Abstract
Orphaned children have been found to be at greater risk of poor health and malnutrition compared to non-orphans in sub-Saharan African countries. However, levels of disadvantage vary by location and little is known about the causal pathways that lead from orphanhood to poorer health and malnutrition. Aggregate data from recent Demographic and Health Surveys in 22 countries were used to compare overall levels of ill-health and malnutrition by orphan status. Data from the Manicaland Child Cohort Study in Zimbabwe – a closed cohort study with detailed longitudinal information on orphan’s experience – were used to describe how patterns of ill-health and malnutrition alter over the child’s life-course and to test causal pathways between orphanhood and ill-health and malnutrition, hypothesized in a previously published theoretical frame-work. Modest increases in ill-health and malnutrition were found in orphans in the Demographic and Health Surveys data, with maternal and double orphans being worst affected. Non-significant associations were found between orphanhood and ill-health in the Manicaland Child Cohort Study data, but no associations with malnutrition were found. None the less, smaller increases in body mass index with age were seen among orphans (ologit test for difference: adjusted odds ratio = 0.68; p = 0.07) and maternal orphans (ologit test for difference: adjusted odds ratio = 0.67; p = 0.03) than among non-orphans. Stigma and discrimination contributed to poor diet, malnutrition and ill-health in children whose mothers had died, while heightened poverty was a more important factor for paternal orphans. These results suggest social and psychological support for orphans and their families could be as important as material support in preventing malnutrition and ill-health.
Keywords: orphans and vulnerable children, Zimbabwe, HIV/AIDS, health, nutrition
Introduction
Orphans and vulnerable children (OVC) can be at greater risk of poor health (Andrews, Skinner, & Zuma, 2006; Bledsoe, Ewbank, & Isiugo-Abanihe, 1988; Oni, 1995; Sarker, Neckermann, & Muller, 2005; Watts et al., 2007) and malnutrition (Lindblade, Odhiambo, Rosen, & DeCock, 2003; Miller, Gruskin, Subramanian, & Heymann, 2007; Watts et al., 2007) compared to non-orphans. Donors are therefore investing large sums of money in programmes to support orphans. However, little is known about how poor health and malnutrition develop as children age or about the causal pathways that lead from orphanhood to poorer outcomes (Watts et al., 2007). It is essential to understand why, how and when orphans are more disadvantaged compared to non-orphans so that effective evidence-based programmes can be developed.
We used aggregated data from Demographic and Health Surveys (DHS) in 22 countries in sub-Saharan Africa first, to describe differentials in ill-health and malnutrition by orphan status. We then used data from a closed cohort study of children, stratified by their initial orphan status, in Zimbabwe to describe how ill-health and malnutrition accumulate over the child’s life-course and to investigate the causal pathways between orphanhood and ill-health and malnutrition using a published theoretical framework.
Methods
Data
DHS data on acute respiratory infection (ARI) and diarrhoea in the last two weeks were obtained for children aged zero to four years at last birthday and data on stunting and underweight were obtained for children aged 0 to 14 years for 22 sub-Saharan African countries. Surveys were selected with the criterion that they had been carried out in the last 10 years (1997–2006).
Manicaland Study (Gregson & Chandiwana, 2001) records were used as the sampling frame for the Manicaland Child Cohort Survey (MCCS). A sample of children stratified by initial orphan status was selected for the MCCS from sites 5 to 12 of the Manicaland Study, using a combination of: (1) listings of newly orphaned children made in verbal autopsy interviews for adults who died between the first round (1999–2000) and the second round (2002–2003) of the Manicaland Study; and (2) listings of children by current parental survival status made in the household census conducted for the second round of the Manicaland Study. Initially, all surviving newly orphaned children identified in the verbal autopsy interviews were selected. Then, sampling fractions of children by orphan status enumerated in the household census were calculated to provide roughly equal samples of paternal, maternal and double orphans and non-orphans. Based on the numbers of children in each orphan status category identified in the verbal autopsies and household census listings, it was estimated that 1 in 50 non-orphans, one in five paternal orphans and all maternal and double orphans would need to be selected for the study in addition to those identified in the verbal autopsy interviews. Using these sampling fractions, children in each orphan category were selected at random from the household census listings.
A total sample of 1430 children aged 0 to 17 years at last birthday (348 paternal orphans, 370 maternal orphans, 434 double orphans and 278 non-orphans) was identified in this way. One year later, in each site (December 2002–March 2004), the first round of the MCCS was conducted and 1003 children (70% of the original sample) were interviewed, comprising 257 paternal orphans, 245 maternal orphans, 279 double orphans and 222 non-orphans. Two further rounds of follow-up were completed between June 2003 and November 2004 (n = 866, 86% of those seen at round 1); and from July 2004 to March 2006 (n = 779, 90% of those seen at round 2).
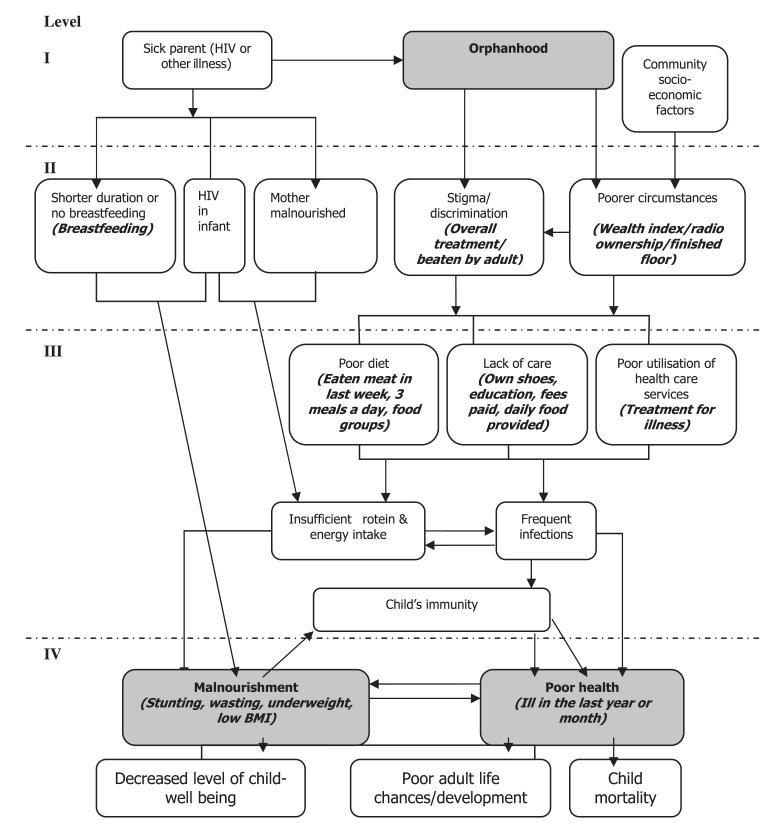
In each round of the MCCS, data were collected on malnutrition and health outcomes and factors hypothesized to lie on the causal pathway between parental illness and death and poorer nutrition and ill-health (Figure 1). The data were collected by social work graduates using structured questionnaires. For children under seven years of age, data were collected with assistance from the primary caregiver. For children aged seven years and above, the child was interviewed alone. To provide data on malnutrition, weight and height measurements were also collected for children of all ages at each survey round. Children were assured that information they provided on their treatment would not be given to their caregivers unless they gave explicit permission.
Figure 1.
Theoretical framework. This framework was developed from the literature to analyse the determinants of child malnutrition and ill-health in orphaned children (Watts et al., 2007). Summary outcome variables for the risk factors are shown in the brackets – variables were created from the Manicaland Child Cohort Study (MCCS) data. BMI, body mass index; HIV, human immunodeficiency virus.
In the third round of the MCCS, faecal samples were collected from 254 children and examined microscopically for parasites. A 5% formalin solution was added to the stool samples to preserve any parasites that might have been present. Free treatment was offered to any children who were found to be infected with a parasite.
The MCCS was approved by the St Mary’s Research Ethics Committee (reference number 04/Q0403/130), the Biomedical Research and Training Institute (reference number AP65/05) and the Medical Research Council of Zimbabwe (reference number MRCZ/A/990).
Data analysis
Malnutrition and ill-health outcomes
The DHS data were used to calculate aggregate prevalence rates by orphan status for ARI and diarrhoea among zero to four-year-olds and for stunting (height-for-age) and under-weight (weight-for-age) among zero to four-year-olds and 5 to 14-year-olds in the 22 sub-Saharan African countries. The MCCS data from Zimbabwe were used to calculate four forms of malnutrition: stunting, wasting (weight-for-height), underweight and body mass index (BMI). In both these analyses, the prevalence of each form of malnutrition was calculated as the percentage of children in the cohort with anthropomorphic measures of less than –2 Z-scores.
For children aged under seven years, the following health outcome indicators were calculated from the MCCS data: (1) all vaccinations up to date (bacillus Calmette–Guérin, polio, diphtheria, measles); (2) vaccinations up to date and verified using the child’s vaccination card; (3) child ill with fever or diarrhoea in last two weeks; (4) child’s health status in past few months – good health, recurring sickness or serious illness; (5) illness in the last year; and (6) for children who had been ill in the last year, receipt of appropriate treatment (i.e. hospital or clinic versus traditional healer or no treatment). For children aged seven years and above, the last three indicators only were calculated. The supplementary data collected in the third round of the MCCS were used to calculate the prevalence of intestinal parasites.
Logistic regression was used to calculate age- and sex-adjusted odds ratios (ORs) for differences in these health and nutrition indicators between orphaned and non-orphaned children.
Trends with increasing age
Ordinal logistic regression was applied to longitudinal data from the three rounds of the MCCS to test whether orphans (by orphan type) were more likely than other children to experience improved or worsened health or nutritional status as they got older. Children who lost a parent between rounds were excluded from this analysis.
Causal pathways between orphanhood and ill-health and malnutrition
A previously published theoretical framework (Figure 1) was used to frame the analysis of determinants of ill-health and malnutrition (Owen, 2007; Watts et al., 2007). The frame-work has four levels and outcome variables were developed for the factors at each level using appropriate data (where available) from children aged 7 to 17 years interviewed in the MCCS (Owen, 2007). The summarized outcome variables are shown in brackets under the corresponding factors in Figure 1. Hypotheses relating to the causal pathways posited between successive levels in the framework were derived and tested a priori.
Results
Ill-health and malnutrition in orphans versus non-orphans
Table 1 shows the age- and sex-adjusted ORs for ill-health and malnutrition among orphans compared to non-orphans in the 22 sub-Saharan African countries combined. Overall, young orphans were more likely to suffer from ARI and than non-orphans and older orphans were more likely to be underweight. However, these differences were not large and no differences were found in the prevalence of diarrhoea or the malnutrition indicators for under-fives or stunting for 5 to 14-year-olds. The results, disaggregated by form of orphan experience, indicate heightened levels of diarrhoea, stunting and (for 5 to 14-year-olds) underweight among maternal and double orphans and ARI and (for 5 to 14-year-olds) underweight among paternal orphans.
Table 1.
Recent ill-health in zero to four-year-olds and malnutrition in zero to four- and 5 to 14-year-olds in sub-Saharan Africa, by orphan type.
| All countries | Comparison group non- orphans |
Orphans |
Maternal orphans |
Paternal orphans |
Double orphans |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | AOR* | p-value | n | % | AOR* | p-value | n | % | AOR* | p-value | n | % | AOR* | p-value | |
| 0–4 year olds | ||||||||||||||||||
| ARI–last 2 weeks | ||||||||||||||||||
| No | 105607 | 87 | 3421 | 86 | 1 | 396 | 86 | 1 | 3114 | 86 | 1 | 93 | 85 | 1 | ||||
| Yes | 15102 | 13 | 565 | 14 | 1.19 | <0.01 | 62 | 14 | 1.15 | 0.30 | 506 | 14 | 1.18 | <0.01 | 17 | 15 | 1.36 | 0.24 |
| Diarrhoea–last 2 weeks | ||||||||||||||||||
| No | 102718 | 84 | 3413 | 85 | 1 | 383 | 82 | 1 | 3108 | 85 | 1 | 87 | 77 | 1 | ||||
| Yes | 19364 | 16 | 617 | 15 | 1.01 | 0.69 | 86 | 18 | 1.31 | 0.02 | 540 | 15 | 0.97 | 0.56 | 26 | 23 | 1.78 | 0.01 |
| 0–4 year olds | ||||||||||||||||||
| Stunting | ||||||||||||||||||
| No | 61965 | 82 | 1960 | 83 | 214 | 77 | 1 | 1791 | 84 | 1 | 45 | 78 | 1 | |||||
| Yes | 13245 | 18 | 401 | 17 | 1.02 | 0.72 | 63 | 23 | 1.50 | 0.01 | 351 | 16 | 0.96 | 0.53 | 13 | 22 | 1.50 | 0.20 |
| Underweight | ||||||||||||||||||
| No | 65872 | 83 | 2057 | 83 | 1 | 238 | 82 | 1 | 1870 | 83 | 1 | 51 | 88 | 1 | ||||
| Yes | 13576 | 17 | 428 | 17 | 1.07 | 0.19 | 54 | 18 | 1.21 | 0.21 | 381 | 17 | 1.05 | 0.43 | 7 | 12 | 0.75 | 0.47 |
| 5–14 year olds | ||||||||||||||||||
| Stunting | ||||||||||||||||||
| No | 70349 | 82 | 8090 | 82 | 1 | 2743 | 81 | 1 | 6325 | 82 | 1 | 978 | 80 | 1 | ||||
| Yes | 15331 | 18 | 1765 | 18 | 0.98 | 0.54 | 663 | 19 | 1.09 | 0.06 | 1347 | 18 | 0.96 | 0.16 | 245 | 20 | 1.12 | 0.13 |
| Underweight | ||||||||||||||||||
| No | 75990 | 84 | 8576 | 82 | 1 | 2925 | 81 | 1 | 6613 | 82 | 1 | 962 | 76 | 1 | ||||
| Yes | 14974 | 16 | 1886 | 18 | 1.10 | <0.01 | 685 | 19 | 1.16 | <0.01 | 1498 | 18 | 1.13 | <0.01 | 297 | 24 | 1.52 | <0.01 |
Notes: Demographic and Health Surveys (DHS) surveys included in Table I: Mali (2001), Gabon (2000), Benin (2001), Ghana (2003), Madagascar (2003/2004), Nigeria (2003), Burkina Faso (2003), Senegal (2005), Guinea (1999), Tanzania (2004), Togo (1996), Cameroon (2004), Ethiopia (2005), Namibia (2000), Mozambique (2003), South Africa (1996), Kenya (2003), Uganda (2000/2001), Zimbabwe (1999), Zambia (2001/2002), Lesotho (2004), Rwanda (2000).
AOR; adjusted odds ratio; controlled for the child’s age and sex.
Table 2 shows the correlations between orphanhood and ill-health and malnutrition in round one of the MCCS. The results from subsequent rounds were similar (not shown). In round 1, orphans overall were more likely than non-orphans to report recurring minor illnesses in the last few months (26% vs. 23%; p = 0.24). More paternal orphans reported recurring minor illnesses than non-orphans (31% vs. 23%; AOR = 1.58; p = 0.03). In all three rounds, double orphans were (non-significantly) less likely to receive appropriate treatment for illnesses than non-orphans.
Table 2.
Correlation between orphanhood and ill-health and malnutrition for round one of the Manicaland Child Cohort Study (MCCS). This table shows the correlation between orphanhood and ill-health and malnutrition in round one of the MCCS. Logistic regression analysis was used to establish whether orphaned children were more or less likely to experience detrimental health outcomes.
| Comparison group non-orphans |
All orphans |
||||||
|---|---|---|---|---|---|---|---|
| Age-group | N | % | N | % | AOR* | p-value | |
| Round 1 | |||||||
| All vaccinations received | |||||||
| Yes | 0–6 | 56 | 95 | 56 | 92 | 1 | |
| No | 3 | 5 | 5 | 8 | 1.19 | 0.83 | |
| All vaccinations + health card seen | |||||||
| All vaccinations + health card seen | 0–6 | 34 | 69 | 25 | 52 | 1 | |
| All vaccinations + health card not seen | 15 | 31 | 23 | 48 | 2.00 | 0.12 | |
| Child ill in last 2 weeks | |||||||
| No illness | 0–6 | 49 | 83 | 54 | 81 | 1 | |
| Yes – fever or diarrhoea | 10 | 17 | 13 | 19 | 1.62 | 0.35 | |
|
Good health or ill in the last
few months? |
|||||||
| Good health | 0–17 | 155 | 70 | 531 | 68 | 1 | |
| Recurring minor illness | 50 | 23 | 203 | 26 | 1.24 | 0.24 | |
| Serious illness | 15 | 7 | 47 | 6 | 0.93 | 0.82 | |
| How long since last experienced illness? | |||||||
| More than a year | 0–17 | 73 | 50 | 379 | 51 | 1 | |
| Less than a year | 72 | 50 | 369 | 49 | 0.90 | 0.56 | |
|
Treatment seeking – if ill in
last 12 months |
|||||||
| Appropriate treatment (hospital, clinic, VCW) |
0–17 | 84 | 74 | 261 | 71 | 1 | |
| No treatment or inappropriate treatment | 29 | 26 | 109 | 29 | 1.20 | 0.47 | |
| Stunting ** | |||||||
| No | 5.17 | 553 | 75 | 164 | 71 | 1 | 1 |
| Yes | 186 | 25 | 68 | 29 | 1.15 | 0.42 | |
| Wasting | |||||||
| No | 0–17 | 197 | 89 | 784 | 97 | 1 | 1 |
| Yes | 25 | 11 | 28 | 3 | 0.58 | 0.08 | |
| Underweight | |||||||
| No | 0–17 | 161 | 73 | 607 | 75 | 1 | 1 |
| Yes | 61 | 27 | 202 | 25 | 0.95 | 0.77 | |
| Low BMI (<2 Z-scores) | |||||||
| No | 2–17 | 159 | 76 | 672 | 83 | 1 | 1 |
| Yes | 51 | 24 | 137 | 17 | 0.78 | 0.19 | |
Adjusted odds ratio (AOR) controlled for the child’s age and sex;
orphans in the stunting comparison are children who lost their parent(s) before the age of five years.
For children under seven years of age, more detailed information was collected from the caregivers regarding recent child illness (diarrhoeal illness and/or a fever in the last two weeks) and vaccination history. Despite the small sample size, paternal orphans were significantly more likely than non-orphans to not have a vaccination health card (65% vs. 48%; AOR = 4.03; p = 0.02) at round 1. Orphans, and particularly paternal orphans, had a higher prevalence of illness than non-orphans in rounds 1 and 2 (p > 0.05).
No statistically significant associations were found between orphanhood and malnutrition. The analyses described above were repeated separately for males and for females, but no differences in results were found (data not shown).
Helminth parasite infections were uncommon, with six children having hookworm infection, two having Schistosoma mansoni and two excreting Ascaris eggs. Protozoan infections were significantly more common in orphaned children (55%; 97 of 176) than in non-orphans (40%; 31 of 78) (Table 3).
Table 3.
Protozoan infections in orphan and non-orphan children. Infections with protozoa for the 254 children who had stool samples analysed.
|
Cryptosporidium
|
Giardia
|
Entamoeba sp. |
|||||
|---|---|---|---|---|---|---|---|
| N | n | % | n | % | n | % | |
|
Comparison group
non-orphan |
78 | 9 | 12 | 4 | 5 | 25 | 32 |
| Maternal orphan | 58 | 9 | 16 | 4 | 7 | 21 | 36 |
| Paternal orphan | 53 | 12 | 23 | 5 | 9 | 22 | 42 |
| Double orphan | 65 | 15 | 23 | 7 | 11 | 31 | 48 |
| All orphan | 176 | 36 | 20 | 16 | 9 | 74 | 42 |
Trends in ill-health and malnutrition with increasing age
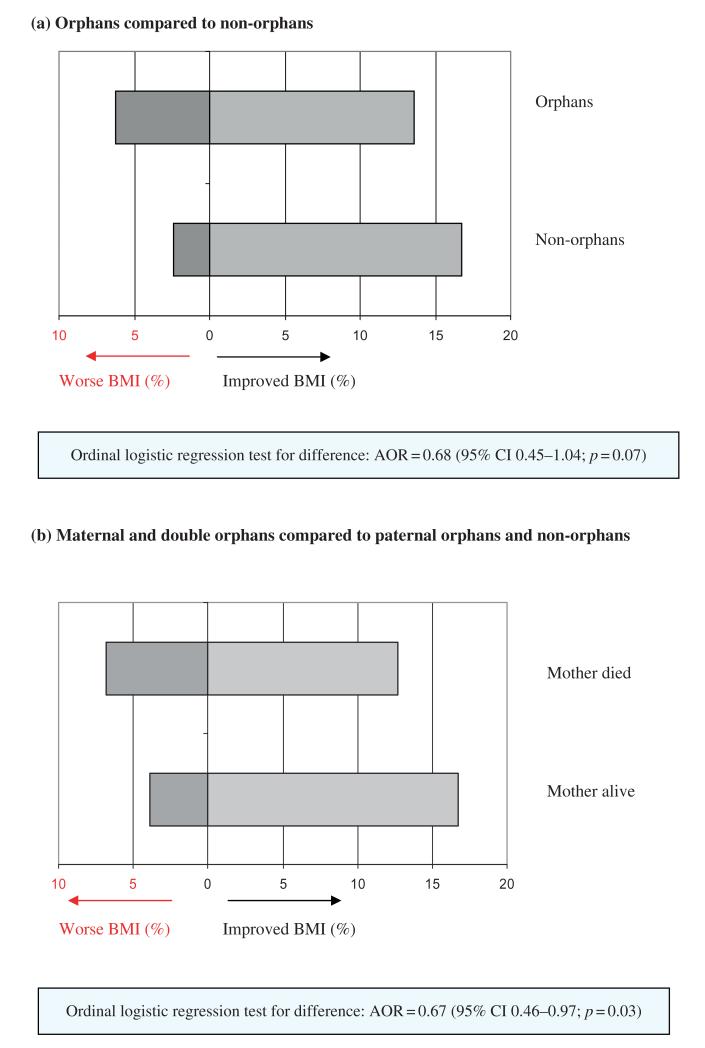
Children’s nutritional status generally improved with increasing age. Orphans overall (ologit test for difference: AOR = 0.68; p = 0.07) and maternal orphans (ologit test for difference: AOR = 0.67; p = 0.03) were significantly less likely than non-orphans to have an improved BMI status as they grew older (Figure 2). No significant differences were found for stunting, wasting, underweight or recurring sickness. However, for stunting, this may be because height deficits normally occur in the first four years of life and, once established, rarely recover to average levels (Branca & Ferrari, 2002).
Figure 2.
Change in body mass index (BMI) status between rounds 1 and 3 of the Manicaland Child Cohort Survey. Ordinal logistic regression was used to test whether orphans (by orphan type) were more likely to have an improved or worse health and nutritional status over time. AOR, adjusted odds ratio; CI, confidence interval; BMI, body mass index.
Causal pathways from orphanhood to greater ill-health and malnutrition
The variables measured from the MCCS data to represent factors hypothesized in the theoretical framework to lie on the causal pathways between orphanhood and poor health and malnutrition are shown in brackets under the respective factors in Figure 1. The numbered square boxes indicate the specific hypotheses that could be tested using these variables.
Associations between parental loss, and stigma and discrimination and poverty
Relatively few children (5%), in the 7 to 17-year age group reported being treated worse than other children. However, orphans (5% vs. 3%, AOR = 2.25; p = 0.13) aged 7 to 17 years were more likely than non-orphans to think they were treated worse than other children of the same age and sex who live in the same household (hypothesis 1a). Maternal orphans (7% vs. 3%, AOR = 2.56; p = 0.01) were significantly more likely than other children to think they are treated worse. No associations were found between orphanhood and being beaten by an adult in the last month.
Overall, orphaned children were not more likely live in poorer households (Lewis, 2000; Lopman et al., 2007) than non-orphans (hypothesis 1b). However, paternal orphans’ households were more likely to not own a radio (73% vs. 66%, AOR = 1.42; p = 0.04) compared to households where the father was alive. No associations were found between orphanhood and floor type or wealth index score.
Associations between stigma and discrimination and poverty, and diet, care and access to health services
Children who perceived themselves to be treated worse than other children of the same age and sex in the same household were more likely not to own a pair of shoes (74% vs. 42% in those experiencing better overall care, AOR = 4.21; p < 0.01); not to have had a new pair of shoes in the last 12 months (68% vs. 47%, AOR = 2.37; p = 0.02), and not to have had their school fees paid (23% vs. 7%, AOR = 3.48; p = 0.01) (hypothesis 2a). However, there was no association between being beaten in the last month and receiving poorer care, due perhaps to the small numbers of children who reported being beaten (n = 40).
Children living in households without a radio were more likely to eat less than three meals per day than children living in households with radios (19% vs. 14%, AOR = 1.46; p = 0.05) (hypothesis 2b). Those living in households with a natural floor were more likely not to be enrolled in school than children living in households with a finished floor (16% vs. 9%, AOR = 2.00; p = 0.01). No associations were found between residence in poorer households (i.e. children living in households with no radio or natural floor or in the poorest quintile of the wealth index) and any of the other outcome variables for children experiencing poorer care.
The median number of months that a child was breastfed was lower for children whose mother died when they were under two years [12 months; 95% confidence interval (CI) 5–16 months] than for children whose mothers were still alive at their second birthday (18 months; 95% CI 18–19 months; Spearman’s rank test Z = 3.6; p < 0.01) (hypothesis 2c).
Associations between diet, care and access to health services, and health and nutrition outcomes
Children aged zero to four years were more likely to be stunted if they had not eaten grains in the day before the interview (63% vs. 28%, AOR = 4.04; p = 0.08) (hypothesis 3a). Young children were more likely to be stunted (80% vs. 28%, AOR = 9.11; p = 0.06) and underweight (60% vs. 18%, AOR = 7.43; p = 0.05) if they had eaten less than three meals the previous day. Children were less likely to be wasted if they had not eaten protein (i.e. meat, poultry, fish, eggs, groundnuts or beans) in the last seven days. However, very few young children eat a great deal of protein. Children aged 5 to 17 years were more likely to be stunted if they have not eaten any protein the previous day (27% vs. 20%, AOR = 1.58; p = 0.08) or in the last seven days (30% vs. 25%, AOR = 1.32; p = 0.06), or if they had had less than three meals the day before the interview (28% vs. 26%, AOR = 1.38; p = 0.09). Children were more likely to have a low BMI if they did not eat any vegetables the day before the interview (20% vs. 15%, AOR = 1.45; p = 0.06).
Children aged 7 to 17 years who experienced a lack of care (i.e. who did not own a pair of shoes) were significantly more likely to have suffered from an illness in the last year (53% vs. 43%, AOR = 1.38; p = 0.02) and from ill-health in the last few months (37% vs. 28%, AOR = 1.43; p = 0.02) (hypothesis 3b). Similarly, children who had not been bought shoes in the last 12 months were more likely to have been ill in the last year (52% vs. 44%, AOR = 1.36; p = 0.02).
No significant differences were found between duration of breastfeeding and subsequent malnutrition; however, there were few children in the relevant age group (two to six years) (hypothesis 3c).
Discussion
Previous studies in sub-Saharan Africa have found disadvantages in the health and nutritional status of orphans compared to non-orphans (Andrews et al., 2006; Bledsoe et al., 1988; Lindblade et al., 2003; Oni, 1995; Sarker et al., 2005; Watts et al., 2007). The DHS analysis of 22 countries presented here supports these findings, although the overall levels of disadvantage observed are relatively modest. The MCCS results also show higher levels of ill-health in orphaned children in line with findings from the national Zimbabwe OVC Baseline Survey (Watts et al., 2007). Few of these differences were large enough to reach statistical significance given the sample sizes available, and no adverse effects of orphanhood on nutritional status were observed. However, the longitudinal MCCS data provided evidence that orphanhood and maternal loss, in particular, can slow recovery from the effects of early malnutrition.
These limited effects of orphanhood on children’s health and nutrition could reflect successful OVC support programmes. In the first round of the MCCS, 21% of households with orphans, compared to 5% of households with no orphans, had received external assistance during the last six months. However, health and nutrition outcomes did not differ between orphans in households receiving and not receiving assistance. Elsewhere, the extended family system has mitigated the impact of orphanhood on children (Floyd et al., 2007; Foster et al., 1995) and this could also be the case in Manicaland (Nyamukapa & Gregson, 2005). A further factor in the MCCS results could be that orphans who had lost their parent(s) recently were purposefully over-sampled. For these children, there may have been insufficient time for detrimental outcomes to develop.
Low prevalence of intestinal helminth infections has also been found in earlier studies in Zimbabwe (Mason, Patterson, & Loewenson, 1986). Nevertheless, the data suggest a more detailed examination of intestinal infection and diarrhoea is warranted, particularly as relatively simple hygiene intervention measures can have a significant impact on child health (Luby et al., 2005).
The MCCS data are limited by the relatively small sample size, their uncertain wider representativeness, and in that the human immunodeficiency virus (HIV) status of participating children was not determined. Differences in HIV prevalence could contribute to differences in health and nutrition outcomes by orphan status and, unless controlled for adequately, obscure the effects of other factors. However, existing studies suggest that such differences may not be large (Brookes, Shisana, & Richter, 2004; Gomo, 2006). A slight deterioration in the accuracy of some of the bathroom scales used to weigh the children may have affected the data on wasting, underweight and BMI (Owen, 2007).
Recent findings of continued increases in orphan incidence, as well as prevalence, placing additional strain on extended families (Watts, Lopman, Nyamukapa, & Gregson, 2005), continuing nutritional and health disadvantages suffered by OVC (Watts et al., 2007) and, apparently, the limited effectiveness of existing programmes emphasize the need to strengthen and extend the coverage of support programmes.
In the national Zimbabwe OVC Baseline Survey and the DHS data presented in this paper, children whose mothers had died tended to be the worst affected by malnutrition, and possibly ill-health. In an analysis of the Zimbabwe national survey data, this pattern was not accounted for by greater exposure to extreme poverty (Watts et al., 2007). The results from the analysis of MCCS data on causal pathways presented here could explain this: maternal orphans experienced greater stigma and discrimination which resulted in poorer care and, ultimately, in poorer health and nutrition. In contrast, we found evidence that paternal orphans do tend to live in poorer households, which is associated with poorer diet and, in turn, with greater malnutrition. This level of detail is important from a policy perspective, because it highlights areas that interventions should target. In particular, our results suggest that social, emotional and psychological forms of support for orphans and their families are as important as material support.
References
- Andrews G, Skinner D, Zuma K. Epidemiology of health and vulnerability among children orphaned and made vulnerable by HIV/AIDS in sub-Saharan Africa. AIDS Care. 2006;18:269–276. doi: 10.1080/09540120500471861. [DOI] [PubMed] [Google Scholar]
- Bledsoe CH, Ewbank DC, Isiugo-Abanihe UC. The effect of child fostering on feeding practices and access to health services in rural Sierra Leone. Social Science and Medicine. 1988;27:627–636. doi: 10.1016/0277-9536(88)90011-1. [DOI] [PubMed] [Google Scholar]
- Branca F, Ferrari M. Impact of micronutrient deficiencies on growth: The stunting syndrome. Annals of Nutrition and Metabolism. 2002;46(Suppl. 1):8–17. doi: 10.1159/000066397. [DOI] [PubMed] [Google Scholar]
- Brookes H, Shisana O, Richter L. The national household HIV prevalence and risk survey of South African children. Human Sciences Research Council; Cape Town: 2004. [Google Scholar]
- Floyd S, Crampin AC, Glynn JR, Madise N, Mwenebabu M, Mnkhondia S, et al. The social and economic impact of parental HIV on children in northern Malawi: Retrospective population-based cohort study. AIDS Care. 2007;19:781–790. doi: 10.1080/09540120601163227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster G, Shakespeare R, Chinemana F, Jackson H, Gregson S, Marange C, et al. Orphan prevalence and extended family care in a peri-urban community in Zimbabwe. AIDS Care. 1995;7:3–17. doi: 10.1080/09540129550126911. [DOI] [PubMed] [Google Scholar]
- Gomo EEA. Household survey of HIV-prevalence and behaviour in Chimanimani District, Zimbabwe, 2005. A baseline study (182pp.) BRTI, NIHR & Ministry of Health; Zimbabwe: 2006. [Google Scholar]
- Gregson S, Chandiwana SK. The Manicaland HIV/STD prevention project: Studies on HIV transmission, impact and control in rural Zimbabwe. Zimbabwe Science News. 2001;35:27–42. [Google Scholar]
- Lewis JJC. Orphanhood prevalence in rural Zimbabwe (279pp.) University of Oxford, Department of Statistics; Oxford: 2000. [Google Scholar]
- Lindblade KA, Odhiambo F, Rosen DH, DeCock KM. Health and nutritional status of orphans <6 years old cared for by relatives in western Kenya. Tropical Medicine and International Health. 2003;8:67–72. doi: 10.1046/j.1365-3156.2003.00987.x. [DOI] [PubMed] [Google Scholar]
- Lopman B, Lewis JJC, Nyamukapa CA, Mushati P, Chandiwana SK, Gregson S. HIV incidence and poverty in Manicaland, Zimbabwe: Is HIV becoming a disease of the poor? AIDS. 2007;21(Suppl. 7):S57–S66. doi: 10.1097/01.aids.0000300536.82354.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, et al. Effect of handwashing on child health: A randomised controlled trial. Lancet. 2005;366:225–233. doi: 10.1016/S0140-6736(05)66912-7. [DOI] [PubMed] [Google Scholar]
- Mason PR, Patterson BA, Loewenson R. Piped water supply and intestinal parasitism in Zimbabwean schoolchildren. Transactions of the Royal Society of Tropical Medicine and Hygeine. 1986;80:88–93. doi: 10.1016/0035-9203(86)90204-x. [DOI] [PubMed] [Google Scholar]
- Miller CM, Gruskin S, Subramanian SV, Heymann J. Emerging health disparities in Botswana: Examining the situation of orphans during the AIDS epidemic. Social Science and Medicine. 2007;64(12):2476–2486. doi: 10.1016/j.socscimed.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Nyamukapa CA, Gregson S. Extended family’s and women’s roles in safeguarding orphans’ education in AIDS-afflicted rural Zimbabwe. Social Science and Medicine. 2005;60:2155–2167. doi: 10.1016/j.socscimed.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Oni JB. Fostered children’s perception of their health care and illness treatment in Ekiti Yoruba households, Nigeria. Health Transition Review. 1995;5:21–34. [Google Scholar]
- Owen H. PhD thesis. Imperial College, London: 2007. The effect of orphanhood on the health and nutritional status of children in Zimbabwe. [Google Scholar]
- Sarker M, Neckermann C, Muller O. Assessing the health status of young AIDS and other orphans in Kampala, Uganda. Tropical Medicine and International Health. 2005;10:210–215. doi: 10.1111/j.1365-3156.2004.01377.x. [DOI] [PubMed] [Google Scholar]
- Watts H, Gregson S, Saito S, Lopman B, Beasley M, Monasch R. Poorer health and nutritional outcomes for orphans and vulnerable young children not explained by greater exposure to extreme poverty in Zimbabwe. Tropical Medicine and International Health. 2007;12:584–593. doi: 10.1111/j.1365-3156.2007.01832.x. [DOI] [PubMed] [Google Scholar]
- Watts H, Lopman B, Nyamukapa C, Gregson S. Rising incidence and prevalence of orphanhood in Manicaland, Zimbabwe, 1998 to 2003. Aids. 2005;19:717–725. doi: 10.1097/01.aids.0000166095.62187.df. [DOI] [PubMed] [Google Scholar]