Abstract
Purpose:
To identify the fracture patterns and mechanism of injury, based on subaxial cervical spine injury classification system (SLIC), on non-contrast computed tomography (NCCT) of cervical spine predictive of vertebral artery injury (VAI).
Patients and Methods:
We retrospectively analyzed cervical spine magnetic resonance imaging (MRI) of 320 patients who were admitted with cervical spine injury in our level I regional trauma center over a period of two years (April 2010 to April 2012). Diagnosis of VAI was based on hyperintensity replacing the flow void on a T2-weighted axial image. NCCT images of the selected 43 patients with MRI diagnosis of VAI were then assessed for the pattern of injury. The cervical spinal injuries were classified into those involving the C1 and C2 and subaxial spine. For the latter, SLIC was used.
Results:
A total of 47 VAI were analyzed in 43 patients. Only one patient with VAI on MRI had no detectable abnormality on NCCT. C1 and C2 injuries were found in one and six patients respectively. In subaxial injuries, the most common mechanism of injury was distraction (37.5%) with facet dislocation with or without fracture representing the most common pattern of injury (55%). C5 was the single most common affected vertebral level. Extension to foramen transversarium was present in 20 (42.5%) cases.
Conclusion:
CT represents a robust screening tool for patients with VAI. VAI should be suspected in patients with facet dislocation with or without fractures, foramina transversarium fractures and C1-C3 fractures, especially type III odontoid fractures and distraction mechanism of injury.
Keywords: Blunt cerebrovascular injury, cervical spine injury, magnetic resonance imaging, vertebral artery injury
INTRODUCTION
Blunt cerebrovascular injuries (BCVI) comprise both carotid artery and vertebral artery injuries. BCVI are encountered in 1% cases of blunt trauma cases.[1] Vertebral artery injuries (VAI) occur in 17-46% patients of blunt cervical spine injury.[2–4] Clinical diagnosis of VAI has notoriously low sensitivity and specificity as majority of patients are asymptomatic for the initial 72 h after injury.[5] This coupled with the devastating consequences of a missed VAI mandates correct diagnosis at an early stage so that an appropriate anticoagulation regimen keeps the incidence of any attendant complications within acceptable limits. An enormous scientific data supports the use of computed tomography over radiography in patients who do not clear the clinical criteria to exclude cervical spine injury (National Emergency X-Radiography Utilization Study and the Canadian Cervical Spine rule).[6,7] CT has also been proposed by the current American college of Radiology appropriateness criteria for all patients with suspected cervical spine injuries.[8] This provides an opportunity to identify patients at high risk for BCVI including VAI using the specific CT patterns of injury.[9] This will guide a more refined and cost effective approach for further management of patients deemed at high risk of BCVI. We conducted a retrospective study at level I trauma center with the objective to strengthen the available data regarding the patterns of cervical spine injury predicting VAI.
MATERIALS AND METHODS
We conducted a retrospective study at our level I trauma center which is the apex trauma center with referral from all parts of the country. Patients with age range 18 to 99 years and mean age of 38 years, who underwent cervical spine MRI as a part of their cervical spine injury evaluation during some part of their hospital stay were selected. MRI was performed on 1.5 T system (Avanto, Seimens, Germany) using a cervical multi-array phase coil. The presumptive diagnosis of VAI was based on analysis of axial T2-weighted MRI (TE 91 msec, TR 4100 msec). Crescentic hyperintensity involving the wall of a vertebral artery with complete loss of flow void was considered indicative of VAI [Figure 1a]. In cases where time of flight angiography (TOF) was available, it was considered as a supportive evidence of VAI [Figure 1b]. CT studies of all positive cases were then retrieved from our database. CT was performed using a 40-detector system (Sensation, Seimens, Germany). Images were acquired using 0.6 mm collimation, 0.6 sec rotation time, 120 kV voltage, automodulation current protocol, pitch of 0.7 and anatomic coverage from above foramen magnum to T2 vertebral body. We analyzed 2-mm thick axial sections with a 1-mm reconstruction interval, with routine 1.5-mm-thick coronal and sagittal reformations. Images were assessed in bone window for the pattern of fractures or dislocations. Soft tissue window was not evaluated. We broadly classified the cervical spine injuries into those involving the C1 and C2 and those involving the subaxial spine. The latter injuries were further assessed based on classification system (the subaxial cervical spine injury classification system) recently proposed by Vaccaro et al.[9] The subaxial injuries were classified into one of the mechanisms: compression, distraction and rotation/translation. Among each of these groups, further analysis was done to identify individual injuries: facet dislocation, facet fracture dislocation, facet dislocation without fracture, pedicle fracture, fracture of lateral mass and spinous process, compression/burst fracture of the vertebral body. In each of the above mentioned injury, extension into foramen transversarium was carefully assessed on consecutive axial images.
Figure 1.
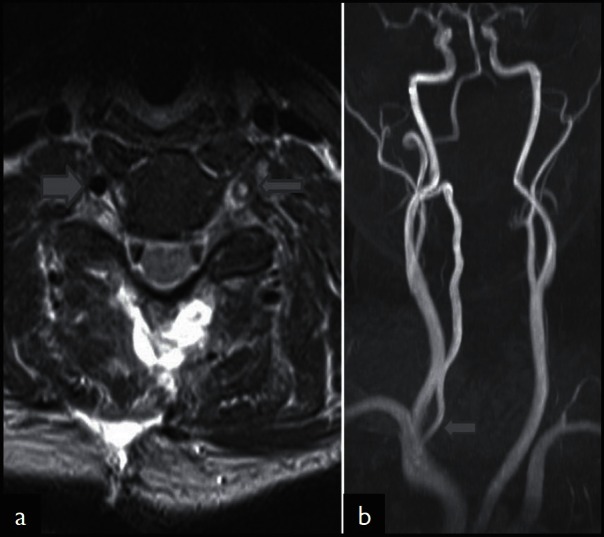
MRI detection of vertebral artery injury. Axial T2-weighted MRI (TE 91 msec; TR 4100 msec; (a) shows hyperintensity in the region of left vertebral artery flow void (thin arrow). The right vertebral artery shows normal flow void (thick arrow). Coronal maximal intensity projection (MIP) of TOF angiography (b) reveals the absent left vertebral artery. The right vertebral artery shows normal flow related enhancement (arrow)
RESULTS
From April 2010 to April 2012, 320 patients had cervical spine MRI. Analysis of these MRI images using the criteria mentioned above yielded 47 VAI in 43 patients. Majority of our patients were males with only six females (14%). Bilateral VAI were noted in four patients (9%) with right sided VAI (66%) distinctly more common than left (34%). Fractures of cervical spine were noted in 36 (76.5%) patients. C1, C2 fractures were noted in 7 patients (15%). Most common among these were type III odontoid fractures noted in four patients [Figure 2]. Single patient with C1 fracture had unilateral fracture of anterior and posterior arch. Among the subaxial injuries, translation/ rotation was the most common mechanism of injury (37.5%), followed by compression (27.5%) and distraction (22.5%). Facet dislocation with or without fracture was noted in 26 cases of VAI (55%). It represented the commonest subaxial pattern of injury [Figure 3]. Three patients had facet fracture without dislocation secondary to a compression type of injury [Figure 4]. The commonest level of dislocation was C5 over C6 followed C4 over C5. However, all levels of facet dislocations were associated with VAI. Of significance was the fact that in 20 cases (42.5%) of VAI, there was extension of the fracture through the foramen transversarium [Figure 5]. This extension was most commonly associated with translation/rotation (60%), followed by compression (30%) and distraction (10%) type of injury. Pedicle fractures were noted in 14 cases [Figure 6]. Again translation type of injuries had highest association with these fractures (71%) followed by compression (29%). Spinous process fractures, compression fractures and burst fractures of subaxial vertebrae were noted in 2 (4%), 3 (6%), and 2 (2%) cases respectively. Tables 1 and 2 summarises the important results.
Figure 2.
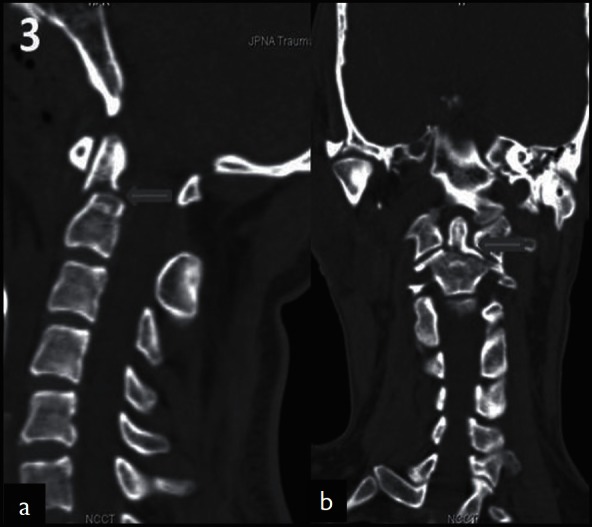
Type 3 odontoid fracture. Sagittal reformatted image (a) of the cervical spine shows fracture of the odontoid process which on the (b) coronal reformatted image is clearly seen to extend to the body of C2. This patient had thrombosis of right vertebral artery
Figure 3.
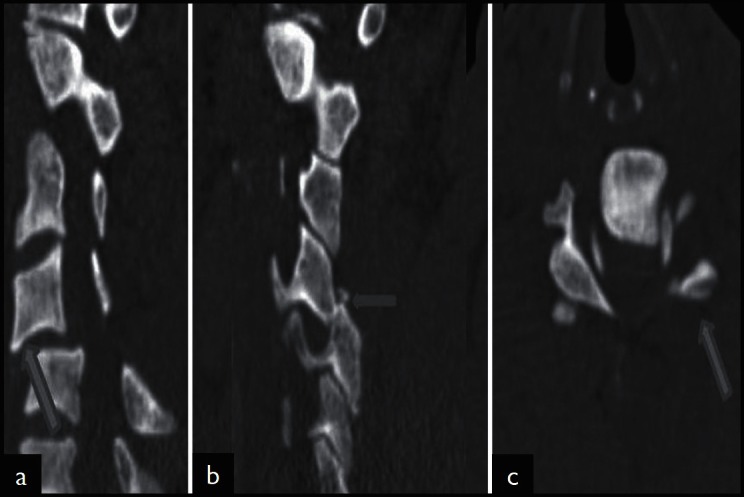
Facet dislocation. Mid sagittal reformatted image (a) shows grade 2 anterolisthesis of C4 over C5. Left parasagittal image (b) reveals locked left facet of C4 over C5. Axial image at the affected level (c) shows the ‘reverse hamburger sign’ on left suggestive of locked facet
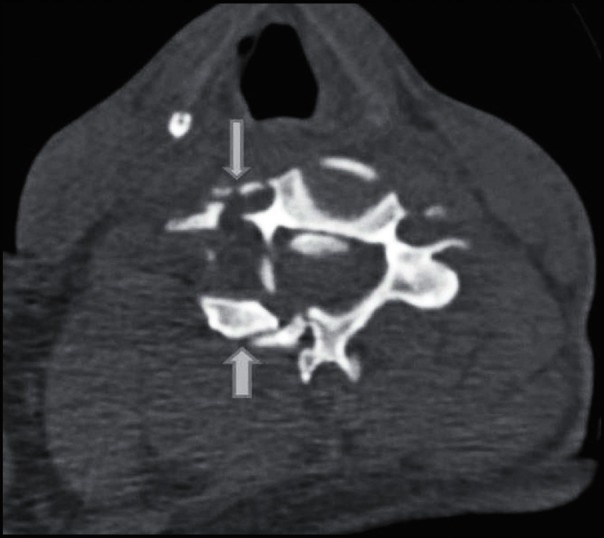
Figure 4.
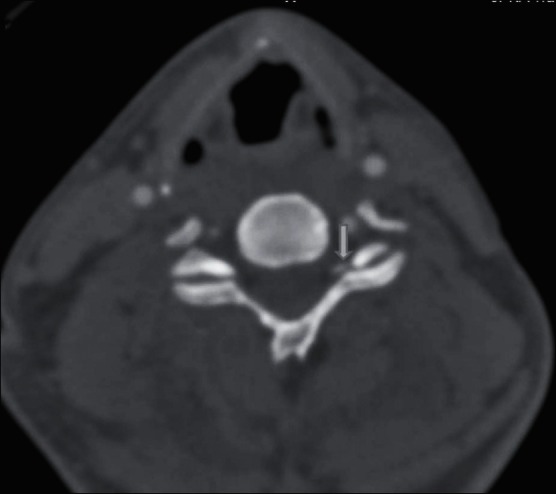
Facet fracture without dislocation. Axial CT image reveals fracture of left C4 facet without dislocation (arrow)
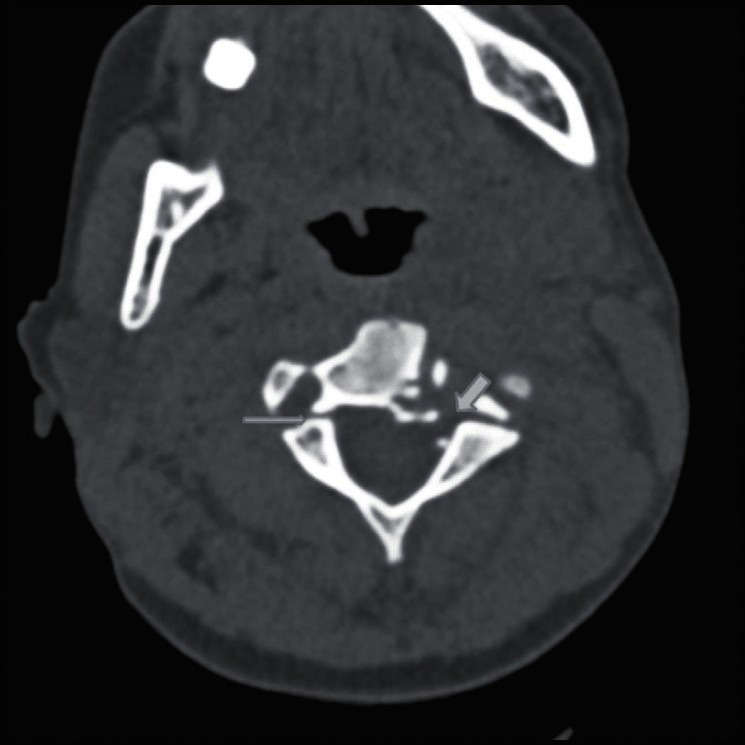
Figure 5.
Extension into foramen transversarium. Axial CT shows extensive fracture of C4 vertebra involving right pedicle, lamina, lateral mass (thick arrow) with extension to right foramen transversarium (thin arrow)
Figure 6.
Pedicle fracture. Axial CT reveals bilateral pedicle fracture (arrows) of C3 vertebra
Table 1.
VAI distribution based on age, sex and side
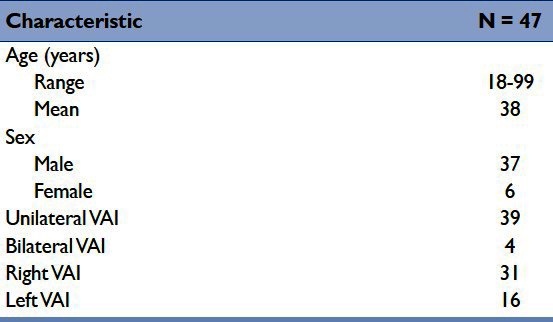
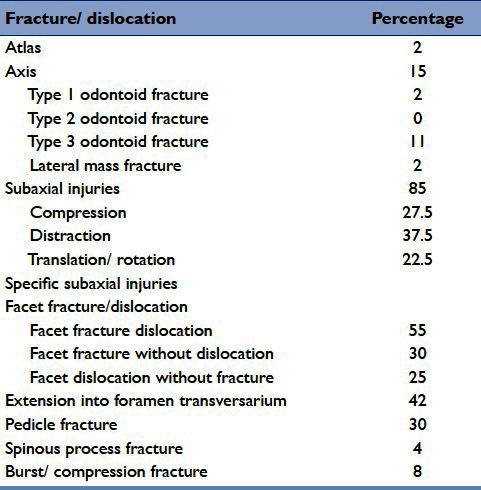
Table 2.
Fracture/ dislocation patterns associated with VAI
DISCUSSION
BCVI represent typical example of missed injury during primary survey of trauma patients. This is due to the lack of neurological symptoms or signs in the hyperacute/ acute stage, exposing the patient to significant neurological damage at a later stage. Untreated VAI over all grades have a stroke rate of 24%.[4] It has been shown that prompt recognition and institution of antithrombotic measures reduces stroke rates in VAI.[4,10,11] This places a significant importance on early suspicion and possibly prediction of VAI during primary survey of trauma patients. This could be accomplished using CT findings predictive of VAI as CT is now preferred over plain radiography for spine imaging and has also been proposed by the current American college of Radiology appropriateness criteria for all patients with suspected cervical spine injuries.[8]
The association of VAI with cervical spine fracture was reported more a decade ago when it was found that cervical spine fractures are independent predictors of VAI.[12] Several researchers have subsequently found that almost 70% of VAI are associated with fractures of cervical spine.[11] More recent studies have attempted to analyze fracture patterns in VAI.[13,14] This has led to identification of several patterns of fracture more commonly in patients with VAI than those without VAI. We also retrospectively analyzed the CT patterns of cervical spine injuries in patients with VAI with inclusion of recently proposed Subaxial Cervical Spine Injury Classification System.[9] The aim was to strengthen the existing evidence supporting the use of CT finding in early screening of patients with VAI to improve their final outcome.
Vertebral artery usually arises from subclavian artery and can be divided into 4 segments. The first segment designated V1 represents the extraosseous segment and extends from the origin at the subclavian artery to the transverse foramen of the sixth cervical vertebra (C6). In 5% of the population, however, the vertebral artery enters a transverse foramen at C7. The foraminal segment (V2) is the segment of vertebral artery passing through the transverse foramen of C6 to C1. The extraspinal segment (V3) starts as the artery exits the foramen transversarium of C1 and courses posteromedially along the upper surface of the posterior arch of atlas before coursing ventral and cephalad to enter the foramen magnum. It ends after penetrating the dura at the foramen magnum. The intradural segment is the last segment that extends to the pontomedullary junction.[15] The two vertebral arteries unite here to form the basilar artery.
Thus the vertebral artery is exposed to injury throughout its course. Vertebral artery injuries can result from direct trauma from fracture fragments or from excessive stretching in dislocations.[16] We found fractures of cervical spine in 36 (76.5%) of our patients. Eleven patients (23.5%) had facet dislocation without fractures.
C1 and C2 spine fractures were noted in 15% patients; of this only one patient had C1 arch fracture (2%). Cothren et al. reported C1 arch fractures in 9% patients.[13] Odontoid fractures were present in five of the six patients with C2 fractures. Type III odontoid fracture was most common pattern in four patients (11%) with type I found in one patient. Jang et al. reported a single case of type III odontoid fracture in their prospective study of 99 patients with 7 cases of VAI, representing 14% cases.[17]
The most common cervical spine injuries associated with VIA were however, those that involved the subaxial spine. In 2007 Vaccaro et al. proposed the subaxial cervical spine injury classification system based on morphology of fracture (as detected by plain radiography, CT or MRI); neurological status of the patient and integrity of disco-ligamentous complex.[9] In our retrospective study, we followed the morphology component of this classification system [Table 3] to relate VAI to a specific mechanism of injury. We found that translation/ rotation was the most common mechanism of injury (37.5%), followed by compression (27.5%) and distraction (22.5%). The predominance of translation/rotation mechanism is not unexpected as it represents the highest impact injury. However, the greater frequency of compression injuries compared to distraction (though the latter represents greater anatomic disruption and instability) in VAI is likely the result of preponderance of lateral compression in our series with resultant extension of fracture through foramen transversarium. Foraminal extension was most common in translation/rotation injury (60%), followed by compression (30%) and distraction (10%).
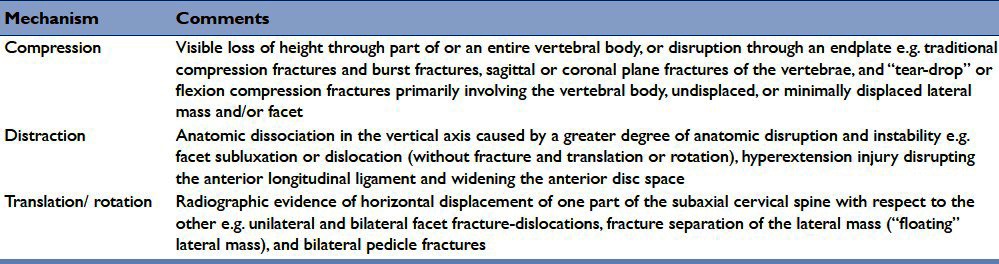
Table 3.
SLIC fracture morphology with associated mechanism (modified from 8)
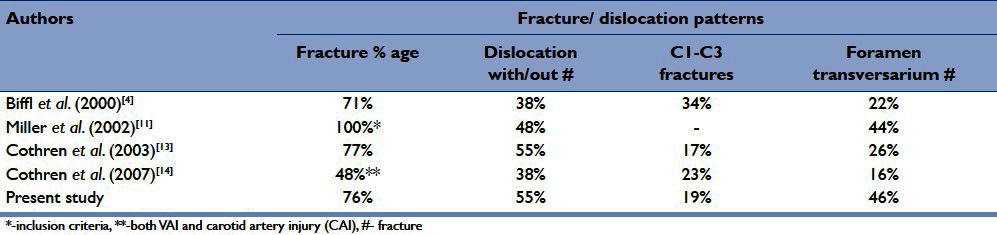
The most common subaxial pattern of injury was facet dislocation with or without fracture in 26 (55%) patients. The commonest level of dislocation was C5 over C6 followed C4 over C5. However, all levels of facet dislocations were associated with VAI. Facet fractures without dislocation were noted in three (6%) patients. As already stated fracture extension through foramen transversarium is an important predictor of VAI; it was present in 20 (46.5%) cases. Pedicle fractures (unilateral or bilateral) were noted in 14 (30%) cases. Least common fracture patterns were isolated spinous process fractures and compression or burst fractures of vertebral bodies. The comparison with results of various studies is depicted in Table 4.
Table 4.
Comparison of various studies on fracture/ dislocation patterns associated with vertebral artery
In conclusion, CT represents a robust screening tool for patients with VAI. VAI should be suspected in patients with facet dislocation with or without fractures, foramina transversarium fractures and C1-C3 fractures, especially type III odontoid fractures. The CT study can then be coupled with CT angiography to confirm the diagnosis and hence hasten the anticoagulation therapy to decrease the devastating consequences of VAI.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bromberg WJ, Collier BC, Diebel LN, Dwyer KM, Holevar MR, Jacobs DG, et al. Blunt cerebrovascular injury prac-tice management guidelines: The Eastern Association for the Surgery of Trauma. J Trauma. 2010;68:471–7. doi: 10.1097/TA.0b013e3181cb43da. [DOI] [PubMed] [Google Scholar]
- 2.Oetgen ME, Lawrence BD, Yue JJ. Does the morphology of foramen transversarium fractures predict vertebral artery in-juries? Spine (Phila Pa 1976) 2008;33:E957–61. doi: 10.1097/BRS.0b013e31818e2f31. [DOI] [PubMed] [Google Scholar]
- 3.Cothren CC, Moore EE, Ray CE, Jr, Johnson JL, Moore B, Burch JM. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery. 2001;141:76–82. doi: 10.1016/j.surg.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Biffl WL, Moore EE, Elliott JP, Ray C, Offner PJ, Franciose RJ, et al. The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000;231:672–81. doi: 10.1097/00000658-200005000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berne JD, Reuland KS, Villarreal DH, McGovern TM, Rowe SA, Norwood SH. Sixteen-slice multi-detector computed tomographic angiography improves the accuracy of screening for blunt cerebrovascular injury. J Trauma. 2006;60:1204–9. doi: 10.1097/01.ta.0000220435.55791.ce. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343:94–9. doi: 10.1056/NEJM200007133430203. [DOI] [PubMed] [Google Scholar]
- 7.Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286:1841–8. doi: 10.1001/jama.286.15.1841. [DOI] [PubMed] [Google Scholar]
- 8.Daffner RH, Hackney DB. ACR Appropriateness Criteria on suspected spine trauma. J Am Coll Radiol. 2007;4:762–75. doi: 10.1016/j.jacr.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA, Jr, et al. The subaxial cervical spine injury classification system: A novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32:2365–74. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 10.Berne JD, Norwood SH, McAuley CE, Villareal DH. Helical computed tomographic angiography: An excellent screening test for blunt cerebrovascular injury. J Trauma. 2004;57:11–7. doi: 10.1097/01.ta.0000135499.70048.c7. [DOI] [PubMed] [Google Scholar]
- 11.Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M, et al. Prospective screening for blunt cerebro-vascular injuries: Analysis of diagnostic m0oalities and outcomes. Ann Surg. 2002;236:386–93. doi: 10.1097/01.SLA.0000027174.01008.A0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: Implications of a new grading scale. J Trauma. 1999;47:845–53. doi: 10.1097/00005373-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Cothren CC, Moore EE, MD, Biffl WL, Ciesla DJ, Ray CE, Jr, Johnson JL, et al. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003;55:811–3. doi: 10.1097/01.TA.0000092700.92587.32. [DOI] [PubMed] [Google Scholar]
- 14.Cothren CC, Moore EE, Ray CE, Jr, Johnson JL, Moore JB, Burch JM. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery. 2007;141:76–82. doi: 10.1016/j.surg.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Gupta S, Goel A. Quantitative anatomy of the lateral masses of the atlas and axis vertebrae. Neurol India. 2000;48:120–5. [PubMed] [Google Scholar]
- 16.Cacciola F, Phalke U, Goel A. Vertebral artery in relationship to C1-C2 vertebrae: An anatomical study. Neurol India. 2004 Jun;52(2):178–84. [PubMed] [Google Scholar]
- 17.Jang J, Lee J, Hur H, Seo B, Lee J, Kim S. Vertebral artery injury after cervical spine trauma: A prospective study using computed tomographic angiography. Surg Neurol Int. 2011;2:39. doi: 10.4103/2152-7806.78255. [DOI] [PMC free article] [PubMed] [Google Scholar]


