 |
241±14 |
114±9 |
146±13 |
241±15 |
101±10 |
| Tumours diagnosed before start of screening |
37±8 |
76±8 |
41±7 |
16±4 |
37±6 |
17±4 |
| Tumours diagnosed after end of screening |
83±8 |
100±10 |
54±5 |
110±13 |
129±7 |
64±9 |
| Mammography examinations in hospital ( × 1000) |
19.0±0.4 |
15.2±0.1 |
24.7±0.3 |
21.1±0.3 |
16.6±02 |
27.4±0.4 |
| Mammography examinations in NBSP ( × 1000) |
0.7±0.1 |
2.2±0.1 |
N.A. |
0.9±0.1 |
2.7±0.1 |
N.A. |
| MRI examinations ( × 1000) |
23.4±0.4 |
15.1±0.1 |
24.2±0.3 |
25.7±0.3 |
16.5±0.2 |
26.8±0.4 |
| False-positive mammographies |
909±21 |
778±25 |
1.097±21 |
1.015±33 |
871±27 |
1.222±33 |
| False-positive MRIs |
3.134±79 |
2.035±28 |
3.273±62 |
3.457±59 |
2.245±49 |
3.624±77 |
| Years of life gained (years per woman)a |
1.625 |
1.368 |
1.628 |
1.231 |
1.077 |
1.231 |
| Additional costs ( × 1000 per woman)b |
2.153 |
1.454 |
2.350 |
2.339 |
1.588 |
2.550 |
| Additional costs per life-year gained compared with the UK strategy ( × 1000 per year per woman) | 2.7 | — | 3.4 | 4.9 | — | 6.2 |
Abbreviations: MRI=magnetic resonance imaging; N.A.=not applicable; NBSP=National Breast Cancer Screening Program; NL=The Netherlands.
Comparison of the UK's screening strategy as implemented in the United Kingdom with the Dutch (NL) and American (US) screening strategy when implemented in the United Kingdom, assuming simultaneous application of the UK NBSP. Average values of absolute numbers±s.d. per 1000 women with a BRCA1 or BRCA2 genetic mutation.
Reference is British NBSP.
Additional costs with reference to British NBSP, all cost estimates based on British prices.
The simulation was carried out in the Netherlands, comparing the three screening strategies with the Dutch population screening as a reference, and a cost threshold of €20 000 was considered (Habbema et al, 1989). As the population screening was the reference and this differs over countries, in a second analysis the simulation was carried out in the United Kingdom and the British population screening was used as a reference. In this analysis, a cost threshold of £25 000 was considered (National Institute for Health and Clinical Excellence, 2007).
Sensitivity analysis
A probabilistic sensitivity analysis (PSA) was performed for the ICER outcome. In 100 simulations, each consisting of 1000 women, the input parameters of the model were randomly selected from a skewed Gaussian distribution, with a mean equal to the parameter's baseline estimate and a negative s.d. equal to half the difference between the mean and the minimum estimate, and with a positive s.d. equal to half the difference between the maximum and the mean estimate (Table 1). On the basis of the outputs of the PSA, cost-effectiveness acceptability curves were constructed (Matchar et al, 2005).
Results
Table 5a summarises model outputs stratified for BRCA1 and BRCA2 for all three screening strategies when implemented in the Netherlands, whereas Table 5b summarises model outputs for all three screening strategies when implemented in the United Kingdom. The earlier the screening started (the Dutch and US strategies), the higher the number of small tumours (<2 cm) that was detected (Table 5a). This effect was most pronounced among the women with a BRCA1 or BRCA2 mutation. In addition, the earlier the screening started, the lower the number of tumours that was diagnosed before commencing the screening; this was most pronounced among women with a BRCA1 mutation.
The longer the screening was continued (the US strategy offers the longest time for continuing screening), the more the tumours were diagnosed. The longer the screening was offered, the smaller the number of tumours that was diagnosed after stopping the screening. More frequent MRI screens (the US strategy offers the most frequent MRI screens) resulted in less interval cancers. The numbers of false positives for mammography screening and for MRI screening were highest in the US strategy and were lowest in the UK strategy for all groups.
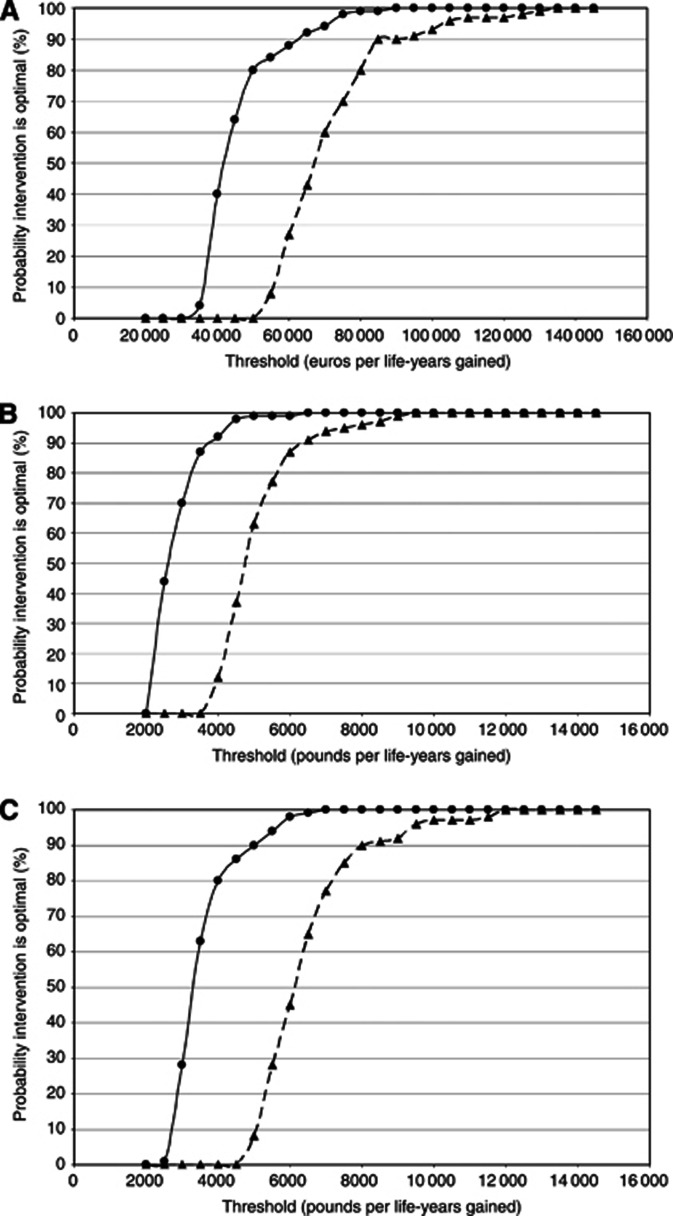
When applying the US strategy in the Netherlands, €43 800 and 68 800 should be paid for an additional life-year gained for BRCA1 and BRCA2, respectively (Table 5a). At a threshold of €20 000 per life-year gained, implementing the US strategy in the Netherlands has a very low probability of being cost-effective. However, if the Dutch are willing to pay €50 000 per life-year gained, then the US strategy has a more than 80% probability of being cost-effective (see Figure 1A). Stepping back to the less-effective UK strategy would save relatively little in costs and result in life-years lost. The ICERs are a few thousand euros per life-year gained, indicating that the Dutch strategy is cost-effective compared with the UK strategy.
Figure 1.
Cost-effectiveness acceptability curves. Cost-effectiveness acceptability curves for the implementation of the US screening strategy in the Netherlands (A), of the Dutch screening strategy in the United Kingdom (B) and of the US screening strategy in the United Kingdom (C) for BRCA1 (solid line, circles) and BRCA2 (dashed line, triangles) mutation carriers. Shown is the probability that the alternative intervention is cost effective at a certain cost threshold in euros or pounds per life-years gained.
When the simulation was carried out in the United Kingdom, the US screening strategy was somewhat more effective for estimates of life-years gained as compared with the Dutch strategy (Table 5b). Both the US and the Dutch screening strategy were more effective for estimates of life-years gained as compared with the UK strategy. When applying the Dutch strategy in the United Kingdom, £2700 and 4900 should be paid for an additional life-year gained for BRCA1 and BRCA2, respectively (Table 5b). Turning to the even more intensive US strategy in the United Kingdom would cost an additional £3400 and 6200 per life-year gained (Table 5b). Thus, at current UK thresholds, the Dutch and the US strategy are an extension with additional costs per QALY that have a high (100%) probability of falling below the UK threshold (see Figures 1B and C).
Discussion
Differences between the currently recommended screening strategies for women at high risk of developing breast cancer reflects the uncertainties surrounding the optimal screening commencement (and stopping) age, duration and frequency of screening, and the schedule for integrating mammography and MRI screening. Using simulation modelling, we found that the US screening strategy showed a small increase in the number of life-years gained compared with the Dutch strategy, and both the US and the Dutch screening strategies were more effective in terms of life-years gained compared with the UK strategy. Applying the US strategy in the Netherlands would cost €43 800 and 68 800 for an additional life-year gained for BRCA1 and BRCA2, respectively. The cost-effectiveness acceptability curves confirm that the Dutch strategy seems the most cost-effective option.
Screening BRCA1 mutation carriers was more cost-effective than screening BRCA2 mutation carriers. This may be partly explained by the higher lifetime risk of breast cancer in BRCA1 mutation carriers than BRCA2 mutation carriers, 0.80 and 0.76 by age 70 years, respectively, as well as the lower mean age of onset in BRCA1 mutation carriers, 53.9 vs 58.5 years, respectively (Chen and Parmigiani, 2007; Van der Kolk et al, 2010). Because of the higher incidence and the lower mean age of breast cancer among BRCA1 mutation carriers, more women with BRCA1 mutations are expected to die of breast cancer and, hence, there may be greater potential for life-years gained by screening this group (Kurain et al, 2010).
For BRCA1 and BRCA2 mutation carriers in the Netherlands, the Dutch screening strategy, starting MRI-only screening at age 25 years, was most cost-effective (Table 5a). The US strategy, which combines MRI scanning and mammography from the age of 25 years, gave only a small increase in the number of life-years gained relative to the Dutch strategy, and a slight reduction in interval cancers. A likely explanation for this finding is that the sensitivity of screening mammography in women between age 25 and 30 years is relatively low, that is, 0.333 (Johnstone et al, 2001). Hence, mammography between age 25 and 30 years does not increase benefit over commencing with MRI-alone screening from 25–30 years (Heijnsdijk et al, 2012). The small increase in the number of life-years gained through screening in the US strategy relative to the Dutch strategy might also be an effect of radiation-induced tumours; the estimated additional amount of induced breast tumours was 0.6% (Jansen-van der Weide et al, 2010; Pijpe et al, 2012). Of note, the longer duration of screening with MRI in the US strategy considerably increases screening costs and false-positive screens relative to the Dutch and UK strategies, which reduces the cost-effectiveness of screening.
The strengths of the modelling reported in this work include the construct of model parameter values, which were mostly derived from publications concerning women with BRCA1 or BRCA2 mutations. Furthermore, the model was applied to currently applied guideline-based screening scenarios, and included the effects of MRI and of X-ray tumour induction, as well as cost analysis, to guide selection of the most cost-effective screening strategy. Importantly, we considered costs of screening, as well as costs of treatment (stratified for tumour size) and hospital stay, whereas most studies on this topic limit their scope to costs of screening. In addition, the costs included in this analysis were based on a detailed country-specific cost study of the prices for diagnostics and treatment of early-stage breast cancer, and a discount rate was applied to costs and life-years.
Estimates for the costs of advanced breast cancer, including distant metastases, diagnostics and treatment, were not included in the current model. For this reason, we think that this model underestimates the costs of breast cancer treatment, which will be a problem when the model is applied to assess the overall cost-effectiveness of the breast cancer screening in high-risk women, rather than choosing which strategy is best. Furthermore, as the main focus of the present paper was to study the cost-effectiveness comparing the different strategies situated in the Netherlands or in the United Kingdom, the US prices were not used. If the simulation had been carried out in the United States, the fact that the per capita health-care expenditures are about 2.05 times higher in the United States has to be taken into account (stats.oecd.org). Another limitation is that we did not incorporate quality-of-life parameters that may be relevant in breast cancer screening, in line with the work of Rijnsburger et al (2004), suggesting that there is no loss of quality of life due to screening in high-risk women. Although we did not consider quality-of-life parameters to be in the scope of the present work, it represents an important topic for further research. A further limitation might be that screening vs clinical detection was not directly but indirectly included by assuming breast cancer mortality to be dependent on tumour volume. In addition, the dose and the sensitivity were based on film mammography, although current clinical practice includes digital mammography, which has a lower dose, and digital mammography is more accurate in women under 50 years and in pre-menopausal women (Pisano et al, 2005) However, as in the population screening programme most screenings are captured on a film, we modelled the film mammography. A related potential limitation is that additional sensitivity analyses, such as two-way sensitivity analysis of diagnostic test performance, were not performed. However, we learned from previous analyses that penetrance was the most influential factor in this model (Greuter et al, 2010); hence, analyses including a lower dose and additional sensitivity analyses are unlikely to alter our findings. An inherent limitation of simulation modelling is that some of the included parameters are associated with uncertainty—in our model, these uncertainties are predominantly determined by the uncertainties in the lifetime risk of developing breast cancer, and also in the preclinical growth model parameter, as indicated by the sensitivity analysis of the main model output. As there is a lot of international variability in the uptake of prevention strategies in BRCA1 and BRCA2 mutation carriers, and as their effect is under debate, this was not included in our model (Metcalfe et al, 2007; Fakkert et al, 2012).
The strategies we evaluated for screening women with BRCA1 or BRCA2 mutations were the recommended strategies in the Netherlands, in the United Kingdom and in the United States. As these strategies are partly based on evidence and partly on expert opinions, recommendations are continuously being adapted to new data. For example, in a recent online publication supplementing the NICE guidelines, it was proposed to intensify frequency of mammography screening in the United Kingdom for age 50–60 years in some high-risk groups (www.icr.ac.uk). Here we have presented information to further support tailoring screening recommendations for women with BRCA1 and BRCA2 mutations.
In conclusion, from a cost-effectiveness perspective, the Dutch screening strategy is preferred in the Netherlands for the screening of high-risk women. The highly intensive US strategy does not seem to be a cost-effective option in the Dutch situation. The less-effective UK strategy would save relatively little in costs and result in life-years lost.
The authors declare no conflict of interest.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- Armstrong K, Moye E, Williams S, Berlin JA, Reynolds EE. Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians. Ann Intern Med. 2007;146:516–526. doi: 10.7326/0003-4819-146-7-200704030-00008. [DOI] [PubMed] [Google Scholar]
- LPRM and NABON 2000Behandelingsrichtlijnen radiotherapie van het operabele mammacarcinoom na mamma-amputatie en okselkliertoilet in Nederland Landelijk Platform voor Radiotherapie en Mammacarcinoom (LPRM) en NABON; 1–13.In Dutch. [Google Scholar]
- BEIR 7 . National Research Council, Committee on the Biological Effects of Ionizing Radiation. Health Effects of Exposure to Low Levels of Ionizing Radiation (BEIR VII Phase 2. National Academy Press: Washington DC; 2006. [Google Scholar]
- Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25:1329–1333. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton DF, Ford D, Bishop DT. Breast and ovarian cancer incidence in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Am J Hum Genet. 1995;56:265–271. [PMC free article] [PubMed] [Google Scholar]
- Fakkert IE, Mourits MJ, Jansen L, van der Kolk DM, Meijer K, Oosterwijk JC, van der Vegt B, Greuter MJ, de Bock GH. Breast cancer incidence after risk-reducing salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers. Cancer Prev Res. 2012;5:1291–1297. doi: 10.1158/1940-6207.CAPR-12-0190. [DOI] [PubMed] [Google Scholar]
- Farmacotherapeutisch Kompas 2000/2001Medisch farmaceutische voorlichting College voor Zorgverzekeringen: Amstelveen; In Dutch. [Google Scholar]
- Flobbe K, Kessels AG, Severens JL, Beets GL, de Koning HJ, von Meyenfeld MF, van Engelshoven JM. Costs and effects of ultrasonography in the evaluation of palpable breast masses. Int J Technol Assess Health Care. 2004;20:440–448. doi: 10.1017/s0266462304001333. [DOI] [PubMed] [Google Scholar]
- Ford D, Easton DF, Stratton M, Narod S, Goldgar D, Devilee P, Bishop DT, Weber B, Lenoir G, Chang-Claude J, Sobol H, Teare MD, Struewing J, Arason A, Scherneck S, Peto J, Rebbeck TR, Tonin P, Neuhausen S, Barkardottir R, Eyfjord J, Lynch H, Ponder BA, Gayther SA, Zelada-Hedman M. Breast Cancer Linkage Consortium. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. Am J Hum Genet. 1998;62:676–689. doi: 10.1086/301749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasziou P, Houssami N. The evidence base for breast cancer screening. Prev Med. 2011;53:100–102. doi: 10.1016/j.ypmed.2011.05.011. [DOI] [PubMed] [Google Scholar]
- Greuter MJW, Jansen-Van der Weide MC, Jacobi CE, Oosterwijk JC, Jansen L, Oudkerk M, de Bock GH. The validation of a simulation model incoporating radiation risk for mammography breast cancer screening in women with a hereditary-increased breast cancer risk. Eur J Cancer. 2010;46:495–504. doi: 10.1016/j.ejca.2009.10.030. [DOI] [PubMed] [Google Scholar]
- Habbema JDF, Casparie AF, Mulder JH, Rutten FFH. Medische Technology Assessment en gezondheidsbeleid. Samson Stafleu: Alphen aan den Rijn; 1989. [Google Scholar]
- Heijnsdijk EA, Warner E, Gilbert FJ, Tilanus-Linthorst MM, Evans G, Causer PA, Eeles RA, Kaas R, Draisma G, Ramsay EA, Warren RM, Hill KA, Hoogerbrugge N, Wasser MN, Bergers E, Oosterwijk JC, Hooning MJ, Rutgers EJ, Klijn JG, Plewes DB, Leach MO, de Koning HJ. Differences in natural history between breast cancers in BRCA1 and BRCA2 mutation carriers and effects of MRI screening-MRISC, MARIBS, and Canadian studies combined. Cancer Epidemiol Biomarkers Prev. 2012;21:1458–1468. doi: 10.1158/1055-9965.EPI-11-1196. [DOI] [PubMed] [Google Scholar]
- Jacobi CE, Nagelkerke NJ, Van Houwelingen JH, De Bock GH. Breast cancer screening, outside the population-screening program, of women from breast cancer families without proven BRCA1/BRCA2 mutations: a simulation study. Cancer Epidemiol Biomarkers Prev. 2006;15:429–436. doi: 10.1158/1055-9965.EPI-05-0223. [DOI] [PubMed] [Google Scholar]
- Jansen-van der Weide MC, Greuter MJ, Jansen L, Oosterwijk JC, Pijnappel RM, de Bock GH. Exposure to low-dose radiation and the risk of breast cancer among women with a familial or genetic predisposition: a meta-analysis. Eur Radiol. 2010;20:2547–2556. doi: 10.1007/s00330-010-1839-y. [DOI] [PubMed] [Google Scholar]
- Johnstone PA, Moore EM, Carrillo R, Goepfert CJ. Yield of mammography in selected patients age<or=30 years. Cancer. 2001;91:1075–1078. doi: 10.1002/1097-0142(20010315)91:6<1075::aid-cncr1102>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Kerlikowske K, Carney PA, Geller B, Mandelson MT, Taplin SH, Malvin K, Ernster V, Urban N, Cutter G, Rosenberg R, Ballard-Barbash R. Performance of screening mammography among women with and without a first-degree relative with breast cancer. Ann Intern Med. 2000;5:855–863. doi: 10.7326/0003-4819-133-11-200012050-00009. [DOI] [PubMed] [Google Scholar]
- Kriege M, Brekelmans CT, Obdeijn IM, Boetes C, Zonderland HM, Muller SH, Kok T, Manoliu RA, Besnard AP, Tilanus-Linthorst MM, Seynaeve C, Bartels CC, Kaas R, Meijer S, Oosterwijk JC, Hoogerbrugge N, Tollenaar RA, Rutgers EJ, de Koning HJ, Klijn JG. Factors affecting sensitivity and specificity of screening mammography and MRI in women with an inherited risk for breast cancer. Breast Cancer Res Treat. 2006;100:109–119. doi: 10.1007/s10549-006-9230-z. [DOI] [PubMed] [Google Scholar]
- Lord SJ, Lei W, Craft P, Cawson JN, Morris I, Walleser S, Griffiths A, Parker S, Houssami N. A systematic review of the effectiveness of magnetic resonance imaging (MRI) as an addition to mammography and ultrasound in screening young women at high risk of breast cancer. Eur J Cancer. 2007;43:1905–1917. doi: 10.1016/j.ejca.2007.06.007. [DOI] [PubMed] [Google Scholar]
- Lu W, Greuter MJ, Schaapveld M, Vermeulen KM, Wiggers T, de Bock GH. Safety and cost-effectiveness of shortening hospital follow-up after breast cancer treatment. Br J Surg. 2012;99:1227–1233. doi: 10.1002/bjs.8850. [DOI] [PubMed] [Google Scholar]
- Matchar DB, Samsa GP, Liu S. Cost-effectiveness of antiplatelet agents in secondary stroke prevention: the limits of certainty. Value Health. 2005;8:572–580. doi: 10.1111/j.1524-4733.2005.00050.x. [DOI] [PubMed] [Google Scholar]
- Metcalfe KA, Ghadirian P, Rosen B, Foulkes W, Kim-Sing C, Eisen A, Ainsworth P, Horsman D, Maugard C, Provencher D, Robideaux A, Gilchrist D, Chudley A, Lemire EG, Armel S, Finch A, Sun P, Narod SA. Variation in rates of uptake of preventive options by Canadian women carrying the BRCA1 or BRCA2 genetic mutation. Open Med. 2007;1:e92–e98. [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence 2007. Briefing paper for the Methods Working Party on the Cost Effectiveness Threshold, 26 November 2007 www.nice.org.uk/TAMethodsReview .
- NICE 2006Familial Breast Cancer: Partial Update of the NICE Clinical Guideline 14, Costing Report, Implementing NICE Guidance in England National Institute for Health and Clinical Excellence: London; Retrieved from http://www.nice.org.uk on 21 June 2012. [Google Scholar]
- Oostenbrink JB, Koopmanschap MA, Rutten FFH.2000Handleiding voor kostenonderzoek, methoden en richtlijnen voor economische evaluaties in de gezondheidszorg College voor Zorgverzekeringen: Amstelveen; In Dutch. [Google Scholar]
- Peer PG, Van Dijck JA, Hendriks JH, Holland R, Verbeek AL. Age-dependent growth rate of primary breast cancer. Cancer. 1993;71:3547–3551. doi: 10.1002/1097-0142(19930601)71:11<3547::aid-cncr2820711114>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Peer PG, Verbeek ALM, Straatman H, Hendriks JH, Holland R. Age-specific sensitivities of mammographic screening for breast cancer. Breast Cancer Res Treat. 1996;38:153–160. doi: 10.1007/BF01806669. [DOI] [PubMed] [Google Scholar]
- Pijpe A, Andrieu N, Easton DF, Kesminiene A, Cardis E, Noguès C, Gauthier-Villars M, Lasset C, Fricker JP, Peock S, Frost D, Evans DG, Eeles RA, Paterson J, Manders P, van Asperen CJ, Ausems MG, Meijers-Heijboer H, Thierry-Chef I, Hauptmann M, Goldgar D, Rookus MA, van Leeuwen FE, GENEPSO, EMBRACE, HEBON Exposure to diagnostic radiation and risk of breast cancer among carriers of BRCA1/2 mutations: retrospective cohort study (GENE-RAD-RISK) Brit Med J. 2012;345:e5660. doi: 10.1136/bmj.e5660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S, Conant EF, Fajardo LL, Bassett L, D'Orsi C, Jong R, Rebner M, Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group Diagnostic performance of digital vs film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773–1783. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, Goh TT, Lindley R, Cairns J. A randomized controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial. Health Technol Assess. 2007;11:1–149. doi: 10.3310/hta11310. [DOI] [PubMed] [Google Scholar]
- Preston DL, Mattsson A, Holmberg E, Shore R, Hildreth NG, Boice JD., Jr Radiation effects on breast cancer risk: a pooled analysis of eight cohorts. Radiat Res. 2002;158:220–235. doi: 10.1667/0033-7587(2002)158[0220:reobcr]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Rijnsburger AJ, Essink-Bot ML, van Dooren S, Borsboom GJ, Seynaeve C, Bartels CC, Klijn JG, Tibben A, de Koning HJ. Impact of screening for breast cancer in high-risk women on health-related quality of life. Br J Cancer. 2004;91:69–76. doi: 10.1038/sj.bjc.6601912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, Morris E, Pisano E, Schnall M, Sener S, Smith RA, Warner E, Yaffe M, Andrews KS, Russell CA, American Cancer Society Breast Cancer Advisory Group American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75–89. doi: 10.3322/canjclin.57.2.75. [DOI] [PubMed] [Google Scholar]
- Slotman BJ, Levendag PC, Botke G, Leer JWH.2000Producttypering in de radiotherapie Medisch Contact 551198–1200.In Dutch. [Google Scholar]
- Tilanus-Linthorst MM, Obdeijn IM, Hop WC, Causer PA, Leach MO, Warner E, Pointon L, Hill K, Klijn JG, Warren RM, Gilbert FJ. BRCA1 mutation and young age predict fast breast cancer growth in the Dutch, United Kingdom, and Canadian magnetic resonance imaging screening trials. Clin Cancer Res. 2007;13:7357–7362. doi: 10.1158/1078-0432.CCR-07-0689. [DOI] [PubMed] [Google Scholar]
- Van der Kolk DM, De Bock GH, Leegte BK, Schaapveld M, Mourits MJ, de Vries J, van der Hout AH, Oosterwijk JC. Penetrance of breast cancer, ovarian cancer and contralateral breast cancer in BRCA1 and BRCA2 families: high cancer incidence at older age. Breast Cancer Res Treat. 2010;124:643–651. doi: 10.1007/s10549-010-0805-3. [DOI] [PubMed] [Google Scholar]
- Warner E, Messersmith H, Causer P, Eisen A, Shumak R, Plewes D. Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann Intern Med. 2008;148:671–679. doi: 10.7326/0003-4819-148-9-200805060-00007. [DOI] [PubMed] [Google Scholar]
- Yankaskas BC, Haneuse S, Kapp JM, Kerlikowske K, Geller B, Buist DS. Performance of first mammography examination in women younger than 40 years. J Natl Cancer Inst. 2010;102:692–701. doi: 10.1093/jnci/djq090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoetelief J, Veldkamp WJ, Thijssen MA, Jansen JT. Glandularity and mean glandular dose determined for individual women at four regional breast cancer screening units in the Netherlands. Phys Med Biol. 2006;51:1807–1817. doi: 10.1088/0031-9155/51/7/012. [DOI] [PubMed] [Google Scholar]