Abstract
Study Objectives:
Short and long sleep duration have been linked with higher rates of comorbid medical and mental health issues, as well as increased mortality. The current study examined the association between sleep duration, mental health problems, and health risk behaviors in a large sample of U.S. Afghanistan/Iraq era veterans.
Design:
NA.
Setting:
Mid-Atlantic VA Medical Center(s).
Patients/Participants:
The sample (N = 1,640) included 20% women (n = 333) and had an average age of 37 years (SD = 10.0).
Interventions:
NA.
Measurements and Results:
Results from logistic regression analyses that included age, minority status, gender, military rank, number of deployments, combat exposure, and health risk behaviors as covariates indicated that very short sleep duration (≤ 5 h of sleep) and long sleep duration (≥ 9 h) were each associated with increased odds of current post traumatic stress disorder (PTSD), major depressive disorder (MDD), and smoking; while poor sleep quality was associated with PTSD, panic disorder (PD), MDD, suicidal ideation (SI), and risky drinking.
Conclusions:
Sleep duration may be an important marker for psychiatric and health risk behavior problems, and our results suggest that clinical assessment of sleep disturbance in this veteran group is warranted to assess for both short and long sleep.
Citation:
Swinkels CM; Ulmer CS; Beckam JC; Buse N; the VA Mid-Atlantic MIRECC Registry Workgroup; Calhoun PS. The association of sleep duration, mental health, and health risk behaviors among U.S. Afghanistan/Iraq era veterans. SLEEP 2013;36(7):1019-1025.
Keywords: Sleep duration, veterans, post traumatic stress, depression, sleep quality
INTRODUCTION
Short sleep duration (SSD) has been linked with medical comorbidities,1–6 mental health problems,7–11 and higher mortality rates in the general public.12–15 Short sleep or insufficient sleep has been identified as a possible risk factor for development of medical and mental health issues. In one of the first studies examining the association between sleep duration and health outcomes in 2,738 redeployed U.S. soldiers who served in Iraq, Luxton and colleagues9 assessed cross-sectional differences on mental health and health behavior outcomes between very short sleep duration (VSSD) as defined by ≤ 5 hours of sleep, short sleep duration (SSD) as defined by ≥ 6 but < 7 hours of sleep, and average sleep duration (ASD) as defined by sleeping ≥ 7 hours per night. The VSSD group was at a significantly higher risk for posttraumatic stress disorder (PTSD), major depressive disorder (MDD), panic disorder (PD), obesity, and mild traumatic brain injury (mTBI) when compared to SSD and ASD. In regards to health behaviors, VSSD was significantly associated with increased risk for smoking, alcohol, and drug use. This study underscored the significant association of VSSD with important psychiatric and behavioral variables but was limited by a lack of clinical psychiatric interviews to establish psychiatric diagnoses.
A similar study,11 utilizing data from the Millennium Cohort Study, examined sleep patterns in 41,225 active duty soldiers before, during, and after deployment and documented that individuals with decreased amounts of pre-deployment sleep (assessed as a continuous variable) were at higher risk of post-deployment MDD (AOR = 2.12), PD (AOR = 2.20), and/or PTSD (AOR = 2.39). In addition, short sleepers were more likely to be smokers (AOR = 1.16) and problem drinkers (AOR = 1.50). Thus, early evidence across two samples of active duty soldiers has indicated that short sleep duration is associated with a wide range of mental health and behavioral health risk factors. However, both of these studies assessed current mental health issues with self-report questionnaires rather than a systematic structured interview. In addition, sleep was assessed with a single item question imbedded in other questionnaires (i.e., demographics and/or PTSD measure).
Although there is evidence that long sleep duration may be equally related to sleep complaints,16 most of the sleep duration research among soldiers with service in Iraq and Afghanistan has been focused on SSD. There has been considerably less attention to the potential health implications of longer sleep duration, i.e., those who sleep ≥ 9 hours per night. This is surprising given that difficulties with sleep onset, sleep maintenance, waking too early or too often, feeling unrefreshed, and daytime sleepiness are noted to be significantly worse in both short and long sleepers.16 There is evidence that prolonged sleep may be associated with increased rates of obesity, cardiovascular issues, diabetes, and mortality.1–6,15 Psychiatric issues associated with sleep duration have found that long sleepers tend to be “worriers.”8
The current study was designed to examine the association between sleep duration, that include both short and long sleepers, and medical, psychiatric, and health risk behaviors in a large sample of U.S. Afghanistan/Iraq era veterans utilizing a structured clinical interview to establish presence of a psychiatric condition. In an extension of previous work examining these associations in active duty soldiers,11 the current study was also designed to examine the impact of longer sleep duration on morbidity, given the previously cited work on long sleep duration and the impact on medical, psychiatric, and health behaviors.
METHODS
Overview/Procedures
The sample in the present study was derived from 1,640 (1,307 males, 333 females) volunteer participants in the multi-site Mid-Atlantic Mental Illness Research, Education and Clinical Center (MIRECC) Recruitment Database for the Study of Post-Deployment Mental Health. Ten veterans were removed from analyses due to missing bedtime and wake time variables. Individuals were contacted through mailings, advertisements and provider referrals to participate. Institutional review boards serving the 4 VA medical centers (Durham, NC; Salisbury, NC; Richmond, VA: and Hampton, VA) from which participants were enrolled gave permission to conduct the study. Inclusion in the study required military service since September 11, 2001. Informed consent was obtained after explaining study-related procedures, which was followed by completion of a structured diagnostic interview for DSM IV TR (SCID) and self-report questionnaires described below.
Instruments
Current psychiatric disorders (e.g., alcohol abuse/dependence [AUD], major depressive disorder [MDD], panic disorder [PD], and posttraumatic stress disorder [PTSD]) were established using the Structured Clinical Interview for DSMIV-TR Axis I Disorders (SCIDI/P), a semi-structured interview administered by trained raters, most of who are doctoral-level raters.17 The mean interrater reliability (n = 22) on scoring a series of 7 SCID training videos for diagnoses was excellent (Fleiss' κ = 0.94). All raters participate in biweekly peer consultation reliability meetings, where diagnoses are reviewed.
Four health risk behaviors, risky alcohol consumption, drug use, tobacco use, and suicidal ideation, were specifically measured.
Risky Drinking
The first 3 consumption items from the World Health Organization's 10-item Alcohol Use Disorders Identification Test (AUDIT)18 were used to assess self-reported risky alcohol use, which is known as the AUDIT-C. In the present study, we used the AUDIT-C cutoff scores of ≥ 3 for women and ≥ 4 for men to identify individuals meeting criteria for risky alcohol use.19 The AUDIT-C has demonstrated adequate reliability and validity in numerous studies comparing outcomes to interview-based diagnostic criteria pertaining to hazardous drinking and alcohol abuse/dependence in VA and general U.S. populations.20–24
Drug Misuse
The Drug Abuse Screening Test (DAST)25 is a 20-item self-report screening measure for drug abuse. Scores range from 0 to 20, with a cutoff score of 6 providing good sensitivity and acceptable specificity for identifying individuals with drug use disorders.
Tobacco Use
Participants were asked to identify themselves as a current smoker, past smoker, or a nonsmoker. Analyses examined likelihood of current smoking.
Suicidal Ideation
The Beck Scale for Suicide Ideation (BSSI)26 is a 19-item self-report instrument that evaluates 3 dimensions of suicidal ideation: active suicidal desire, specific plans for suicide, and passive suicidal desire. The BSSI has demonstrated strong internal consistency, with reported coefficient α ranging from 0.90 to 0.97,27 and there is evidence of the instrument's convergent, discriminative, and predictive validity.28,29 Using survival analyses, Brown and colleagues29 determined that a cutoff score of 3 on the BSS yielded the highest hazard ratio in prediction of risk for actual suicide in a sample of almost 7,000 psychiatric outpatients. This cutoff score was employed here to create a dichotomous index (≤ 2 OR ≥ 3) of suicidal ideation.
Combat Exposure
Combat exposure was assessed using the Combat Exposure Scale (CES),30 a 7-item self-report measure that assesses wartime stressors. Items are rated on a 5-point Likert scale, with higher scores reflecting greater exposure to combat. The CES has been found to demonstrate excellent test-retest and internal consistency.30
Sleep Quality
The Pittsburgh Sleep Quality Index-Addendum (PSQI-A)31 is a widely used self-report instrument that measures of the quality and patterns of sleep in adults. It differentiates “poor” from “good” sleep by measuring sleep over the last month with questions rated on a 0 to 3 Likert scale, whereby a score of 3 reflects the negative extreme. Sleep duration was determined from the question, “How much sleep on average do you get per night?” Participants were categorized into 4 groups based on their reported average length of sleep: very short sleep duration (VSSD; ≤ 5 h of sleep per night), short sleep duration (SSD; > 5 but < 7 h of sleep), average sleep duration (ASD; between 7 and 8 h of sleep), and long sleep duration (LSD; ≥ 9 h of sleep). The total score of the PSQI was utilized to assess overall sleep quality. Insufficient sleep quality is defined as a total PSQI score > 5.31 Lastly, we assessed presence of possible sleep apnea and shift work based on items on the PSQI-A. To qualify for a possible sleep apnea, questions asking about difficulty breathing and snoring (items 5d and e) were scored as positive if the veteran answered positively to either once or twice a week or ≥ 3 times a week on either question. For possible shift work, bedtime (item 1) was used as a proxy for determining group allocation with individuals indicating bedtimes between 6 am and 6 pm who also endorsed working (full-time or part-time). Since the PTSD addendum version was used, periodic limb movement questions were not evaluated.
Statistical Analyses
Analysis of variance and χ2 tests were used to examine bivariate associations between sleep duration and demographic variables. Adjusted logistic regression analyses were used to examine the association between sleep duration and dependent measures while adjusting for age, minority status, gender, combat exposure, military rank, and number of military tours. In addition, health risk behaviors were added as covariates in the model. In each analysis, average sleep duration (ASD) and Commissioned/Warrant officer were used as the referent category.
RESULTS
The sample (N = 1,640) included 20% women (n = 335), and over half (56%, n = 917) were Caucasian. Age had a bimodal distribution, with modes at 25 and 46. The median score was 37 and the mean was 37.4 (SD = 10.04). Non-commissioned officers comprised 59% (n = 975) of the sample, while Junior Enlisted service members accounted for 33% (n = 539), and 8% (n = 126) were Commissioned or Warrant Officers. Forty-nine percent (n = 803; VSSD) of the sample endorsed sleeping < 6 h per night over the past month, 23% (n = 383; SSD) slept between 6 and 7 h per night, 25% (n = 405; ASD) slept > 7 but < 9 h, and 3% (n = 49; LSD) slept ≥ 9 h per night. Poor sleep quality was endorsed by 72% of the sample (n = 1,173). Demographics for each of the sleep duration groups are shown in Table 1.
Table 1.
Characteristics of sample
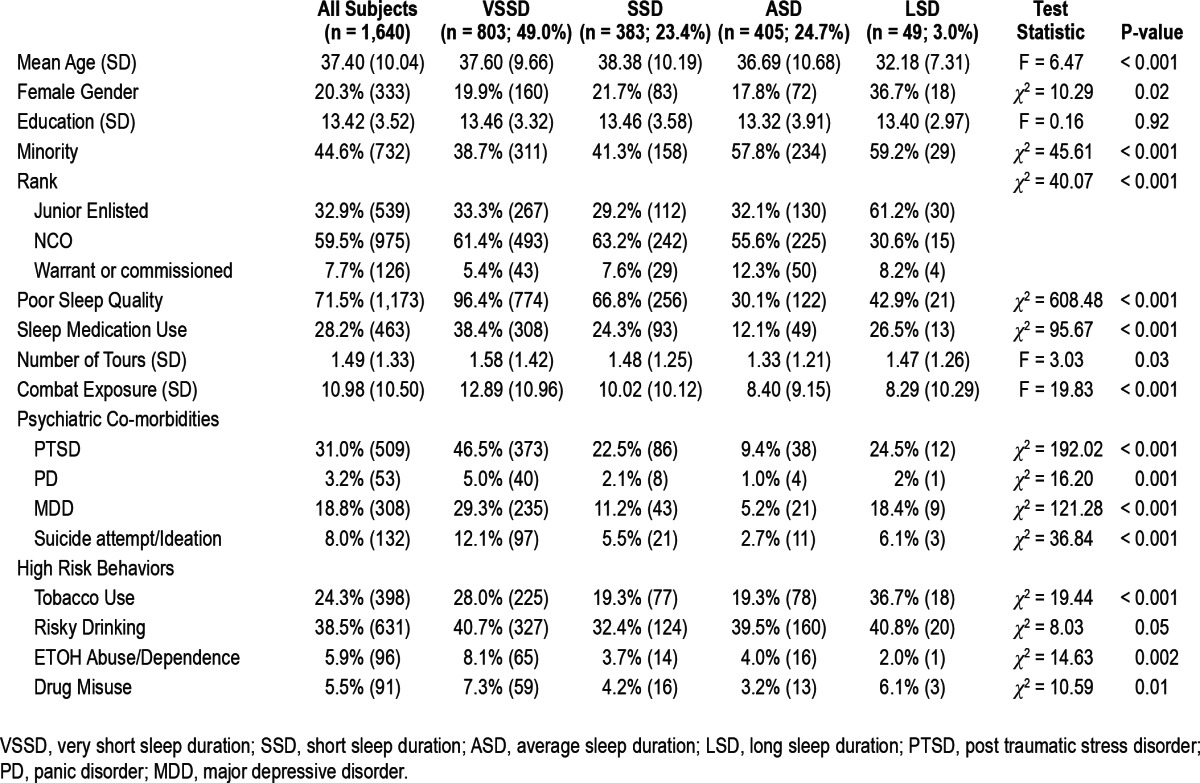
As noted in Table 1, there are small but statistically signifi-cant differences between sleep duration groups in age, combat exposure, and number of tours. LSD individuals were 4 to 6 years younger on average than all of the other groups. In terms of gender, there were more women in the LSD group and fewer in the ASD group. Those with VSSD had significantly more combat exposure than all of the other groups. However, all groups averaged in the mild-to-moderate categories of combat exposure. Lastly, number of tours was significantly different between ASD (1.33) and VSSD individuals (1.58). There were no significant differences in number of tours served among the other sleep duration groups.
Sleep duration groups differed in gender, with a greater proportion of women in the LSD group than the VSSD, SSD, and ASD groups. Minority status was significantly different between VSSD and SSD compared to ASD, as there were more Caucasians in the VSSD and SSD groups. Rank was assessed for sleep duration group differences and we found that Junior Enlisted individuals were more likely to be in either the VSSD or the LSD groups when compared to NCO or Commissioned groups.
All groups differed significantly from each other on self-reported sleep quality due to the following percentages of each group identifying as having “poor” sleep quality: VSSD = 96%, SSD = 67%, ASD = 30%, and LSD = 43%. Sleep medication use was significantly different between all groups except between SSD and LSD. VSSD group reported the most use (38%) with SSD (24%) and LSD (27%) reporting less usage. Some ASD individuals (12%) endorsed sleep medication use. The majority of veterans reported bedtimes between 9 pm and midnight with 75% (n = 304) in the ASD group, 78% (n = 297) in the SSD group, 61% (n = 492) in the VSSD group, and 61% (n = 30) in the LSD group. The estimated number of possible shift workers in each sleep category did not significantly differ (χ23 = 2.33, P = 0.51). In total, 20 participants were identified as possible shift workers, including 5 in the ASD group, 12 in the VSSD group, 2 in the SSD group, and 1 in the LSD group. In regards to possible OSA diagnosis, there was a significant difference between sleep duration groups (χ23 = 92.26, P < 0.001). VSSD and SSD groups had a greater proportion of veterans with possible sleep apnea (52.2%, n = 419; 37.3%, n = 143; respectively), while 24.7% (n = 100) of the ASD group and 26.5% (n = 13) of the LSD met self-reported threshold.
Bivariate analyses examining the association between sleep duration and diagnostic categories (PTSD, PD, MDD) and health behaviors (suicidal ideation, tobacco use, risky drinking, alcohol use disorder, and drug misuse) are shown in Table 1. Sleep duration was significantly associated with PTSD, PD, and MDD (see Table 1). Contrasts indicated there were significant differences between all groups in PTSD rates except between SSD and LSD groups. VSSD and LSD groups only significantly differed on rates of PTSD but all other rates were not significantly different. In terms of health risk behaviors, VSSD endorsed higher frequencies of drug misuse, alcohol use disorders, and suicidal ideation compared to ASD, and higher frequencies of smoking, alcohol use disorder, and drug misuse than SSD. Smoking status was also significantly different in LSD individuals when compared to either SSD or ASD groups, with LSD reporting a higher rate of current smoking.
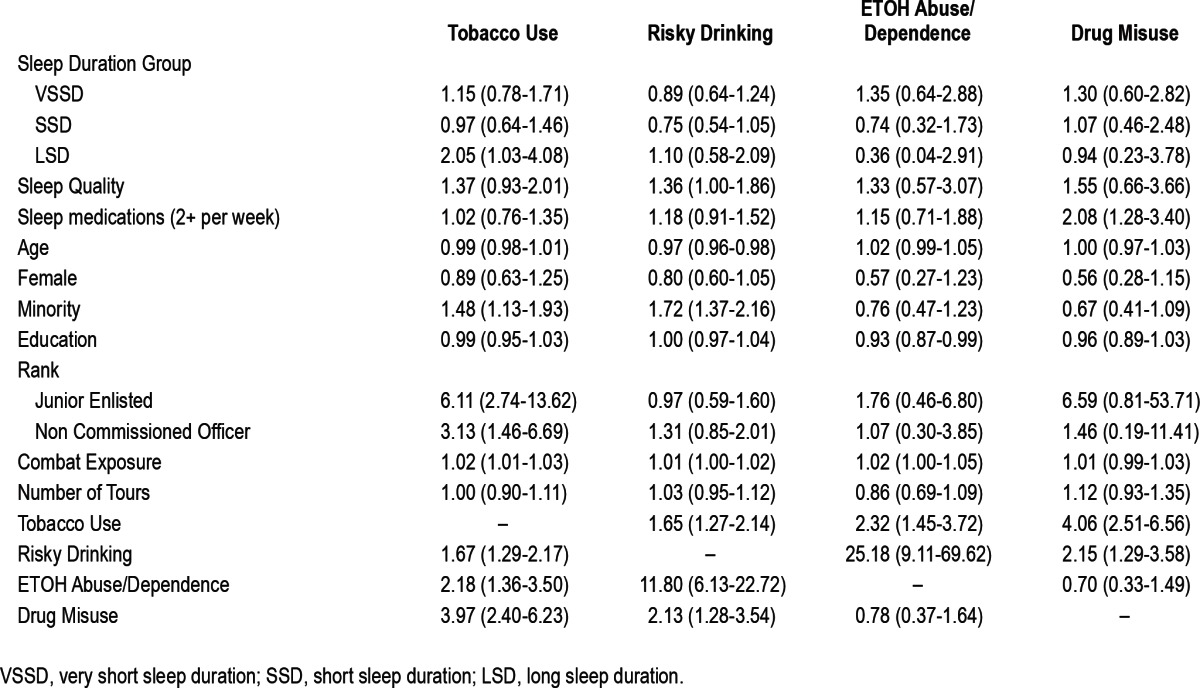
Results from logistic regression analyses that adjusted for overall sleep quality, sleep medication use, age, gender, education, minority status, military rank, number of deployments, combat exposure, and health risk behaviors (tobacco use, risky drinking, drug misuse, and alcohol abuse/dependence) as covariates indicated that both VSSD and LSD were associated with increased odds of PTSD and MDD. Adjusted odds ratios (AOR) are presented in Tables 2 and 3. LSD was associated with increased odds of current smoking, but sleep duration was not related to other health risk behaviors in adjusted analyses. Overall, self-reported sleep quality and sleep medication use was associated with increased odds of PTSD, Panic, MDD, and SI. In terms of health risk behaviors, sleep quality was associated with increased odds of risky drinking, while sleep medication was associated with increased odds of drug misuse.
Table 2.
Adjusted Odds Ratio and 95% CI measuring associations between predictor variables and mental health issues
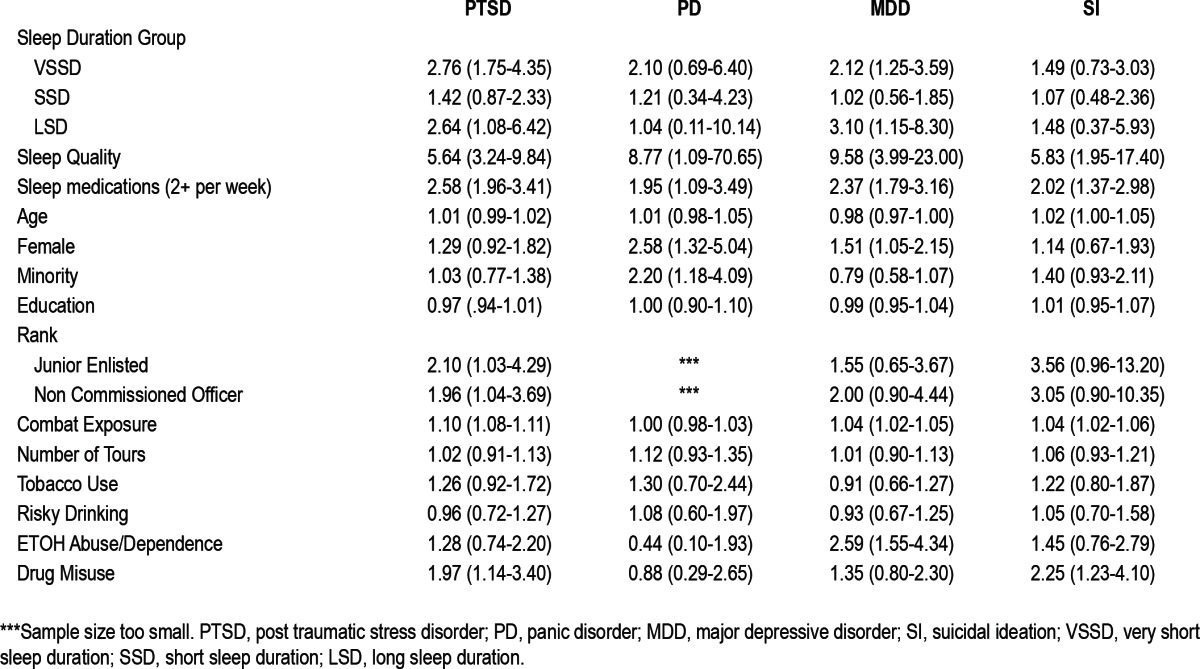
Table 3.
Adjusted Odds Ratio and 95% CI measuring associations between predictor variables and health behaviors
DISCUSSION
Few studies have addressed the relationship between sleep duration across the full sleep spectrum in relation to psychiatric and health risk behaviors in U.S. Iraq/Afghanistan era veterans. Similar to previous work examining active duty soldiers,9,11 very short sleep duration (VSSD) was associated with increased mental health conditions and health risk behaviors. The present study made an important distinction between average sleep duration (ASD) and long sleep duration (LSD). In redefining group allocation, we were able to assess the associations with longer sleep duration that were undetected in previous work. Generally, we found that compared to the short sleep duration (SDD) and ASD groups, both the VSSD and LSD groups were more likely to have mental health issues. Most strikingly, both VSSD and LSD were associated with three times the rate of PTSD and MDD diagnoses relative to the ASD group. When compared to the Luxton study,9 the current sample of very short sleepers had similar OR for PTSD (4.7 and 2.8, respectively) but were dissimilar for depression (11.4 and 2.1, respectively), which may be the result of method of measurement (self-report versus structured diagnostic interview). LSD was associated with more than double the rate of current smoking of the ASD group. Poor sleep quality was dramatically associated with PTSD (5 times the rate), MDD (9 times the rate), and suicidal ideation (almost 6 times the rate), and is consistent with other studies.7,11
These findings are important because they further define the increased risk association that too little or too much sleep can have with mental health. The finding from this study that LSD was associated with increased risk of current smoking is consistent with other studies that have found both short sleep and long sleep were associated with increased physical health risks (i.e., obesity, cardiovascular issues, and diabetes). As compared to a previous study assessing sleep duration in a sample from the general population,14 an incident rate of 7.6% of long sleepers was higher than the reported 3% in the current study. Although the reported rates of long sleep duration were lower in the veteran sample, tobacco use was found to be significantly higher in this sample. Taken together with previous studies, it might be useful to evaluate sleep duration as a proxy to identify individuals at increased risk of both mental and physical health conditions. Assessing sleep duration in veterans may play an important role in identifying individuals at risk for mental and medical health issues. It might also provide a useful tool in creating a prevention intervention to avoid future health issues. However, the temporal relationships between sleep disturbance and psychiatric disorder and risky health behaviors, as well as what, when, and whether intervention would be helpful, will require longitudinal studies.
There were surprising findings in the current study regarding sleep medication usage that should be further assessed. While the highest use of sleep medication was by those reporting VSSD, 27% of LSD individuals utilized sleep medications. This is a higher rate of usage than has been reported for the general population. In two earlier studies,32,33 17% to 18% of adults reported using prescription medications for sleep, 7.1% used over-the-counter medications,32 and 13% used alcohol to sleep.33 Given their self-reported long sleep duration, it would be important to identify reasons for use and whether the medication is “responsible” for the elongated total sleep time reported in this sample. Interesting, those endorsing drug misuse were more likely to use sleep medications two or more times per week.
Conclusions from the present study are limited by the assessment of sleep duration, which was based on self-report. Ideally, future studies would include a method of verifying daily tracking sleep duration that could time stamp entries, such as digital diaries, voice recording systems (VRS), and be compared to an objective measure of sleep, such as actigraphy. Self-report sleep measures may introduce recall bias and involve inaccurate evaluation of actual sleep. However, self-report measures offer an insight into how one perceives his/her own sleep, which may affect his/her cognitive beliefs about him/herself. These cognitions may play a role in the comorbidity of other psychiatric issues, such as depression, PTSD, and anxiety. Secondly, the measure used to assess sleep is not a diagnostic tool that can identify specific sleep disorders. Thus, other etiologies for duration of sleep (such as sleep apnea, periodic limb movement, shift work) and/or comorbid conditions (such as chronic pain or chronic fatigue) were undetermined in this study and would require further investigation to evaluate whether specific sleep disorder diagnoses are associated with VSSD, LSD, specific psychiatric diagnoses, and risky health behaviors. Lastly, the data were cross sectional in nature so causal inference is not possible
CONCLUSION
The present study provides additional confirmation that sleep duration is related to increased risk for mental health issues and increased smoking prevalence among U.S. Afghanistan/Iraq era veterans. It extends previous findings by demonstrating that those having longer sleep duration are also at an increased risk. Grandner and Drummond13 posited several possible mechanism of action that may need to be considered for future investigation as to the contributing factors linking sleep duration to mortality, such as sleep fragmentation (or prolonged time spent in bed), fatigue (decreased resistance to stress), changes in cytokine expression, reduced time spent in well lit environments, lack of physicality, underlying disease process, or underlying psychological processes. The current study could be extended to investigation possible causal relationships between these variables.
The necessity of short sleep while in combat is prevalent among active duty soldiers.11,32,34,35 However, there has been little focus on “re-training” these individuals to sleep once they have returned, which may leave them susceptible to both medical and mental health issues. Data from the current large volunteer sample of veterans who had been discharged for an average of 2.7 years (SD = 2.63) indicated that many continue to struggle with short and long sleep duration disturbance as well as psychiatric morbidity and health risk behaviors, which could be related to deployment stressors (including combat exposure). Regardless of temporal sequence of occurrence, sleep duration may be an important marker in returning veterans for comorbid psychiatric and health risk behavior problems, and our results suggest that clinical assessment of sleep disturbance in this veteran group is warranted to assess for both short and long sleep.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This research is supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Durham VA Medical Center, and the Department of Veterans Affairs Mid-Atlantic Mental Illness Research, Education, and Clinical Center (VISN 6 MIRECC).
The VA Mid-Atlantic MIRECC workgroup for this publication includes John A. Fairbank, Christine E. Marx, Scott D. Moore, Rajendra A. Morey, Mira Brancu, Larry A. Tupler from the Durham VA Medical Center, Durham, NC; Marinell Miller-Mumford from the Hampton VA Medical Center, Hampton, Virginia; Scott D. McDonald, Treven Pickett from the Hunter Holmes McGuire VA Medical Center, Richmond, Virginia; and Robin Hurley, Katherine H. Taber, Ruth E. Yoash-Gantz from the W.G. Hefner VA Medical Center, Salisbury, NC.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or any of the other institutions with which the authors are affiliated. We thank those who kindly volunteered to participate in this study.
REFERENCES
- 1.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 2.Cappuccio FP, Stranges S, Kandala N, et al. Gender-specific associations of short sleep duration with prevalence and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first national health and nutrition examination survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 4.Mallon L, Broman J, Hetta J. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28:2762–7. doi: 10.2337/diacare.28.11.2762. [DOI] [PubMed] [Google Scholar]
- 5.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eisen SV, Schultz MR, Vogt D, et al. Mental and physical health status and alcohol and drug use following return from deployment to Iraq and Afghanistan. Am J Public Health. 2012;102:S66–S72. doi: 10.2105/AJPH.2011.300609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartmann E, Baekeland F, Zwilling GR. Psychological differences between long and short sleepers. Arch Gen Psychiatry. 1972;26:463–8. doi: 10.1001/archpsyc.1972.01750230073014. [DOI] [PubMed] [Google Scholar]
- 9.Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34:1189–95. doi: 10.5665/SLEEP.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national survey replication (NCS-R) Biol Psychiatry. 2006;60:1364–71. doi: 10.1016/j.biopsych.2006.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during , and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–22. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 13.Grandner MA, Drummond SPA. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11:341–60. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 15.Stranges S, Dorn JM, Shipley MJ, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States. Am J Epidemiol. 2008;168:1353–64. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grandner MA, Kripke DF. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom Med. 2004;66:239–41. doi: 10.1097/01.psy.0000107881.53228.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.First MB, Spitzer RL, Miriam G, Williams JBW. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/PSY SCREEN) [Google Scholar]
- 18.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd ed. Geneva, Switzerland: Department of Mental Health and Substance Dependence, World Health Organization; 2001. [Google Scholar]
- 19.Calhoun PS, Elter JR, Jones ER, Kudler H, Straits-Troster K. Hazardous alcohol use and receipt of risk-reduction counseling among U.S. veterans of the wars in Iraq and Afghanistan. J Clin Psychiatry. 2008;69:1686–93. doi: 10.4088/jcp.v69n1103. [DOI] [PubMed] [Google Scholar]
- 20.Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821–9. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- 21.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA for the Ambulatory Care Quality Improvement Project. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158:1789–95. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 22.Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29:844–54. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- 23.Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): a review of recent research. Alcohol Clin Exp Res. 2002;26:272–9. [PubMed] [Google Scholar]
- 24.Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test: an update of research findings. Alcohol Clin Exp Res. 2007;31:185–99. doi: 10.1111/j.1530-0277.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- 25.Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the drug abuse screening test in the assessment of DSM-III drug disorders. Br J Addict. 1989;84:301–7. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- 26.Beck AT, Steer RA. Manual for Beck scale for suicidal ideation. New York: Pennsylvania Corporation; 1991. [Google Scholar]
- 27.Steer RA, Rissmiller DJ, Ranieri WF, Beck AT. Dimensions of suicidal ideation in psychiatric inpatients. Behav Res Ther. 1993;31:229–36. doi: 10.1016/0005-7967(93)90090-h. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicidal ideation with psychiatric outpatients. Behav Res Ther. 1997;35:1039–46. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 29.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J Consult Clin Psych. 2000;68:371–7. [PubMed] [Google Scholar]
- 30.Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a meaure to assess combat exposure. Psychol Assessment. 1989;1:53–5. [Google Scholar]
- 31.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiat Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 32.Goodwin RD, Hasin DS. Sedative use and misuse in the United States. Addiction. 2002;97:555–63. doi: 10.1046/j.1360-0443.2002.00098.x. [DOI] [PubMed] [Google Scholar]
- 33.Johnson EO, Roehrs T, Roth T, Breslau N. Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep. 1998;21:178–86. doi: 10.1093/sleep/21.2.178. [DOI] [PubMed] [Google Scholar]
- 34.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173:230–5. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- 35.Mental Health Advisory Team (MHAT) V Operation Iraqi Freedom 06-08. Office of the Surgeon Multi-National Force-Iraq and Office of the Surgeon General United States of Army Medical Command [Google Scholar]


