Abstract
Study Objectives:
To investigate whether sleep disturbances are bidirectionally related to anxiety and depression, and thus identify potential risk factors for each problem.
Design:
A systematic review was conducted on 9 studies (8 longitudinal, 1 retrospective) that assessed bidirectionality between a sleep disturbance, and anxiety or depression. Treatment studies were excluded, along with those solely based on clinical samples or cohorts at high risk of suffering from a sleep disturbance, anxiety and depression. Eligible studies were identified by searching PubMed, PsychINFO, Embase, and Scopus databases, and reference lists of eligible studies. Publication dates ranged from the beginning of each database to December 2011.
Measurements and Results:
Syntheses of longitudinal studies suggested insomnia and sleep quality were bidirectionally related to anxiety and depression, and depression/anxiety, respectively. Childhood sleep problems significantly predicted higher levels of depression and a combined depression/anxiety variable, but not vice-versa. A one-way relationship was found where anxiety predicted excessive daytime sleepiness, but excessive daytime sleepiness was not associated with depression.
Conclusions:
Definitive conclusions regarding bidirectionality cannot be made for most sleep disturbances due to the small number and heterogeneity of cohort samples used across studies. Nevertheless, best available evidence suggests insomnia is bidirectionally related to anxiety and depression. Clinical and theoretical implications are discussed.
Citation:
Alvaro PK; Roberts RM; Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. SLEEP 2013;36(7):1059-1068.
Keywords: Anxiety, depression, insomnia, sleep disturbances, systematic review
INTRODUCTION
Sleep disturbances encompass various potentially overlapping symptoms and disorders including insomnia, hypersomnia, excessive daytime sleepiness, circadian rhythm disturbance, and extrinsic sleep disorders (related to insufficient sleep and sleep hygiene). Sleep disturbances, anxiety and depression are common problems that lead to neuropsychological impairment,1–3 alcohol and drug abuse,4 and suicidal ideation.5–7 Recent studies have established high comorbidity rates between sleep disturbances (such as insomnia, narcolepsy, sleep apnea, and circadian rhythm complaints), and depression and anxiety,8–10 rates which vary across different anxiety disorders.11 Longitudinal associations have also been established between sleep disturbances, anxiety, and depression.12,13 Nevertheless, the etiological relationship between these problems remains unclear. Understanding the etiological relationship could help determine whether the onset of one is a risk-factor for the onset of the others, and inform public health campaigns and clinical interventions for each disorder.11,14,15
Research on bidirectionality can achieve such goals. Bidirectionality is established by accounting for the base rate of outcome variables,16 considering whether a sleep disturbance independently predicts the onset of anxiety or depression, and whether anxiety or depression independently predicts the onset of a sleep disturbance.
Various studies have found a bidirectional relationship between sleep disturbances, anxiety and depression, suggesting that each contribute to the development and are a consequence of one another.14,15,17 Other studies have suggested the existence of two distinct cause-effect associations, where anxiety predicts a sleep disturbance and a sleep disturbance predicts depression, but not vice-versa.11,18 The inconsistent nature of the research may relate to variations of sleep disturbances that have been assessed across studies. The statistical significance and magnitude of the relationship between sleep disturbances, anxiety and depression differs across sleep and mental health variables (anxiety and depression),18–21 which in turn may affect the results of bidirectionality studies. The current study, therefore, presents a systematic review that aims to determine whether a variety of sleep disturbances are risk factors for the development of anxiety or depression, and whether anxiety or depression are risk factors for the development of sleep disturbances.
METHODS
Data Sources and Study Selection
An extensive search of PubMed, PsychINFO, Embase, and Scopus was conducted using the following search terms in combinations specified for each database: (anxiety OR anxious* OR phobic OR phobia* OR psychological stress OR stress OR stresses OR internalization OR internalization OR obsessive compulsive OR asthenia OR depression OR depress* OR depressive disorder OR dysthym* OR seasonal affective disorder OR rumination) AND (sleep initiation and maintenance disorders OR sleep* OR insomnia OR early awakening OR early waking OR non-restorative OR non-restorative OR night waking). The Embase and Scopus searches also included the following terms to account for the large number of search hits: NOT (neoplasm OR cancer OR tumor OR tumour OR carcinoma* OR oncolog* OR ‘cardiovascular disease’ OR dementia* OR Alzheimer* OR parksinson* OR therapy' OR ‘psychiatric treatment’ OR medicat* OR treatment). Publication dates for the searches ranged from the beginning of each database to December 2011, and all searches were limited to English and human studies. The Reference lists of retrieved studies were also assessed for other citations.
Studies were eligible if the following criteria was met: (1) Study assessed any sleep disturbance; (2) Study assessed an anxiety or depression variable; (3) Study reported a significance test when assessing bidirectionality; (4) Study accounted for baseline/previous sleep, anxiety or depression variable. Based on the recommendations of Jansson-Frojmark and Lind-blom,15 treatment studies, along with those who solely included clinical samples or cohorts at high risk of suffering from a sleep disturbance, anxiety, and depression were excluded due to the potential bias towards a stronger association between sleep disturbances, anxiety, and depression. The inclusion/exclusion criteria were developed by the primary author and reviewed by the secondary author.
Quality Assessment
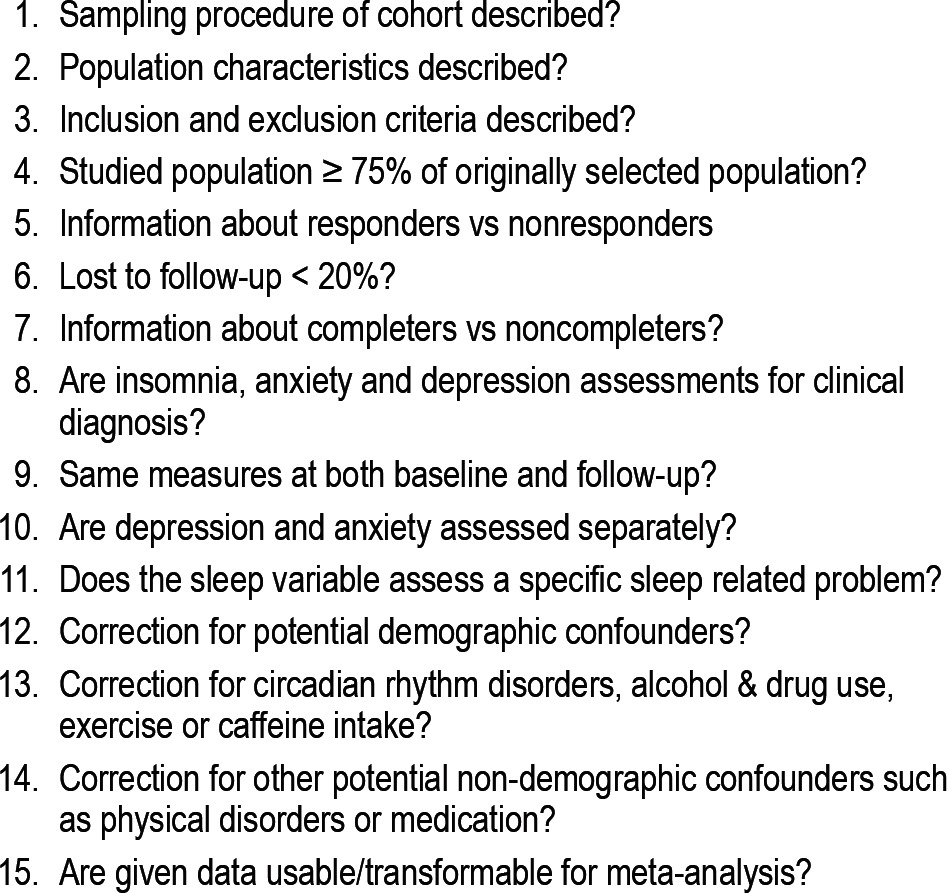
The methodological quality of the eligible studies was assessed by the first author who used a modified version of a 15-item checklist from a recent meta-analysis (Table 1).22 Items 10 and 11 were included because the nature and magnitude of associations between sleep disturbances, anxiety, and depression often differs across sleep and mental health variables.18–21 Sleep disturbances, anxiety and depression have been found to be associated with demographic information (e.g., age and gender),23,24 circadian rhythm disorders,25–27 alcohol and drug use,4,28 exercise,29,30 and caffeine,31–33 thus providing the rationale behind items 12 and 13. Each item was labelled with a (+) or (-), depending on whether the study satisfied the criterion or not. A cutoff score was not used as a reference for quality because such methods assign equal importance to all criteria. However, items were not weighted: the Cochrane Collaboration recommend against this method due to difficulties in justifying the weights assigned to each item.34 Instead, quality was assessed along a continuum that ranged from 0-15, where lower scores indicated lower quality and higher scores indicated higher quality.
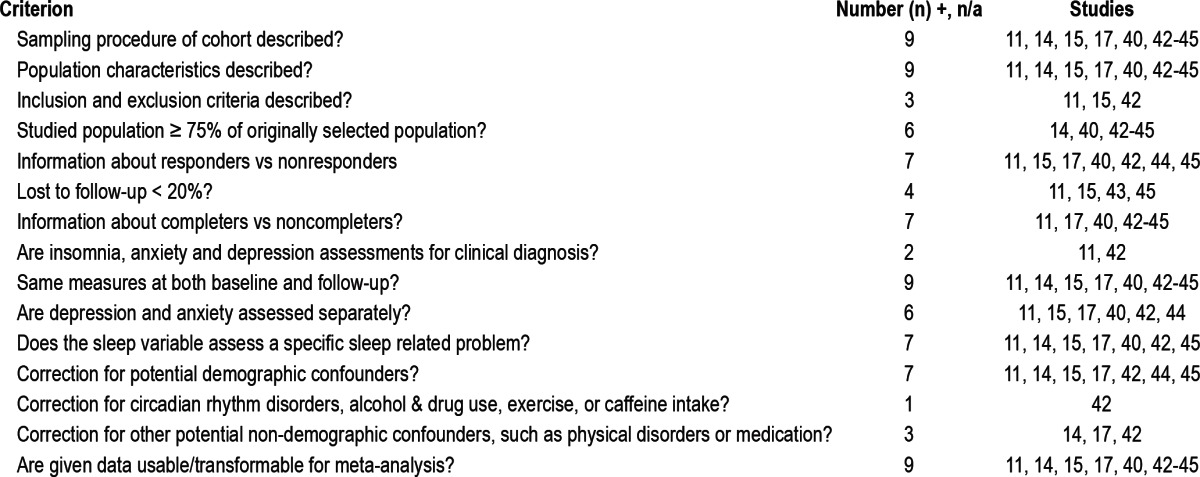
Table 1.
Items for quality assessment
Data Extraction and Synthesis
A coding form was developed to extract the following data from each study: geographical location of the study, sample size at baseline and follow-up, response rate, method of participant recruitment, method of data collection, use of medication, study methodology, possible biases, prediction and outcome variables, demographic statistics at baseline and (when available) follow-up, descriptive statistics for the variables of sleep disturbance, anxiety and depression, statistical analyses, variables controlled for, results, interpretation of results, author(s)' conclusions, and cited articles that were potentially relevant. Data extraction was conducted by the first author.
A meta-analysis could not be conducted due to the heterogeneous characteristics of the studies that met the inclusion criteria. Therefore, the research questions were analyzed by two narrative syntheses. The first presented an overall representation of the findings from each study, whereas the second compared results across different sleep variables.
RESULTS
Included and Excluded Studies
The PubMed, PsychInfo, Embase, and Scopus database searches identified 2,273, 2,352, 1,252, and 2,664 studies, respectively, and one study was identified from the reference searches. Ninety-three studies were selected as potentially relevant following the application of the inclusion criteria to the titles and abstracts. Most articles were excluded because they did not assess bidirectionality. Five studies13,35–38 assessed bidirectionality but not between a sleep disturbance and anxiety or depression; one study assessed bidirectionality but used a cohort that was at risk for sleep disturbances, anxiety, and depression39; and one study did not report a significance test when assessing bidirectionality.18 Therefore, 10 studies were eligible for analysis in the systematic review (12% of the original articles). Two eligible studies contained identical samples40,41 and hence were collapsed into 1, leaving 9 independent studies that were included in the systematic review (refer to Figure 1 for a representation of the database searches and summary of the reasons for exclusion). Eligibility of each study was assessed by the first author.
Figure 1.
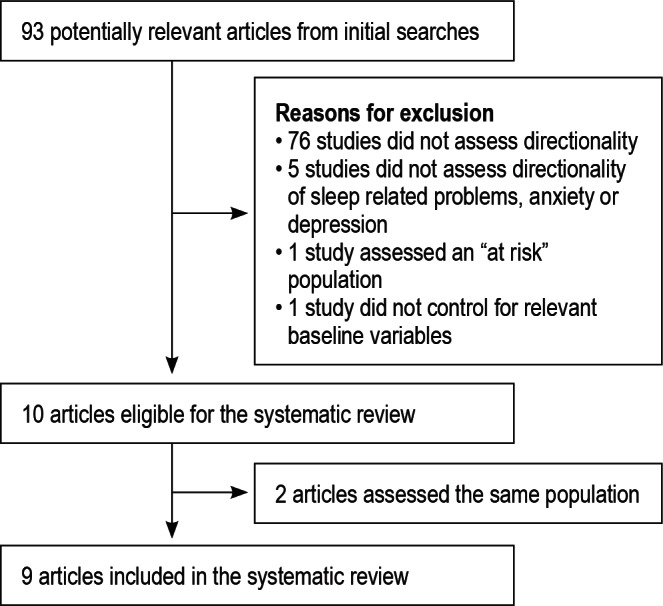
Summary of the reasons for exclusion.
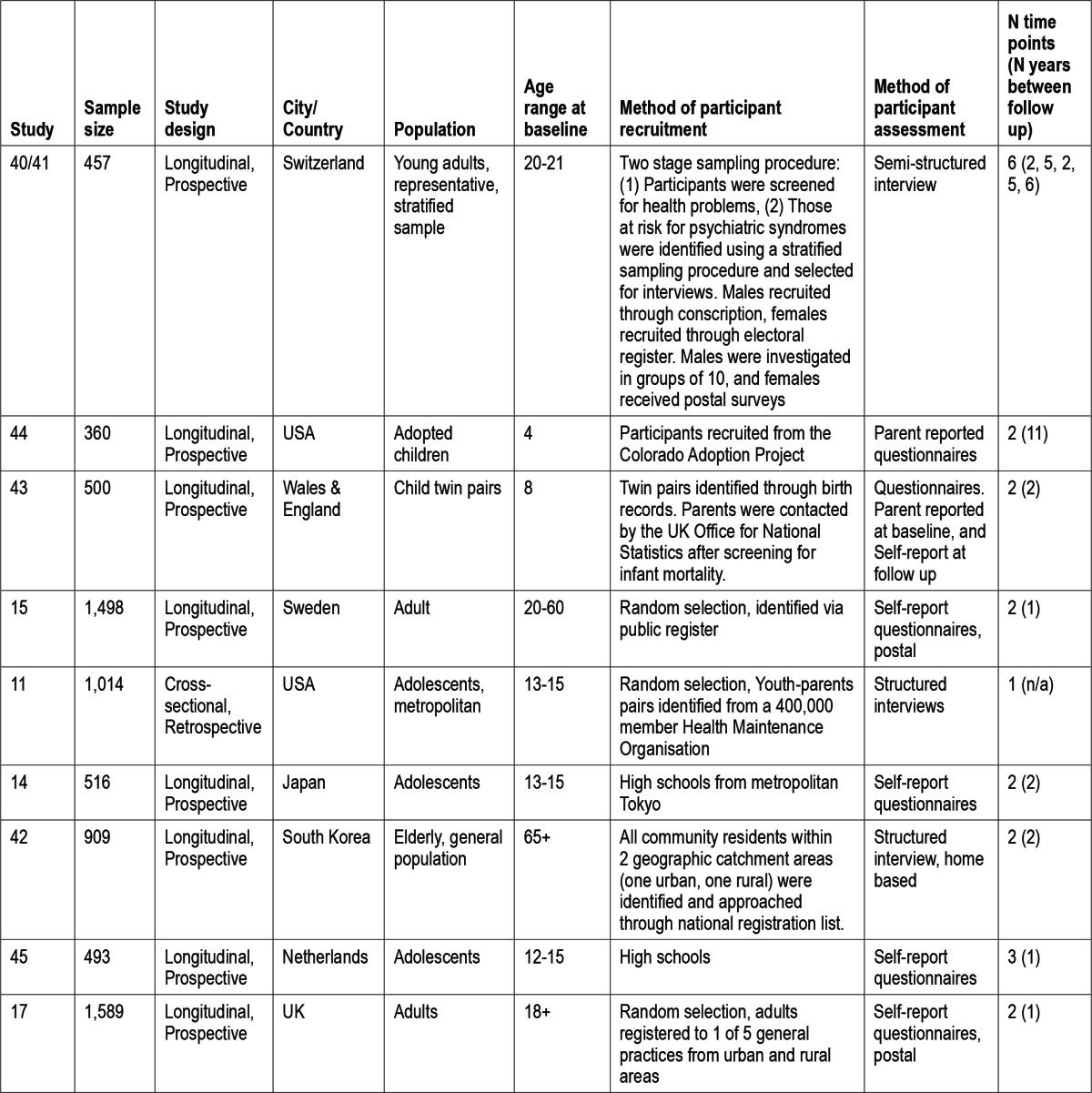
Table 2 displays the general characteristics of each study. All studies were conducted between 2002 and 2010; 8 were longitudinal and prospective, and the other study was retrospective and cross-sectional. Studies were set in various countries; 2 in the USA, 2 in the UK, and 1 each in Switzerland, Sweden, Japan, South Korea, and the Netherlands. Sample populations also differed across studies; adolescents were assessed by 3 studies, adults by 2, and young adults, the elderly, child twin pairs, and adopted children were assessed by 1 study each. Participants were recruited by random selection in 3 studies, high schools in 2, and a 2-stage sampling procedure, the Colorado adoption agency, birth records, and a national registrations list of all community residents were used in 1 study each. Participants were recruited by self-report questionnaires in 4 studies (2 were postal surveys), interviews in 3 (2 were structured and 1 was semi-structured), parent reported questionnaires in 1, and parent reported and self-reported questionnaires in 1 study.
Table 2.
General Characteristics of Each Study Included in the Systematic Review
Quality Assessment
Study quality ratings ranged from 7 to 13 (M = 9.9, SD = 1.9). All studies described the sampling procedure and population characteristics, used the same measures at baseline and follow-up, and gave data useable for a meta-analysis. Seven studies compared responders to non-responders and completers to non-completers, assessed a specific sleep disturbance, and corrected for potential demographic confounders; 6 studies retained 75% of the originally selected population and assessed depression and anxiety separately; 4 studies lost more than 20% of participants at follow-up; 3 studies described the inclusion and exclusion criteria, and corrected for other potential non-demographic confounders such as physical disorders; 2 studies assessed insomnia, anxiety, and depression according to a clinical diagnosis; 1 study corrected for alcohol and exercise; and no study corrected for circadian rhythm disorders, drug use, or caffeine intake (Table 3).
Table 3.
Amount of studies (n) that met each criterion of quality assessment
Overall Synthesis
Table 4 presents the data for the overall synthesis. Four of the 9 independent studies supported the bidirectional theory,14,15,17,42 2 of which assessed insomnia, anxiety, and depression,15,17 1 assessed insomnia and depression,42 and 1 assessed insomnia and mental health status.14 The unidirectional theory discussed above was supported by 3 studies.11,43,44 One study found 2 one-way relationships where anxiety predicted insomnia and insomnia predicted depression but not vice-versa11; the other reported that childhood sleep problems predicted depression but not vice-versa43; and the last suggested that childhood sleep problems predicted higher levels of depression/anxiety, but not vice-versa.44 However, this does not necessarily support the unidirectional theory discussed above, as the mental health variable that was used (depression/anxiety) assessed anxiety and depression as a single construct rather than separate variables.
Table 4.
Main findings from each study
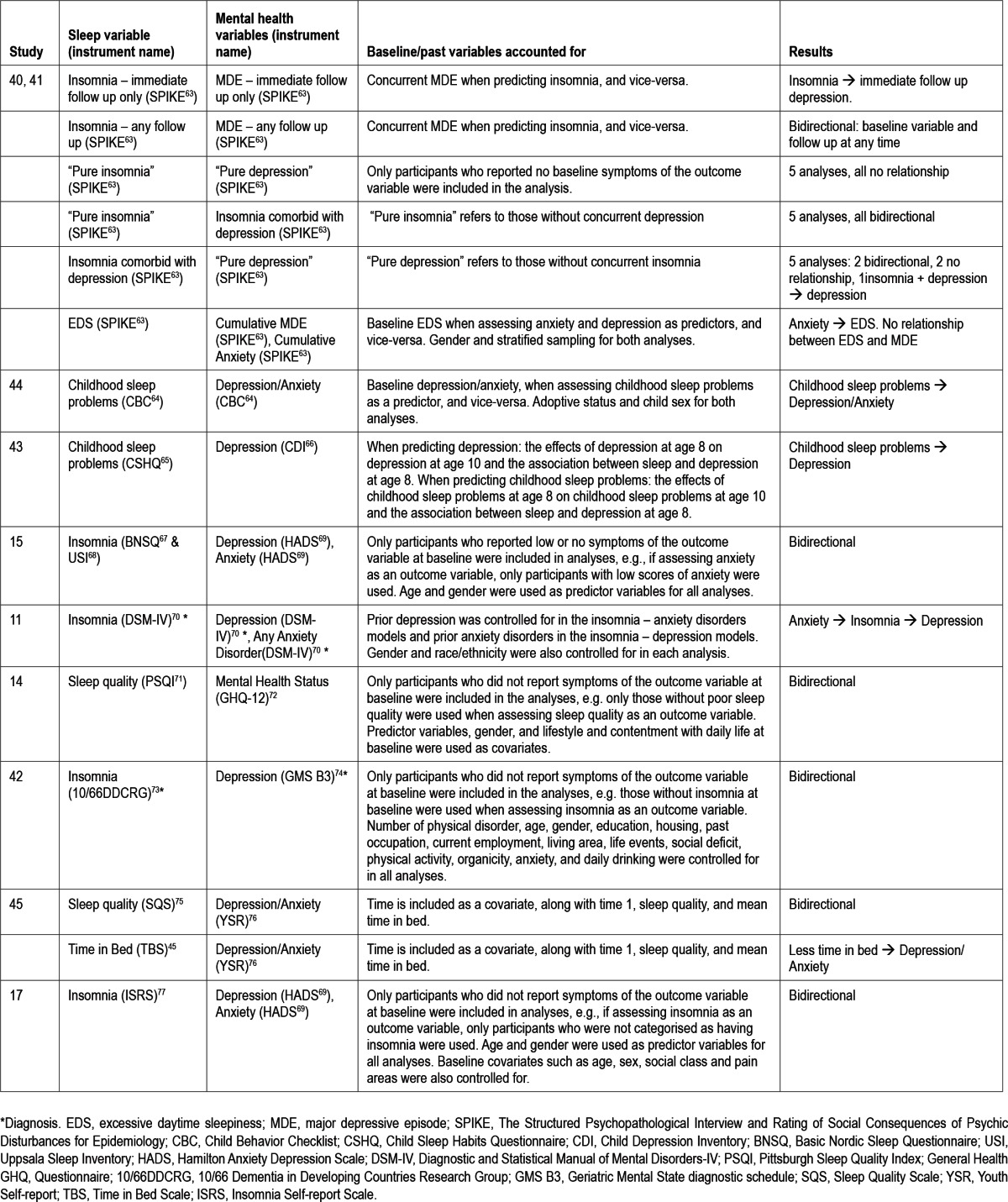
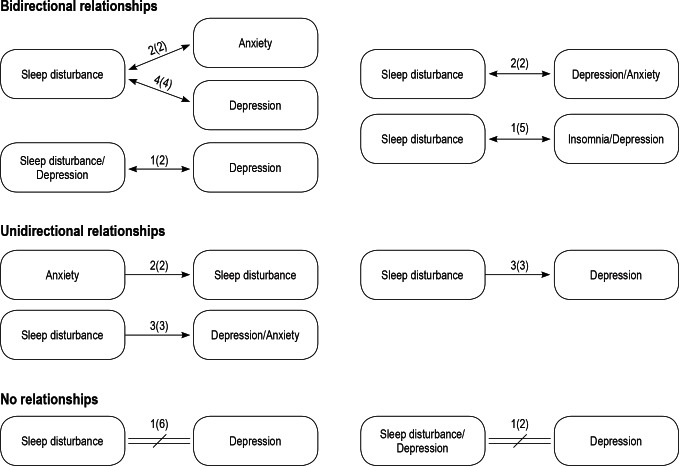
Two independent studies reported mixed results.40,41,45 One study found no relationship between excessive daytime sleepiness and major depressive episodes or “pure insomnia” (insomnia without concurrent depression) and “pure depression” (depression without concurrent insomnia), a bidirectional relationship between insomnia and major depressive episodes, and a one-way relationship where anxiety predicted excessive daytime sleepiness.40,41 The other found a bidirectional relationship between sleep quality and depression/anxiety and a one-way relationship between time in bed and depression/anxiety, where less time in bed at baseline predicted higher levels of depression/anxiety, but not vice-versa.45 Therefore, 6 independent studies supported the bidirectional theory,14,15,17,40–42,45 5 supported a unidirectional relationship,11,40,41,43–45 and 1 study did not find a significant relationship between excessive daytime sleepiness and major depressive episodes or “pure insomnia” and “pure depression.”40,41 Figure 2 depicts the number of studies and analyses that supported each type of relationship.
Figure 2.
Summary of the total number of studies (analyses) that supported each type of relationship between sleep disturbances, anxiety and depression.
Synthesis of Sleep Variables
Insomnia was the most commonly assessed sleep variable,11,15,17,40,42 followed by childhood sleep problems,43,44 sleep quality,14,45 excessive daytime sleepiness,41 and time in bed (Table 5).45 Studies that assessed bidirectionality between anxiety, depression, and other common sleep disturbances such as sleep apnea were not found.
Table 5.
Comparison of study findings between sleep variables
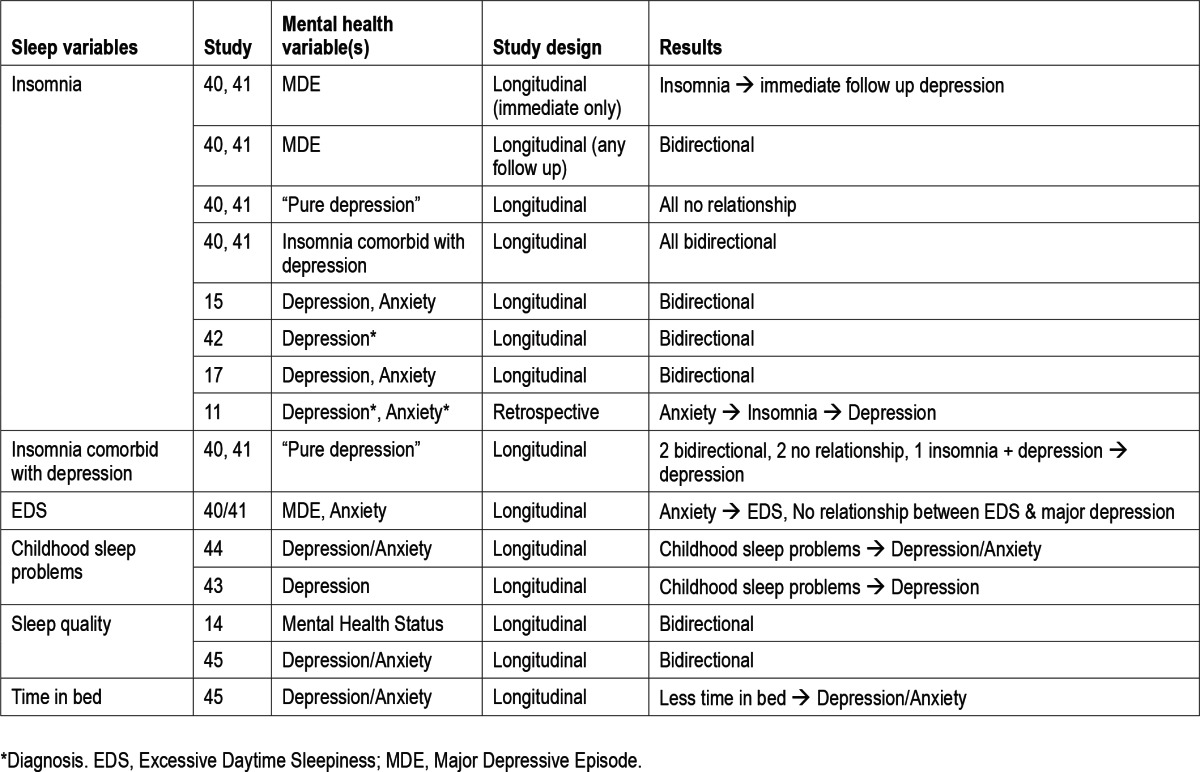
For insomnia, 3 of the 5 studies supported the bidirectional theory.15,17,42 One study supported the unidirectional theory, where anxiety disorders predicted insomnia, which predicted major depressive disorder.11 The remaining independent study reported several analyses across 6 time points over 20 years. No relationship was found in either direction between “pure insomnia” and “pure depression,” along with a bidirectional relationship between insomnia and insomnia comorbid with depression across 5 separate bidirectional analyses over 20 years.40 The same study also found conflicting results across these 5 analyses when assessing bidirectionality between “pure depression” and insomnia comorbid with depression (2 bidirectional relationships, a one-way relationship where insomnia comorbid with depression predicted pure depression but not vice-versa, and 2 relationships where no association was found in either direction). Finally, insomnia without concurrent depression predicted the development of depression at the interview directly following baseline and interviews at any given follow-up, whereas depression without concurrent insomnia predicted insomnia at the interview at any given time-point only.40
Regarding sleep quality, both studies found a bidirectional relationship, one with depression/anxiety45 and the other with mental health status (a variable that contains a depression/anxiety scale).14 Childhood sleep problems predicted depression and depression/anxiety but not vice-versa.43,44 One study found that less time in bed at baseline is associated with more severe symptoms of depression/anxiety at follow-up, but not vice-versa.45 Finally, one study found a one-way relationship where anxiety predicted excessive daytime sleepiness, but no relationship between excessive daytime sleepiness and depression (i.e., excessive daytime sleepiness did not predict depression and vice-versa).41
DISCUSSION
Each study included in the systematic review reported at least one significant relationship between a sleep disturbance, anxiety and/or depression, which further consolidates the notion of an association between these problems.8,23,44 Interestingly, one study41 found that anxiety predicted later excessive daytime sleepiness but no relationship between excessive daytime sleepiness and major depressive disorder symptoms, suggesting that a bidirectional relationship is not consistent across mental health problems. This is surprising given the overlap of abnormalities in neurotransmitters and brain structures involved in problems with the sleep wake cycle, anxiety, and depression,46–53 but Hasler and colleagues41 suggested that the association between excessive daytime sleepiness and depression may be mediated by sleep disorder symptoms and co-morbid anxiety. More studies are needed to draw a definitive conclusion on whether excessive daytime sleepiness, anxiety, and depression are bidirectionally related.
Best available evidence suggests that insomnia is bidirectionally related to anxiety and depression. One retrospective study reported a one-way relationship where anxiety predicted depression, but not vice-versa.11 Conversely, four longitudinal studies found a bidirectional relationship between insomnia, anxiety and/or depression.15,17,40,54 Due to the retrospective nature of, and hence the memory bias apparent in retrospective methodology,55 longitudinal study designs allow for more accurate causal inferences and reliable assessment of bidirectionality, and are therefore the preferred methodology for bidirectional studies.14
Interestingly, insomnia could predict depression more consistently than depression predicts insomnia. Buysse and colleagues40 assessed bidirectionality over a 20-year period across six time-points. They found consistent bidirectional relationships between “pure insomnia” and insomnia comorbid with depression, yet conflicting relationships between “pure depression” and insomnia comorbid with depression. Such results suggest that insomnia at baseline is a stronger and more persistent predictor of follow-up depression than baseline depression is of follow-up insomnia.
Various types of mechanisms may explain the bidirectional association between insomnia, anxiety and depression. Common neurobiological underpinnings (i.e., neurotransmitters and brain structures, discussed above) have been associated with insomnia, anxiety, and depression.46–53 Batterham and colleagues56 hypothesize there may also be biological factors such as increased inflammatory dysregulation in response to sleep disturbances57 that are associated with anxiety58 and depression.59 Three other potential mechanisms discussed by Kaneita and colleagues,14 which may coexist, include common factors (e.g., genetic, familial, social, or environmental) that independently contribute to the development of insomnia, anxiety and depression; insomnia, anxiety, and depression may be related, in which only the order of appearance of symptoms may alter; and insomnia, anxiety, and depression may be independent, but mutually influencing disorders.
A definitive conclusion is difficult to make regarding whether sleep disturbances, anxiety, and depression are bidirectionally related. Firstly, the small number of studies that assessed each sleep disturbance variable prevents an accurate representation of the true relationship between sleep disturbances, anxiety, and depression. Further longitudinal studies are needed to understand whether there is a bidirectional relationship between sleep disturbances, anxiety, and depression.
Secondly, sleep disturbance variables that were assessed by the studies in this systematic review were limited and sometimes problematic. Prevalent sleep disorders such as obstructive sleep apnea and circadian rhythm sleep disorders were not investigated, while insomnia symptoms such as problems with sleep latency, nighttime awakenings, and daytime functioning deficits as a result of sleep were incorporated in the definition of sleep quality14,45 and childhood sleep problems.43,44 The definition of childhood sleep problems also incorporated other sleep disturbances such as nightmares, sleep duration, overtiredness, bedtime resistance, sleep anxiety, parasomnias, sleep disordered breathing, and daytime sleepiness. Therefore, implying differences in findings across sleep variables is problematic because distinctions between sleep variables are obscured and the definition of childhood sleep problems was overly inclusive. Future bidirectionality studies should focus on a broader range of clearly defined sleep disturbances that contain reasonable conceptual overlap.
Variables of anxiety and depression were also sometimes defined using conceptually overlapping and overly inclusive variables, along with non-diagnostic self-report questionnaires, and may variably reflect current diagnostic criteria. Such cases include a combined depression/anxiety variable, which assessed depression and anxiety as one construct. These inventories could mask potential differences in bidirectionality across variables, and are problematic because bidirectional inferences cannot be made about the relationship between sleep disturbances. Indeed, only two studies assessed diagnosed insomnia, anxiety, and depressive disorders.11,42 Future studies should refrain from using overly inclusive variables, and use definitions based on established diagnostic criteria.
Moreover, bidirectionality between anxiety, depression, and different types of insomnia symptoms (i.e., sleep onset insomnia, early morning awakening) was not assessed. Recent studies have suggested that the association between insomnia, anxiety and depression may differ across specific insomnia symptoms.19,20 Therefore, it remains unclear whether anxiety and depression are bidirectionally related across insomnia symptoms. Further contributions to the field may consider different insomnia profiles.
Also, studies did not consider bidirectionality across different types of anxiety disorders. Johnson et al.,11 found that comorbidity rates of insomnia vary across different subtypes. Future research can assess whether sleep disturbances are consistently bidirectionally associated with different anxiety profiles.
Furthermore, the samples used by the included studies were heterogeneous, assessing children, adolescents, young adults, adults, and the elderly. Recent evidence has suggested age may be related to types and prevalence rates of sleep disturbances,60–62 rendering a comparison between studies potentially flawed at this time. The heterogeneous samples across studies also prevented the use of meta-analytic techniques to perform quantitative analyses.
Finally, important potential covariates were not controlled for. One study corrected for alcohol and exercise, but no study accounted for variables that have been associated with sleep disturbances, anxiety, and depression such as lifestyle factors, medical conditions, and other sleep disorders.4,25–33 Bidirectionality is difficult to infer without controlling for such variables. Future research should account for variables such as circadian rhythm disorders, drug and alcohol use, caffeine intake, and exercise.
Although few conclusions can be made, this study contributes to the burgeoning understanding of the etiological relationship between, and prevention of anxiety, depression and various sleep disturbances. At the very least, patients who present with a sleep disturbance should also be assessed for anxiety and depression, and vice-versa.
Bidirectionality was found between insomnia, anxiety, and depression, suggesting that insomnia predicts and is predicted by anxiety and depression. Therefore, successful treatment of insomnia may prevent the onset of subsequent or exacerbation of comorbid anxiety or depression, and vice-versa.14 Future research should consider the most appropriate and cost-effective targets of prevention and intervention for insomnia, anxiety and depression.
The unidirectional relationship between childhood sleep problems and depression suggests that some sleep disturbances may significantly contribute to depression, at least in children, but not vice-versa. Such conclusions should be treated with caution due to the limited research in this area, the overly inclusive nature of the childhood sleep problems variable, and the conceptual overlap with insomnia. Further research is needed to identify the specific sleep disturbance profiles that independently predict anxiety and depression.
In conclusion, due to the small number of studies in this area and the heterogeneity of cohort samples used across studies, few definitive conclusions about the bidirectionality of most sleep disturbances can be made. Best available evidence to date suggests depression bidirectional relationship between insomnia, anxiety, and depression, and further consolidates the association found between sleep disturbances, anxiety, and depression. Therefore, treatment of insomnia may prevent the development of anxiety and depressive disorders, and vice-versa. Future research should consider whether insomnia, anxiety, or depression should be targeted to ensure the most efficient and cost-effective method for prevention and intervention of these disorders.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Authors did not have conflict of interests, including specific financial interests and relationships and affiliations relevant to the subject of this manuscript. The principal author “had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.”
REFERENCES
- 1.Airaksinen E, Larsson M, Forsell Y. Neuropsychological functions in anxiety disorders in population-based samples: Evidence of episodic memory dysfunction. J Psychiatr Res. 2005;39:207–14. doi: 10.1016/j.jpsychires.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Fernández-Mendoza J, Calhoun S, Bixler EO, et al. Insomnia with objective short sleep duration is associated with deficits in neuropsychological performance: A general population study. Sleep. 2010;33:459–65. doi: 10.1093/sleep/33.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gualtieri CT, Johnson LG, Benedict KB. Neurocognition in depression: Patients on and off medication versus healthy comparison subjects. J Neuropsychiatry Clin Neurosci. 2006;18:217–25. doi: 10.1176/jnp.2006.18.2.217. [DOI] [PubMed] [Google Scholar]
- 4.Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Alcohol Drug Depend. 2001;64:1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 5.Achte K. Depression and suicide. Psychopathology. 1986;19(Suppl. 2):210–4. doi: 10.1159/000285157. [DOI] [PubMed] [Google Scholar]
- 6.Sareen J, Cox BJ, Afifi TO, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: A population-based longitudinal study of adults. Arch Gen Psychiatry. 2005;62:1249–57. doi: 10.1001/archpsyc.62.11.1249. [DOI] [PubMed] [Google Scholar]
- 7.Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behav Sleep Med. 2003;1:227–47. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 8.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 9.Alfano CA, Ginsburg GS, Kingery JN. Sleep-related problems among children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:224–32. doi: 10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- 10.Spoormaker VI, Van Den Bout J. Depression and anxiety complaints; Relations with sleep disturbances. Eure Psychiatry. 2005;20:243–5. doi: 10.1016/j.eurpsy.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Fichter MM, Kohlboeck G, Quadflieg N, Wyschkon A, Esser G. From childhood to adult age: 18-year longitudinal results and prediction of the course of mental disorders in the community. Soc Psychiatry Psychiatr Epidemiol. 2009;44:792–803. doi: 10.1007/s00127-009-0501-y. [DOI] [PubMed] [Google Scholar]
- 14.Kaneita Y, Yokoyama E, Harano S, et al. Associations between sleep disturbance and mental health status: A longitudinal study of Japanese junior high school students. Sleep Med. 2009;10:780–6. doi: 10.1016/j.sleep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 15.Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychsom Res. 2008;64:443–9. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addict Behav. 1998;23:827–40. doi: 10.1016/s0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- 17.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 18.Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 19.Ohayon MM. Prevalence and correlates of nonrestorative sleep complaints. Arch Intern Med. 2005;165:35–41. doi: 10.1001/archinte.165.1.35. [DOI] [PubMed] [Google Scholar]
- 20.Hartz AJ, Daly M, Kohatsu ND, Stromquist AM, Jogerst G, Kukoyi O. Risk factors in insomnia in a rural population. Ann Epidemiol. 2007;17:940–7. doi: 10.1016/j.annepidem.2007.07.097. [DOI] [PubMed] [Google Scholar]
- 21.Lindberg E, Janson C, Gislason T, Björnsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: Can gender differences be explained by differences in psychological status? Sleep. 1997;20:381–7. doi: 10.1093/sleep/20.6.381. [DOI] [PubMed] [Google Scholar]
- 22.Luppino FS, De Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 23.Sivertsen B, Krokstad S, Øverland S, Mykletun A. The epidemiology of insomnia: Associations with physical and mental health. The HUNT-2 study. J Psychsom Res. 2009;67:109–16. doi: 10.1016/j.jpsychores.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Essau CA, Lewinsohn PM, Seeley JR, Sasagawa S. Gender differences in the developmental course of depression. J Affect Disord. 2010;127:185–90. doi: 10.1016/j.jad.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferber R. Sleep schedule-dependent causes of insomnia and sleepiness in middle childhood and adolescence. Pediatrician. 1990;17:13–20. [PubMed] [Google Scholar]
- 26.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 27.Randler C, Bilger S, Díaz-Morales JF. Associations among sleep, chronotype, parental monitoring, and pubertal development among German adolescents. J Psychol. 2009;143:509–20. doi: 10.3200/JRL.143.5.509-520. [DOI] [PubMed] [Google Scholar]
- 28.Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin Psychol Rev. 2005;25:629–44. doi: 10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 29.Asztalos M, De Bourdeaudhuij I, Cardon G. The relationship between physical activity and mental health varies across activity intensity levels and dimensions of mental health among women and men. Public Health Nutriti. 2010;13:1207–14. doi: 10.1017/S1368980009992825. [DOI] [PubMed] [Google Scholar]
- 30.Brand S, Gerber M, Beck J, Hatzinger M, Pühse U, Holsboer-Trachsler E. High exercise levels are related to favorable sleep patterns and psychological functioning in adolescents: A comparison of athletes and controls. J Adolesc Health. 2010;46:133–41. doi: 10.1016/j.jadohealth.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 31.Calamaro CJ, Mason TBA, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: Effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–e10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 32.James JE, Kristjánsson ÁL, Sigfúsdóttir ID. Adolescent substance use, sleep, and academic achievement: Evidence of harm due to caffeine. J Adolesc. 2011;34:665–73. doi: 10.1016/j.adolescence.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 33.Whalen DJ, Silk JS, Semel M, et al. Caffeine consumption, sleep, and affect in the natural environments of depressed youth and healthy controls. J Pediatr Psychol. 2008;33:358–67. doi: 10.1093/jpepsy/jsmo86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] 2011. [Accessed 13 February 2012]. http://www.cochrane-handbook.org.
- 35.Armon G, Shirom A, Shapira I, Melamed S. On the nature of burnout-insomnia relationships: A prospective study of employed adults. J Psychosom Res. 2008;65:5–12. doi: 10.1016/j.jpsychores.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 36.Skouteris H, Wertheim EH, Rallis S, Milgrom J, Paxton SJ. Depression and anxiety through pregnancy and the early postpartum: An examination of prospective relationships. J Affect Disord. 2009;113:303–8. doi: 10.1016/j.jad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Jansson-Fröjmark M, Lindblom K. Is there a bidirectional link between insomnia and burnout? A prospective study in the Swedish workforce. Int J Behav Med. 2010;17:306–13. doi: 10.1007/s12529-010-9107-8. [DOI] [PubMed] [Google Scholar]
- 38.Cukrowicz KC, Otamendi A, Pinto JY, Bernert RA, Krakow B, Joiner TE., Jr The impact of insomnia and sleep disturbances on depression and suicidality. Dreaming. 2006;16:1–10. [Google Scholar]
- 39.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67:1240–58. doi: 10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]
- 40.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasler G, Buysse DJ, Gamma A, et al. Excessive daytime sleepiness in young adults: A 20-year prospective community study. J Clin Psychiatry. 2005;66:521–9. doi: 10.4088/jcp.v66n0416. [DOI] [PubMed] [Google Scholar]
- 42.Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Yoon JS. Insomnia, depression, and physical disorders in late life: A 2-year longitudinal community study in Koreans. Sleep. 2009;32:1221–8. doi: 10.1093/sleep/32.9.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gregory AM, Rijsdijk FV, Lau JYF, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: A study of twins aged 8 and 10 years. Sleep. 2009;32:189–99. doi: 10.1093/sleep/32.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gregory MA, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41:964–71. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 45.Meijer AM, Reitz E, Deković M, van den Wittenboer GL, Stoel RD. Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. J Child Psychol Psychiatry. 2010;51:1278–86. doi: 10.1111/j.1469-7610.2010.02261.x. [DOI] [PubMed] [Google Scholar]
- 46.Holmes A, Murphy DL, Crawley JN. Abnormal behavioral phenotypes of serotonin transporter knockout mice: Parrellels with human anxiety and depression. Biol Psychiatry. 2003;54:953–9. doi: 10.1016/j.biopsych.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 47.Nestler EJ, Carlezon WAJ. The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59:1151–9. doi: 10.1016/j.biopsych.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 48.Ouellet M-C, Savard J, Morin CM. Insomnia following traumatic brain injury: A review. Neurorehabil Neural Repair. 2004;18:187–96. doi: 10.1177/1545968304271405. [DOI] [PubMed] [Google Scholar]
- 49.Peroutka SJ, Price SC, Wilhoit TL, Jones KW. Comorbid migraine with aura, anxiety, and depression is associated with dopamine D2 receptor (DRD2) NcoI alleles. Mol Med. 1998;4:14–21. [PMC free article] [PubMed] [Google Scholar]
- 50.Silver MJ, McAllister TW, Yudofsky SC, editors. Textbook of traumatic brain injury. Washington: American Psychiatric Publishing, Inc; 2005. [Google Scholar]
- 51.Yoshioka M, Matsumoto M, Togashi H, Saito H. Effect of conditioned fear stress on dopamine release in the rat prefrontal cortex. Neurosci Lett. 1996;209:201–3. doi: 10.1016/0304-3940(96)12631-8. [DOI] [PubMed] [Google Scholar]
- 52.Lesch K-P, Bengel D, Heils A, et al. Association of Anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science. 1996;274:1527–31. doi: 10.1126/science.274.5292.1527. [DOI] [PubMed] [Google Scholar]
- 53.Mann JJ, Huang YY, Underwood MD, et al. A serotonin transporter gene promoter polymorphism (5-HTTLPR) and prefrontal cortical binding in major depression and suicide. Arch Gen Psychiatry. 2000;57:729–38. doi: 10.1001/archpsyc.57.8.729. [DOI] [PubMed] [Google Scholar]
- 54.Fava M. Daytime sleepiness and insomnia as correlates of depression. J Clin Psychiatry. 2004;65(suppl 16):27–32. [PubMed] [Google Scholar]
- 55.Golub A, Johnson BD, Labouvie E. On correcting biases in self-Reports of age at first substance use with repeated cross-section analysis. J Quant Criminol. 2000;16:45–68. doi: 10.1023/A:1007573411129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Batterham PJ, Glozier N, Christensen H. Sleep disturbance, personality and the onset of depression and anxiety: Prospective cohort study. Aust N Z J Psychiatry. 2012;46:1089–98. doi: 10.1177/0004867412457997. [DOI] [PubMed] [Google Scholar]
- 57.Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32:200–4. doi: 10.1093/sleep/32.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maes M, Song C, Lin A, et al. The effects of psychological stress on humans: Increased production of pro-inflammatory cytokines and a Th1-like response in stress-induced anxiety. Cytokine. 1998;10:313–8. doi: 10.1006/cyto.1997.0290. [DOI] [PubMed] [Google Scholar]
- 59.Müller N, Myint AM, Schwarz MJ. Inflammatory biomarkers and depression. Neurotoxicity Res. 2011;19:308–18. doi: 10.1007/s12640-010-9210-2. [DOI] [PubMed] [Google Scholar]
- 60.Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–34. [PubMed] [Google Scholar]
- 61.Liu X, Zhou H. Sleep duration, insomnia and behavioral problems among Chinese adolescents. Psychiatry Res. 2002;111:75–85. doi: 10.1016/s0165-1781(02)00131-2. [DOI] [PubMed] [Google Scholar]
- 62.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: An epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 63.Angst J, Dobler-Mikola A, Binder J. The Zurich study. a prospective epidemiological study of depressive, neurotic and psychosomatic syndromes. I. Problem, methodology. Eur Arch Psychiatry Neurol Sci. 1984;234:13–20. doi: 10.1007/BF00432878. [DOI] [PubMed] [Google Scholar]
- 64.Achenbach TM, Edelbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington: University of Vermont: Department of Psychiatry; 1983. [Google Scholar]
- 65.Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51. [PubMed] [Google Scholar]
- 66.Kovacs M. The Children's Depression Inventory (CDI) Psychopharmacol Bull. 1985;21:995–8. [PubMed] [Google Scholar]
- 67.Partinen M, Gislason T. Basic nordic sleep questionnaire (BNSQ): A quantitated measure of subjective sleep complaints. J Sleep Res, Supplement. 1995;4:150–5. doi: 10.1111/j.1365-2869.1995.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 68.Broman JE, Lundh LG, Hetta J. Insufficient sleep in the general population. Neurophysiologie Clinique. 1996;26:30–9. doi: 10.1016/0987-7053(96)81532-2. [DOI] [PubMed] [Google Scholar]
- 69.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scan. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 70.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 71.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 72.Doi Y, Minowa M. Factor structure of the 12-item General Health Questionnaire in the Japanese general adult population. Psychiatry Clin Neurosci. 2003;57:379–83. doi: 10.1046/j.1440-1819.2003.01135.x. [DOI] [PubMed] [Google Scholar]
- 73.Prince M, Acosta D, Chiu H, Scazufca M, Varghese M. Dementia diagnosis in developing countries: A cross-cultural validation study. Lancet. 2003;361:909–17. doi: 10.1016/S0140-6736(03)12772-9. [DOI] [PubMed] [Google Scholar]
- 74.Copeland JRM, Dewey ME, Griffiths-Jones HM. A computerized psychiatric diagnostic system and case nomenclature for elderly subjects: GMS and AGECAT. Psychol Med. 1986;16:89–99. doi: 10.1017/s0033291700057779. [DOI] [PubMed] [Google Scholar]
- 75.Meijer AM, van den Wittenboer GLH. The joint contribution of sleep, intelligence and motivation to school performance. Pers Indiv Diff. 2004;37:95–106. [Google Scholar]
- 76.Achenback TM. Manual for the Youth Self-Report and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 77.Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–21. doi: 10.1016/0895-4356(88)90138-2. [DOI] [PubMed] [Google Scholar]