Abstract
Study Objectives:
To evaluate predeployment sleep duration and insomnia symptoms in relation to the development of mental health symptoms.
Design:
Longitudinal cohort study.
Setting:
The Millennium Cohort Study survey is administered via a secure website or US mail.
Participants:
Data were from 15,204 participants who completed their first deployment between the submissions of 2 consecutive Millennium Cohort questionnaires (2001-2008).
Interventions:
N/A.
Measurements and Results:
Using self-reported data from the Millennium Cohort Study we evaluated the association of predeployment sleep duration and insomnia symptoms on the development of new-onset mental disorders among deployers. Multivariable logistic regression was used to estimate the odds of developing posttraumatic stress disorder (PTSD), depression, and anxiety, while adjusting for relevant covariates including combat-related trauma. The study outcomes were assessed using validated instruments, including the PTSD checklist-civilian version, and the PRIME-MD Patient Health Questionnaire. We identified 522 people with new-onset PTSD, 151 with anxiety, and 303 with depression following deployment. In adjusted models, combat-related trauma and predeployment insomnia symptoms were significantly associated with higher odds of developing posttraumatic stress disorder, depression, and anxiety postdeployment.
Conclusions:
Sleep characteristics, especially insomnia symptoms, are related to the development of mental disorders following military deployments. Assessment of insomnia symptoms predeployment may help to better identify those at highest risk for subsequent adverse mental health outcomes.
Citation:
Gehrman P; Seelig AD; Jacobson IG; Boyko EJ; Hooper TI; Gackstetter GD; Ulmer CS; Smith TC; for the Millennium Cohort Study Team. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. SLEEP 2013;36(7):1009-1018.
Keywords: Stress disorders, post-traumatic, anxiety, depression, sleep
INTRODUCTION
Military personnel, particularly those engaged in combat situations, are at increased risk for developing mental disorders such as posttraumatic stress disorder (PTSD) and depression.1–3 Postdeployment assessments of personnel returning from Operation Enduring Freedom and Operation Iraqi Freedom (OEF/ OIF) found that 20.3% of active duty and 42.4% of reserve soldiers reported significant mental health symptoms.1 Insomnia symptoms often occur in association with military deployment, with combat-related trauma and the presence of mental health symptoms substantially increasing the likelihood of difficul-ties with sleep.4 While it is reasonable to expect that insomnia symptoms are a consequence of these situations, there is reason to believe that preexisting insomnia may increase the risk of developing mental disorders in response to extremely stressful situations such as combat.5,6 Longitudinal studies have demonstrated that insomnia confers significant risk for the development of new-onset major depressive disorder and anxiety disorders, including PTSD.7–19 Insomnia is both a symptom and a risk factor for mental illness and may present a modifiable target for intervention among military personnel.
The Millennium Cohort Study20 provides a unique ability to enhance understanding of the role of insomnia symptoms and sleep duration as risk factors for new-onset mental disorders in a large, population-based, prospective investigation of military personnel. The aim of our study was to evaluate predeployment sleep in relation to the development of PTSD, depression, and anxiety, and whether combat-related trauma modified these associations.
METHODS
Study Population and Data Sources
In mid-2001, over 200,000 military personnel on active service rosters were contacted to participate in the first panel of the Millennium Cohort; 77,047 (36.0%) were enrolled. Of these, 55,021 (71%) completed a first follow-up questionnaire (2004-2006), 54,790 (71%) completed a second follow-up (2007-2008), and 46,438 (60%) completed both follow-ups. Another 31,110 (25%) were enrolled in a second panel (2004-2006). Of these individuals, 17,152 (55%) completed a first follow-up survey (2007-2008). Additional details regarding Millennium Cohort methodology have been published elsewhere.20–22
In order to prospectively examine risk factors for postdeployment new-onset mental health disorders, eligibility criteria for this study included: having at least one deployment between their baseline and a follow-up questionnaire; having no deployments before their baseline questionnaire; screening negative for PTSD, depression, anxiety, or panic predeployment; and no indication of a prior diagnosis of a mental disorder or use of psychotropic medications predeployment. For the depression model, an additional eligibility criterion was that women must not have reported being pregnant or recently giving birth on their predeployment assessment to avoid instances of postpartum depression. Based on these criteria to execute the study design, 18,175 Millennium Cohort participants were eligible for these analyses. After removing those missing outcome (n = 1,196), exposure (n = 240), or covariate data (n = 1,535), our final study population was 15,204 for PTSD and anxiety models, and 15,000 for the depression model.
This study population, comprised only of deployers, was grouped based on the timing of their first deployment. The early deployment group (Group 1, n = 9,043) included Panel 1 members who had their first deployment between the first (2001-2003) and second (2004-2006) survey cycles. The later deployment group (Group 2, n = 6,161) were Panel 1 and Panel 2 participants who had their first deployment between the second (2004-2006) and third (2007-2008) survey cycles.
Military-specific data, including deployment dates, deployment location, service branch, pay grade, occupation, service component, and demographics, were provided by the Defense Manpower Data Center (see Table 1). Millennium Cohort questionnaire data were used to assess all other covariates. Current smokers were defined as those who indicated smoking > 100 cigarettes in their lifetime and had not tried or were unsuccessful at quitting. The 4-item CAGE (Cut-back, Annoy, Guilty, Eye-opener) questionnaire was used to assess potential problem drinkers, where individuals who positively endorsed ≥ 1 item were defined as having potential alcohol problems.23 History of life stressors was determined using scoring mechanisms adapted from the Holmes and Rahe Social Readjustment Rating Scale.24
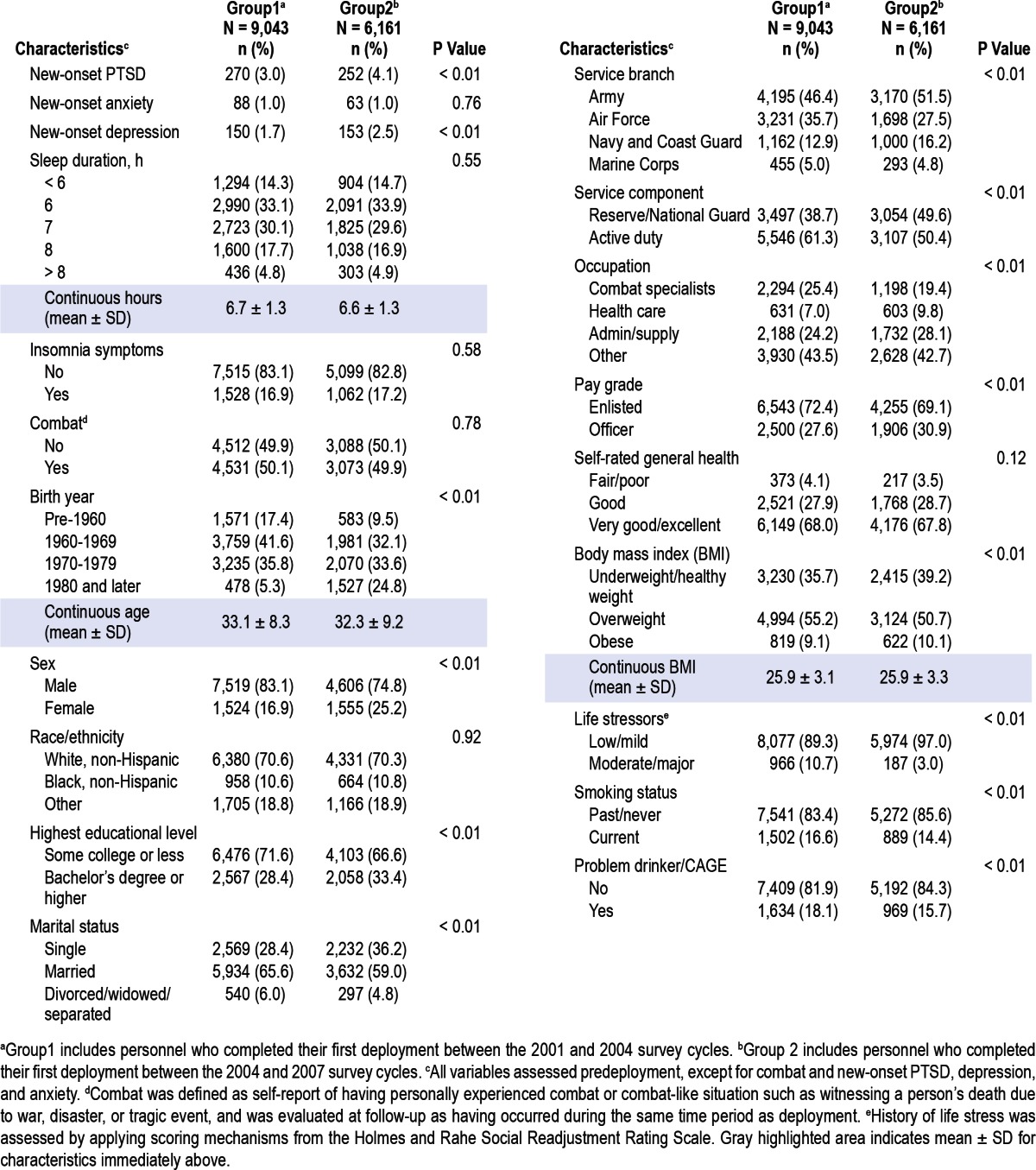
Table 1.
Demographic, military and behavioral characteristics of 15,204 Millennium Cohort participants by timing of first deployment
Predeployment sleep was assessed in 2 ways: insomnia symptoms and sleep duration. Average sleep duration (in a 24-h period) during the past month was self-reported in whole number hourly increments. Insomnia symptoms were assessed using questions from the Patient Health Questionnaire (PHQ)25,26 for anxiety and the PTSD Checklist, Civilian Version (PCL-C).27 Insomnia symptoms were defined as responding “moderately” or above in response to the question “In the past month, have you had trouble falling asleep or staying asleep?” on the PCL-C; or responding “several days” or longer to the question “Over the last 4 weeks, how often have you experienced trouble falling asleep or staying asleep?” on the PHQ.
Combat-related traumas were defined as having personally (1) witnessed a death due to war, disaster, or tragic event; (2) witnessed instances of physical abuse; (3) been exposed to dead or decomposing bodies; (4) been exposed to maimed soldiers or civilians; or (5) been exposed to prisoners of war or refugees. These were evaluated at follow-up as having occurred during the same time period as deployment. All covariates, except combat-related trauma, were assessed at the predeployment survey.
Outcomes
New-onset PTSD was assessed using the 17-item PCL-C.27,28 A participant screened positive according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria when ≥ 3 avoidance symptoms, 2 hyperarousal symptoms, and 1 intrusion symptom were endorsed at “moderate” or higher levels.27,29 Since the sleep item from the PCL-C was used to define insomnia symptoms, PTSD was scored without this item.
New-onset depression was assessed using the PHQ-9, a validated screening instrument based on DSM-IV diagnostic criteria.25,30–32 Participants screened positive if they responded “more than half the days” or “nearly every day” to ≥ 5 of the 9 depressive symptoms, and 1 of the 5 items endorsed was depressed mood or anhedonia.25
New onset of generalized anxiety disorder was assessed using the 7-item anxiety module in the PHQ, which is composed of generalized anxiety disorder symptoms excluding anxiety related to panic attacks or exclusively in relation to PTSD. Persons screened positive if they indicated feeling nervous, anxious, on edge; or worrying a lot on more than half the days over the past 4 weeks and they indicated experiencing ≥ 3 of the 6 other anxiety symptoms on more than half the days. The sleep item in the anxiety module was used to create the insomnia symptoms variable, so the anxiety outcome was scored without this item.
Statistical Analyses
Chi-square tests of association and univariate logistic regression models were used to assess unadjusted relationships between each mental disorder and all covariates. Multivariable logistic regression models were used to determine the odds of new-onset PTSD, depression, and anxiety postdeployment, in relation to predeployment sleep duration and insomnia symptoms, after adjusting for relevant demographic, military, and health covariates. All covariates were included in models based on published literature. Race/ethnicity was included because previous research has shown that ethnic minority veterans have higher rates of mental illness than Caucasian veterans.33,34 Regression diagnostics were used to assess multicollinearity between all covariates.
In multivariable analyses, interactions were tested to examine whether combat-related trauma modified the relationship between insomnia symptoms and each mental health outcome, with the criterion for significance being α = 0.10, 2-sided. In addition, 2 sensitivity analyses were performed. The first included additional deployment-related exposures (deployment location, percent time deployed, multiple deployments, and dwell time). Dwell time is a ratio of the time spent at home between 2 deployments to the time spent on the preceding deployment. The second sensitivity analysis tested the combat variable to ensure that 1 of the items, “witnessed instance of physical abuse,” was not driving a spurious association. The 5 items used to identify combat-related trauma were evaluated at follow-up and asked about experiences over the last 3 years, which corresponded to the same time period as a deployment. However, participants were not specifically asked if these events occurred while deployed, and the physical abuse item has the most potential to be unrelated to deployment. Therefore, we conducted sensitivity analyses where combat-related trauma was reevaluated excluding the abuse item. In addition, to explore mental health outcomes for the most severe phenotype of insomnia symptoms with short sleep duration, a secondary analysis was run to examine those who reported insomnia symptoms and the shortest nightly sleep duration (< 6 h). The sleep exposure variables were combined and categorized into 4 groups: (1) insomnia symptoms and < 6 h sleep per night, (2) insomnia symptoms and ≥ 6 h sleep per night, (3) no insomnia symptoms and < 6 h of sleep per night, (4) no insomnia symptoms and ≥ 6 hours of sleep per night (reference).
This study was approved by the Naval Health Research Center Institutional Review Board, and informed consent was obtained from all subjects. Data management and statistical analyses were performed using SAS statistical software, version 9.3 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
At follow-up, 522 people screened positive for new-onset PTSD, 151 for anxiety, and 303 for depression. Approximately 50% of subjects reported combat-related trauma, and 17% reported insomnia symptoms predeployment (Table 1). Mean predeployment sleep duration was similar for Group 1 and Group 2—6.7 and 6.6 h, respectively. Compared with Group 2, Group 1 subjects, who deployed earlier, were more likely to be older, male, less educated, married, in the Air Force, serving on active duty, combat specialists, enlisted, overweight, and to report greater life stress, current smoking, and problem drinking.
PTSD
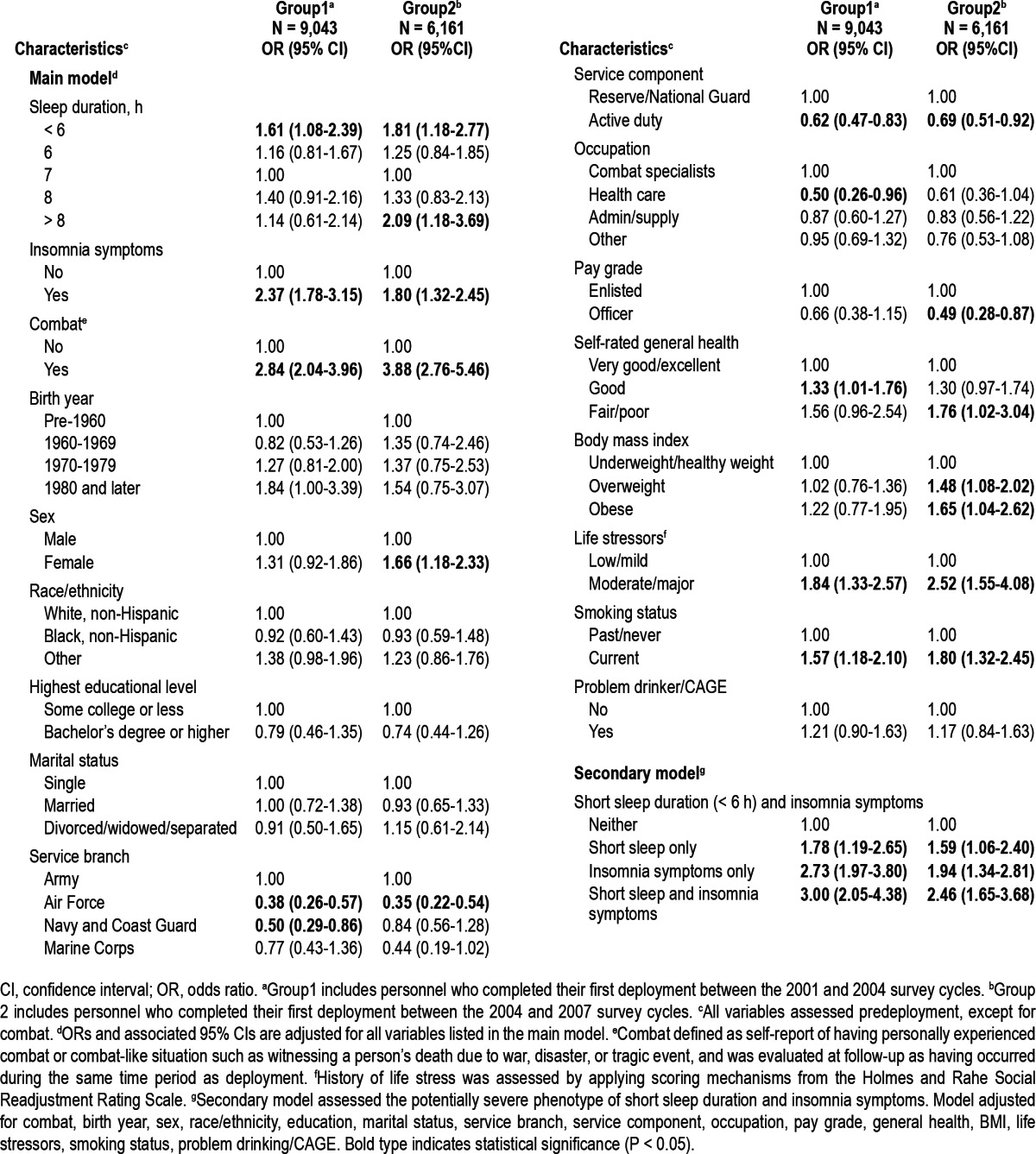
The association between predeployment sleep duration and postdeployment new-onset PTSD was modified by the Group variable (P = 0.02), so all analyses were stratified by deployment group. For both Groups, those who slept < 6 h predeployment had significantly greater odds of developing PTSD than those who slept 7 hours (Table 2). Among Group 1 and Group 2, those who reported insomnia symptoms prior to deployment had increased odds (odds ratio [OR], 2.37; 95% confidence interval [CI], 1.78-3.15, and OR, 1.80; 95% CI, 1.32-2.45, respectively) of developing PTSD. Among Group 2, those who slept > 8 h had increased odds of developing PTSD following deployment, as did those with insomnia symptoms. Participants who reported combat-related trauma had over 2 times the odds of developing PTSD in both groups. Additional factors associated with increased odds of new onset PTSD among both groups included being in the Army compared with the Air Force, being in the Reserve/Guard, and reporting higher stress and current smoking. There was no significant interaction between combat-related trauma and insomnia symptoms. Among Group 1 and Group 2, those with the most severe phenotype (insomnia symptoms and short sleep [< 6 h per night]) had significantly increased odds of developing PTSD following deployment (OR: 3.00, 95% CI: 2.05-4.38, and OR: 2.46 95% CI: 1.65-3.68, respectively).
Table 2.
Adjusted odds of new-onset PTSD following deployment in 15,204 Millennium Cohort participants (2001-2008)
Depression
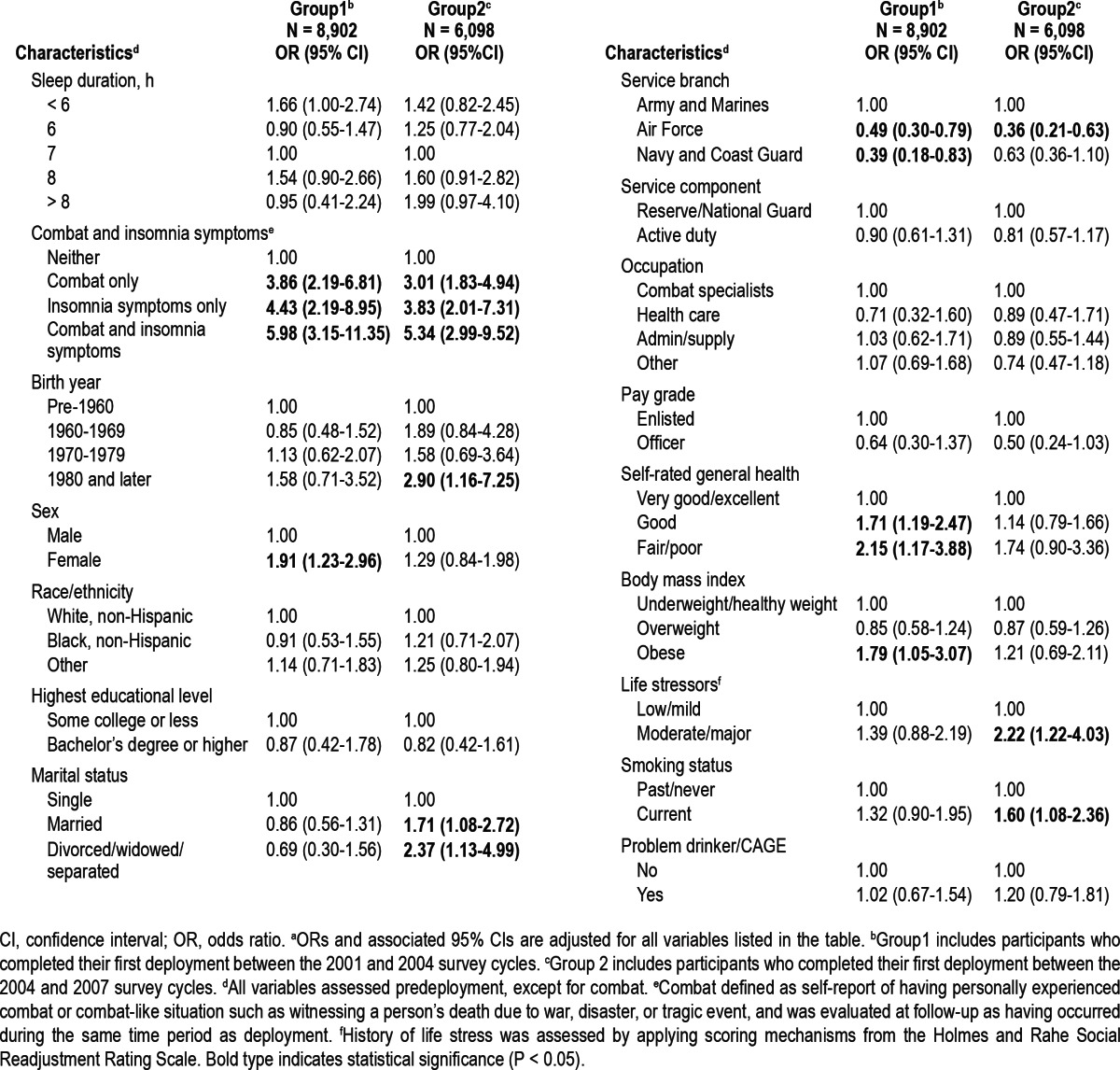
Combat significantly modified the association between depression and insomnia symptoms (Group 1, P < 0.01; Group 2, P = 0.04), so the odds of depression in relation to insomnia symptoms are presented separately for persons with and without combat-related trauma. For Group 1, the adjusted odds of developing depression were highest in those with both insomnia symptoms and combat (OR, 5.98; 95% CI, 3.15-11.35), followed by insomnia symptoms only, then combat only (Table 3). The same pattern and similar strength of association was seen in Group 2. Differences in sleep duration were not significant. Among Group 1, women, individuals in the Army and Marines, those with lower general health, and those considered obese, had significantly increased odds of developing depression. Among Group 2, younger, single participants, those with high stress, and current smokers had increased odds of developing depression. Secondary analyses assessing those who reported insomnia symptoms and short sleep duration were not performed for the depression model due to the interaction between combat and insomnia symptoms.
Table 3.
Adjusteda odds of new-onset depression following deployment in 15,000 Millennium Cohort participants (2001-2008)
Anxiety
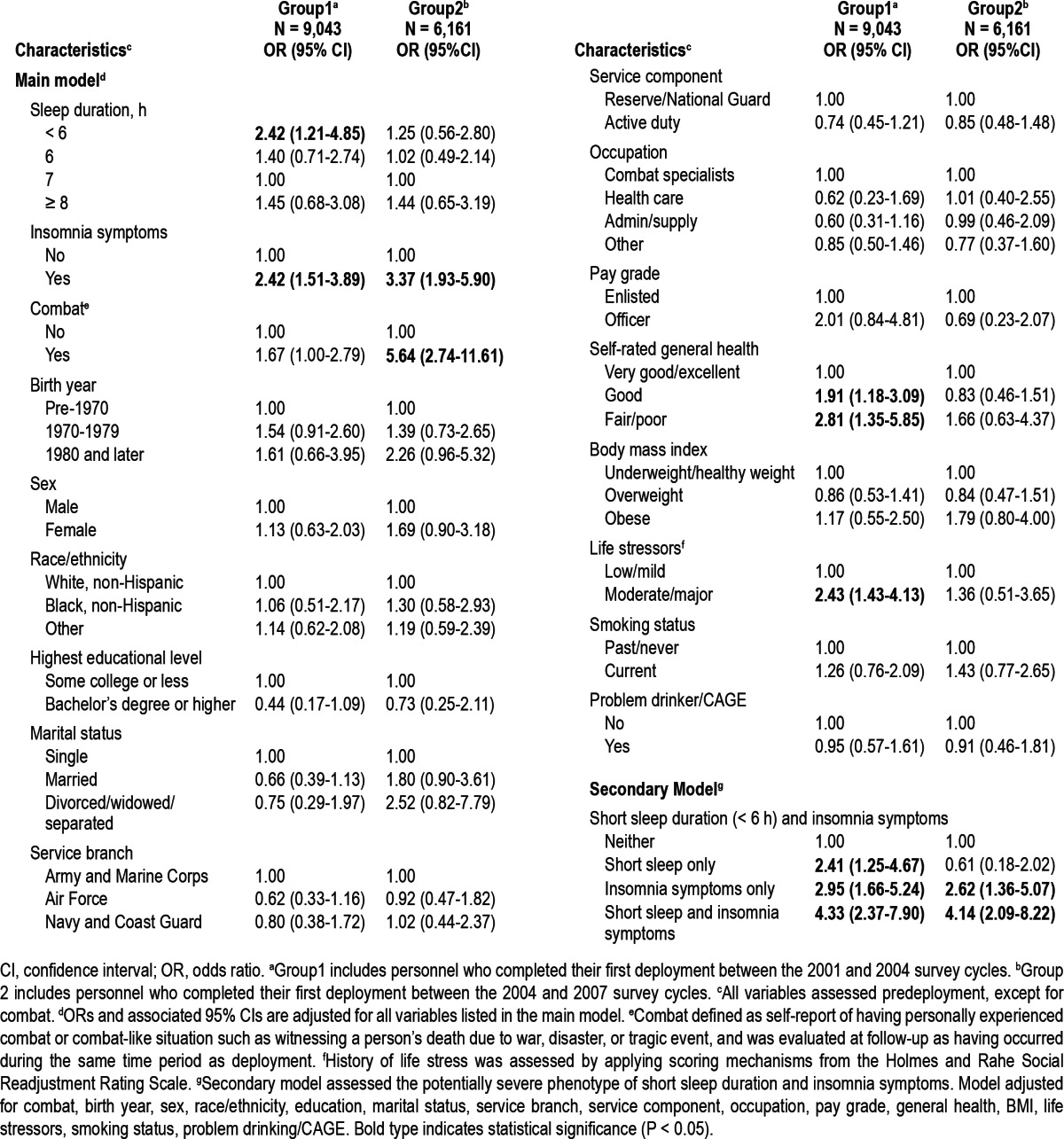
Among Group 1 participants, those who slept < 6 h per day and those with insomnia symptoms had increased odds of developing anxiety postdeployment (Table 4). Among Group 2, sleep duration was not significant, but those who reported insomnia symptoms or combat-related trauma had significantly increased odds, which were the only significant variables for this Group. Group 1 showed that those with lower general health and higher stress had increased odds for anxiety. There was no significant interaction between combat-related trauma and insomnia symptoms in relation to new-onset anxiety. Among Group 1 and Group 2, those with insomnia symptoms and < 6 h sleep per night had significantly increased odds of developing anxiety following deployment compared to those who did not have insomnia symptoms and slept ≥ 6 h per night (Group 1 OR: 4.33, 95% CI: 2.37-7.90, and Group 2 OR: 4.14 95% CI: 2.09-8.22).
Table 4.
Adjusted odds of new-onset anxiety following deployment in 15,204 Millennium Cohort participants (2001-2008)
Insomnia Symptoms
Since this study used one sleep item from the PHQ and one sleep item from the PCL to evaluate insomnia symptoms, and this is not a validated measure of sleep, we assessed the overlap between the 2 sleep items. Results indicated notable overlap among those who met the criteria for insomnia symptoms: 30% met the criteria on both scales, 50% met the criteria on the PHQ only (a more sensitive measure), and 20% met the criteria on the PCL only (a more specific measure). To further examine whether or not using the 2 items combined created a more sensitive measure for insomnia symptoms, we ran new models defining insomnia symptoms based on each sleep item separately and compared these results to those from our original models. Findings showed that the point estimates decreased when the PCL sleep item was used and increased when the PHQ sleep item was used. However, for both the PCL and PHQ sleep models, the point estimates were within the 95% CI of the original models.
Sensitivity Analyses
Sensitivity analyses comparing the main models to models with additional deployment variables showed consistent results and did not reveal any additional factors that contribute to mental disorders. The strength and direction of the associations between predeployment sleep and postdeployment mental disorders remained stable after the addition of deployment location, number of deployments, percent time deployed, and dwell time (data not shown). Sensitivity analyses comparing the results of the main models using the 5-item combat definition to the 4-item combat definition also showed no significant differences (data not shown).
DISCUSSION
Understanding environmental and behavioral risk factors associated with the onset of common major mental disorders is of great importance in a military occupational setting. This study is the first prospective investigation of the relationship between sleep disturbance and development of newly identified positive screens for mental disorders in a large military cohort who have been deployed in support of the recent operations in Iraq or Afghanistan. We found a statistically significant increased risk for new-onset PTSD, depression, and anxiety positive screens in those reporting predeployment insomnia symptoms independent of other potential risk factors. Additionally, short sleep duration (< 6 h) was associated with new-onset PTSD symptoms. These results are consistent with the large body of prior research that has found insomnia to be a risk factor for new-onset mental illness, particularly depression, in non-military populations.7–19 Given the unique experiences of deployed military personnel relative to the general population, the results of this study significantly add to this body of research.
Other investigations have documented mental health symptoms among recently deployed US service members. Using the Post-Deployment Health Assessment survey, the prevalence of mental health problems among service members returning from Iraq and Afghanistan was 20.3%1 and 19.1%35 (42.4% in Reservists).1 In contrast, our study captured new-onset cases, thereby excluding those who screened positive predeployment for PTSD, depression, and anxiety, which might explain why our postdeployment rates were lower than in past studies. Our prospective results are consistent with previous findings of an increased risk of mental disorders following exposures to combat,36–38 but they are the first to show that insomnia symptoms may confer further susceptibility among military personnel. However, by early identification of those most vulnerable, the potential exists for the designing and testing of preventive strategies that may reduce the occurrence of PTSD, anxiety, and depression.
One of the more interesting findings of this study is not only the degree of risk conferred by predeployment insomnia symptoms, but also the relative magnitude of this risk compared with combat-related trauma. The risk conferred by insomnia symptoms was almost as strong as our measure of combat exposure in adjusted models. There is evidence demonstrating a temporal relationship between insomnia symptoms and the future development of mental disorders, but empirically based explanations for these relationships are limited.6,39–46 The mechanisms linking insomnia symptoms and mental health may involve processes related to specific sleep stages. REM sleep mechanisms are one potential candidate, given that REM fragmentation has been proposed in the development of PTSD.41,47 Alternatively, cognitive mechanisms may be implicated, such as those involved in rumination/worry or coping. Future research should investigate the causal pathways linking insomnia symptoms and new-onset mental health disorders.48
A consistent theme of these findings is the association between insomnia symptoms and newly screening positive for mental disorders. Less consistent is the association between perceived sleep duration, with shorter and longer sleep duration associated with higher odds of PTSD, shorter sleep duration only for anxiety, and neither for depression. Insomnia symptoms as opposed to perceived sleep quantity, therefore, emerge from these results as a more consistent predictor of mental health outcomes. This is consistent with a study among girls at higher risk for depression who reported insomnia symptoms but not short sleep duration.49 It may be that short sleep would be a more significant risk factor in those with higher sleep need, but there are currently no clear means of assessing individual sleep requirements that would allow these patterns to be further explored. There is also a growing body of literature assessing health outcomes among those with insomnia and short sleep duration that has demonstrated this group is at increased risk for hypertension,50–53 type 2 diabetes,54 mental illness,55,56 and mortality.57,58 Findings from this study support and add to the previous literature, suggesting that this unique group may need additional research and interventions.
The relationship between combat-related trauma and mental disorders has been documented in other studies from this cohort.2,3,59 Insomnia symptoms have also been shown to be a risk factor for depression,7–19 as was confirmed in this study. Although we hypothesized that insomnia symptoms would modify the relationship between combat and new-onset mental disorders, this effect modification was only statistically signifi-cant for depression. Furthermore, the interaction was opposite the expected direction, with the odds of depression associated with insomnia symptoms and combat-related trauma lower than would have been expected from the multiplicative product of the odds ratio for each exposure measured separately. Thus, insomnia symptoms prior to deployment did not amplify the elevation in risk of postdeployment depression associated with combat-related trauma. Perhaps there is a unique biological aspect to the development of depression versus the development of PTSD, which appears to have a stronger, independent association with combat-related trauma regardless of insomnia symptoms.
This study had several limitations that must be noted. The variable “insomnia symptoms” was created using the sleep items found on the PCL-C and the anxiety scale on the PHQ. While the PHQ and PCL-C are validated instruments, those specific sleep items have not been validated for use as a measure of insomnia symptoms. Also, our measure of combat exposure is based on witnessing or being exposed to combat-related trauma, but is not a direct measure of active engagement in combat, so it is not clear if it is combat per se that was associated with an increased risk of new-onset mental illness. In addition, 84% of our eligible study population had complete data for final models. However, among those removed from the analyses due to missing outcome data, approximately 15% reported insomnia symptoms and the mean sleep duration was 6.7 hours; this was very similar to the prevalence of insomnia symptoms (17%) and mean sleep duration (6.6-6.7 h) of those included in analyses. Since we are unable to ascertain whether these individuals developed a mental disorder following deployment, these missing data may have biased our results in either direction. However, an examination of nonresponse bias in the Millennium Cohort has shown that prospective analyses are not substantially biased by nonresponse.60 Self-reported data may be subject to recall bias and may not represent the true prevalence of a characteristic, although investigation of this cohort suggests that participant data are reliable for health and military data (e.g., vaccinations and occupations).61–64 Furthermore, since the burden of mental disorders may be underrepresented in medical record data because not all individuals seek care, screening tools on confidential surveys may have captured a greater burden of disease. Finally, overestimations of nightly sleep duration have been reported in normal sleepers,65,66 while those with insomnia tend to underestimate their actual sleep duration.67
Despite these limitations, this study had many strengths. The exposure of interest, sleep disturbance, was measured in 2 ways: sleep duration and insomnia symptoms. The study included participants from all branches and components of the service, and our population was stratified by timing of first deployment, which accounted for issues like operational tempo, for which we could not otherwise control. The study had a large sample size and information on many covariates, allowing us to control for potential confounders, including important deployment-related characteristics. In addition, this study was longitudinal in design, with two consecutive surveys for all participants.
Temporal patterns of the relationship between insomnia symptoms, traumatic exposures, and the development of mental disorders among military suggest a potential role for predeployment screening to identify persons at higher risk for postdeployment mental disorders. Insomnia symptoms could be a marker of vulnerability to mental disorders, an early manifestation of illness, or represent reduced capacity for emotional or physical resources to deal with stressors, thus hindering recovery from posttraumatic stress reactions.5,6,13 Notably, resolution of sleep disorders has previously been associated with reduced incidence of psychiatric disorders.13 Future studies are needed to investigate whether routine inquiry of insomnia symptoms and application of appropriate early, effective interventions reduces subsequent morbidity from mental disorders. In a military population, assessment of insomnia symptoms could be incorporated into routine predeployment screening. Insomnia symptoms are important predictors of future mental health, and both sleep quality and quantity should be considered as indicative of future vulnerability to mental disorders.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the Millennium Cohort Study participants, without whom these analyses would not be possible. We thank Scott Seggerman from the Management Information Division, US Defense Manpower Data Center, Seaside, California; Michelle LeWark from the Naval Health Research Center; and all the professionals from the US Army Medical Research and Materiel Command, especially those from the Military Operational Medicine Research Program, Fort Detrick, Maryland. We appreciate the support of the Henry M. Jackson Foundation for the Advancement of Military Medicine, Rockville, Maryland.
Funding: The Millennium Cohort Study is funded through the Military Operational Medicine Research Program of the US Army Medical Research and Materiel Command, Fort Detrick, Maryland. VA Puget Sound Health Care System provided support for Dr. Boyko's involvement in this research. Dr. Ulmer was supported by a VA Career Development Award (CDA 09-218). The funding organization had no role in the design and conduct of the study; collection, analysis, or preparation of data; or preparation, review, or approval of the manuscript.
Additional Contributions: In addition to the authors, the Millennium Cohort Study Team includes Melissa Bagnell, Nancy Crum-Cianflone, Nisara Granado, Jaime Horton, Andrea Ippolito, Kelly Jones, Lauren Kipp, Cynthia LeardMann, William Lee, Gordon Lynch, Amanda Pietrucha, Teresa Powell, Beverly Sheppard, Katherine Snell, Steven Speigle, Kari Sausedo, Besa Smith, Jennifer Walstrom, Lawrence Wang, John Wessner, Martin White, James Whitmer, and Charlene Wong, from the Department of Deployment Health Research, Naval Health Research Center, San Diego, California; Paul Amoroso, from the MultiCare Health System Research Institute, Tacoma, Washington; Margaret Ryan from the Naval Hospital Camp Pendleton, Camp Pendleton, California; and Timothy Wells, from OptumInsight, Ann Arbor, MI.
Disclaimer: This article represents report 12-03, supported by the Department of Defense, under work unit number 60002. The views expressed in this work are those of the authors, and do not reflect the official policy or position of the Department of the Navy, Department of the Army, Department of the Air Force, Department of Veterans Affairs, Department of Defense, or the US Government. Approved for public release; distribution is unlimited. Human subjects participated in this study after giving their free and informed consent. This research has been conducted in compliance with all applicable federal regulations governing the protection of human subjects in research.
Footnotes
A commentary on this article appears in this issue on page 967.
REFERENCES
- 1.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the iraq war. JAMA. 2007;298:2141–8. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 2.Wells TS, LeardMann CA, Fortuna SO, et al. A prospective study of depression following combat deployment in support of the wars in iraq and afghanistan. Am J Public Health. 2009;100:90–100. doi: 10.2105/AJPH.2008.155432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith TC, Ryan MA, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: Prospective population based us military cohort study. BMJ. 2008;336:366–71. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seelig AD, Jacobson IJ, Smith B, et al. Sleep patterns before, during and after deployment to iraq and afghanistan. Sleep. 2010;33:1615–22. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and ptsd: A critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bryant RA, Creamer M, O'Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69–74. doi: 10.1093/sleep/33.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hohagen F, Rink K, Kappler C, et al. Prevalence and treatment of insomnia in general practice. A longitudinal study. Eur Arch Psychiatry Clin Neurosci. 1993;242:329–36. doi: 10.1007/BF02190245. [DOI] [PubMed] [Google Scholar]
- 8.Brabbins CJ, Dewey ME, Copeland JRM, et al. Insomnia in the elderly - prevalence, gender differences and relationships with mobidity and mortality. Int J Geriatr Psychiatry. 1993;8:473–80. [Google Scholar]
- 9.Riemann D, Voderholzer U. Primary insomnia: A risk factor to develop depression? J Affect Disord. 2003;76:255–9. doi: 10.1016/s0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- 10.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 11.Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression - the Johns Hopkins Precursors Study. Am J Epidemiol. 1997;146:105–14. doi: 10.1093/oxfordjournals.aje.a009241. [DOI] [PubMed] [Google Scholar]
- 12.Eaton WW, Badawi M, Melton B. Prodromes and precursors - epidemio-logic data for primary prevention of disorders with slow onset. Am J Psychiatry. 1995;152:967–72. doi: 10.1176/ajp.152.7.967. [DOI] [PubMed] [Google Scholar]
- 13.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 14.Livingston G, Blizard B, Mann A. Does sleep disturbance predict depression in elderly people - a study in Inner London. Br J Gen Pract. 1993;43:445–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Vollrath M, Wicki W, Angst J. The Zurich study. Viii. Insomnia: Association with depression, anxiety, somatic syndromes, and course of insomnia. Eur Arch Psychiatry Neurol Sci. 1989;239:113–24. doi: 10.1007/BF01759584. [DOI] [PubMed] [Google Scholar]
- 16.Paffenbarger RS, Jr., Lee IM, Leung R. Physical activity and personal characteristics associated with depression and suicide in american college men. Acta Psychiatr Scand Suppl. 1994;377:16–22. doi: 10.1111/j.1600-0447.1994.tb05796.x. [DOI] [PubMed] [Google Scholar]
- 17.Morin CM, Kowatch RA, Barry T, Walton E. Cognitive-behavior therapy for late-life insomnia. J Consult Clin Psychol. 1993;61:137–46. doi: 10.1037//0022-006x.61.1.137. [DOI] [PubMed] [Google Scholar]
- 18.Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission of insomnia among elderly adults: An epidemiologic study of 6,800 persons over three years. Sleep. 1999;22(Suppl 2):S366–72. [PubMed] [Google Scholar]
- 19.Weissman MM, Greenwald S, NinoMurcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. Gen Hosp Psychiatry. 1997;19:245–50. doi: 10.1016/s0163-8343(97)00056-x. [DOI] [PubMed] [Google Scholar]
- 20.Ryan MA, Smith TC, Smith B, et al. Millennium cohort: Enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. 2007;60:181–91. doi: 10.1016/j.jclinepi.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 21.Gray GC, Chesbrough KB, Ryan MA, et al. The millennium cohort study: A 21-year prospective cohort study of 140,000 military personnel. Mil Med. 2002;167:483–8. [PubMed] [Google Scholar]
- 22.Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. 2008;300:663–75. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 24.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11:213–8. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of prime-md: The phq primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The prime-md 1000 study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 27.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Annual Meeting of the International Society for Traumatic Stress Studies; 1993 October; San Antonio, Texas. 1993. [Google Scholar]
- 28.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the ptsd checklist (PCL) Behav Res Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 29.Association AP. 4 ed. American Psychiatric Association; 2000. Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR) [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fann JR, Bombardier CH, Dikmen S, et al. Validity of the patient health questionnaire-9 in assessing depression following traumatic brain injury. J Head Trauma Rehabil. 2005;20:501–11. doi: 10.1097/00001199-200511000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the prime-md patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: The prime-md patient health questionnaire obstetrics-gynecology study. Am J Obstet Gynecol. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 33.Beals J, Manson SM, Shore JH, et al. The prevalence of posttraumatic stress disorder among american indian vietnam veterans: Disparities and context. J Trauma Stress. 2002;15:89–97. doi: 10.1023/A:1014894506325. [DOI] [PubMed] [Google Scholar]
- 34.Loo CM. Race-related PTSD: The Asian American Vietnam veteran. J Trauma Stress. 1994;7:637–56. doi: 10.1007/BF02103012. [DOI] [PubMed] [Google Scholar]
- 35.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–32. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 36.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 37.Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, Rath MB. Prospective risk factors for new-onset post-traumatic stress disorder in national guard soldiers deployed to Iraq. Psychol Med. 2011;41:687–98. doi: 10.1017/S0033291710002047. [DOI] [PubMed] [Google Scholar]
- 38.Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and national guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry. 2010;67:614–23. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- 39.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: A 1-year prospective study of injured survivors of motor vehicle accidents. Am J Psychiatry. 2002;159:855–7. doi: 10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- 41.Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. Rem sleep and the early development of posttraumatic stress disorder. Am J Psychiatry. 2002;159:1696–701. doi: 10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- 42.Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: Secondary symptom or core feature? Sleep Med Rev. 2008;12:169–84. doi: 10.1016/j.smrv.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 43.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 44.Franzen PL, Buysse DJ. Sleep disturbances and depression: Risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10:473–81. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perlis M, Shaw PJ, Cano G, Espie CA. Models of insomnia. In: Kryger MH, Roth T, Dement WC, editors. Principles and practices of sleep medicine. St. Louis: Elsevier; 2011. [Google Scholar]
- 46.Peterson MJ, Bence RM. Mood disorders. In: Kryger MH, Roth T, Dement WC, editors. Principles and practices of sleep medicine. St Louis: Elsevier; 2011. [Google Scholar]
- 47.Mellman TA, Knorr BR, Pigeon WR, Leiter JC, Akay M. Heart rate variability during sleep and the early development of posttraumatic stress disorder. Biol Psychiatry. 2004;55:953–6. doi: 10.1016/j.biopsych.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 48.Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the vietnam generation: Findings from a nationally representative sample of male vietnam veterans. Am J Psychiatry. 1998;155:929–33. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- 49.Chen MC, Burley HW, Gotlib IH. Reduced sleep quality in healthy girls at risk for depression. J Sleep Res. 2012;21:68–72. doi: 10.1111/j.1365-2869.2011.00934.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: Analyses of the first national health and nutrition examination survey. Hypertension. 2006;47:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 51.Johansson JK, Kronholm E, Jula AM. Variability in home-measured blood pressure and heart rate: Associations with self-reported insomnia and sleep duration. J Hypertens. 2011;29:1897–905. doi: 10.1097/HJH.0b013e32834abccd. [DOI] [PubMed] [Google Scholar]
- 52.Fernandez-Mendoza J, Vgontzas AN, Liao D, et al. Insomnia with objective short sleep duration and incident hypertension: The Penn State Cohort. Hypertension. 2012;60:929–35. doi: 10.1161/HYPERTENSIONAHA.112.193268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–7. doi: 10.1093/sleep/32.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: A population-based study. Diabetes Care. 2009;32:1980–5. doi: 10.2337/dc09-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: The role of objective short sleep duration and mental health. Sleep. 2012;35:61–8. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Troxel WM, Kupfer DJ, Reynolds CF, 3rd, et al. Insomnia and objectively measured sleep disturbances predict treatment outcome in depressed patients treated with psychotherapy or psychotherapy-pharmacotherapy combinations. J Clin Psychiatry. 2012;73:478–85. doi: 10.4088/JCP.11m07184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chien KL, Chen PC, Hsu HC, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: Report from a community-based cohort. Sleep. 2010;33:177–84. doi: 10.1093/sleep/33.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vgontzas AN, Liao D, Pejovic S, et al. Insomnia with short sleep duration and mortality: The Penn State Cohort. Sleep. 2010;33:1159–64. doi: 10.1093/sleep/33.9.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jacobson IG, Smith TC, Smith B, et al. Disordered eating and weight changes after deployment: Longitudinal assessment of a large us military cohort. Am J Epidemiol. 2009;169:415–27. doi: 10.1093/aje/kwn366. [DOI] [PubMed] [Google Scholar]
- 60.Littman AJ, Boyko EJ, Jacobson IG, et al. Assessing nonresponse bias at follow-up in a large prospective cohort of relatively young and mobile military service members. BMC Med Res Methodol. 2010;10:99. doi: 10.1186/1471-2288-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smith TC, Jacobson IG, Smith B, Hooper TI, Ryan MA, Team FT. The occupational role of women in military service: Validation of occupation and prevalence of exposures in the millennium cohort study. Int J Environ Health Res. 2007;17:271–84. doi: 10.1080/09603120701372243. [DOI] [PubMed] [Google Scholar]
- 62.Smith B, Leard CA, Smith TC, Reed RJ, Ryan MA. Anthrax vaccination in the millennium cohort: Validation and measures of health. Am J Prev Med. 2007;32:347–53. doi: 10.1016/j.amepre.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 63.Smith TC, Smith B, Jacobson IG, Corbeil TE, Ryan MA. Reliability of standard health assessment instruments in a large, population-based cohort study. Ann Epidemiol. 2007;17:525–32. doi: 10.1016/j.annepidem.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 64.LeardMann CA, Smith B, Smith TC, Wells TS, Ryan MA. Smallpox vaccination: Comparison of self-reported and electronic vaccine records in the millennium cohort study. Hum Vaccin. 2007;3:245–51. doi: 10.4161/hv.4589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gehrman P, Matt GE, Turingan M, Dinh Q, Ancoli-Israel S. Towards an understanding of self-reports of sleep. J Sleep Res. 2002;11:229–36. doi: 10.1046/j.1365-2869.2002.00306.x. [DOI] [PubMed] [Google Scholar]
- 66.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: How similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Edinger JD, Fins AI. The distribution and clinical significance of sleep time misperceptions among insomniacs. Sleep. 1995;18:232–9. doi: 10.1093/sleep/18.4.232. [DOI] [PubMed] [Google Scholar]


