Abstract
Informatics tools can help support the health and independence of older adults. In this paper, we present an approach towards integrating health-monitoring data and describe several techniques for the assessment and visualisation of integrated health and well-being of older adults. We present three different visualisation techniques to provide distinct alternatives towards display of the same information, focusing on reducing the cognitive load of data interpretation. We demonstrate the feasibility of integrating health-monitoring information into a comprehensive measure of wellness, while also highlighting the challenges of designing visual displays targeted at multiple user groups. These visual displays of wellness can be incorporated into personal health records and can be an effective support for informed decision-making.
Keywords: data visualisation, older adults, integrated health, graphical displays, electronic healthcare
1 Introduction
The Health Resources and Services Administration (2002) predicts that in the USA the demographic population greater than 65 years of age will grow by 54% between 2000 and 2020. Though this is a testament towards modern medicine and healthcare, the significant growth of the ageing population does present challenges. Healthcare costs are expected to increase such that by 2029 the Medicare trust fund will be depleted (Lubitz et al., 2003). Factors such as chronic illness, increased medication needs, and reduced independence contribute to the growing costs of supporting an older adult population (Rogowski et al., 1997; Guralnik et al., 2002; Loeb et al., 2003). Despite improvements in healthcare, the longevity of older adults is tempered by declining health, reduced mobility, and diminished social interactions (Johnson and Wolinsky, 1993; Alpass and Neville, 2003). Limited resources and a declining workforce make it difficult to provide comprehensive care for older adults (Health Resources and Services Administration, 2002). One solution to this problem is through the development of innovative informatics tools. These include monitoring tools installed in a residential setting to help support independence and quality of life (Demiris and Hensel, 2008). Older adults are willing to adapt such monitoring tools, especially if their perceived needs are greater than their concerns with privacy (Courtney, 2008). These positive attitudes are associated with the recognition that new technologies can improve daily life (Demiris et al., 2004). Applications to electronic home healthcare often face issues of accessible design (Demiris, 2004); development of data visualisations can further support communication between patient and provider and facilitate health monitoring (Alamantariotou and Zisi, 2010).
This work expands on a prior investigation involving the use of health monitoring tools within an independent and assisted living facility (Thompson et al., 2011). In that study, researchers collected data over an eight-week period examining cognitive, physiological, social, and spiritual measures of well-being within a population of older adults. The data collected from these health-monitoring technologies provided valuable insights towards the health and well-being of older adults. However, the monitoring technologies also produced large amounts of data, which can be difficult to manage and present in a meaningful manner. In order to organise the data more effectively, we applied Halbert Dunn’s conception of wellness, defined as “an integrated method for functioning which is oriented toward maximising the potential of which the individual is capable… maintain a continuum of balanced and purposeful direction within the environment where he/she is functioning” (Dunn, 1959) towards presenting holistic health. In this context, a wellness assessment can be a comprehensive summary of health and well-being; its visualisation can provide a meaningful overview of one’s health progress over time. We present several techniques for visualising wellness guided by cognitive design principles. These techniques provide examples of integrated health monitoring information for a holistic view of wellness that older adults, family members, and clinicians can leverage for informed decision-making. It is also possible to apply the data visualisation techniques within applications such as personal health records (PHR) or mobile platforms to support electronic healthcare.
2 Background and significance
2.1 Integration of health data
Applications to monitor the health status of older adults have been an increasing area of work (Helal et al., 2005; Chan et al., 2008; Cook and Schmitter-Edgecombe, 2009; Sagahyroon et al., 2009). The quickest growing demographic group in the USA is that of older adults greater than 85 years of age (Campion, 1994; James and Schneider, 2010). This presents opportunities to apply informatics tools that can help support optimal functionality and overall health for older adults. These information technologies include a wide range of assessment systems that produce large amounts of data. However, the overall well-being of an individual is still difficult to assess despite the availability of data provided about the status of an individual. Rather than relying on the user to synthesise independent measures of health from multiple sources, an integrated visualisation tool can reduce the cognitive load, while presenting a holistic assessment of the individual’s health and well-being. There is a growing challenge to integrate heterogeneous sources of health information and to visualise in an effective manner (Cabarcos et al., 2010). The appropriate design of visualisations for complex data sets can help facilitate electronic healthcare delivery.
2.2 Impact of visualisation on decision-making
To develop and apply different techniques of data visualisation from health information technologies, we have examined the impact of visualisation on decision-making. Cognitive theories on graph comprehension have proposed different models for the interpretation of visual graphics. Pinker proposes a model of cognitive processing for the translation of raw visual graphics into an encoded visual description. These include principles for the mapping of visual relationships based on spatial location, magnitude, and groupings of images (Pinker, 1990). Cleveland and McGill (1984) identified a set of six elementary perceptual tasks involved during data visualisation. They further ordered these elementary perceptual tasks based on accuracy of performance. These elementary tasks include identification of position along a common scale, position along a non-aligned scale, length and angle, area, volume, and shading. We applied these models for perception and cognition of visual graphics as guidelines toward the development of cognitively appealing visualisations of health data.
The interpretation of graphical visualisations can play a significant role in decision-making, influencing both the types of decisions made and the efficiency with which they are made. Carpenter and Shah (1998) introduce a cognitive model for graphical display comprehension that consists of bottom up and top-down processing. For both approaches, errors and biases can occur; however, an experienced viewer attempts to limit these biases. The presentation of visual information can also reduce these biases while increasing efficiency. In a study by Hoeke et al. (2000), a set of 12 lab results were presented using four different visual displays. Researchers then assessed the accuracy and speed of classifying abnormal lab results. They found statistical significances in differences of speed in decision-making, though the study did not provide enough evidence to show differences in accuracy of these decisions (Hoeke et al., 2000). A separate study by Elting et al. (1999) examined the impact of visual display on physician decisions to stop clinical trials. The researchers found that the graphical display of data influenced the accuracy of decision making despite the same numerical data.
Visual displays can also influence decision making from the patient perspective. Feldman-Stewart et al. (2007) examined differences in accuracy and ease of processing for risk assessment through different graphical displays. For each of six display formats, pair-wise data were presented and users identified which figure had greater survival rates. The type of visual display influenced both accuracy and speed of decision-making. Morrow et al. (1998) found that an icon display integrated with text was more effective at presenting medication information to older adults compared to a text only method. Their results suggested quicker, more accurate, and broader retention of medication information using these icon displays. These studies provide a framework for the importance of properly designing visual displays that can support decision making in an efficient and accurate manner. However, there has been limited work describing the visualisation of integrated health information targeted at an older adult population. An integrated visual display can provide a comprehensive overview of health and wellness. By reducing the complexity of health data, these visual displays can be important tools to support shared decision making between older adults and healthcare providers (Frosch and Kaplan, 1999; Naik et al., 2005).
3 Development of data visualisation techniques
3.1 Preliminary studies
In prior work, a pilot study combined commercially available health technologies for the comprehensive assessment of wellness (Thompson et al., 2011). The platform architecture for the pilot study included a telehealth kiosk and cognitive assessment software. Questionnaires provided additional information on social and spiritual components of well-being. Researchers conducted the pilot study in a retirement community over an eight-week period with enrolment of 27 older adults (average age of 88.2 years). This preliminary work demonstrated the feasibility of applying health assessment tools within an older adult community. Focus groups indicated a strong acceptance of assessment technologies and users were interested in future applications of the health data (Thompson et al., 2011).
Data collected from that pilot study were conceptualised by our group into the four categories as described by Dunn’s theoretical framework for wellness: functional/physiological (i.e. systolic blood pressure, activities of daily living, health-related quality of life), social (i.e. social support by family, friends, significant other), spiritual (i.e. spirituality scale), and cognitive health (i.e. specific cognitive tasks like planning). In order to create one integrated measure for each wellness category, we generated a composite measure using weighted t-scores of the constituent variables, normalised relative to published adult data. We chose the t-score as it is more easily interpretable than other similar composite metrics (e.g. scores above 50 are above the mean). We calculated this score for each participant at baseline and at the end of the eight-week pilot study, which we then used for the development of data visualisation techniques.
3.2 Design principles for data visualisation
We focused on two primary components during the development of visualisation techniques: (a) a holistic wellness graph, and (b) a view of longitudinal data for the detection of health trends. Our approach first involved developing integrated graphical displays, which combined each wellness category (physiological, social, spiritual, and cognitive). Cognitive design principles guided these visual graphs, with an emphasis on reducing cognitive load for processing of visual information. We applied Pinker’s theory of graphical comprehension, which states that the ability to extract information from a graph becomes increasingly difficult as the number of inferential and top-down processing steps is required (Pinker, 1990). Larkin and Simon (1987) provided further insights for the design process, addressing the cognitive efficiencies of a graph to substitute information for complex non-visual operators and to reduce the search space for desired information. These theories suggested designs that were minimalistic while supporting the ability of users to abstract information not otherwise apparent through tabular representations. To address the accuracies of graphical comprehension, we applied the theories of Cleveland and McGill (1984), which identified a set of elementary perceptual tasks and ranked them based on accuracy of graphical comprehension. The perceptual tasks ranged from identification of position, to differences in shading. Our visual displays applied these principles to minimise possible errors during graphical interpretation.
The second component of visualisation involved extending our visual techniques for longitudinal analysis and identification of trends. This becomes important within a health related setting where early intervention can delay the progression of health decline for older adults (Drewnowski and Evans, 2001; Chang et al., 2004; Cattan et al., 2005). We applied the visual techniques to display wellness data at baseline and at the completion of the pilot study, corresponding to pre and post data. These comparisons provide information on changes in functional health states as measured through health monitoring technologies over an eight-week period. We also generated a hypothetical data set across a 12-month interval to observe the effectiveness of the graphical methods towards identifying longitudinal trends in health. We designed these displays to multiple stakeholders including older adults, family members, and healthcare providers. Creating a visual display that fills the needs across all user groups was a challenge; we present three different approaches to visualising this information.
4 Data visualisation techniques
We developed three visual designs to integrate and present health data while demonstrating distinct approaches to visualising complex longitudinal health related data sets. The designs focused on presenting information in a cognitively enhancing manner, while allowing users to monitor trajectories of wellness over time. Our designs included a stacked bar chart, a Wellness Polygon, and a partitioned donut. These designs provide distinct data visualisation alternatives allowing for comparisons across scales of length and area. We extended data collected from the pilot study to create a hypothetical data set spanning 12 months. We plotted the same data set across each visual display to examine differences in visual techniques rather than focusing on differences in data.
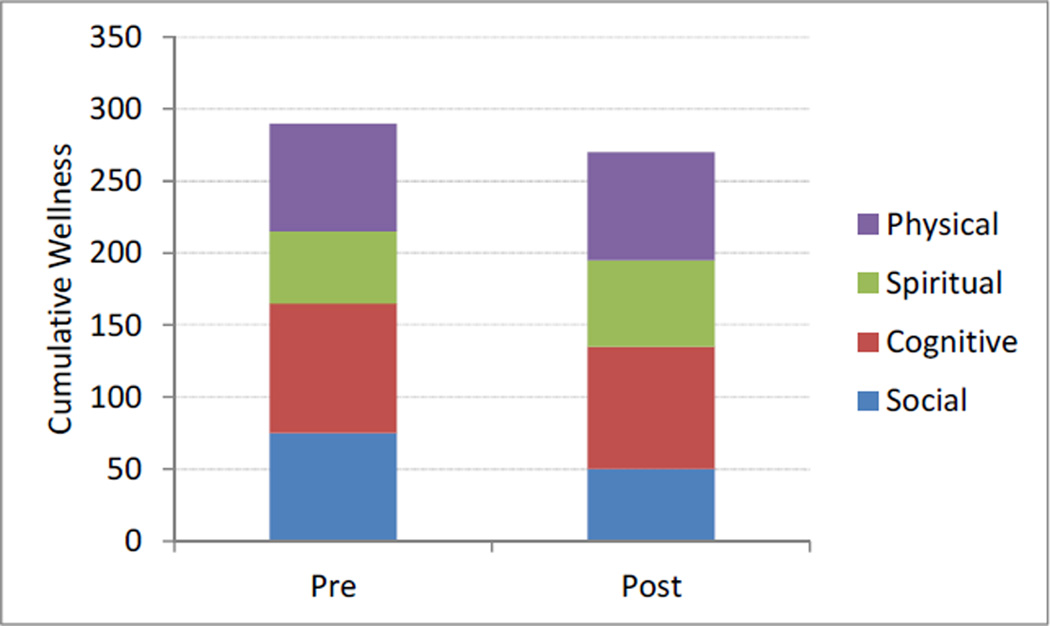
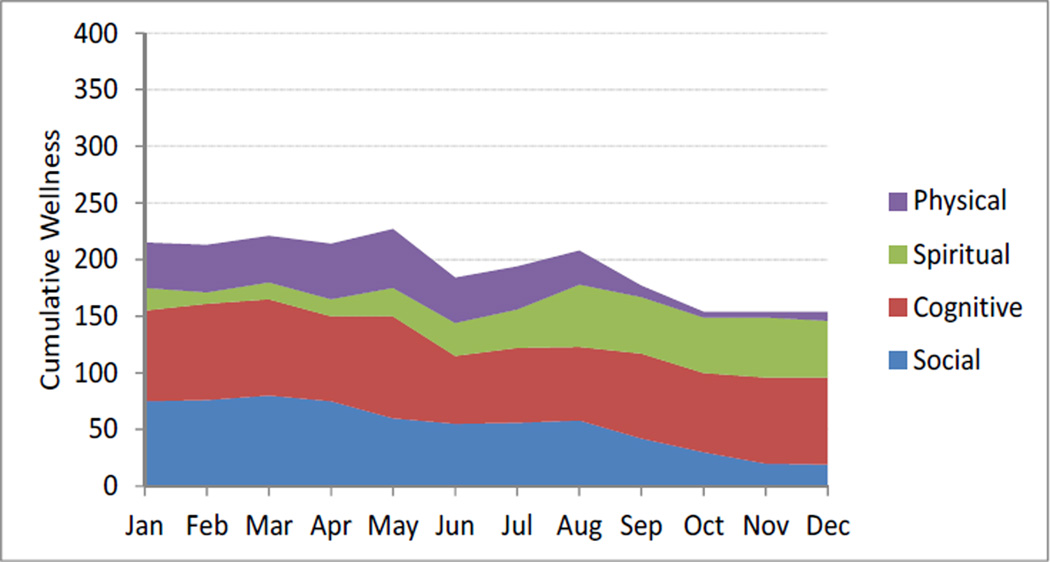
4.1 Visualisation technique 1 – stacked bar chart
We applied a stacked bar chart to present integrated health information. The bar corresponds to a cumulative measure of wellness while each stack within the bar is a different component of wellness. The scale of each stack represents the normalised score for each component of wellness. This graphical presentation of data reduces the cognitive load required to interpret health information collected from multiple assessment technologies by comparing measures along a common aligned scale (Cleveland and McGill, 1984). A comparison of bar length for pre and post data allows users to identify overall changes to wellness. Examining each stack in the bar provides further information on individual components of wellness. Comparisons within stack are cognitively more difficult since the visualisation no longer aligns each stack along the vertical scale. Longitudinal presentation of this information simply extends each bar chart temporally on the x-axis with monthly data points. For example, longitudinal data can indicate declining trends in overall wellness, while examining changes in segment size allows for comparisons of individual components of health. We selected this visual technique to provide a simple, efficient method for displaying integrated health data over time.
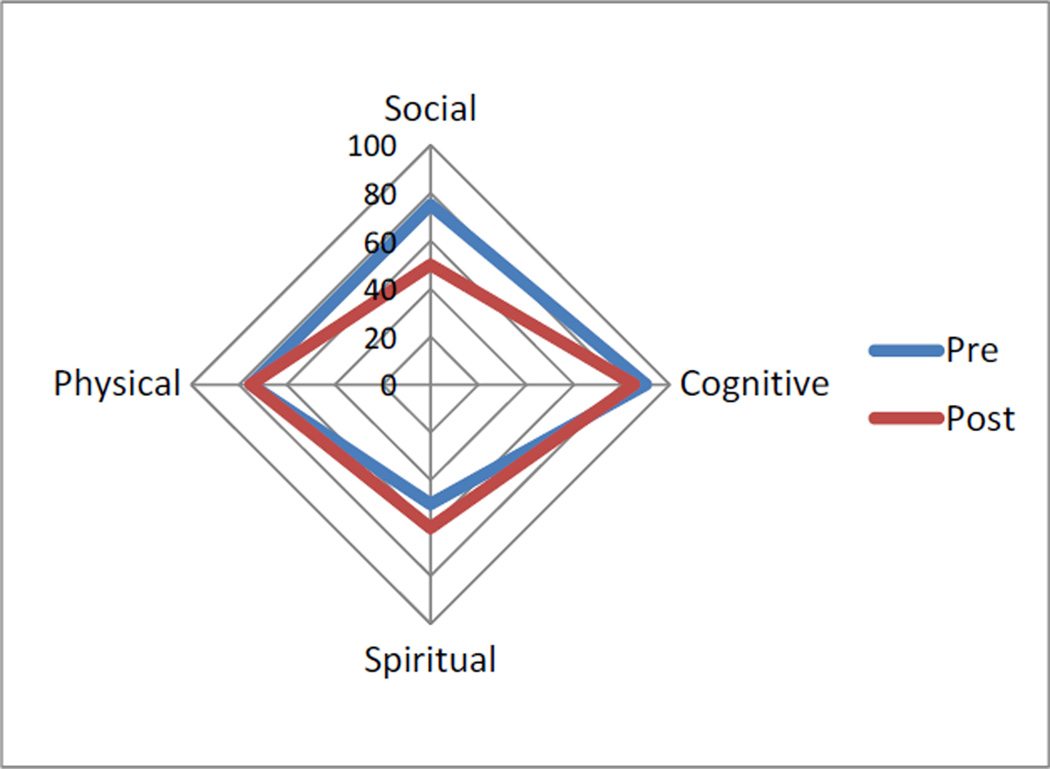
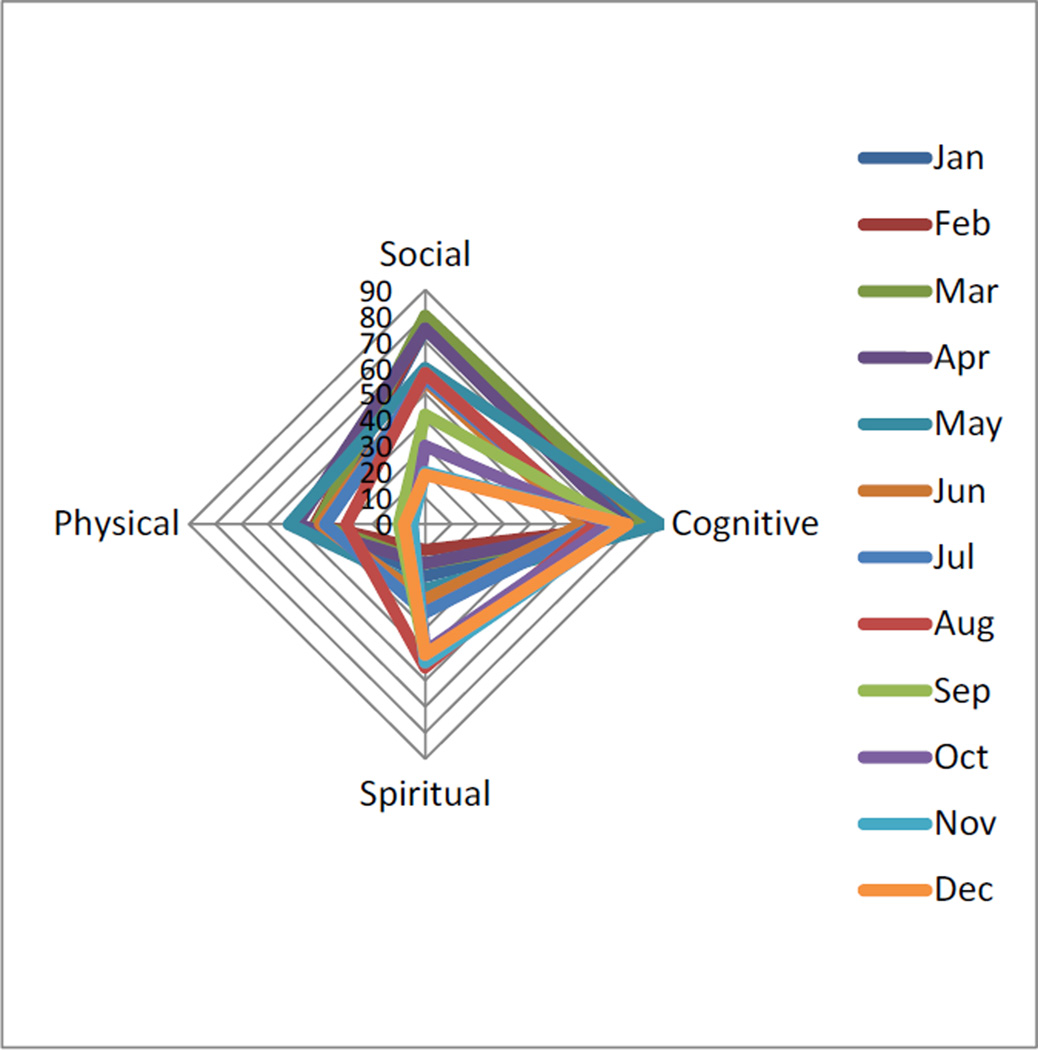
4.2 Visualisation technique 2 – Wellness Polygon
We developed the Wellness Polygon to provide a more cohesive interpretation of wellness. In particular, we wanted a visual display that represented the four components of wellness (social, cognitive, spiritual, and physical health) within a single figure. The display visualises data using a modified polygon. Each vertex of the polygon represents the four primary components of wellness. Values are plotted along each axis and connected to form a polygon. The scale along each axis ranges from zero to one-hundred for the possible normalised scores and the area of the polygon provides an overall measure of wellness. Depending on the values for each component of wellness, the shape of the polygon is distorted, either contracting or expanding to display shifts in health. Use of a polygonal display allows for a holistic interpretation of data. The visualisation directs perceptual focus towards the polygon as a whole rather than its individual components (Hughes and MacRae, 1994). This fits within our theoretical concept of wellness. The visualisation presents users with information as a complete unit, while still allowing for analysis at the component level. For example, a decrease in cognitive health distorts the visualisation into a skewed polygon. For longitudinal visualisation, we plotted data collected monthly as overlaid polygons. This visual display is perhaps less effective at presenting trends in wellness. Users are required to compare multiple polygons on a graph while referencing an extended legend. The cognitive load for this processing detracts from the visual presentation of data.
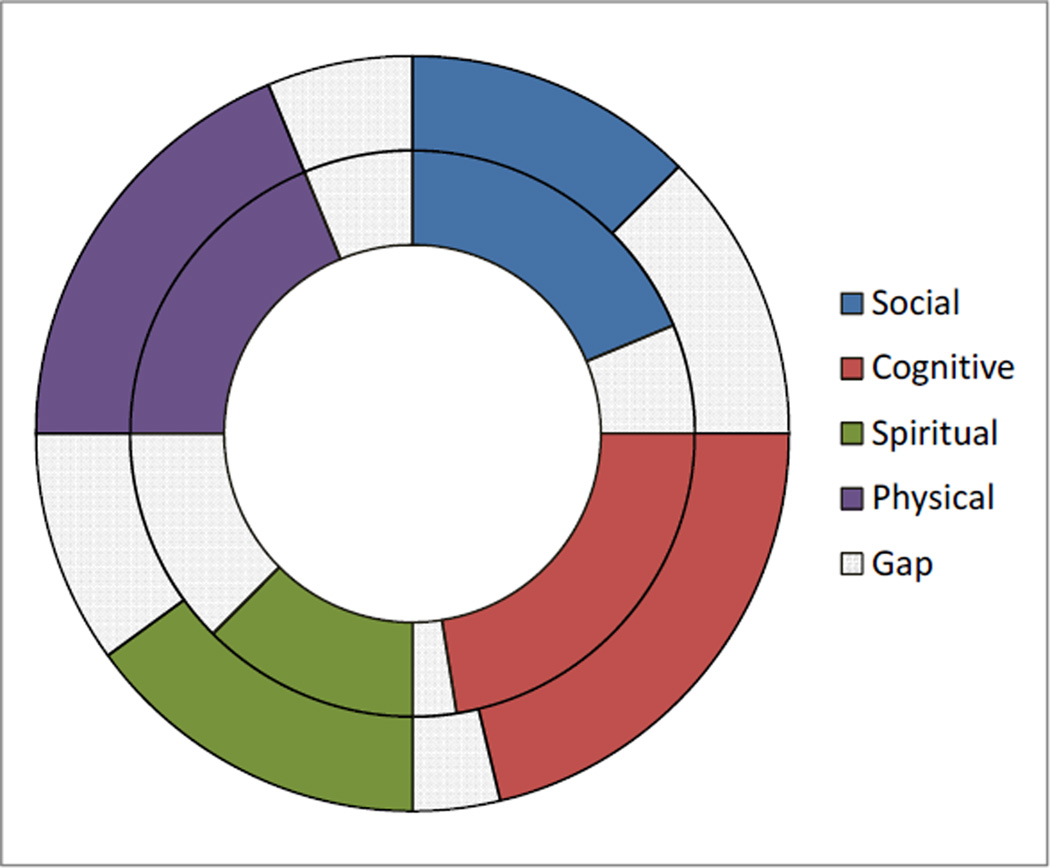
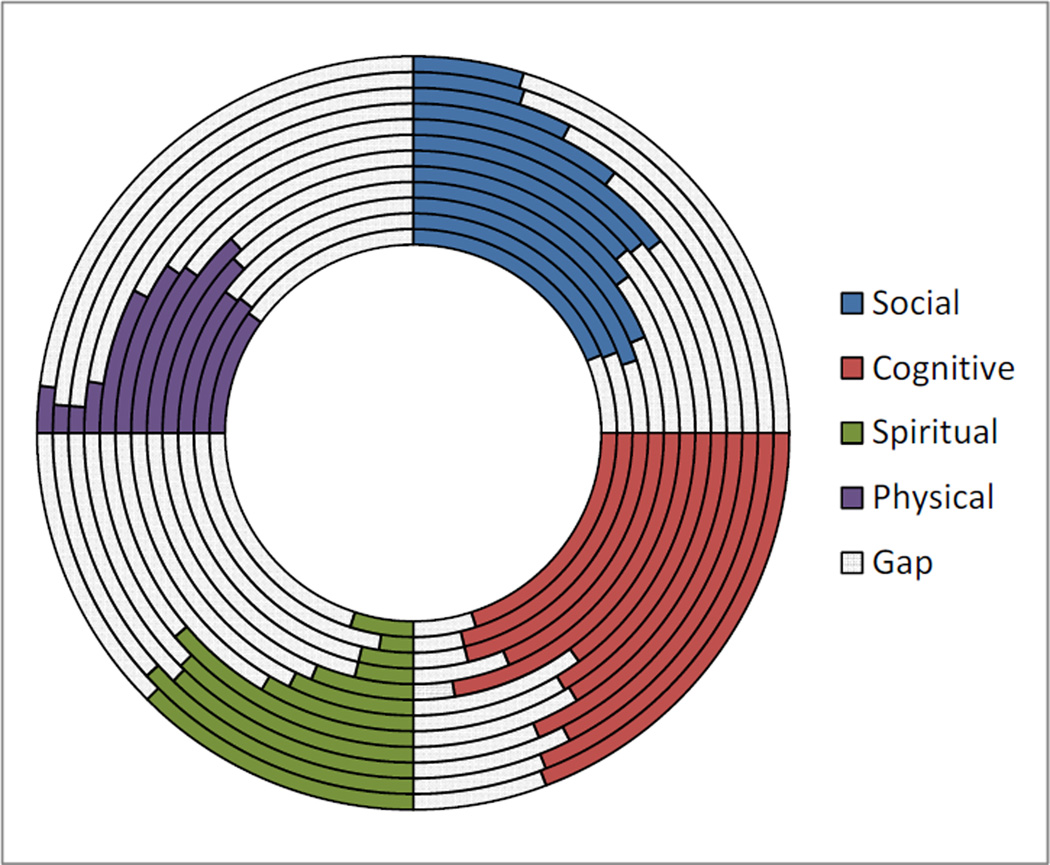
4.3 Visualisation technique 3 – partitioned donut
For the partitioned donut, we plotted data along a polar coordinate system divided into quadrants for each component of wellness. Each concentric ring of the visual display represents a different date for the data, with the oldest towards the centre, while the most recent at the outer ring of the display. To normalise for differences in sizes of the ring, each quadrant contained empty regions (or ‘gaps’) representing the remaining scores required to maximise at one-hundred.
In this visualisation, our goal was to enable easy understanding of changes in the subcomponents. Although this can negatively affect the holistic view of wellness, it may be more useful for monitoring a single component of interest. At the same time, this visualisation technique more clearly delineates the longitudinal changes in wellness state compared to the Wellness Polygon solution presented earlier. However, as each radial ring of the donut expands, the area also increases. Therefore, a comparison of two concentric rings in the donut may mislead users based on area of the filled regions, as opposed to an interpretation based on angular comparisons.
4.4 Comparison of visualisation techniques
We selected the visual displays in this section to emphasise different techniques for presenting integrated health information. We applied principles of cognitive design to minimise the cognitive load required to process information. These design approaches demonstrate the feasibility of incorporating multiple health measurements into a holistic visual display. From our design principles, the stacked bar charts provide a simple display of information that is familiar to most users. Comparisons are along a linear scale and it is possible to extend the display for longitudinal data. However, the stacks may detract away from an overall view of wellness, especially if the visualisation first draws users to differences along stacks. Comparisons across stacks involve increased cognitive load since the visualisation did not align stacks along a common scale (Cleveland and McGill, 1984). To provide a singular area of wellness display, we designed a visualisation that represented components of health as vertices along a polygon. The polygonal displays highlight overall shape and area of the graph as a measure of wellness. It is still possible for users to identify changes in components of health (as differences in the location of the vertices), though the purpose of this graph is to focus on the overall visual display of wellness. However, the polygonal display becomes limited when extended towards longitudinal comparisons. The overlaid polygons make it difficult to distinguish trends, and references to an extensive legend are cognitively distracting. The last visualisation technique presented in this article is the partitioned donut. This approach is similar to the Wellness Polygon in that each component of wellness has a dedicated quadrant in the image. By presenting the longitudinal data in a series of bands, this approach allows for the examination of trends in each component, an improvement over the polygon techniques, and is invariant to the loss component data, which can negatively affect the understanding of the stacked bar chart approach. Unfortunately, due to the distinct separation of components in the donut, the reading of the holistic view of wellness has a higher cognitive load than in either of the two other approaches described.
We developed the visualisations for three primary audiences: older adults, family members, and healthcare providers. This is a challenge since users may have different needs for data display. Older adults have recognised the potential of and expressed an interest in using health technology to monitor wellness (Demiris et al., 2011). The visualisation provides information at a broad level to display overall trends in wellness. Healthcare providers may require data at both the macro-level and at the micro-level when there are sudden shifts in health trends. It is possible that a single visual display will not fit the needs of both user groups. We developed these displays as early prototypes to demonstrate different techniques for combining health information. A continuous design cycle is needed to refine and assess the effectiveness of visual displays. Formative usability studies allow end users to provide feedback on early prototypes, which we can then reincorporate into the design of visual displays. We can follow-up with a summative usability study to evaluate the speed and accuracy of the visual displays. This addresses the effectiveness of different visual techniques at presenting longitudinal measures of wellness.
4.5 Limitations
We have demonstrated the feasibility of integrating multiple measures of health monitoring data into a holistic display of wellness. We also highlighted the challenges of presenting this visual information effectively for different audiences. Though our visualisations were guided by cognitive design principles, future work involves a full evaluation by older adults and clinicians that can provide objective feedback on our designs. This can provide insights on which elements of the visual displays were more salient for a given audience, how relevant users found the information, and how these visual displays can be incorporated within various applications.
5 Discussion
5.1 Integrating health information
We developed visualisation techniques to reduce the information overload of presenting multiple health measures. The design of our pilot study incorporated commercially available health technologies, which collected a wide range of measurements. We designed visual displays with a focus on integrating this information into a measure of holistic wellness. Older adults have a complex set of health needs; measuring only one component of health may be limiting. For example, both social isolation and cognitive decline have been found to affect physiological health, correlating with blood pressure, cortisol, and cholesterol levels (Sabbagh et al., 2007; Grant et al., 2009). An integrated view of wellness allows users to identify trends in overall health. This macro-level display allows both older adults and healthcare providers to quickly examine a highly detailed and complex data set. We can generalise the visual displays to incorporate further components of wellness, for example by adding stacks on the bar chart, vertices on the polygon, or sectors on the partitioned donut. This provides additional granularity for health information, while maintaining the representation of overall wellness through comparisons of length or area in the visual displays.
5.2 Applying visual displays
It can be possible to integrate the visual displays into different interfaces, providing greater flexibility for users. This can address differences in use case scenarios for the data across stakeholder groups. Users can select visual displays based on preference or need; for example, a focus on holistic wellness might employ the Wellness Polygon, while a focus on longitudinal trends would be more effective with a stacked bar chart or a partitioned donut. Allowing users the option to zoom in or out of a visualisation display and to specify a time range for the data display provide added levels of granularity. These visualisation techniques can be applied to mobile platforms, especially when there is a need to quickly examine data trends. Mobile healthcare, as described by Shieh et al. (2008), seeks to provide continuous access to patient health data. Challenges identified with mobile healthcare include integrating from multiple electronic health records and developing better display techniques. Effective visualisation techniques become important, especially if users have limited time and need a concise method to display multiple measures of health for a holistic measure of wellness.
It is also possible to use these visual displays for generating alerts within a user interface. If visual displays indicate sudden drops or significant changes in health data, it becomes important to provide notifications of this change. The visualisations can also highlight differences within the display to draw attention towards key changes. The information presented in the graphs can be used with a coaching tool for older adults. Social and behavioural interventions have been found to successfully improve physical health of older adults (Drewnowski and Evans, 2001; King, 2001; van der Bij et al., 2002). Notifications can suggest improvements, provide educational resources, or provide encouragement that are supported through visual displays of wellness.
5.3 Health data for decision support
A preliminary literature review has shown the impact of visual displays on decision making within health related fields. However, the literature has yet to address the effects of an integrated data visualisation technique for decision making of older adults and clinicians. We have presented several approaches to visualising wellness data focusing on integrated visualisation and changes in health status. This information can be leveraged by both older adults and clinicians for informed decision-making. With greater available personalised data, older adults are more aware of their own health status and are able to use this information to facilitate shared decision making with a physician or family member. A study analysing the role of independence and shared decision making within the context of smart home technology found that perceptions of these terms differed amongst user groups. Researchers and designers of the systems often identified shared decision making as linking educational information to the patient, while older adult users perceived it as active involvement and empowerment within the decision making process (Demiris, 2009). Development of health monitoring tools must recognise these differences in perceptions in order to reconcile the goals of the older adult user with that of the healthcare provider.
One possibility for the use of integrated health monitoring data could be for a personal health record (PHR). PHR systems can be potentially used in combination with or as an extension of monitoring technologies such as the ones used in our pilot study, allowing older adults and their families to store and process their own data supporting disease management efforts and/or communication with healthcare providers (Demiris and Thompson, 2011). Development of integrated visualisation techniques could provide critical tools to support shared decision making across stakeholder groups and a more efficient understanding of trends and trajectories over time. PHR systems supported by such data visualisation tools can therefore play a significant role in disease prevention and wellness promotion for older adults, which will be critical for public health.
6 Conclusions
This work explored diverse visualisation techniques to synthesise wellness parameters obtained from older adults in a community setting using diverse technologies. The resulting visualisation prototypes incorporate a theoretical visualisation framework and proven display techniques addressing the challenge of processing large and complex data sets while enabling a quick overview of trends and trajectories over time. These visual techniques are designed for a broad group of stakeholders (older adults, family members, and clinicians). Designing appropriate visualisations has proven to be a challenge, especially if different stakeholders have differing information needs. It is important to recognise the needs of different users within the development of visual displays; techniques of visualisation should address these needs while also understanding the intended goals of the displays. To further inform the design of our prototype visual displays, we will involve stakeholders in formative usability studies, which can be iteratively incorporated within our design process. Though this work is within the context of health monitoring technologies for older adults, the data visualisation techniques can be generalised for other applications involving data display. It becomes important to develop effective techniques of data visualisation as information technologies continually provide opportunities to gather large amounts of data. The abstraction of information into visual displays helps organise and communicate data. Efforts for data abstraction and visualisation such as the ones presented here can inform policies for data representation and dissemination features of integrated health systems. Without this abstraction of information, data can become complex and difficult to manage. The techniques described integrate multiple sources of health information into an effective visual display that can support decision making and provide facile detection of longitudinal trends.
Figure 1.
Comparison of pre and post data using a stacked bar chart (see online version for colours)
Figure 2.
Stacked bar chart extended for longitudinal data (see online version for colours)
Figure 3.
Comparison of pre and post data using the Wellness Polygon (see online version for colours)
Figure 4.
Comparison of Wellness Polygons across a 12-month period (see online version for colours)
Figure 5.
Comparison of pre and post data using a partitioned donut graphical display (see online version for colours)
Figure 6.
Extension of the partitioned donut visual display across 12 months (older data is on inner ring while newer data is on outer) (see online version for colours)
Biographies
Thai Le is a doctoral student in the division of Biomedical and Health Informatics in the School of Medicine at the University of Washington. His area of interest is data visualisation techniques to support older adult health.
Katarzyna Wilamowska is a post-doctoral fellow in the division of Biomedical and Health Informatics in the School of Medicine at the University of Washington. She completed her PhD in computer vision and medical applications from the Computer Science and Engineering Department at the University of Washington.
George Demiris is a Professor in Biomedical and Health Informatics, School of Medicine, and Biobehavioral Nursing and Health Systems, School of Nursing at the University of Washington. His research focuses on the use of information technology to improve quality of life for older adults. He is exploring the design and evaluation of ‘smart home’ applications that support older adults to remain independent and the use of telehealth technologies for home care and hospice patients and caregivers. He is Graduate Program Director of Biomedical and Health Informatics, and the Director of the Clinical Informatics and Patient Centered Technologies Program. He is also the Lead Convener of the Technology and Aging Special Interest Group of the Gerontological Society of America.
Hilaire Thompson is an Associate Professor in the department of Biobehavioral Nursing and Health Systems in the School of Nursing at the University of Washington. Her program of research has focused on preventing brain injury and testing interventions to improve outcome following injury. She served as the Editor of the American Association of Neuroscience Nursing’s Clinical Practice Guideline Series and is the chair of the Health Sciences Education section of the Gerontological Society of America.
Contributor Information
Thai Le, Email: tle23@uw.edu, Department of Biomedical Informatics and Medical Education, University of Washington, Box 357240, 1959 NE Pacific Street, HSB I-264, Seattle, WA 98195, USA.
Katarzyna Wilamowska, Email: kasiaw@uw.edu, Department of Biomedical Informatics and Medical Education, University of Washington, Box 357240, 1959 NE Pacific Street, HSB I-264, Seattle, WA 98195, USA.
George Demiris, Email: gdemiris@uw.edu, Department of Biomedical Informatics and Medical Education, University of Washington, Box 357240, 1959 NE Pacific Street, HSB I-264, Seattle, WA 98195, USA.
Hilaire Thompson, Email: hilairet@uw.edu, Biobehavioral Nursing and Health Systems, University of Washington, Box 357266, Seattle, WA 98195, USA.
References
- Alamantariotou K, Zisi D. Consumer health informatics and interactive visual learning tools for health. International Journal of Electronic Healthcare. 2010;Vol. 5(No. 4):414–424. doi: 10.1504/IJEH.2010.036211. [DOI] [PubMed] [Google Scholar]
- Alpass FM, Neville S. Loneliness, health and depression in older males. Aging & Mental Health. 2003;Vol. 7(No. 3):212–216. doi: 10.1080/1360786031000101193. [DOI] [PubMed] [Google Scholar]
- Cabarcos A, Sanchez T, Seoane JA, Aguiar-Pulido V, Freire A, Dorado J, Pazos A. Retrieval and management of medical information from heterogeneous sources, for its integration in a medical record visualisation tool. International Journal of Electronic Healthcare. 2010;Vol. 5(No. 4):371–385. doi: 10.1504/IJEH.2010.036208. [DOI] [PubMed] [Google Scholar]
- Campion EW. The oldest old. The New England Journal of Medicine. 1994;Vol. 330(No. 25):1819–1820. doi: 10.1056/NEJM199406233302509. [DOI] [PubMed] [Google Scholar]
- Carpenter PA, Shah P. A model of the perceptual and conceptual processes in graph comprehension. Journal of Experimental Psychology: Applied. 1998;Vol. 4(No. 2):75–100. [Google Scholar]
- Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing & Society. 2005;Vol. 25(No. 1):41–67. doi: 10.7748/nop.17.1.40.s11. [DOI] [PubMed] [Google Scholar]
- Chan M, Estève D, Escriba C, Campo E. A review of smart homes – present state and future challenges. Computer Methods and Programs in Biomedicine. 2008;Vol. 91(No. 1):55–81. doi: 10.1016/j.cmpb.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, Roth EA, Shekelle PG. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;Vol. 328(No. 7441):680. doi: 10.1136/bmj.328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleveland WS, McGill R. Graphical perception: theory, experimentation, and application to the development of graphical methods. Journal of the American Statistical Association. 1984;Vol. 79(No. 387):531–554. [Google Scholar]
- Cook DJ, Schmitter-Edgecombe M. Assessing the quality of activities in a smart environment. Methods of Information in Medicine. 2009;Vol. 48(No. 5):480–485. doi: 10.3414/ME0592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney KL. Privacy and senior willingness to adopt smart home information technology in residential care facilities. Methods of Information in Medicine. 2008;Vol. 47(No. 1):76–81. doi: 10.3414/me9104. [DOI] [PubMed] [Google Scholar]
- Demiris G. Electronic home healthcare: concepts and challenges. International Journal of Electronic Healthcare. 2004;Vol. 1(No. 1):4–16. doi: 10.1504/IJEH.2004.004655. [DOI] [PubMed] [Google Scholar]
- Demiris G. Independence and shared decision making: the role of smart home technology in empowering older adults. Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society; IEEE Engineering in Medicine and Biology Society; 2009. pp. 6432–6436. [DOI] [PubMed] [Google Scholar]
- Demiris G, Hensel BK. Technologies for an aging society: a systematic review of “smart home” applications. Yearbook of Medical Informatics. 2008:33–40. [PubMed] [Google Scholar]
- Demiris G, Rantz M, Aud M, Marek K, Tyrer H, Skubic M, Hussam A. Older adults’ attitudes towards and perceptions of “smart home” technologies: a pilot study. Medical Informatics and the Internet in Medicine. 2004;Vol. 29(No. 2):87–94. doi: 10.1080/14639230410001684387. [DOI] [PubMed] [Google Scholar]
- Demiris G, Thompson H. Smart homes and ambient assisted living applications: from data to knowledge-empowering or overwhelming older adults? IMIA Yearbook. 2011;Vol. 6(No. 1):51–57. [PubMed] [Google Scholar]
- Demiris G, Thompson HJ, Reeder B, Wilamowska K, Zaslavsky O. Using informatics to capture older adults’ wellness. [accessed on 7 April 2012];International Journal of Medical Informatics. 2011 doi: 10.1016/j.ijmedinf.2011.03.004. Available online at: http://dx.doi.org.offcampus.lib.washington.edu/10.1016/j.bbr.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Evans WJ. Nutrition, physical activity, and quality of life in older adults: summary. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001;Vol. 56(No. 2):89–94. doi: 10.1093/gerona/56.suppl_2.89. [DOI] [PubMed] [Google Scholar]
- Dunn HL. High-level wellness for man and society. American Journal of Public Health and the Nations Health. 1959;Vol. 49(No. 6):786–792. doi: 10.2105/ajph.49.6.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elting LS, Martin CG, Cantor SB, Rubenstein EB. Influence of data display formats on physician investigators’ decisions to stop clinical trials: prospective trial with repeated measures. BMJ. 1999;Vol. 318(No. 7197):1527–1531. doi: 10.1136/bmj.318.7197.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman-Stewart D, Brundage MD, Zotov V. Further insight into the perception of quantitative information: judgments of gist in treatment decisions. Medical Decision Making: An International Journal of the Society for Medical Decision Making. 2007;Vol. 27(No. 1):34–43. doi: 10.1177/0272989X06297101. [DOI] [PubMed] [Google Scholar]
- Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. American Journal of Preventive Medicine. 1999;Vol. 17(No. 4):285–294. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- Grant N, Hamer M, Steptoe A. Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 2009;Vol. 37(No. 1):29–37. doi: 10.1007/s12160-009-9081-z. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Alecxih L, Branch LG, Wiener JM. Medical and long-term care costs when older persons become more dependent. American Journal of Public Health. 2002;Vol. 92(No. 8):1244–1245. doi: 10.2105/ajph.92.8.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration. Projected Supply, Demand, and Shortages of Registered Nurses: 2000–2020. [accessed on 12 January 2011];2002 Available online at: http://www.ahcancal.org/research_data/staffing/Documents/Registered_Nurse_Supply_Demand.pdf. [Google Scholar]
- Helal S, Mann W, El-Zabadani H, King J, Kaddoura Y, Jansen E. The Gator Tech Smart House: a programmable pervasive space. Computer. 2005;Vol. 38(No. 3):50–60. [Google Scholar]
- Hoeke JO, Bonke B, van Strik R, Gelsema ES. Evaluation of techniques for the presentation of laboratory data: support of pattern recognition. Methods of Information in Medicine. 2000;Vol. 39(No. 1):88–92. [PubMed] [Google Scholar]
- Hughes T, MacRae AW. Holistic peripheral processing of a polygon display. Human Factors. 1994;Vol. 36(No. 4):645–651. doi: 10.1177/001872089403600406. [DOI] [PubMed] [Google Scholar]
- James BD, Schneider JA. Increasing incidence of dementia in the oldest old: evidence and implications. Alzheimer’s Research & Therapy. 2010;Vol. 2(No. 3):9. doi: 10.1186/alzrt32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RJ, Wolinsky FD. The structure of health status among older adults: disease, disability, functional limitation, and perceived health. Journal of Health and Social Behavior. 1993;Vol. 34(No. 2):105–121. [PubMed] [Google Scholar]
- King AC. Interventions to promote physical activity by older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001;Vol. 56(No. 2):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- Larkin JH, Simon HA. Why a diagram is (sometimes) worth ten thousand words. Cognitive Science. 1987;Vol. 11(No. 1):65–100. [Google Scholar]
- Loeb SJ, Penrod J, Falkenstern S, Gueldner SH, Poon LW. Supporting older adults living with multiple chronic conditions. Western Journal of Nursing Research. 2003;Vol. 25(No. 1):8–23. doi: 10.1177/0193945902238830. [DOI] [PubMed] [Google Scholar]
- Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. The New England Journal of Medicine. 2003;Vol. 349(No. 11):1048–1055. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- Morrow DG, Hier CM, Menard WE, Leirer VO. Icons improve older and younger adults’ comprehension of medication information. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1998;Vol. 53(No. 4):240–254. doi: 10.1093/geronb/53b.4.p240. [DOI] [PubMed] [Google Scholar]
- Naik AD, Schulman-Green D, McCorkle R, Bradley EH, Bogardus ST., Jr Will older persons and their clinicians use a shared decision-making instrument? Journal of General Internal Medicine. 2005;Vol. 20(No. 7):640–643. doi: 10.1111/j.1525-1497.2005.0114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinker S. A theory of graph comprehension. In: Freedle R, editor. Artificial Intelligence and the Future of Testing. Lawrence Erlbaum Associates Ltd; 1990. pp. 73–126. [Google Scholar]
- Rogowski J, Lillard LA, Kington R. The financial burden of prescription drug use among elderly persons. The Gerontologist. 1997;Vol. 37(No. 4):475–482. doi: 10.1093/geront/37.4.475. [DOI] [PubMed] [Google Scholar]
- Sabbagh MN, Lahti T, Connor DJ, Caviness JN, Shill H, Vedders L, Mahant P, Samanta J, Burns RS, Evidente VGH, Driver-Dunckley E, Reisberg B, Bircea S, Adler CH. Functional ability correlates with cognitive impairment in Parkinson’s disease and Alzheimer’s disease. Dementia and Geriatric Cognitive Disorders. 2007;Vol. 24(No. 5):327–334. doi: 10.1159/000108340. [DOI] [PubMed] [Google Scholar]
- Sagahyroon A, Raddy H, Ghazy A, Suleman U. Design and implementation of a wearable healthcare monitoring system. International Journal of Electronic Healthcare. 2009;Vol. 5(No. 1):68–86. doi: 10.1504/IJEH.2009.026273. [DOI] [PubMed] [Google Scholar]
- Shieh YY, Tsai FY, Anavim A, Shieh M, Wang MD, Lin C-MC. Mobile healthcare: the opportunities and challenges. International Journal of Electronic Healthcare. 2008;Vol. 4(No. 2):208–219. doi: 10.1504/IJEH.2008.019793. [DOI] [PubMed] [Google Scholar]
- Thompson HJ, Demiris G, Rue T, Shatil E, Wilamowska K, Zaslavsky O, Reeder B. A holistic approach to assess older adults’ wellness using e-health technologies. Telemedicine and e-Health. 2011;Vol. 17(No. 10):794–800. doi: 10.1089/tmj.2011.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Bij AK, Laurant MGH, Wensing M. Effectiveness of physical activity interventions for older adults – a review. American Journal of Preventive Medicine. 2002;Vol. 22(No. 2):120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]