Abstract
OBJECTIVES
To validate the recently described Mercy method for weight estimation in an independent cohort of children living in the United States.
METHODS
Anthropometric data including weight, height, humeral length, and mid upper arm circumference were collected from 976 otherwise healthy children (2 months to 14 years old). The data were used to examine the predictive performances of the Mercy method and four other weight estimation strategies (the Advanced Pediatric Life Support [APLS] method, the Broselow tape, and the Luscombe and Owens and the Nelson methods).
RESULTS
The Mercy method demonstrated accuracy comparable to that observed in the original study (mean error: −0.3 kg; mean percentage error: −0.3%; root mean square error: 2.62 kg; 95% limits of agreement: 0.83–1.19). This method estimated weight within 20% of actual for 95% of children compared with 58.7% for APLS, 78% for Broselow, 54.4% for Luscombe and Owens, and 70.4% for Nelson. Furthermore, the Mercy method was the only weight estimation strategy which enabled prediction of weight in all of the children enrolled.
CONCLUSIONS
The Mercy method proved to be highly accurate and more robust than existing weight estimation strategies across a wider range of age and body mass index values, thereby making it superior to other existing approaches.
INDEX TERMS: adolescent, body weight, child, developing countries, infant, life support
INTRODUCTION
In no other patient population is there more calculation and manipulation of drug doses than in children. The need to individualize pediatric doses introduces the potential for errors along the entire process of drug delivery, from prescribing and transcribing the dose to diluting, compounding, dispensing, and administering the final formulation.1–4 With most pediatric doses determined by body weight, interventions aimed at minimizing medication errors in children are rendered ineffectual if the patient's weight is incorrectly recorded or unavailable. In settings where obtaining a child's weight prior to treatment is simply not feasible (e.g., prehospital/hospital emergency settings, resource-constrained facilities in developing countries), the provision of age-appropriate, weight-based therapies remains a fundamental challenge.
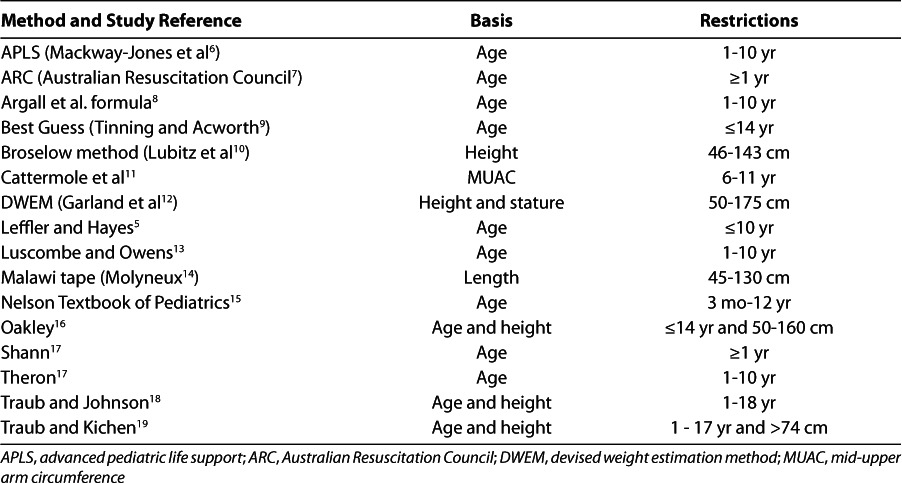
Apart from parental recall or provider estimation, the most commonly used strategies for estimating body weight rely on a child's age or length (Table 1).5–19 These single-parameter weight estimation methods can be simple and easy to integrate into clinical practice; however, most perform well in only a subset of the pediatric population. The utility of many of the methods are restricted to children meeting age or length criteria (Table 1); most methods overestimate weight in children who are underweight and underestimate weight in children who are overweight/obese,20 and several have been demonstrated to be less robust in children in whom race and ethnicity differ from the population in which the method was developed.14,17,21–23 Thus, there remains an unmet need for pediatric weight estimation strategies that are accurate across a broad range of ages, weights, heights, and statures in children of all nationalities.
Table 1.
Published Weight Estimation Methods
Recently, investigators at the Children's Mercy Hospital developed a weight estimation strategy (i.e., the Mercy method) that was designed to address limitations inherent in the existing weight estimation methods.20 The Mercy method incorporates anthropometric surrogates for both stature (humeral length [HL]) and body habitus (mid-upper arm circumference [MUAC]), which provides a more accurate estimate of weight than methods that rely on a single variable. It requires no subjective assessments and performs robustly, independently of age and height, over a broad range of weights. This method was developed and internally validated using a dataset of 19,266 children from the National Health and Nutrition Examination Survey (NHANES)24; however, there have been no prospective studies that have evaluated the method in an independent dataset. This study describes the external validation of the Mercy method in a cohort of children living in the midwestern United States.
MATERIALS AND METHODS
Subjects and Study Design
This was a prospective, single-center study of otherwise healthy children aged 2 months through 16 years, with constitutionally normal growth and development. Children were enrolled from the Children's Mercy Hospital (CMH), CMH-affiliated daycare centers, and CMH-sponsored family events between July 2009 and June 2011. Children with known or apparent limb deformities, those unable to be positioned for height/length measurements, and those with an underlying pathological condition or pharmacological management that could produce abnormal body composition for age (e.g., severe edema, chronic oral corticosteroid use) were ineligible for participation. All children were enrolled with informed parental permission and assent (if >7 years of age) under a protocol that was reviewed and approved by the Institutional Review Board at CMH.
Rater Training
All study personnel performing measurements (i.e., the principal investigator and seven certified clinical research coordinators) were required to undergo prequalification prior to their participation in the study. Raters performed each of the study-related anthropometric measurements in triplicate on a minimum of three other adult raters. Intra-rater variance was required to be less than 5% for each measure, and inter-rater concordance was required to exceed 90%. Raters failing initial prequalification were offered the opportunity for remediation, and those failing a second quality assessment (QA) were not permitted to participate in the study.
Data Collection
The anthropometric measurements collected included height, weight, HL, and MUAC. Children who could stand unassisted were positioned with their heels, buttocks, and head in contact with a wall or a height rule, and their height was measured using a traditional tape measure or a portable stadiometer. In infants unable to stand, recumbent (heel-to-crown) length was measured on an examining table using an infantometer or traditional tape measure. Each participant was weighed with as little outer clothing as possible, using a portable electronic scale that was calibrated daily. HL was measured from the upper edge of the posterior border of the acromion process to the tip of the olecranon process. MUAC was measured at the midpoint of the humerus with the arm hanging down at the child's side. Both limb measurements were taken on the child's right side using a standard vinyl tape measure and recorded to the nearest millimeter. Family members of participating children were given verbal instructions describing the location of the anatomic landmarks and asked to perform the same measurements in an attempt to assess whether care givers could reasonably obtain the data necessary to apply the Mercy method.
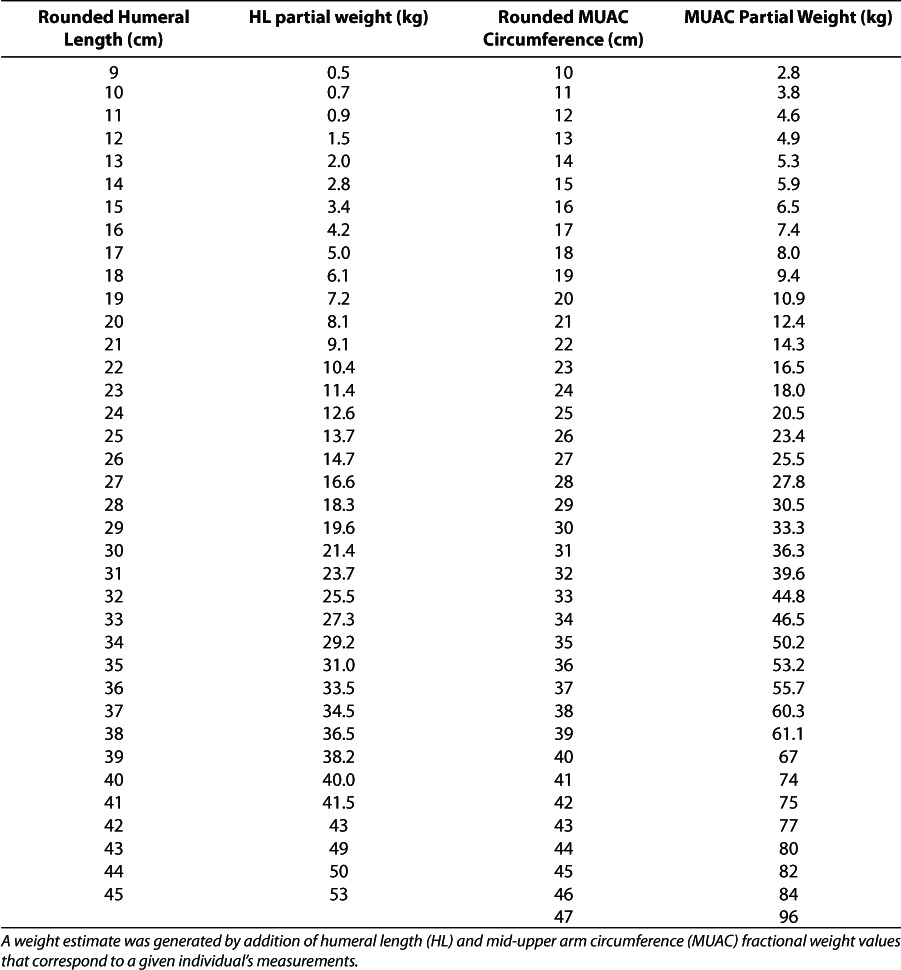
Data Analysis
The Mercy method was applied to HL and MUAC data as previously described.20 Briefly, both measures were rounded up or down to the nearest 1.0 cm, and the corresponding fractional weight was determined as shown in Table 2. Fractional weights for both measures were summed to generate an estimated weight for each participant child (e.g., an HL of 21.2 cm and an MUAC of 18.6 cm would correspond with fractional weights of 9.1 kg and 9.4 kg, respectively. Thus, the estimated weight of this child would be 18.5 kg). Four other commonly used weight estima tion strategies were also evaluated. Three calculate weight based on the child's age. The formula described by Advanced Pediatric Life Support (APLS) is (2 × [age in years + 4]).6 The methods in Nelson's Textbook of Pediatrics are (age in months + 9)/2 for children 3 to 12 months old; ([age in years × 2] + 8) for children 1 to 6 years old; and ([age in years × 7.5]/2) for children 7 to 12 years old.15 The method of Luscombe and Owens is (3 × [age] + 7).13 The Broselow tape (2007 edition B) was used to generate a weight estimate based on the child's length.
Table 2.
Fractional Weight Values for Humeral Length and Mid-Upper Arm Circumference Measures
The predicted weight of each child was compared to their observed weight, and the following parameters were generated: slope with 95% confidence interval (CI), intercept, Pearson correlation coefficient, and 95% limits of agreement (LOA). Mean error (ME) and mean percentage error (MPE) were calculated by taking the difference between predicted and actual weights for the former and dividing that value by the actual weight after multiplying ×100 to arrive at the latter. Root mean square error (RMSE) was calculated by taking the square root of the average squared error. Bland-Altman plots using log-transformed data were constructed to evaluate agreement between the various weight estimation methods and the observed weight. Concordance between raters and parents was determined by simple linear regression. Reliability between raters as determined by the prequalification measurements was assessed using the intraclass correlation coefficient (ICC). All mathematical and statistical analyses were performed with Excel 2003 (Microsoft) and SPSS version 12 software. The significance limit established for all statistical analyses was α = 0.05.
RESULTS
A total of 976 children were enrolled in this study by one of eight different raters. The pediatric participants were equally distributed by sex (49% male, 51% female) and averaged 6.2 ± 3.4 years, 25.4 ± 14.7 kg, 115.8 ± 25 cm, and 17.6 ± 3.5 kg/m2 for age, weight, height, and body mass index (BMI), respectively. BMI percentile for a majority of children (60%) was classified “normal” as defined by the US Centers for Disease Control, followed by obese (12.3%), overweight (12.1%), and underweight (3%). The remaining 12.6% of children fell into the “infant” category. Study raters consisted of 1 pharmacist, 5 registered nurses, 1 certificate nurse, and 1 non-health care provider, the latter 7 of whom were Certified Clinical Research Coordinators. Family member raters ranged in age from 7 to 69 years old and consisted of parents (88.2%), grandparents (6.0%), siblings (2.9%), other first-degree relatives (1.9%), and others (0.9%).
Accuracy of the Mercy method in this independent cohort of children was comparable to that of findings of the original internal validation dataset, although the LOA were broader in the current investigation (Table 3).20 Performance of each weight estimation strategy in the current population is shown in Figure 1. As illustrated, there is less scatter around the line of unity and tighter limits of agreement for the Mercy method than for the other weight estimation methods that were evaluated. Moreover, the Mercy method was the only weight estimation strategy able to predict a weight for every child enrolled in this investigation (Figure 1). Segregation of the data by BMI percentile category highlights the consistent performance of the Mercy method across BMI. In contrast, the APLS, Broselow, Luscombe and Owens, and Nelson methods tended to overestimate weight in children who are underweight and underestimate weight in children that are overweight and obese (Figure 2).
Table 3.
Performance of the Mercy Method, Overall and by Rater
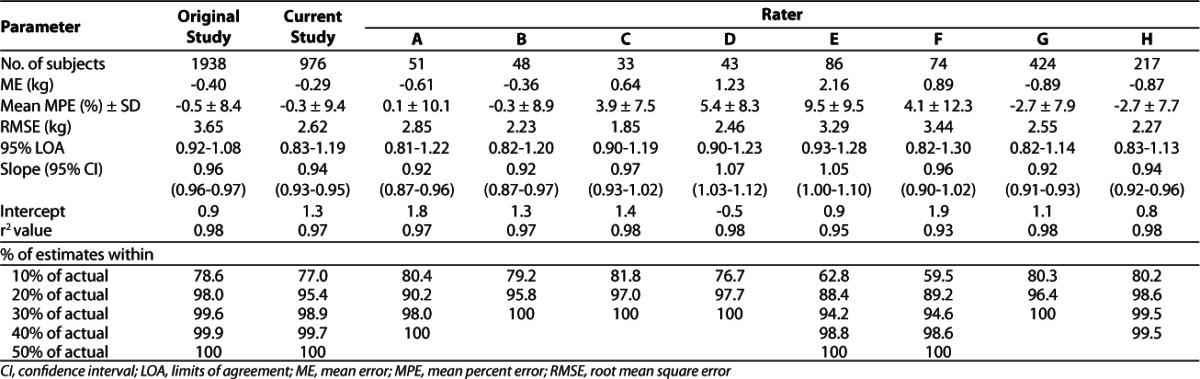
Figure 1.
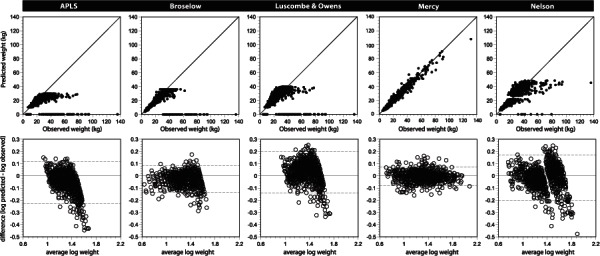
Observed Versus Predicted Weights for Weight Estimation Methods Evaluated in this Study
(Upper panels) Values that fall on the x-axis indicate individuals for whom no weight could be calculated because length and/or age exceeded the bounds of the estimation method. (Lower panels) Bland-Altman plots depicting the log-transformed difference between predicted weight and observed weight versus average log weight for the children in this external validation data set. Dashed lines depict the 95% limits of agreement.
Figure 2.
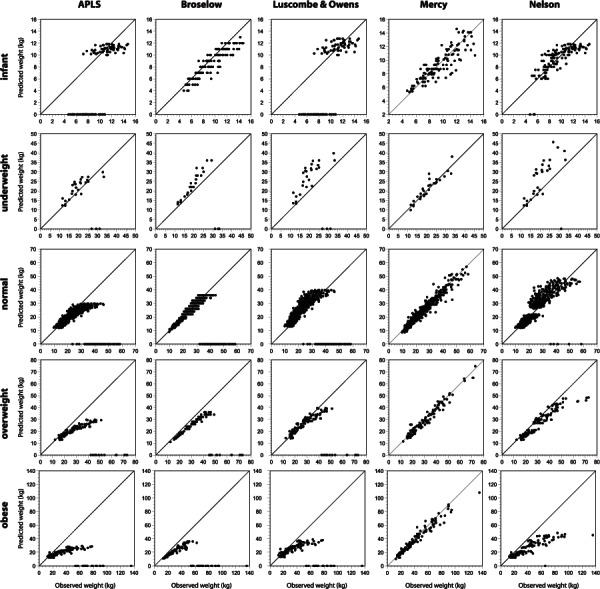
Observed Versus Predicted Weights by BMI Percentile Category for the Weight Estimation Methods Evaluated in this Study
In total, the Mercy method estimated weight within 10% of the child's actual weight in 77% of the population (Table 3). This is compared to 34.4% for APLS, 53.5% for Broselow, 29.7% for Luscombe and Owens, and 43% for Nelson. The Mercy method estimated weight to within 20% of actual for nearly all of the children who were evaluated (95%) compared with 58.7% for APLS, 78% for Broselow, 54.4% for Luscombe and Owens and 70.4% for Nelson.
Although estimates of inter-rater reliability determined during the prestudy QA sessions were excellent as measured by an ICC of 0.99, rater performance during the actual study varied (Table 2). Concordance between family members and study raters for measures of HL and MUAC was good (Figure 3), although predictive performance with family rater-generated measurements was lower than that observed for the study rater-generated measurements (ME: −2.2, MPE: −7.7 ± 14.4, RMSE: 3.4). Data derived from family members demonstrated higher rates of under-prediction than that from study raters (Figure 3) and with only 42% and 80% of estimates within 10% and 20% of actual, respectively.
Figure 3.
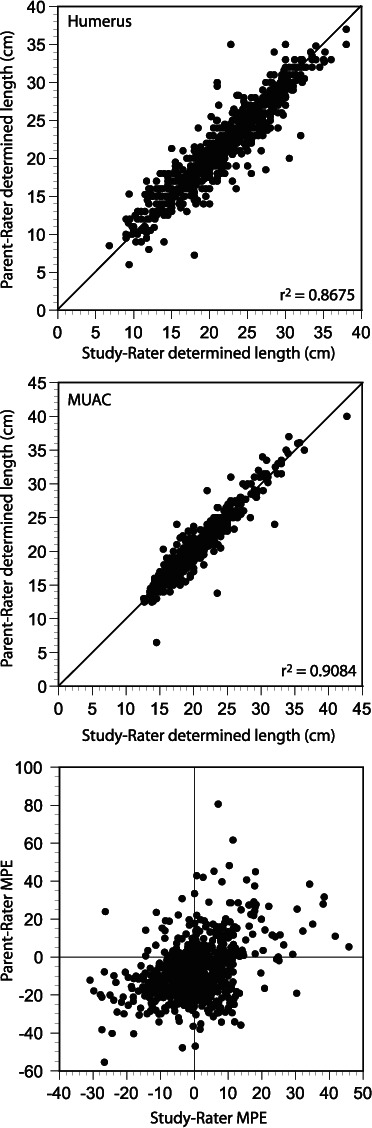
Concordance Between Humeral Length (upper) and Mid-Upper Arm Circumference (middle) Determinations Made by Study Staff Versus Family Members of the Study Participants
(Lower) Percent variance in weight (predicted-observed) estimated using the Mercy method for data from study raters versus family raters.
DISCUSSION
Health care providers in emergency and resource-constrained settings continue to rely on weight estimation to facilitate the delivery of age-appropriate therapies. Although published weight estimation strategies demonstrate value in these settings, they are also accompanied by well-known limitations. The accuracy of these methods 1) decreases with increasing age, 2) substantially decreases in children at the extremes of weight, and 3) varies in children of different racial and ethnic backgrounds.8–10,13,17,21,22,25–32 Those few methods that offer improvements in accuracy over expanded age ranges (e.g., Traub-Johnson18 and Traub-Kichen19) require the user to solve more complicated exponential equations.
The Mercy method appears to address many of these limitations as reflected by the data from the present study, which corroborate the earlier findings that this method is accurate over a broad range of ages and body compositions.20 We did observe broader limits of agreement than were reported in the original study. This may have been due, in part, to training that was less rigorous than that received by the NHANES staff, resulting in slight differences in the designation of anatomic landmarks by our study raters. The fact that this was not reflected by inter-rater agreement in the prestudy QA sessions also suggests that the intermittent nature of enrollment by some of the study raters (reflected by the imbalance in enrollment numbers [Table 2]) could have limited the opportunity to refine their measurement technique. Notably, the level of anatomical knowledge accompanying raters who were health care professionals did not appear to convey greater accuracy in weight determination with the Mercy method compared to our trained non-clinician rater (Table 3, rater H), who did not have a background in pharmacy or nursing.
As expected, predictive performance of the Mercy method was lower in family member raters who were given only brief verbal instructions before performing the measurements. Nonetheless, the data binning strategy used by the Mercy method was able to compensate for the lack of familiarity with anatomic landmarks such that family member raters predicted weight within 20% of actual for the majority (80%) of children in this study. While we did not examine the reliability of the weight estimates from our family raters as a function of educational level, it is reasonable to speculate that societal and cultural differences might occur. Consequently, more detailed instruction may need to accompany materials for performing the Mercy method in remote communities wherein community members are relied upon to perform basic health care functions. Importantly, the Mercy method performed no worse in the hands of family members than did the other weight estimation methods in the hands of trained study raters.
Two of the four weight estimation methods selected for comparison in this study, the APLS and Nelson equations, were selected because they derive from resources, which are readily available to pediatric practitioners. The other two methods (i.e., Broselow and Luscombe and Owens) were selected because they experience considerable use in emergency settings. Regardless, the Mercy method outperformed each of these methods with 1) limits of agreement that were narrower, 2) broader age and length ranges over which weight could be estimated, 3) less bias across BMI percentiles, and 4) a larger proportion of children predicted within 10% to 20% of their actual weight. Notably, the differences we observed between the Mercy method and the other weight estimation methods reflect a more conservative difference than would have been observed had we been able to enroll a greater proportion of adolescents in this study, a population for which larger estimates of bias in methods other than the Mercy method are typically observed. The population of eligible children presenting to CMH during the course of the current study was weighted heavily toward preteens, thereby restricting the number of children available for evaluation at the upper age limit of the Mercy method (16.9 years old).
The Mercy method appears to be a simple weight estimation strategy that performs robustly across the continuum of pediatric ages and weights. However, closer inspection of the findings by BMI percentile group suggests a wider degree of bias in the infant population than with children >2 years of age, regardless of BMI. In these patients, a refinement of the Mercy method to include different surrogates of girth and stature may be required. Additional studies of the Mercy method in populations that are older (i.e., >12 years old) and composed of a higher proportion of children who are underweight, overweight, or obese should confirm the findings presented herein.
The clinical relevance associated with the Mercy method resides primarily with its accuracy and relative ease of use. A method that predicts body weight within 10% and 20% of actual in most children should have profound impact on the efficacy and safety of weight-based drug doses. Moreover, a reliable weight estimation method that can be easily adopted by community health care workers in parts of the developing world, where scales for weighing children do not exist, could do much to improve the treatment of serious diseases that claim the lives of countless infants and children each year (e.g., tuberculosis, human immunodeficiency virus infection, malaria). Ongoing studies evaluating the Mercy method in India, West Africa, and China will further delineate the role of the Mercy method in children of various ethnic and geographic origin.
ACKNOWLEDGMENTS
We extend sincere appreciation to Connie Aubin, Kathy Vandiver, RN, Katherine Collum, RN, Allison Gardner, RN, MSN, and Mandy Day for assisting with the successful execution of this study.
ABBREVIATIONS
- APLS
advanced pediatric life support
- ARC
Australian Resuscitation Council
- BMI
body mass index
- CI
confidence interval
- DWEM
devised weight estimation method
- HL
humeral length
- ICC
intraclass correlation coefficient
- LOA
limits of agreement
- ME
mean error
- MPE
mean percentage error
- MUAC
mid-upper arm circumference
- NHANES
National Health and Nutrition Examination Survey
- QA
quality assessment
- RMSE
root mean square error
Footnotes
DISCLOSURES The Children's Mercy Hospital (CMH) has filed a patent on the Mercy method, which is currently pending with the US Patent Office. CMH will own the patent if awarded, and all of the authors are employed by CMH. S.M.A.-R. had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis.
REFERENCES
- 1.Glover ML, Sussmane JB. Assessing pediatric residents' mathematical skills for prescribing medication: a need for improved training. Acad Med. 2002;77(10):1007–1010. doi: 10.1097/00001888-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Potts MJ, Phelan KW. Deficiencies in calculation and applied mathematics skills in pediatrics among primary care interns. Arch Pediatr Adolesc Med. 1996;150(7):748–752. doi: 10.1001/archpedi.1996.02170320094016. [DOI] [PubMed] [Google Scholar]
- 3.Madlon-Kay DJ, Mosch FS. Liquid medication dosing errors. J Fam Pract. 2000;49(8):741–744. [PubMed] [Google Scholar]
- 4.Cousins D, Clarkson A, Conroy S, Choonara I. Medication errors in children—an eight year review using press reports. Paediatr Perinat Drug Ther. 2002;5(2):52–58. [Google Scholar]
- 5.Leffler S, Hayes M. Analysis of parental estimates of children's weights in the ED. Ann Emerg Med. 1997;30(2):167–170. doi: 10.1016/s0196-0644(97)70137-9. [DOI] [PubMed] [Google Scholar]
- 6.Mackway-Jones K, Molyneux E, Phillips B, Wieteska S. Advanced Paediatric Life Support. London: BMJ Books; 2001. [Google Scholar]
- 7.Advanced Life Support Committee of the Australian Resuscitation Council. Paediatric advanced life support—the Australian resuscitation council guidelines. Med J Aust. 1996;165:199–206. doi: 10.5694/j.1326-5377.1996.tb124926.x. [DOI] [PubMed] [Google Scholar]
- 8.Argall JA, Wright N, Mackway-Jones K, Jackson R. A comparison of two commonly used methods of weight estimation. Arch Dis Child. 2003;88(9):789–790. doi: 10.1136/adc.88.9.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tinning K, Acworth J. Make your best guess: an updated method for paediatric weight estimation. Emerg Med Australas. 2007;19(6):535–541. doi: 10.1111/j.1742-6723.2007.01026.x. [DOI] [PubMed] [Google Scholar]
- 10.Lubitz D, Seidal JS, Chameides L. A rapid method for estimating weight and resuscitation drug dosages from length in the pediatric age group. Ann Emerg Med. 1988;17(6):576–581. doi: 10.1016/s0196-0644(88)80396-2. et al. [DOI] [PubMed] [Google Scholar]
- 11.Cattermole GN, Leung PYM, Maka PSK. Mid-arm circumference can be used to estimate children's weights. Resuscitation. 2010;81(9):1105–1110. doi: 10.1016/j.resuscitation.2010.05.015. et al. [DOI] [PubMed] [Google Scholar]
- 12.Garland JS, Kishaba RG, Nelson DB. A rapid and accurate method for estimating body weight. Am J Emerg Med. 1986;4(5):390–393. doi: 10.1016/0735-6757(86)90184-1. et al. [DOI] [PubMed] [Google Scholar]
- 13.Luscombe M, Owens B. Weight estimation in resuscitation: is the correct formula still valid? Arch Dis Child. 2007;92(5):412–415. doi: 10.1136/adc.2006.107284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molyneux E, Brogan R, Mitchell G, Gove S. Children's weights: guess or measure by tape? Lancet. 1999;354(9190):1616. doi: 10.1016/S0140-6736(99)04552-3. [DOI] [PubMed] [Google Scholar]
- 15.Needlman RD. The first year. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson Textbook of Pediatrics. 17th ed. Philadelphia: WB Saunders; 2004. p. 31. In. eds. [Google Scholar]
- 16.Oakley PA. Inaccuracy and delay in decision making in paediatric resuscitation, and a proposed reference chart to reduce error. Br Med J. 1988;297(6652):817–819. doi: 10.1136/bmj.297.6652.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Theron L, Adams A, Jansen K, Robinson E. Emergency weight estimation in Pacific Island and Maori children who are large-forage. Emerg Med Australas. 2005;17(3):238–243. doi: 10.1111/j.1742-6723.2005.00729.x. [DOI] [PubMed] [Google Scholar]
- 18.Traub SL, Johnson CE. Comparison of methods of estimating creatinine clearance in children. Am J Hosp Pharm. 1980;37(2):195–201. [PubMed] [Google Scholar]
- 19.Traub SL, Kichen L. Estimating ideal body mass in children. Am J Hosp Pharm. 1983;40(1):107–110. [PubMed] [Google Scholar]
- 20.Abdel-Rahman SM, Ridge AL. An improved pediatric weight estimation strategy. Open Med Dev J. 2012;4:87–97. [Google Scholar]
- 21.Varghese A, Vasudevan VK, Lewin S. Do the length-based (Broselow) tape, APLS, Argall and Nelson's formulae accurately estimate weight of Indian children? Indian Pediatr. 2006;43(10):889–894. et al. [PubMed] [Google Scholar]
- 22.Ramarajan N, Krishnamoorthi R, Strehlow M. Internationalizing the Broselow tape: how reliable is weight estimation in Indian children. Acad Emerg Med. 2008;15(5):431–436. doi: 10.1111/j.1553-2712.2008.00081.x. et al. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen K, Krieser D, Kerr D. Failed validation of the Argall weight formula for estimating children's weight in an Australian emergency department. Acad Emerg Med. 2007;14(5):486–488. doi: 10.1197/j.aem.2006.12.009. et al. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. National Health and Nutrition Examination survey: questionnaires, datasets, and related documentation. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed September 12, 2012. [Google Scholar]
- 25.Krieser D, Nguyen K, Kerr D. Parental weight estimation of their child's weight is more accurate than other weight estimation methods for determining children's weight in an emergency department? Emerg Med J. 2007;24(11):756–759. doi: 10.1136/emj.2007.047993. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Black K, Barnett P, Wolfe R, Young S. Are methods used to estimate weight in children accurate? Emerg Med. 2002;14(2):160–165. doi: 10.1046/j.1442-2026.2002.00311.x. [DOI] [PubMed] [Google Scholar]
- 27.Casey J, Borland M. Best guess method: a further external validation study and comparison with other methods. Emerg Med Australas. 2010;22(1):68–74. doi: 10.1111/j.1742-6723.2009.01258.x. [DOI] [PubMed] [Google Scholar]
- 28.Thompson M, Reading M, Acworth J. Best guess method foe age-based weight estimation in paediatric emergencies: Validation and comparison with current methods. Emerg Med Australas. 2007;19(6):535–542. doi: 10.1111/j.1742-6723.2007.01031.x. [DOI] [PubMed] [Google Scholar]
- 29.Hofer CK, Ganter MT, Tucci M. How reliable is length-based determination of body weight and tracheal tube size in the paediatric age group? The Broselow tape reconsidered. Br J Anaesth. 2002;88(2):283–285. doi: 10.1093/bja/88.2.283. et al. [DOI] [PubMed] [Google Scholar]
- 30.Jang HY, Shin SD, Kwak YH. Can the Broselow tape be used to estimate weight and endotracheal tube size in Korean children? Acad Emerg Med. 2007;14(5):489–491. doi: 10.1197/j.aem.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 31.DuBois D, Baldwin S, King WD. Accuracy of weight estimation methods for children. Pediatr Emerg Care. 2007;23(4):227–230. doi: 10.1097/PEC.0b013e31803f5aca. [DOI] [PubMed] [Google Scholar]
- 32.Vilke GM, Marino A, Fisher R, Chan TC. Estimation of pediatric patient weight by EMT-PS. J Emerg Med. 2001;21(2):125–128. doi: 10.1016/s0736-4679(01)00354-7. [DOI] [PubMed] [Google Scholar]


