Abstract
Objective
Because evidence-based psychotherapies of 12 to 20 sessions can be perceived as too lengthy and time intensive for the treatment of depression in primary care, a number of studies have examined abbreviated psychotherapy protocols. The purpose of this study was to conduct a systematic review and meta-analysis to determine the efficacy of brief psychotherapy (i.e., ≤ 8 sessions) for depression.
Methods
We used combined literature searches in PubMed, EMBASE, PsycINFO, and an Internet-accessible database of clinical trials of psychotherapy to conduct two systematic searches: one for existing systematic reviews and another for randomized controlled trials (RCTs). Included studies examined evidence-based psychotherapy(s) of 8 or fewer sessions, focused on adults with depression, contained an acceptable control condition, were published in English, and used validated measures of depressive symptoms.
Results
We retained 2 systematic reviews and 15 RCTs evaluating cognitive behavioral therapy, problem-solving therapy, and mindfulness-based cognitive therapy. The systematic reviews found brief psychotherapies to be more efficacious than control, with effect sizes ranging from −0.33 to −0.25. Our meta-analysis found six to eight sessions of cognitive behavioral therapy to be more efficacious than control (ES −0.42, 95% CI −0.74 to −0.10, I2=56%). A sensitivity analysis controlled for statistical heterogeneity but showed smaller treatment effects (ES −0.24, 95% CI −0.42 to −0.06, I2=0%).
Conclusions
Depression can be efficaciously treated with six to eight sessions of psychotherapy, particularly cognitive behavioral therapy and problem-solving therapy. Access to non-pharmacologic treatments for depression could be improved by training health care providers to deliver brief psychotherapies.
Index Words: depression, psychotherapy, primary health care, meta-analysis, review, systematic, psychotherapy, brief
INTRODUCTION
Depressive disorders present a major public health concern. The prevalence of current depression among U.S. adults is 6.6% [1], with a lifetime prevalence rate of 16 to 18% [2]. Particularly high rates have been found in primary care settings [3] where a high proportion of patients with depressive disorders are treated [4]. Medication is by far the most commonly utilized intervention in primary care settings [5, 6], despite extensive evidence and clinical guidelines suggesting that efficacious treatments for depression include both pharmacotherapy and psychotherapy [7].
In recent years, there has been a growing interest in and commitment to the integration of psychotherapy and other mental health services into primary care settings [8]. Providing primary care patients with the option of receiving psychotherapy for depression is an important objective for multiple reasons: there are many patients who prefer psychotherapy to medication [9]; there is a need to provide alternative treatments for patients who do not improve on or cannot tolerate antidepressant medication [10]; and there may be unique benefits from psychotherapy in terms of costs and relapse prevention [11].
Perhaps the most significant barrier to providing psychotherapies in primary care settings is that many empirically supported psychotherapy treatment protocols consist of at least 12 to 20 weekly 1-hour sessions [12, 13]. While this treatment duration is much abbreviated compared with older approaches to the provision of psychotherapy [14], it is arguably still too intensive for reliable implementation in primary care settings [15].
Recognizing that time and resource constraints present important barriers to effectively implementing standard-duration psychotherapies (i.e., 12 to 20 sessions) for depression in primary care settings, this review evaluates whether psychotherapy for depression can be efficacious after a period of 8 or fewer sessions. Eight sessions is roughly half the length of standard-duration psychotherapies, and this treatment duration has been used in previous research examining standard-duration vs. brief psychotherapy [16]. The present review aimed to evaluate the evidence on brief psychotherapy for depression by employing a complex systematic review methodology [17], with particular attention devoted to the training received by providers delivering brief psychotherapies and the reporting of clinical outcomes beyond depression severity.
METHODS
We utilized a combined approach for conducting a complex systematic review [17], identifying and evaluating existing systematic reviews and supplementing these reviews by searching for and evaluating original research not included in these reviews.
SEARCH STRATEGY
We developed search strategies in consultation with a master librarian and conducted searches in three stages. First, we searched MEDLINE (via PubMed), Embase, and PsycINFO for relevant, good-quality, English-language systematic reviews that were published within the past 10 years (January 1, 2000 – May 2010). Second, we used a well-documented Internet-accessible database of psychotherapy trials that was current through January 2010 [18]. We used this database of 243 trials as a data source for original research, searching for studies coded as including adults with a mood disorder who received face-to-face psychotherapy at a dose of eight or fewer therapy sessions. Finally, we searched for publications in MEDLINE (via PubMed), PsycINFO, and Embase from January 2009 (one year prior to the search date of the online database) through August 1, 2010 to complement the Internet-accessible database of psychotherapy trials. We supplemented electronic searching by examining the bibliographies of included studies and review articles. The full search strategies are available upon request from the authors.
STUDY SELECTION
Using prespecified inclusion/exclusion criteria, pairs of trained researchers (either PhD or MD) reviewed the list of titles and abstracts, then selected articles identified from any of the computerized and manual searches described above for further review of the full text. Each article retrieved was reviewed using a brief screening form. To be included in our study, systematic reviews had to be rated as good-quality using quality criteria adapted from a previous review [19], and original research studies had to be an RCT, compare an eligible psychotherapy of eight or fewer sessions to control, and report effects on depressive symptoms. Detailed eligibility criteria are described in Table 1.
Table 1.
Summary of Inclusion and Exclusion Criteria
| Study characteristic | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Study design | Randomized controlled trial | None |
| Population | Adults with major depressive disorder (MDD), dysthymic disorder, or subthreshold (minor) depression in acute-phase treatment | Treatment-resistant depression, postpartum depression, premenstrual dysphoric disorder, bipolar disorder, seasonal affective disorder, or double depression (i.e., MDD and dysthymia) |
| Interventionsa | Cognitive behavioral therapy (CBT) (including cognitive therapy and behavior therapy), interpersonal therapy (IPT), problem-solving therapy (PST), mindfulness-based cognitive therapy (MBCT), cognitive behavioral analysis system of psychotherapy (CBASP), dialectical behavioral therapy (DBT), functional analytic psychotherapy (FAP), acceptance and commitment therapy (ACT), or short-term psychodynamic therapy with ≤ 8 planned sessions | Generic counseling, life review therapy, psychoeducational therapy, supportive therapy, bibliotherapy, or Internet-based psychotherapies |
| Comparators | Waitlist, attention control, usual care Antidepressant medication if intervention is psychotherapy plus antidepressant |
Another psychotherapy |
| Setting | Outpatient general medical or general mental health clinic | Study conducted outside of North America, Western Europe, New Zealand, or Australia |
| Outcome | Depressive symptoms using a validated instrument reported at ≥ 6 weeks after randomization | None |
Interventions to include and exclude were selected using the Chambless et al.[REFERENCE] update on empirically validated therapies as a guide.
DATA EXTRACTION AND QUALITY ASSESSMENT
For systematic reviews, we assessed the comprehensiveness of the search strategy, the description and appropriateness of inclusion criteria, whether primary studies were assessed for quality and the adequacy of the quality measure, the reproducibility of methods to assess studies, whether the results of relevant studies were combined appropriately, whether heterogeneity and publication bias were assessed, and whether the conclusions were supported by the data presented. Systematic reviews were rated “good” if the conclusions were supported by the data presented and there were no important study limitations.
For newly identified original research studies, trained researchers abstracted data in duplicate from published reports into evidence tables. For eligible trials previously included in the two systematic reviews, we abstracted summary data from the reviews and supplemented these data by using the original publications when the reviews had incomplete information. We assessed risk of bias using the key quality criteria described in the Agency for Healthcare Research and Quality (AHRQ) Methods Guide for Effectiveness and Comparative Effectiveness Reviews [20], adapted for this specific topic. We abstracted data on adequacy of randomization and allocation concealment, comparability of groups at baseline, blinding, completeness of followup and differential loss to followup, whether incomplete data were addressed appropriately, validity of outcome measures, and conflict of interest. Using these data elements, we assigned a summary quality score of “good,” “fair,” or “poor” to individual RCTs.
DATA SYNTHESIS AND ANALYSIS
When good-quality systematic reviews were identified, we summarized the reviews’ findings in narrative form. For original research studies, we critically analyzed their characteristics, methods, and findings, and then used published guidelines to evaluate whether the new evidence was likely to change estimates from prior reviews [20]. If so, we updated prior meta-analyses.
Because studies did not use a single common instrument to measure depression severity, our meta-analysis calculated effect sizes for each study by subtracting (at posttest) the average score of the control group from the average score of the experimental group and dividing the result by the pooled standard deviations (SDs) of the experimental and control groups. We then converted these estimates to the number needed to treat (NNT) using the approach described by Kraemer [21]. When studies used more than one validated instrument to assess depression severity, we used the mean of the effect sizes so that each study (or control group) contributed only one effect size. When means and SDs were not reported, we used other statistics (e.g., event rates) to calculate the effect size. For studies with more than one active eligible psychotherapeutic intervention (e.g., behavioral therapy and cognitive therapy arms) compared to a single control, we combined the intervention arms to avoid lack of independence that would be created if we entered each intervention into the analysis separately [22].
We assessed for heterogeneity in outcomes between studies using the Q statistic and the I2 statistic [23]. Publication bias was tested by inspecting the funnel plot of the meta-analysis. We conducted preplanned subgroup analyses by study quality and type of control group; there was not sufficient variability or numbers of studies to conduct other subgroup analyses. We used an influence analysis, which drops one study at a time and recomputes the treatment effect, to determine the influence of individual studies on the overall effect. We used the computer program Comprehensive Meta-analysis, Version 2.2.021 (www.meta-analysis.com/pages/about_us.html), to conduct all meta-analyses. Finally, we assigned strength of evidence ratings for the different brief psychotherapies using principles from the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) Working Group [24].
RESULTS
SEARCH RESULTS
Systematic Reviews
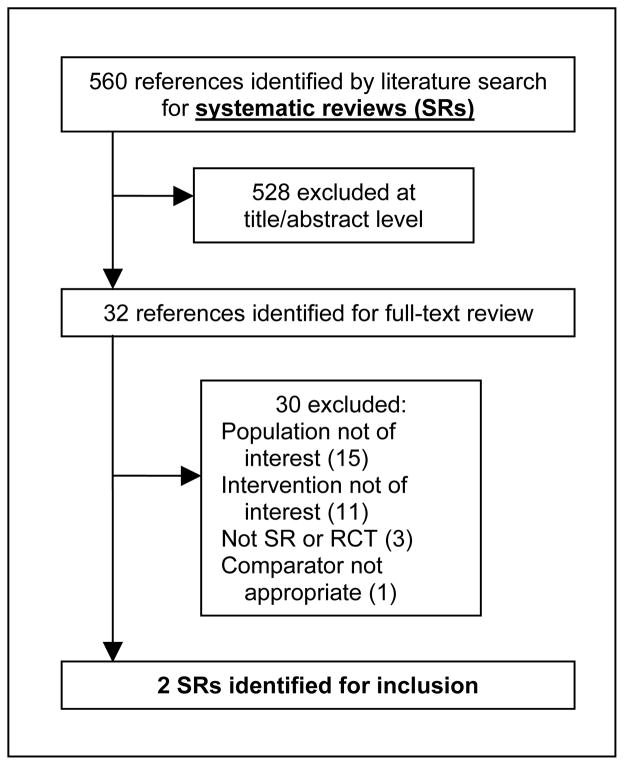
Using the combined literature search of PubMed, Embase, and PsycINFO, we identified references for 560 potential systematic reviews (Figure 1). Two eligible reviews were retained: Cuijpers and colleagues [25] and Cape and colleagues [26]. Neither review focused exclusively on brief psychotherapy for depression. Cuijpers completed a good-quality meta-analysis of 15 studies that examined psychotherapies for depression in primary care; a sub-analysis was completed on the studies of psychotherapies with 6 or fewer sessions (k=7). Cape completed a good-quality meta-analysis and meta-regression of 34 studies examining the effectiveness of psychotherapies for various mental health problems that consisted of fewer than 10 sessions; sub-analyses were completed on the studies of cognitive behavioral therapy (CBT; k=4), problem-solving therapy (PST; k=5), and counseling (k=4) specifically for depression.
Figure 1. Results of literature search for systematic reviews.
Systematic review search: (“depressive symptoms” or “depression [Mesh]” or “depressive disorder [Mesh]” or “depression” or (“minor” and “depression”) or (“subthreshold” and “depression”) or (“subsyndromal” and “depression”) or “major depressive disorder [Mesh]” or “dysthymia” or “dysthymic disorder [Mesh]” or “adjustment disorder [Mesh]”) and (“cognitive behavioral therapy” or “CBT” or “cognitive therapy” or “behavior therapy” or “interpersonal therapy” or “IPT” or “problem-solving therapy” or “PST” or “mindfulness-based cognitive therapy” or “MBCT” or (“cognitive behavioral analysis system” and “therapy”) or “CBASP” or “dialectical behavioral therapy” or “DBT” or “functional analytic psychotherapy” or “FAP” or (“acceptance” and “commitment” and “therapy”) or “ACT” or “short-term psychodynamic therapy” or “psychotherapy, brief [Mesh]”) and (“Cochrane Database Syst Rev [TA]” or “search [Title/Abstract]” or “meta-analysis [Publication type]” or “MEDLINE [Title/Abstract] or (“systematic [Title/Abstract]” and “review [Title/Abstract]”)). Limits: English, adults 19+ years, publication date from 2000.
Primary Literature
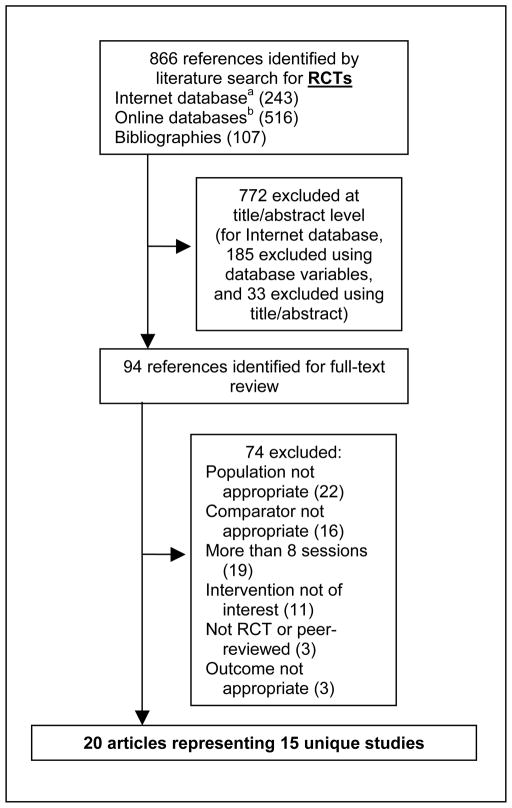
Using the combined searches for primary literature in electronic databases (MEDLINE, Embase, and PsycINFO), in a well-documented Internet-accessible database of psychotherapy trials [18], and in bibliographies of included studies, we identified 866 citations (Figure 2). We retained 20 articles representing 15 unique studies. Only 8 of these 15 studies had been previously reviewed in either the Cuijpers [25] or Cape [26] reviews. Study characteristics from the 15 relevant RCTs of brief psychotherapy are summarized in Table 2. For quality assessments, studies rated as fair or poor were often rated as such due to inadequately addressing incomplete outcome data and not having outcome assessors who were blind to treatment assignment. Characteristics of psychotherapy interventions used in the 15 RCTs of brief psychotherapy are summarized in Table 3. Data were infrequently reported on quality of life, social functioning, occupational status, patient satisfaction, and adverse treatment effects (Table 4).
Figure 2. Results of literature search for RCTs.
RCT search: ((RCTs coded in Cuijpers (2008) internet database (http://www.psychotherapyrcts.org/index.php?id=3) as “Nsessions ≤ 8” and “Targetgruop = 1 or 2 or 3 or 6” and “FormGSH = 0”) or (“Interpersonal therapy” or “problem-solving therapy” or “mindfulness-based cognitive therapy” or “cognitive behavioral analysis system of psychotherapy” or “dialectical behavior therapy” or “functional analytic psychotherapy” or “acceptance and commitment therapy”)) and (“depressive disorder [Mesh]” or (“depressive” and “disorder”) or “depressive disorder” or “depression” or “depression [Mesh]” or “depressive”). Limits: English, human, adults 19+ years, randomized controlled trial, publication date from January 1, 2009 to July 31, 2010.
Table 2.
Summary of Study Characteristics
| Author, year | Depressive disorder | Age mean (SD) | % Female | % White | Setting | Country | Recruitment | Most distal followupa | Depression outcomes | Qualityb |
|---|---|---|---|---|---|---|---|---|---|---|
| Barnhofer et al., 2009 [29] and Hargus et al., 2010 [31] | MDD or subthreshold MDD | 41.9 (10.4) | 68% | NR | MH | UK | Advertisement and referral | 8 weeks | BDI | Good |
| Barrett et al., 2001 [32] and Frank et al., 2002 [3] | Minor depression or dysthymia | 43.6 (NR) | 67% | 89% | PC | US | Screening and referral | 11 weeks | HRSD-17; HSCL-20 | Fair |
| Dowrick et al., 2000 [4] | MDD, dysthymia, adjustment disorder, or other depression | NR; Range: 18–65 | 66% | NR | PC | EU | Screening from census and registry | 52 weeks | BDI | Fair |
| Laidlaw et al., 2008 [33] | MDD | 74.0 (8.0) | 73% | NR | PC | UK | Referral | 26 weeks | BDI; GDS; HRSD | Fair |
| Lynch et al., 1997 [34] | Elevated depressive symptoms without MDD | 48.4 (NR) | 86% | NR | PC | US | Screening | 7 weeks | HRSD; BDI | Poor |
| Lynch et al., 2004 [35] | Elevated depressive symptoms | 38.5 (13.7) | 83% | NR | PC | US | Screening | 6 weeks | HRSD; BDI; DHP | Poor |
| Mynors-Wallis et al., 1995 [36] | MDD | 37.1 (11.4) | 77% | 95% | PC | UK | Referral | 12 weeks | HRSD; BDI | Fair |
| Mynors-Wallis et al., 2000 [37] | MDD | 34.5 (NR) | 78% | 93% | PC | UK | Referral | 52 weeks | HRSD; BDI | Good |
| Nezu, 1986 [38] | MDD | 41.7 (12.8) | 81% | NR | MH | US | Advertisement | 26 weeks | BDI; MMPI-D | Fair |
| Scott et al., 1997 [39] | MDD | 41 (10.4) | 67% | NR | PC | UK | Referral | 52 weeks | HRSD; BDI | Fair |
| Simon et al., 2004 [40] and Simon et al., 2009 [41] | Antidepressant and depressive symptoms | 44.8 (15.5) | 74% | 80% | PC | US | Registry | 24 weeks | SCL | Good |
| Ward et al., 2000 [42] and King et al., 2000 [43] | Depression or mixed anxiety depression | 36.8 (12.2) | 76% | 89% | PC | UK | Referral | 52 weeks | BDI-21 | Fair |
| Williams et al., 2000 [44] and Frank et al., 2002 [3] and Katon et al., 2002 [45] | Dysthymia or minor depression | 71 (7.1) | 43% | 76% | PC | US | Screening and referral | 11 weeks | HSCL-D-20; HRSD | Good |
| Wilson, 1982 [28] | Self-report of depression | 38.8 (NR) | 66% | NR | MH | AUS | Advertisement | 26 weeks | BDI | Poor |
| Wilson, 1983 [27] | Self-report of depression | 39.5 (NR) | 80% | NR | MH | AUS | Advertisement | 8 weeks | BDI; HRSD | Fair |
Weeks since baseline assessment.
Quality assessments were conducted for the seven newly identified RCTs, and in order to conduct the meta-analysis on studies of brief CBT, quality assessments were completed for two studies that had been included in the systematic reviews.
Italicized studies were included in the Cuijpers or Cape review, or both.
Abbreviations: AUS = Australia, BDI = Beck Depression Inventory, DHP = Diabetes Health Profile, DIS = Diagnostic Interview Schedule, EU = European
Countries, GDS = Geriatric Depression Scale, GP = general practitioner, HRSD = Hamilton Rating Scale for Depression, HSLC-D = Headache Specific Locus of Control-Depression, MDD = major depressive disorder, MH = mental health, MMPI-D = Minnesota Multiphasic Personality Inventory Depression Scale, MOS-D = Medical Outcomes Study-Depression, NR = not reported, PC = primary care, PRIME-MD = Primary Care Evaluation of Mental Disorders Patient Health Questionnaire, RDC = Research Diagnostic Criteria, SADS-L = Schedule for Affective Disorders and Schizophrenia–Lifetime Version, SCAN = Schedules for Clinical Assessment in Neuropsychiatry, SCL = Symptom Checklist, UK = United Kingdom, US = United States
Table 3.
Summary of Intervention Characteristics
| Author, year | Therapy | # sessions | Session length | Session frequency | Modality | Therapist | Treatment fidelity? | Therapy completed [n (%)] | Control |
|---|---|---|---|---|---|---|---|---|---|
| Barnhofer et al., 2009 [29] and Hargus et al., 2010 [31] | MBCT (n = 16) | 8 | 2 hours | Weekly | Group | MBCT therapists | Yes | 14 (88%) | TAU (n = 14) |
| Barrett et al., 2001 [32] and Frank et al., 2002 [3] | PST (n = 80) | 6 | 30 min | Ever 2 weeks | Individual | PhD psychologist | Yes | 64 (80%) | Placebo (n = 81) |
| Dowrick et al., 2000 [4] | PST (n = 128) | 6 | 30 min | NR | Individual | Psychologists, nurses, allied health professionals | Yes | 80 (63%) | Waitlist (n = 189) |
| Laidlaw et al., 2008 [33] | CBT (n = 21) | 8 | NR | NR | Individual | Master’s-level psychologist | Yes | 20 (95%) | TAU (n = 23) |
| Lynch et al., 1997 [34] | PST (n = 15) | 6 | 20 min | Weekly | Individual; telephone | Graduate students | No | 11 (73%) | Usual care (n = 14) |
| Lynch et al., 2004 [35] | PST (n = 18) | 6 | NR | Weekly | Individual; telephone | Nurses | Yes | NR | Usual care (n = 18) |
| Mynors-Wallis et al., 1995 [36] | PST (n = 30) | 6 | 30 min | Every 2 weeks | Individual | Experienced psychiatrist and trained GPs | No | 28 (93%) | Placebo (n = 30) |
| Mynors-Wallis et al., 2000 [37] | PST+Med (n = 35) | 6 | 30 min | Every 2 weeks | Individual | Research practice nurse | No | 34 (97%) | Med alone (n = 36) |
| Nezu, 1986 [38] | PST (n = 12) | 8 | 1.75 hours | Weekly | Group | Graduate students | Yes | 11 (92%) | Waitlist control (n = 9) |
| Scott et al., 1997 [39] | CBT (n = 24) | 6 | 30 min | Weekly | Individual | CBT therapist | Yes | 18 (75%) | Usual care (n = 24) |
| Simon et al., 2004 [40] and Simon et al., 2009 [41] | CBT+TCM (n = 195) | 8 | 35 min | Every 1.5 weeksa | Individual; Telephone | Master’s-level psychologist | No | 167 (86%) | TCM (n = 207) |
| Ward et al., 2000 [42] and King et al., 2000 [43] | CBT (n = 63) | 6 | 50 min | Weekly | Individual | Experienced psychologists | Yes | 56 (89%) | Usual care (n = 67) |
| Williams et al., 2000 [44] and Frank et al., 2002 [3] and Katon et al., 2002 [45] | PST (n = 138) | 6 | 30 min | Every 2 weeks | Individual | PhD psychologist, social workers, master’s-level counselors | Yes | 108 (78%) | Medication; placebo (n = 140) |
| Wilson, 1982 [28] | CBT (n 32)b | 7 | 1 hour | Weekly | Individual | Graduate students | NR | 21 (66%) | Minimal contactc (n ≈ 32)b |
| Wilson, 1983 [27] | CBT (n = 16) | 8 | 1 hour | Weekly | Individual | NR | No | 12 (75%) | Waitlist (n = 9) |
Weekly sessions for first 4 weeks, with frequency ranging from every 1 to 4 weeks for remaining four sessions.
Estimate based on data provided in article.
Minimal contact consisted of two 1-hour nondirective therapy sessions to coincide with medication refills.
Italicized studies were included in the Cuijpers or Cape review, or both.
Abbreviations: CBT = cognitive behavioral therapy (includes cognitive therapy and behavioral therapy), MBCT = mindfulness-based cognitive therapy, min = minutes, NR = not reported, PST = problem-solving therapy, TAU = treatment as usual, TCM = telephone case management
Table 4.
Key Clinical Outcome Measures
| Study | Quality of life | Social functioning | Occupational status | Patient satisfaction | Adverse treatment effects |
|---|---|---|---|---|---|
| Barnhofer et al., 2009 [29] and Hargus et al., 2010 [31] | NR | NR | NR | NR | NR |
| Barrett et al., 2001 [32] and Frank et al., 2002 [3] | Yes, SF-36 | NR | NR | NR | NR |
| Dowrick et al., 2000 [4] | Yes, SF-36 | NR | NR | NR | NR |
| Laidlaw et al., 2008 [33] | Yes, WHOQOL-BREF | Yes, social relationships | NR | NR | NR |
| Lynch et al., 1997 [34] | NR | Yes | NR | NR | NR |
| Lynch et al., 2004 [35] | NR | NR | NR | NR | NR |
| Mynors-Wallis et al., 1995 [36] | NR | Yes | NR | Yes | NR |
| Mynors-Wallis et al., 2000 [37] | NR | Yes, Social Adjustment Scale | NR | NR | Yes, medication side effects |
| Nezu, 1986 [38] | NR | NR | NR | NR | NR |
| Scott et al., 1997 [39] | NR | NR | NR | NR | NR |
| Simon et al., 2004 [40] and Simon et al., 2009 [41] | NR | NR | NR | Yes | NR |
| Ward et al., 2000 [42] and King et al., 2000 [43] | Yes, EuroQoL | Yes | NR | NR | NR |
| Williams et al., 2000 [44] and Frank et al., 2002 [3] and Katon et al., 2002 [45] | Yes, SF-36 | NR | NR | NR | NR |
| Wilson, 1982 [28] | NR | NR | NR | NR | NR |
| Wilson, 1983 [27] | NR | NR | NR | NR | NR |
Italicized studies were included in the Cuijpers or Cape review, or both.
Abbreviations: NR = not reported, WHOQOL = World Health Organization Quality of Life
EFFICACY OF BRIEF PSYCHOTHERAPY
Systematic Reviews
In the Cuijpers’ systematic review [25], the sub-analysis examining psychotherapies with six or fewer sessions (k=5 PST and 2 CBT) found these treatments to have a small but significant positive effect for the treatment of depression in primary care (ES −0.25, 95% CI −0.48 to −0.02, NNT=7.14). This effect size was not significantly different from that for psychotherapies of 7 to 16 sessions (ES −0.36, 95% CI −0.54 to −0.17). In Cape’s review [26], the sub-analyses on psychotherapies for depression with 10 or fewer sessions demonstrated a significant but small effect favoring brief CBT over usual general practitioner care for depression (k=4; ES −0.33, 95% CI −0.60 to −0.06) and positive but statistically nonsignificant effects for PST (k=5; ES −0.26, 95% CI −0.49 to 0.03) and counseling (k=4; ES −0.41, 95% CI −0.84 to 0.03) over usual general practitioner care. No significant differences in efficacy were found between CBT, PST, and counseling.
Primary Literature
While six of the eight identified PST studies were previously included in the systematic reviews, the prior reviews only included two of the six CBT studies that we identified. Because the 4 newly identified studies of CBT contained 535 of the total 713 participants across the 6 CBT studies, we conducted an updated and more adequately powered meta-analysis of brief CBT (6 to 8 sessions) for depression.
In the meta-analysis, we found that participants receiving brief CBT for depression were more likely than participants receiving a control treatment to have reduced symptoms of depression (ES −0.42, 95% CI −0.74 to −0.10), but treatment effects differed significantly across studies (Cochran Q=13.74, p=0.03, I2=56%) (Figure 3). The ES of −0.42 corresponds to an NNT of approximately 4.5. A funnel plot did not suggest significant publication bias, but with only six studies, this method has limited power to detect publication bias. In an influence analysis conducted to examine the moderate level of variability present, the summary estimate ranged from −0.24 to −0.53, with the trial by Wilson [27] having the greatest influence. This trial was the only CBT study to use a waitlist control condition as the comparator. Based on a priori hypotheses of variables that might influence the effect size estimate, we conducted two sensitivity analyses. In the first, we removed the single poor-quality study [28] and found that brief CBT for depression continued to be significantly more effective than control (ES −0.50, 95% CI −0.91 to −0.09), but treatment effects remained significantly heterogeneous (Cochran Q=13.71, p=0.008, I2=71%). In the second, we removed the poor-quality [28] study and the study with a waitlist comparator [27] and found that treatment effects of brief CBT for depression were smaller (ES −0.24, 95% CI −0.42 to −0.06) but homogeneous (Cochran Q=1.44, p=0.70, I2=0%). This effect size corresponds to an NNT of approximately 8.
Figure 3.
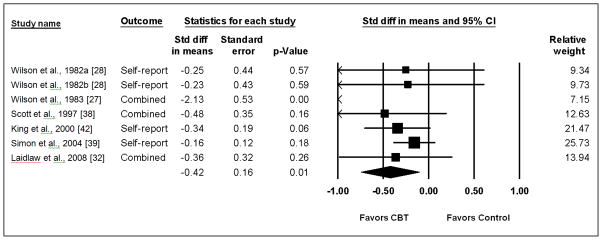
Meta-analysis of Brief CBT for Depression
Since only 92 of the total 973 participants across the 8 PST studies were from the 2 newly identified studies of PST, we did not conduct an updated meta-analysis for PST. The single study of MBCT identified in our review found 8 sessions of MBCT to be more efficacious than treatment as usual at reducing depressive symptoms at 8 weeks (F=13.42, p=0.001) [29].
NON-MENTAL HEALTH TREATMENT PROVIDERS
In all four trials that involved non-mental health professionals (e.g., nurses, allied health professionals, and general practitioners) as treatment providers, the intervention was PST. Compared to the PST trials that used solely mental health professionals, the trials involving non-mental health professionals did not have a pattern of results suggesting any meaningful differences in efficacy for PST. Quantitative syntheses to examine differences on the basis of provider type, treatment intensity, individual versus group, or telephone versus in-person could not be completed because there was not an adequate number of studies in each of these subgroups.
DISCUSSION
We identified 2 systematic reviews and 15 randomized controlled trials of brief psychotherapy (i.e., ≤ 8 sessions) for depression, encompassing 1716 patients with MDD or depressive symptomatology. Both systematic reviews concluded that brief CBT and PST are efficacious for the acute-phase treatment of depression in primary care. This conclusion was corroborated by our analyses of 15 randomized controlled trials, 7 of which had not been included in either of the two identified systematic reviews. Effect sizes for brief psychotherapy are modest but at present appear comparable to those observed in trials of antidepressant medications and of standard duration psychotherapies [30]. Table 5 summarizes the strength of evidence.
Table 5.
Summary of the Strength of Evidence
| Intervention | Risk of Bias: Design/Quality | Consistency | Directness | Precision | Standardized mean difference (95% CI) and strength of evidence |
|---|---|---|---|---|---|
| Brief CBT | RCTs/Fair | Consistent | Direct | Some imprecision | −0.42 (−0.74 to −0.10) Moderate |
| Brief PST | RCTs/Good | Consistent | Direct | Some imprecision | −0.26 (−0.49 to 0.03) Moderate |
| MBCT | RCT/Good | NA | Direct | Serious imprecision | Low |
| Other therapies | NA | NA | NA | NA | Insufficient |
Our review found that brief psychotherapies have been provided by psychologists, graduate students, nurses, general practitioners, and other allied health professionals who had received training and supervision specific to the intervention being conducted. Details about training were sparse, meaning that the degree of training necessary to replicate studies’ results is uncertain. A key component of replicating positive treatment effects may be fidelity monitoring, which is likely to be particularly important with generalist clinicians.
This review aimed to determine the overall efficacy of brief psychotherapies rather than the comparative effectiveness of brief vs. standard-duration psychotherapies. However, Cuijpers’ review [25] found no statistically significant differences between psychotherapies delivered in 6 sessions compared to psychotherapies delivered in 7 to 16 sessions. Additionally, in an important trial conducted by Shapiro and colleagues [16], 117 patients with depression were randomized to either 8 or 16 sessions of manualized psychotherapy, and 16 sessions was found to be superior to 8 only for those with severe depression. This trial did not meet our inclusion criteria due to the comparator condition being an active psychotherapy, but the findings are consistent with those from the present review and the trial design merits imitation by other researchers.
The present study has a number of strengths, including a protocol-driven review, a comprehensive search, careful quality assessment, and rigorous quantitative synthesis methods. Additionally, this is the first review to our knowledge to focus exclusively on brief psychotherapy for depression. However, the existing literature leaves multiple unresolved questions. First, the question of whether brief psychotherapies are less efficacious than standard-duration psychotherapies (i.e., 12 to 20 sessions) needs to be more fully answered in the context of controlled trials. Second, too few studies assessed long-term outcomes after the conclusion of brief psychotherapies (e.g., 6 months or longer) or included a broad set of outcome measures (e.g., quality of life, social functioning, and occupational status). Third, it remains to be determined which brief psychotherapies (CBT, PST, or other) can be provided with high treatment fidelity by different professionals, such as nurses, nurse practitioners, primary care physicians, social workers, or clinical chaplains. Fourth, the studies included in this review were composed primarily of Caucasian, middle-aged females, limiting applicability to many other segments of society. Finally, the relatively few studies included in this review did not allow for stratified comparisons on important variables such as depression severity (i.e., mild, moderate, severe), treatment setting (e.g., mental health clinic, primary care), or augmentation of brief psychotherapy with medication.
CONCLUSIONS
Brief psychotherapy is an effective option for the acute-phase treatment of depression. With many protocols requiring only 6 sessions of 30 minutes each that can be provided by either mental health professionals or trained non-mental health providers, brief psychotherapies present an attractive treatment alternative for implementation in the primary care environment. Although future research is plainly needed, immediate attention is demanded by the enormous human suffering and high economic burden associated with depressive disorders.
Acknowledgments
We would like to thank the VHA Office of Quality Performance, the project staff at the Durham VA Evidence-based Practice Center, the peer reviewers of the original VA evidence synthesis report, the VA Mid-Atlantic MIRECC, and the VA Health Services Research and Development Evidence Synthesis Program. The Department of Veterans Affairs Evidence-based Synthesis Program funded this review. The views and opinions in this manuscript are those of the authors and do not reflect those of the VA.
References
- 1.Current depression among adults---United States, 2006 and 2008. MMWR Morb Mortal Wkly Rep. 2010;59:1229–1235. [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 3.Frank E, Rucci P, Katon W, Barrett J, Williams JW, Jr, Oxman T, Sullivan M, Cornell J. Correlates of remission in primary care patients treated for minor depression. Gen Hosp Psychiatry. 2002;24:12–19. doi: 10.1016/s0163-8343(01)00173-6. [DOI] [PubMed] [Google Scholar]
- 4.Dowrick C, Dunn G, Ayuso-Mateos JL, Dalgard OS, Page H, Lehtinen V, Casey P, Wilkinson C, Vazquez-Barquero JL, Wilkinson G. Problem solving treatment and group psychoeducation for depression: multicentre randomised controlled trial. Outcomes of Depression International Network (ODIN) Group. BMJ. 2000;321:1450–1454. doi: 10.1136/bmj.321.7274.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gill D, Hatcher S. Antidepressants for depression in medical illness. Cochrane Database of Systematic Reviews. 2000;(4):Art. No.: CD001312. doi: 10.1002/14651858.CD001312.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulberg HC, Block MR, Madonia MJ, Scott CP, Lave JR, Rodriguez E, Coulehan JL. The 'usual care' of major depression in primary care practice. Arch Fam Med. 1997;6:334–339. doi: 10.1001/archfami.6.4.334. [DOI] [PubMed] [Google Scholar]
- 7.Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C. Combined pharmacotherapy and psychological treatment for depression: a systematic review. Arch Gen Psychiatry. 2004;61:714–719. doi: 10.1001/archpsyc.61.7.714. [DOI] [PubMed] [Google Scholar]
- 8.DeLeon PH, NPR, Smedley BD. The future is primary care. In: Frank RG, McDaniel SH, Bray JH, Heldring M, editors. Primary care psychology. Washington: American Psychological Association; 2004. pp. 317–325. [Google Scholar]
- 9.van Schaik DJF, Klijn AFJ, van Hout HPJ, van Marwijk HWJ, Beekman ATF, de Haan M, van Dyck R. Patients' preferences in the treatment of depressive disorder in primary care. General Hospital Psychiatry. 2004;26:184–189. doi: 10.1016/j.genhosppsych.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Trivedi RB, Nieuwsma JA, Williams JW., Jr Examination of the utility of psychotherapy for patients with treatment resistant depression: A systematic review. Journal of General Internal Medicine. 2010;26:643–650. doi: 10.1007/s11606-010-1608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fava GA, Rafanelli C, Grandi S, Canestrari R, Morphy MA. Six-year outcome for cognitive behavioral treatment of residual symptoms in major depression. Am J Psychiatry. 1998;155:1443–1445. doi: 10.1176/ajp.155.10.1443. [DOI] [PubMed] [Google Scholar]
- 12.Beck JS. Cognitive Therapy: Basics and Beyond. New York: Guilford Press; 1995. [Google Scholar]
- 13.Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- 14.Dewan MJ, Steenbarger BN, Greenberg RP, Hales RE, Yudofsky SC, Gabbard GO. The American Psychiatric Publishing textbook of psychiatry. 5. Arlington, VA: American Psychiatric Publishing, Inc; 2008. Brief psychotherapies; pp. 1154–1170. [Google Scholar]
- 15.Robinson P. Adapting empirically supported treatments to the primary care setting: A template for success. In: O'Donohue WT, Byrd MR, Cummings NA, Henderson DA, editors. Behavioral Integrative Care: Treatments that work in the primary care setting. New York: Brunner-Routledge; 2005. pp. 53–72. [Google Scholar]
- 16.Shapiro DA, Barkham M, Rees A, Hardy GE, Reynolds S, Startup M. Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioral and psychodynamic-interpersonal psychotherapy. Journal of Consulting and Clinical Psychology. 1994;62:522–534. doi: 10.1037/0022-006x.62.3.522. [DOI] [PubMed] [Google Scholar]
- 17.Whitlock EP, Lin JS, Chou R, Shekelle P, Robinson KA. Using existing systematic reviews in complex systematic reviews. Ann Intern Med. 2008;148:776–782. doi: 10.7326/0003-4819-148-10-200805200-00010. [DOI] [PubMed] [Google Scholar]
- 18.Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychological treatment of depression: a meta-analytic database of randomized studies. [Accessed January 12, 2011];BMC Psychiatry. 2008 8:36. doi: 10.1186/1471-244X-8-36. Available at: ( www.psychotherapyrcts.org/index.php?id=3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality; [Accessed January 12, 2011]. Available at: www.effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports/?pageaction=displayproduct&productid=318. [Google Scholar]
- 21.Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry. 2006;59:990–996. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Borenstein M. Introduction to meta-analysis. Chichester, West Sussex, U.K. ; Hoboken: John Wiley & Sons; 2009. [Google Scholar]
- 23.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 24.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O'Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer TT, Varonen H, Vist GE, Williams JW, Jr, Zaza S. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuijpers P, van Straten A, van Schaik A, Andersson G. Psychological treatment of depression in primary care: a meta-analysis. British Journal of General Practice. 2009;59:e51–60. doi: 10.3399/bjgp09X395139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cape J, Whittington C, Buszewicz M, Wallace P, Underwood L. Brief psychological therapies for anxiety and depression in primary care: meta-analysis and meta-regression. BMC Med. 2010;8:38. doi: 10.1186/1741-7015-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson PH. Comparative efficacy of behavioral and cognitive therapies of depression. Cognitive Therapy and Research. 1983;7:111–124. [Google Scholar]
- 28.Wilson PH. Combined pharmacological and behavioural treatment of depression. Behav Res Ther. 1982;20:173–184. doi: 10.1016/0005-7967(82)90116-4. [DOI] [PubMed] [Google Scholar]
- 29.Barnhofer T, Crane C, Hargus E, Amarasinghe M, Winder R, Williams JM. Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behav Res Ther. 2009;47:366–373. doi: 10.1016/j.brat.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spielmans GI, Berman MI, Usitalo AN. Psychotherapy versus second-generation antidepressants in the treatment of depression: A meta-analysis. Journal of Nervous and Mental Disease. 2011;199:142–149. doi: 10.1097/NMD.0b013e31820caefb. [DOI] [PubMed] [Google Scholar]
- 31.Hargus E, Crane C, Barnhofer T, Williams JM. Effects of mindfulness on meta-awareness and specificity of describing prodromal symptoms in suicidal depression. Emotion. 2010;10:34–42. doi: 10.1037/a0016825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barrett JE, Williams JW, Jr, Oxman TE, Frank E, Katon W, Sullivan M, Hegel MT, Cornell JE, Sengupta AS. Treatment of dysthymia and minor depression in primary care: a randomized trial in patients aged 18 to 59 years. Journal of Family Practice. 2001;50:405–412. [PubMed] [Google Scholar]
- 33.Laidlaw K, Davidson K, Toner H, Jackson G, Clark S, Law J, Howley M, Bowie G, Connery H, Cross S. A randomised controlled trial of cognitive behaviour therapy vs treatment as usual in the treatment of mild to moderate late life depression. Int J Geriatr Psychiatry. 2008;23:843–850. doi: 10.1002/gps.1993. [DOI] [PubMed] [Google Scholar]
- 34.Lynch DJ, Tamburrino MB, Nagel R. Telephone counseling for patients with minor depression: preliminary findings in a family practice setting. Journal of Family Practice. 1997;44:293–298. [PubMed] [Google Scholar]
- 35.Lynch D, Tamburrino M, Nagel R, Smith MK. Telephone-based treatment for family practice patients with mild depression. Psychological Reports. 2004;94:785–792. doi: 10.2466/pr0.94.3.785-792. [DOI] [PubMed] [Google Scholar]
- 36.Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mynors-Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ. 2000;320:26–30. doi: 10.1136/bmj.320.7226.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. J Consult Clin Psychol. 1986;54:196–202. doi: 10.1037//0022-006x.54.2.196. [DOI] [PubMed] [Google Scholar]
- 39.Scott C, Tacchi MJ, Jones R, Scott J. Acute and one-year outcome of a randomised controlled trial of brief cognitive therapy for major depressive disorder in primary care. British Journal of Psychiatry. 1997;171:131–134. doi: 10.1192/bjp.171.2.131. [DOI] [PubMed] [Google Scholar]
- 40.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292:935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 41.Simon GE, Ludman EJ, Rutter CM. Incremental benefit and cost of telephone care management and telephone psychotherapy for depression in primary care. Arch Gen Psychiatry. 2009;66:1081–1089. doi: 10.1001/archgenpsychiatry.2009.123. [DOI] [PubMed] [Google Scholar]
- 42.Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S, Gabbay M, Tarrier N, Addington-Hall J. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy, and usual general practitioner care for patients with depression. I: clinical effectiveness. BMJ. 2000;321:1383–1388. doi: 10.1136/bmj.321.7273.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, Byford S. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care. Health Technology Assessment. 2000;4:1–83. [PubMed] [Google Scholar]
- 44.Williams JW, Jr, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, Cornell J, Sengupta A. Treatment of dysthymia and minor depression in primary care: A randomized controlled trial in older adults. JAMA. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 45.Katon W, Russo J, Frank E, Barrett J, Williams JW, Jr, Oxman T, Sullivan M, Cornell J. Predictors of nonresponse to treatment in primary care patients with dysthymia. Gen Hosp Psychiatry. 2002;24:20–27. doi: 10.1016/s0163-8343(01)00171-2. [DOI] [PubMed] [Google Scholar]