Abstract
Background
Homecare is a growth enterprise. The nature of the care provided in the home is growing in complexity. This growth has necessitated both examination and generation of evidence around patient safety in homecare. The purpose of this paper is to examine the findings of a recent scoping review of the homecare literature 2004-2011 using the World Health Organization International Classification for Patient Safety (ICPS), which was developed for use across all care settings, and discuss the utility of the ICPS in the home setting. The scoping review focused on Chronic Obstructive Pulmonary Disease (COPD), and Congestive Heart Failure (CHF); two chronic illnesses commonly managed at home and that represent frequent hospital readmissions. The scoping review identified seven safety markers for homecare: Medication mania; Home alone; A fixed agenda in a foreign language; Strangers in the home; The butcher, the baker, the candlestick maker; Out of pocket: the cost of caring at home; and My health for yours: declining caregiver health.
Methods
The safety markers from the scoping review were mapped to the 10 ICPS high-level classes that comprise 48 concepts and address the continuum of health care: Incident Type, Patient Outcomes, Patient Characteristics, Incident Characteristics, Contributing Factors/Hazards, Organizational Outcomes, Detection, Mitigating Factors, Ameliorating Actions, and Actions Taken to Reduce Risk.
Results
Safety markers identified in the scoping review of the homecare literature mapped to three of the ten ICPS classes: Incident Characteristics, Contributing Factors, and Patient Outcomes.
Conclusion
The ICPS does have applicability to the homecare setting, however there were aspects of safety that were overlooked. A notable example is that the health of the caregiver is inextricably linked to the wellbeing of the patient within the homecare setting. The current concepts within the ICPS classes do not capture this, nor do they capture how care responsibilities are shared among patients, caregivers, and providers.
Background
A steadily increasing demand for homecare services within Canada co-exists with the aging population. It is estimated that within the next 25 years seniors will make up 25% of the population [1]. In addition, The World Health Organization (WHO) 2010 Global Status report [2] indicated that developing one or more chronic illnesses is more likely with advancing age. The increasing reliance on homecare to provide health system services is therefore not surprising. What is surprising is the lack of focus on patient safety within the homecare context. We conducted a scoping review to begin to address this gap by identifying safety related markers for homecare patients, caregivers, and health care providers. A full report of the findings is published elsewhere (http://www.tandfonline.com/eprint/vxHsUwV68wbUXqKheD7p/full#.UaPkpkqmWIQ) [3]. The purpose of this paper is to employ the WHO International Classification for Patient Safety (ICPS) as a lens to re-present our findings. In particular we were interested in the applicability of the ICPS within the homecare context.
Research on patient safety has primarily stemmed from institutional settings. The Victorian Order of Nurses (VON), Canada’s largest not for profit homecare organization, approached the Canadian Patient Safety Institute (CPSI) in 2005 to address patient safety in homecare. Following a national roundtable discussion with researchers and decision makers, CPSI published Broadening the Patient Safety Agenda to Include Homecare[4]. This foundational report identified that the context of care in the home is different than in hospitals or institutional settings and that the health of the homecare patient and caregiver is inextricably linked. In addition, this report confirmed the lack of literature focusing on homecare safety. Subsequently, in 2008, the CPSI formed the Core Safety in Homecare Team with researchers and decision makers to further patient safety research in homecare [5-7]. Included in this program of research was a scoping review of the homecare literature to identify safety related markers for patients, their (unpaid/family) caregivers, and paid health providers. It should be noted that although it is customary within homecare research to use the term clients for those receiving care, we will use the WHO designated term, thus referring to clients as patients. The review focused on the homecare literature surrounding chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF). These two chronic illnesses require a great deal of care, most of which is provided in the home by a family caregiver [8], and have the highest readmission rate to acute care of all medical conditions [9]. In light of the accumulating evidence related to safety in homecare and the absence of literature linking safety in homecare with the ICPS, this manuscript was conceived.
In 2002, the WHO was urged to focus on patient safety and quality of care by developing global norms and standards, as well as supporting efforts to develop patient safety policies and practices. In order to meet this call, the WHO created the World Alliance for Patient Safety in October, 2004. One of its initiatives was to develop an International Classification for Patient Safety (ICPS), and a Drafting Group was formed to meet this initiative [10]. The Drafting Group’s main objective was to “define, harmonize and group patient safety concepts into an internationally agreed classification in a way that is conducive to learning and improving patient safety across systems” [10], p3. In order to meet this objective, the Group followed a set of principles that included developing “categories applicable to the full spectrum of health care settings” [10], p5 and required that that the framework be “a genuine convergence of international perceptions of the main issues related to patient safety” [10], p6. The framework consists of 10 high level classes: 1) Incident Type; 2) Patient Outcomes; 3) Patient Characteristics; 4) Incident Characteristics; 5) Contributing Factors/Hazards; 6) Organizational Outcomes; 7) Detection; 8) Mitigating Factors; 9) Ameliorating Actions; and 10) Actions Taken to Reduce Risk. The framework also consists of a number of associated concepts, and is not considered a comprehensive classification of patient safety [10].
The conceptual framework “was designed to provide a much needed model for organizing patient safety data and information so that it can be aggregated and analyzed to compare patient safety data across disciplines, between organizations, and across time and borders; examine the roles of system and human factors in patient safety; identify potential patient safety issues; and develop priorities and safety solutions” [10], p4. In consideration of its goals, purposes, and principles, we questioned if the ICPS framework was applicable to patient safety within the homecare context. While studies exist demonstrating its successful application to research findings [11,12], there are also those that have critiqued the ICPS and its applicability as a classification system [13]. In all these cases, the ICPS was evaluated through and utilized in clinical institutional settings and contexts. In order to verify this classification system and its potential to apply to “the full spectrum of health care settings” we have used the ICPS as a lens with which to present our scoping review findings.
In this paper we view the results of our scoping review, which identified markers that may compromise the safety of homecare patients and their unpaid caregivers, through the lens of the ICPS. The markers are introduced and explained in the process of examining them through the high classes of the ICPS framework.
Methods
The purpose of a scoping review is to allow the researcher to explore the breadth of a topic, in our case, the home care literature related to COPD and CHF. All research designs are included in the review. Unlike a systematic review, a scoping review does not begin with a defined question [14]. We used the following methods in order to assure trustworthy review findings: describing the sources of the data; developing inclusion/exclusion criteria; searching relevant work based on predetermined criteria; collecting the data; and synthesizing the data and explaining the method for synthesis. The sources of data searched included 12 electronic bibliographic databases and five sources of grey literature. The inclusion/exclusion criteria considered: geographical location of study (North America, European Union, Australia), year of publication (2004-2011), and language (French and English). The predetermined search criteria included the terms COPD and CHF in the title fields, as well as a developed list of search terms. This resulted in 376 articles. Further screening involving a three stage triaging process where selected team members ranked the titles, abstracts, or full-text articles as relevant, potentially relevant, and not relevant, resulted in 180 relevant articles. These articles were analyzed by both researcher and decision-maker team members using interpretive description methods [15] to identify patterns that would represent safety-related markers for patients and their unpaid caregivers.
Results
Applying the 10 high-level classes to findings
The ten high-level classes outlined above have been grouped to enhance meaning. One grouping is Incident Type and Patient Outcomes. The second grouping is context relevant and contains the classes of Patient Characteristics, Incident Characteristics, and Contributing Factors. A third grouping captures information related to prevention, recovery, and system resilience and is comprised of Detection, Mitigating Factors, Ameliorating Actions and Actions Taken to Reduce Risk. The safety markers identified in the scoping review map to the high-level classes as follows: Medication mania fits in Incident Characteristics; Home alone, A fixed agenda in a foreign language, Strangers in the home, and The butcher, the baker, the candlestick maker are Contributing Factors; and Out of pocket: the cost of caring at home and My health for yours: declining caregiver health are Patient Outcomes.
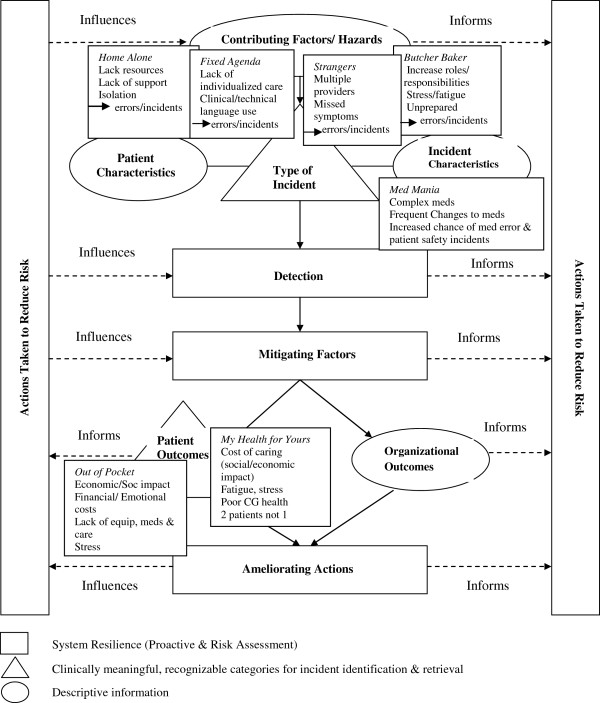
The high-level classes and the safety markers will now be defined, and the markers presented in relation to their fit with the respective high-level classes and associated concepts. The safety marker definitions were derived from the data in the scoping review and used to map the markers to the framework high classes (see Figure 1).
Figure 1.
The conceptual framework for the international classification for patient safety [[10]], p.8. ©WHO, 2009. All Rights Reserved. WHO/IER/PSP/2010.2. Permission obtained for reproduction. The seven safety markers that resulted from our Scoping Review: Medication mania; Home alone; A fixed agenda in a foreign language; Strangers in the home; The butcher, the baker, the candlestick maker; Out of pocket: the cost of caring at home; and My health for yours: declining caregiver health were mapped to the high-level classes of the ICPS. The findings mapped to three of the high-level classes: Contributing Factors/Hazards; Incident Characteristics; and Patient Outcomes as shown.
Incident characteristics
The class Incident Characteristics is defined in the ICPS as classifying the information about the circumstances surrounding the incident such as where and when the incident occurred, who was involved, and who reported the incident. The three main concepts under this class include Origin of Incident, Discovery of Incident, and Reporting of Incident. Medication mania is a safety marker identified through the scoping review that refers to the number and complexity of medications patients are required to take and manage. In viewing this safety marker through the lens of the high-level class Incident Characteristics, it was apparent that the setting of homecare and the role of the unpaid caregivers were recognized. However, we also discovered that while a link existed within this class between the patient and caregiver, the dynamic or importance of the relationship between patient and caregiver was not clearly depicted by the framework.
For instance, this marker can map to the concept of Origin of Incident in considering the complex nature of medication regimes for individuals with chronic illness and the risk of medication errors. Patients with severe heart failure may follow medication regimes that include five or more medications while those with co-morbid conditions may follow regimes with 10 or more medications [16]. For both caregivers and patients, having to monitor such complex regimes may lead to safety concerns such as duplicating, omitting, or misusing medications [17-20]; forgetting or confusing the number of medications to take, when to take, and which medications to avoid mixing [21-23]; medication errors [24,25]; worsening of symptoms and increased exacerbations [24]; higher risk of anxiety and potential overdose [24-28]; and health decline [16,22,25].
These medication errors can be linked to caregivers, either because they manage the regime, or they discover or report the incident. However, the framework does not depict how or why caregivers can be linked to patient medication errors. The framework seems to focus on the care setting and timing of the incident rather than to consider the dynamic and complex relationship that exists between patient and caregiver, health, and care related incidents.
For example, while the Origin of Incident includes the sub-concepts of
‘Who’, listing those who may be involved, including caregivers, and ‘When’ or Stage of Care, listing Homecare and Management of Household Regime, it does not go further to consider the characteristics of the caregiver and the caregiver’s health. These are key considerations because the age and health of the caregiver will determine if he/she also has a medication regime to manage on top of assisting with the patient’s [18,29]. The literature shows that caregivers may experience increased stress when having to monitor both their own medications and that of the homecare patient [18,29]. Additionally, caregivers are more likely to make mistakes as their own health declines under the pressures and burden of their rising care responsibilities [21,30]. Caregivers in the literature reported feeling the expectation to take on multiple responsibilities with little information or preparation regarding how to manage their loved one’s illness [31].
It is evident that while we can view our findings relating to the marker Medication mania through the concepts that exist under Incident Characteristics, the framework relegates caregivers to the role of discovery or reporting of safety-related incidents, thereby missing the true nature of the caregiver’s role in homecare settings and their relationship to the patient and the patient’s health.
Contributing factors/hazards
This class is defined within the ICPS as circumstances, actions, or influences which are thought to have played a part in the origin or development of an incident or to increase risk of an incident. We mapped four safety markers to the high-level class Contributing Factors: Home alone; A fixed agenda in a foreign language; Strangers in the home; and The butcher, the baker, the candlestick maker. Home alone is defined in the scoping review as patients feeling left on their own to deal with their illness without adequate information or support. A fixed agenda in a foreign language is defined as the perception that information offered by health care providers regarding illness often follows a fixed script and uses medical or clinical terminology that can be hard to understand, sounding like a foreign language to patients and caregivers. Strangers in the home is defined as the interaction between homecare patients and the multiple and various health professionals coming into their homes to provide care. And The butcher, the baker, the candlestick maker describes the increasing responsibilities and multiple roles caregivers take on, thus becoming the butcher, the baker, the candlestick maker, and any other role necessary in caring for loved ones.
Many of the concepts associated with Contributing Factors related well to our findings. However, the unique setting of receiving care at home was not accounted for, as we will illustrate. Staff Factors, a concept of Contributing Factors, fit with our findings relating to Home alone, A fixed agenda and Strangers in the home. In these three markers we identified staff communication as a key issue. For example, the literature revealed that patients and caregivers perceived health professionals as lacking time to answer questions, provide clear information, and grasp their individual needs [32,33]. Patients and caregivers also described information, education, or communication provided by health care professionals as insufficient or inadequate, which lead to feelings of neglect, abandonment, and being left on their own to deal with their illness [31,32,34].
In addition, health professionals were seen to provide sporadic information [35,36], use language that was too technical or clinical thus limiting patient and caregiver’s ability to be involved in their own care [37], use euphemisms that weakened understandings of the health issues at hand [38], and provide conflicting information and approaches regarding treatments [38]. This lack of specific information or failure to explain information in clear terms was linked to greater patient anxiety as well as strain on caregivers, leading to mismanagement of symptoms and thus increased patient hospitalizations [32,34,39].
Staff Factors described in the ICPS, such as the sub-concepts of Performance Factors and Behaviour, overlook key staff issues in homecare, such as collaboration and coordination. If providers do not collaborate or coordinate amongst themselves as well as with patients and caregivers, this can negatively impact on patients’ and caregivers’ lives. For instance, patients and caregivers must often work with numerous health professionals from multiple independent agencies [38]. As a result, they may feel overwhelmed, insecure, and uncomfortable with the number of ‘strangers’ in their home, leading to feelings of confusion or being a burden [39,40]. This can, in turn, result in a further decline in overall collaboration among health professionals and patients [39-43], and can contribute to the possibility of: care errors and poor health [30,31,44]; patient stress and fatigue [31,44]; feelings of anxiety and depression from loss of control within the home [36]; and re-hospitalization due to care errors such as the omission or duplication of tasks [31,44].
Patient Factors, another concept within Contributing Factors, is also useful in presenting our findings as the sub-concepts Cognitive, Performance, Behaviour, Communication, Emotional, and Social factors can easily be applied to the four identified markers. For example, the literature shows that aspects associated with patients include difficulties in the reception and comprehension of information due to cognitive impairments such as memory loss or decreased functionality due to illness or medications [45-49]. Challenges with technology also occur as the symptoms of illness, such as diminished attention and slower motor reactions in patients with CHF, make it more difficult for patients to learn to use equipment or devices [19,45,50-52].
Also within Contributing Factors, Emotional, Behavioural, and Social Factors were seen as applicable concepts to our findings. This is illustrated in that a diagnosis of COPD or CHF was strongly linked to: feelings of isolation, depression, anxiety, decreased quality of life, and being housebound or left alone due to the associated symptoms of the illness (breathlessness, fatigue, insomnia, headaches, falls and reduced mobility); unpredictability of disease process and progression; and diminished physical ability, which limits a patient’s ability to participate in activities and social engagements [19,31,34,40,53-56]. Patients also resisted asking for help, which increased feelings of isolation, due to shame, guilt, and embarrassment, or not wanting to be a burden to family or friends [22,31,32]. Cultural and language barriers were also identified as issues whereby the homecare team (patient, caregiver, and health professionals) may not be communicating and understanding each other’s perceptions of health and healing [57].
Despite three of the four markers mapping quite smoothly to the high-level class of Contributing Factors, our third marker, Butcher, baker, candlestick maker, illustrates a weakness in sensitivity of the ICPS framework to the homecare context. Caregivers’ behaviour, performance, cognitive, communication, emotional, and social factors have a significant impact on how the client is cared for at home, and thus should be considered as concepts within this class. Caregivers must take on multiple roles [58,59]; experience changes in family dynamics and boundaries [60,61]; and face an increasing work load in caring for a loved one (see Table 1 for a list of responsibilities described in the literature that caregivers are expected to take on) on top of their existing responsibilities and employment [31,59,62,63]. Assuming these roles and responsibilities can lead to frustration, resentment, anxiety, stress, exhaustion, and declining health [30,35,64-66]. Consequently, patients may be at risk for medical and care errors as their caregiver’s health declines, or abuse from caregivers who feel frustrated or resentful due to increasing demands and stress [21,30,67].
Table 1.
Caregiver responsibilities
| • Medication and symptom management [17,59,61,64,68-71] |
• Physical work (e.g., moving a frail client, bathing, laundry and cleaning, etc.) [18,39,69] |
| • Awareness of hygiene and nutritional needs and exercise regimes [17,32,69,72-74] |
• Use of technical devices and equipment (e.g., defibrillators, IVs, ventricular assistant devices, insulin pens, home dialysis devices, etc.) [17,71,74,79,80] |
| • Providing physical, psychological and emotional support (e.g., transportation, company or social support) [42,69,74-76]. | |
| • Managing client behaviours and temperaments [18,29,75,81] | |
| • Emergency management of issues (e.g., trouble breathing, pain management, recognizing signs and symptoms of problems) [18,69,71,77,78] | |
| • Handling household and illness related finances [59,68,75] | |
| • Carrying out decision making and problem solving needs [21,73,82] |
An additional shortcoming within Contributing Factors is that the concept Work/Environment Factors is primarily framed within an institutional model, neglecting to consider the blurred lines that exist within the homecare model. When care is moved into the home it changes the home environment into a care setting, thus blurring the lines as to where care ends and the home begins and vice versa. Patients and health care providers may have difficulty navigating this environment: providers consider the home their work environment, while patients consider the home their personal domain. However, maintenance, upkeep, and financial management of the home remain the responsibility of the patient. The literature shows that patients living alone, and thus bearing these responsibilities alone, run a higher risk of loneliness, anxiety, depression, and risk of non-adherence [19,34,40,53,56]. Additionally, these patients may have an increased need for follow-up care visits [19,34,40]. This demonstrates once more the importance of considering the physical environment beyond that of an institutional setting in order to adequately consider the dynamics of those living and working within the home.
It is apparent that while existing concepts within this class were representative of some of our findings, others were neglected, reflecting a lack of sensitivity and specificity to the homecare setting.
Patient outcomes
Our last two safety markers Out of pocket and My health for yours: declining caregiver health mapped to the high-level class Patient Outcomes. ICPS defines this as the class that contains the concepts that relate to the impact upon a patient which is wholly or partially attributable to an incident. Patient outcomes can be classified according to the type of harm, the degree of harm, and any social and/or economic impact. There is a relationship between the descriptive classes, such as Patient Characteristics and Contributing Factors, and this high-level class.
Out of pocket: the cost of caring at home is the safety marker that refers to the emotional and economic burden that caring at home can create for patients and their caregivers. For instance, common economic and emotional aspects of receiving care at home include changes in financial status or well-being, stress, poor or uncertain quality of care, and depression [35,66,75]. The Patient Outcomes class includes the concept of Social and/or Economic Impact to which our safety marker Out of pocket maps well. For example, a common economic challenge for patients and caregivers (although caregivers are not considered in this class) is the loss of wages or reduction in wages because either the patient’s health limits his/her ability to work or the caregiver must reduce work hours in order to care for the patient [30,83,84]. Having to adjust to decreasing financial means, and sometimes lower-status employment through wage loss or reduction contributes to an increase in financial stress and a negative future economic outlook for both patients and caregivers [30,57,66,84,85].
In addition, the literature shows that patients and their families face personal expenses for needed home modifications, services, and equipment due to lack of financial coverage or difficulties in accessing funded support [30,39,48,86]. The economic and emotional impact on patients and caregivers strongly links to the status of their health and health outcomes.
My health for yours: declining caregiver health is a safety marker that describes how caregivers often sacrifice their own health for the health of their loved ones. Although caregivers are not included within the class of Patient Outcomes or its associated concepts, the literature shows a connection between the number and complexity of caring responsibilities, the caregivers’ health, and the health outcomes of the patient. For this reason, we have mapped this safety marker to Patient Outcomes and its concepts of Degree of Harm and Type of Harm. For instance, caregivers may experience depression, poor health, fatigue, exhaustion, and isolation which can affect the care they provide to their loved ones, resulting in safety risks and poor quality of care for the patients [30,57,66,75,85].
The types of harm facing family caregivers who provide care to patients with chronic illness include stress, fatigue, loss of sleep and concentration [33,35,39,59,61,67], as well as helplessness, anxiety, frustration, guilt, and strain [30,35,58,59,64,65,82,87],[88]. These problems can lead to varying degrees of harm from lower quality of life [61]; depression [76,82,89]; social isolation [18,29,87]; and psychological, physical, and emotional distress [18,30,39,61,79,90,91]; to, most significantly, increased morbidity [61] and mortality [61,63]. Hospital readmissions are consistently identified in the literature as patient health outcomes that result from caregivers’ poor health and diminished ability to care for patients safely [18,76,79,82,87,92,93].
It was possible to link these two safety markers, Out of pocket and My health for yours: declining caregiver health, to the class of Patient Outcomes, but as the health of the patient is inextricably linked to that of the caregiver [4] it would be far more prudent to include a high-level class that related directly to caregiver outcomes. Adapting the ICPS to consider the health of the caregiver and how it relates to the patient would add to the comprehensiveness of the classification system as well as patient health and safety. It has, for example, been shown that the level of emotional and mental health of the caregiver is positively linked to the psychological and emotional adjustment of the patient [61]. This interconnecting relationship should not be ignored and illustrates the need for an emphasis on patient/caregiver linkages within the ICPS concepts.
Discussion
In our application of the WHO ICPS to our findings, we discovered that our seven safety markers mapped to three of the ten high-level classes. In working through these three classes and their associated concepts, we also discovered some lack of specificity relating to patient safety within the homecare setting (e.g. classes and concepts did not incorporate outcomes for unpaid caregivers), and that the clinical basis and structure of the ICPS also posed a challenge, particularly in applying findings from the scoping review to the system.
The clinical origins of the ICPS are apparent when examining the literature on patient safety associated with the WHO World Alliance for Patient Safety. For instance, their focus was on recognizing gaps in the knowledge regarding unsafe care and a high degree of error for hospitalized patients [94]. In order to establish priorities for research on patient safety, they established major topics in patient safety by examining clinical and organizational issues identified through types and causes of adverse events (AEs) that are harmful to patients [94]. When care is moved into the home it changes the home environment into a care setting, thus blurring the lines as to where care ends and the home begins and vice versa. The spirit of the classification system remains focused on institutional settings. This creates the potential to overlook the distinct and diverse needs and safety concerns located in the homecare setting, such as the provision of health care services, role of unpaid caregivers (friends/family members), and the characteristics and life circumstances of the patient (and caregiver) [95]. Furthermore, creating a classification system oriented toward a clinical institutional setting limits the applicability to the patient/caregiver perspective.
A second, and perhaps more important, point is the obscurity of the caregiver within the classification system. Caregivers are included within some of the ICPS concepts but failure to include the role of caregivers, and particularly caregiver outcomes, at the class level limits the specificity of the framework in capturing safety issues within the homecare setting. Homecare relies on the efforts and work of unpaid caregivers; if caregivers are ill or do not have the support they require, they cannot attend to the needs of the patient and may face their own declining health. This impacts the health and safety of both the patient and caregiver. It is integral to see the link between caregiver and patient health and safety; yet in the ICPS, the significance of caregivers has been reduced to one of incident reporting and being included within descriptions of incident characteristics. Concepts and classes specific to the homecare setting are required to maximize the applicability of the ICPS across all health care settings.
Finally, it was agreed, as others have reported [96] that a guide to using the ICPS within various settings would be beneficial. We also found to a degree, as Schulz et al. [13] observed, that there was limited guidance on how to deal with overlapping categories or classes.
Conclusion
The scoping review findings resulted in the identification of markers relating to the safety of patients and caregivers. We did encounter some limitations in the application of the ICPS to homecare safety research. The ICPS, although applicable to our findings, did not effectively allow for locating all of the safety risks we identified within the homecare setting, due in part to a lack of specificity related to the patient caregiver linkages, and to a blurring of the lines that exist between the home and health care settings and the shared responsibilities that exist among patients, caregivers, and health care providers. In conclusion, although the intent in the development of the ICPS was to improve patient safety and care across disciplines and care settings, this will be achieved only by adapting the ICPS to reflect the uniqueness of the homecare setting. Following publication of this manuscript, we plan to engage with the WHO ICPS framework architects to discuss adaptations for relevance to homecare.
Competing interests
The authors declare there are no financial and/or non-financial competing interests.
Authors’ contributions
MM and AL contributed to every step in the generation of the evidence used to examine the usability of the WHO ICPS for safety in homecare, and shared the manuscript preparation; TB, JS, LS, KI and SD contributed to all aspects of the development of the knowledge used to examine the applicability of the ICPS to safety in homecare, and the review and editing of this article. TB and MM also incorporated the ICPS into the article and conducted the mapping of the safety markers. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Marilyn T Macdonald, Email: marilyn.macdonald@dal.ca.
Ariella Lang, Email: ariella.lang@sympatico.ca.
Janet Storch, Email: jstorch@uvic.ca.
Lynn Stevenson, Email: lynn.stevenson@viha.ca.
Tanya Barber, Email: tanya.barber@dal.ca.
Kristine Iaboni, Email: kristine.iaboni@gmail.com.
Susan Donaldson, Email: sdonaldson@powergate.ca.
Acknowledgements
Hélène LaCroix, St. Elizabeth Healthcare. Sheri Roach, Capital District Health Authority. The authors acknowledge the funding support from the Canadian Institutes of Health Research (CIHR) for the Scoping Review that produced the findings discussed in relation to the WHO ICPS.
References
- Statistics Canada. Population projections: Canada, the provinces and territories 2009-2013. Ottawa, Canada: Statistics Canada; 2009. Retrieved from: http://www.statcan.gc.ca/pub/91-520-x/91-520-x2010001-eng.pdf. [Google Scholar]
- World Health Organization. Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization; 2011. Retrieved from: http://www.who.int/nmh/publications/ncd_report_full_en.pdf. [Google Scholar]
- Macdonald M, Lang A, Storch J, Stevenson L, Barber T, Iaboni K, Donaldson S, LaCroix H. Home Care Safety Markers: A Scoping Review. 2013. (Home Healthcare Services Quarterly). Retrieved from http://www.tandfonline.com/eprint/vxHsUwV68wbUXqKheD7p/full#.UaPkpkqmWIQ. [DOI] [PubMed]
- Lang A, Edwards N. Safety in homecare: A background paper for round table discussion. Edmonton, AB: Canadian Patient Safety Institute (CPSI); 2006. [Google Scholar]
- Lang A, Macdonald MT, Storch J, Elliott K, Stevenson L, LaCroix H, Donaldson S, Geering Curry C, Corsisi-Munt S, Francis F. Homecare safety perspectives from clients, family members, caregivers, and paid providers. Healthc Q. 2009;12(Sp):23–27. doi: 10.12927/hcq.2009.20720. Invited to submit. http://www.longwoods.com/home.php?cat=592#loopBack. 10.12927.hcq.2009.20720. [DOI] [PubMed] [Google Scholar]
- Macdonald M, Lang A, Storch J, Stevenson L, Elliott K, LaCroix H, Donaldson S. Safety in Home Care for Unpaid Caregivers. Edmonton, Canada: Canadian Patient Safety Institute; 2010. (Commissioned by the Canadian Patient Safety Institute). Retrieved from http://www.patientsafetyinstitute.ca/English/research/commissionedResearch/SafetyinHomeCare/Pages/UnpaidCaregivers.aspx. [Google Scholar]
- Macdonald MT, Lang A, MacDonald J. Mapping a research agenda for home care safety: perspectives from researchers, providers, and decision-makers. Can J Aging. 2011;30(2):233–245. doi: 10.1017/S0714980811000055. [DOI] [PubMed] [Google Scholar]
- Canadian Home Care Association. Home care the next essential service: Meeting the needs of our aging population. Mississauga, Ontario, Canada: Canadian Home Care Association; 2008. Retrieved from: http://www.cdnhomecare.ca/media.php?mid=1902. [Google Scholar]
- Canadian Institute for Health Information. All-Cause Readmission to Acute Care and Return to the Emergency Department. Ottawa, Canada: Canadian Institute for Health Information; 2012. Retrieved from https://secure.cihi.ca/free_products/Readmission_to_acutecare_en.pdf. [Google Scholar]
- World Health Organization. Conceptual Framework for the International Classification for Patient Safety. Geneva, Switzerland: World Health Organization; 2009. (Technical Report, Version 1.1). Retrieved from: http://www.who.int/patientsafety/implementation/taxonomy/en/ [Google Scholar]
- de Feijter JM, de Grave WS, Muijtjens AM, Scherpbier AJJA, Koopmans RP. A comprehensive overview of medical error in hospitals using incident-reporting systems, patient complaints and chart review of inpatient deaths. PLoS One. 2012;7(2):e31125. doi: 10.1371/journal.pone.0031125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsal S, Heffner JE. Creating a web-based incident analysis and communication system. Journal of hospital medicine: an official publication of the Society of Hospital Medicine. 2012;7(2):142–147. doi: 10.1002/jhm.956. [DOI] [PubMed] [Google Scholar]
- Schulz S, Karlsson D, Daniel C, Cools H, Lovis C. Is the “international classification for patient safety” a classification? Stud Health Technol Inform. 2009;150:502–506. [PubMed] [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Thorne S, Kirkham SR, O’Flynn-Magee K. The analytic challenge in interpretive description. International Journal for Qualitative Methods. 2004;3(1):1–20. [Google Scholar]
- Morgan AL, Masoudi FA, Havranek EP, Jones PG, Peterson PN, Krumholz HM, Spertus JA, Rumsfield JS. Difficulty taking medications, depression, and health status in heart failure patients. J Card Fail. 2006;12(1):54–60. doi: 10.1016/j.cardfail.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Quinn C. End-of-life care with the heart failure patient in home health: a case study. J Infus Nurs. 2005;28(6):393–398. doi: 10.1097/00129804-200511000-00006. [DOI] [PubMed] [Google Scholar]
- Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure: Review and analysis. Eur J Heart Fail. 2005;7(4):592–603. doi: 10.1016/j.ejheart.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Sauvé MJ, Lewis WR, Blankenbiller M, Rickbaugh B, Pressler SJ. Cognitive impairments in chronic heart failure: a case controlled study. J Card Fail. 2009;15(1):1–10. doi: 10.1016/j.cardfail.2008.08.007. [DOI] [PubMed] [Google Scholar]
- Triller D, Hamilton RA. Effect of pharmaceutical care services on outcomes for home care patients with heart failure. Am J Health Syst Pharm. 2007;64:2244–2249. doi: 10.2146/ajhp050492. [DOI] [PubMed] [Google Scholar]
- Clark A, Reid ME, Morrison CE, Capewell S, Murdoch DL, McMurray JJ. The complex nature of informal care in home-based heart failure management. J Adv Nurs. 2007;61(4):373–383. doi: 10.1111/j.1365-2648.2007.04527.x. [DOI] [PubMed] [Google Scholar]
- Horne G, Payne S. Removing the boundaries: palliative care for patients with heart failure. Palliat Med. 2004;18:291–296. doi: 10.1191/0269216304pm893oa. [DOI] [PubMed] [Google Scholar]
- Vanderschaaf K, Olson KL, Billups S, Hartsfield CL, Rice M. Self-reported inhaler use in patients with chronic obstructive pulmonary disease. Respir Med. 2010;104:99–106. doi: 10.1016/j.rmed.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Fromer L, Goodwin E, Walsh J. Customizing inhaled therapy to meet the need of COPD patients. Postgrad Med. 2010;122(2):83–93. doi: 10.3810/pgm.2010.03.2125. [DOI] [PubMed] [Google Scholar]
- Schmidt S, Sheikzadeh S, Beil B, Pattern M, Stettin J. Acceptance of telemonitoring to enhance medication compliance in patients with chronic heart failure. Telemedicine and e-Health. 2008;14(5):426–433. doi: 10.1089/tmj.2007.0076. [DOI] [PubMed] [Google Scholar]
- Polzien G. Practical interventions to prevent or lower emergent care and rehospitalisation. Home Healthc Nurse. 2007;25(7):482–485. doi: 10.1097/01.NHH.0000281616.81423.5b. [DOI] [PubMed] [Google Scholar]
- Quinn C. Low-technology heart failure care in home health: Improving patient outcomes. Home Healthc Nurse. 2006;24(8):533–540. doi: 10.1097/00004045-200609000-00012. [DOI] [PubMed] [Google Scholar]
- Roberts MM, Leeder SR, Robinson TD. Nurse-led 24-h hotline for patients with chronic obstructive pulmonary disease reduces hospital use and is safe. Intern Med J. 2008;38:334–340. doi: 10.1111/j.1445-5994.2007.01519.x. [DOI] [PubMed] [Google Scholar]
- Hwang B, Luttik ML, Dracup K, Jaarsma T. Family caregiving for patients with heart failure: Types of care provided and gender differences. J Card Fail. 2010;16(5):398–403. doi: 10.1016/j.cardfail.2009.12.019. [DOI] [PubMed] [Google Scholar]
- Brewin A. The quality of life of carers of patients with severe lung disease. Br J Nurs. 2004;13(15):906–912. doi: 10.12968/bjon.2004.13.15.15529. [DOI] [PubMed] [Google Scholar]
- Aldred H, Gott M, Gariballa S. Advanced heart failure: impact on older patients and informal carers. J Adv Nurs. 2005;49(2):116–124. doi: 10.1111/j.1365-2648.2004.03271.x. [DOI] [PubMed] [Google Scholar]
- Hopp FP, Thornton N, Martin L. The lived experience of heart failure at the end of life: a systematic literature review. Health Soc Work. 2010;35(2):109–117. doi: 10.1093/hsw/35.2.109. [DOI] [PubMed] [Google Scholar]
- Quaglietti SE, Artwood EA, Ackerman L, Froelicher V. Management of the patient with congestive heart failure using outpatient, home, and palliative care. Prog Cardiovasc Dis. 2000;23(3):259–274. doi: 10.1053/pcad.2000.19803. [DOI] [PubMed] [Google Scholar]
- Brännström M, Ekman I, Norberg A, Boman K, Strandberg G. Living with severe chronic heart failure in palliative advanced home care. Eur J Cardiovasc Nurs. 2006;5:295–302. doi: 10.1016/j.ejcnurse.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Hasson F, Spence A, Waldron M, Kernohan G, McLaughlin D, Watson B, Cochrane B. Experiences and needs of bereaved carers during palliative and end-of-life care for people with chronic obstructive pulmonary disease. J Palliat Care. 2009;25(3):157–163. [PubMed] [Google Scholar]
- Scott LD, Setter-Kline K, Britton AS. The effects of nursing interventions to enhance mental health and quality of life among individuals with heart failure. Appl Nurs Res. 2004;17(4):248–256. doi: 10.1016/j.apnr.2004.09.004. [DOI] [PubMed] [Google Scholar]
- Michaels C, Meek PM. The language of breathing among individuals with chronic obstructive pulmonary disease. Heart Lung. 2004;33(6):390–400. doi: 10.1016/j.hrtlng.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Chattoo S, Atkin K. Extending specialist palliative care to people with heart failure: semantic historical and practical limitations to policy guidelines. Soc Sci Med. 2009;69:147–153. doi: 10.1016/j.socscimed.2009.02.025. [DOI] [PubMed] [Google Scholar]
- Hasson F, Spence A, Waldron M, Kernohan G, McLaughlin D, Watson B, Cochrane B. I can not get a breath: experiences of living with advanced chronic obstructive pulmonary disease. International Journal of Family Nursing. 2008;14(11):526–531. doi: 10.12968/ijpn.2008.14.11.31756. [DOI] [PubMed] [Google Scholar]
- Davidson P, Paull G, Rees D, Daly J, Cockburn J. Activities of home-based heart failure nurse specialists: a modified narrative analysis. Am J Crit Care. 2005;14(5):426–433. [PubMed] [Google Scholar]
- Barnett M. Caring for a patient with COPD: a reflective account. Nurs Stand. 2005;19(36):41–46. doi: 10.7748/ns.19.36.41.s58. [DOI] [PubMed] [Google Scholar]
- Boyd KJ, Worth A, Kendall M, Pratt R, Hockley J, Denvir M, Murray SA. Making sure services deliver for people with advanced heart failure: a longitudinal qualitative study of patients, family carers, and health professionals. Palliat Med. 2009;23(8):767–776. doi: 10.1177/0269216309346541. [DOI] [PubMed] [Google Scholar]
- British Thoracic Guideline Development Group. Intermediate care- hospital-at-home in chronic obstructive pulmonary disease: British thoracic society guideline. Thorax: An International Journal of Respiratory Medicine. 2004;62:200–210. doi: 10.1136/thx.2006.064931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsello P, Tinkelman D. Optimizing disease management of chronic obstructive pulmonary disease. Disease Management and Health Outcomes. 2008;16(5):289–296. doi: 10.2165/0115677-200816050-00004. [DOI] [Google Scholar]
- Bartoli L, Zanaboni P, Masella C, Ursini N. Systematic review of telemedicine services for patients affected by Chronic Obstructive Pulmonary Disease (COPD) Telemedicine and E-Health. 2009;15(9):877–883. doi: 10.1089/tmj.2009.0044. [DOI] [PubMed] [Google Scholar]
- Dansky KH, Vasey J, Bowles K. Use of telehealth by older adults to manage heart failure. Res Gerontol Nurs. 2008;1(1):25–32. doi: 10.3928/19404921-20080101-01. [DOI] [PubMed] [Google Scholar]
- Horton K. The use of telecare for people with chronic obstructive pulmonary disease: implications for management. J Nurs Manag. 2008;16:173–180. doi: 10.1111/j.1365-2834.2008.00845.x. [DOI] [PubMed] [Google Scholar]
- Law S, Lehoux P. Hospital technology at home portable oxygen therapy in COPD. Québec: AETMIS (Agence d’évaluation des technologies et des modes d’intervention en Santé); 2004. [Google Scholar]
- Slater SG Neander L Carey G Measuring quality of life outcomes through the use of home telehealth: using a case study model in terminal heart failure patient Home Health Care Management & Practice 2006184333–335. 10.1177/108482230528395123720383 [DOI] [Google Scholar]
- Myers S, Grant RW, Lugn NE, Holbert B, Kvedar JC. Impact of home-based monitoring on the care of patients with congestive heart failure. Home Health Care Management Practice. 2006;18(6):444–451. doi: 10.1177/1084822306289991. [DOI] [Google Scholar]
- Radai MM, Arad M, Zlochiver S, Krief H, Engelman T, Abboud S. A Novel telemedicine system for monitoring congestive heart failure patients. Congest Heart Fail. 2008;14:239–244. doi: 10.1111/j.1751-7133.2008.00004.x. [DOI] [PubMed] [Google Scholar]
- Scherr D, Kastner P, Kollmann A, Hallas A, Auer J, Krappinger H, Schuchlenz H, Stark G, Grander W, Jakl G, Schreier G, Fruhwald FM. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: Randomized controlled trial. J Med Internet Res. 2009;11(3):1–12. doi: 10.2196/jmir.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert NM, Zeller R. Depressed patients understand heart failure prognosis but not how to control it. Heart Lung. 2009;38:382–391. doi: 10.1016/j.hrtlng.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Cortis JD, Williams A. Palliative and supportive needs of older adults with heart failure. Int Nurs Rev. 2007;54:263–270. doi: 10.1111/j.1466-7657.2007.00558.x. [DOI] [PubMed] [Google Scholar]
- Elofsson LC. Meanings of being old and living with chronic pulmonary disease. Palliat Med. 2004;18:611–618. doi: 10.1191/0269216304pm922oa. [DOI] [PubMed] [Google Scholar]
- Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS. Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol. 2004;44(12):2333–2338. doi: 10.1016/j.jacc.2004.09.034. [DOI] [PubMed] [Google Scholar]
- Evangelista L, Ter-Galstanyan A, Moughrabi S, Moser DK. Anxiety and depression in ethnic minorities with chronic heart failure. J Card Fail. 2009;15(7):572–579. doi: 10.1016/j.cardfail.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris S. COPD and coping with breathlessness at home: a review of the literature. Br J Community Nurs. 2007;12(9):411–415. doi: 10.12968/bjcn.2007.12.9.27234. [DOI] [PubMed] [Google Scholar]
- Spence A, Hasson F, Waldron M, Kernohan G, McLaughlin D, Cochrane B, Watson B. Active carers: Living with chronic obstructive pulmonary disease. Int J Palliat Nurs. 2008;14(8):368–372. doi: 10.12968/ijpn.2008.14.8.30771. [DOI] [PubMed] [Google Scholar]
- Goodlin SJ. End-of-life care in heart failure. Curr Cardiol Rep. 2009;11(3):184–191. doi: 10.1007/s11886-009-0027-7. [DOI] [PubMed] [Google Scholar]
- Luttik ML, Blaauwbroek A, Dijker A, Jaarsma T. Living with heart failure: partner perspectives. J Cardiovasc Nurs. 2007;22(2):131–137. doi: 10.1097/00005082-200703000-00010. [DOI] [PubMed] [Google Scholar]
- Nordtug B Holen A Simlarities and differences in caring burden of home dwellers with partners suffering from chronic obstructive pulmonary disease or dementia Home Health Care Management & Practice 201123293–101. 10.1177/108482231036863323720383 [DOI] [Google Scholar]
- Saunders MM. A Comparison of employed and unemployed caregivers of older heart failure patients. Holist Nurs Pract. 2010;24(1):16–22. doi: 10.1097/HNP.0b013e3181c8e469. [DOI] [PubMed] [Google Scholar]
- Brännström M, Ekman I, Boman K, Strandberg G. Being a close relative of a person with severe, chronic heart failure in palliative advanced home care – a comfort but also a strain. Scand J Caring Sci. 2007;21:338–344. doi: 10.1111/j.1471-6712.2007.00485.x. [DOI] [PubMed] [Google Scholar]
- Brännström M, Ekman I, Boman K, Strandberg G. Narratives of a man with severe chronic heart failure and his wife in palliative advanced home care over a 4.5-year period. Contemp Nurse. 2007;27:10–22. doi: 10.5172/conu.2007.27.1.10. [DOI] [PubMed] [Google Scholar]
- Hwang B, Dracup K. Impact of caregiving on family caregivers of patients with heart failure. Chase, MD: Heart Failure Society of America; 2010. (The 14th Annual Scientific Meeting #CHFSA S5, 011). [Google Scholar]
- Wolfe P, McMillan M, Conway J. The needs of caregivers of people with COPD: a study. Aust J Prim Health. 2007;13(1):28–35. [Google Scholar]
- Heart Failure Society of America. Executive summary: CHFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16(6):475–539. doi: 10.1016/j.cardfail.2010.04.005. [DOI] [Google Scholar]
- Jansen DJA, Wouters EFM, Schols JMGA, Spruit MA. Self-perceived symptoms and care needs of patients with severe to very severe chronic obstructive pulmonary disease, congestive heart failure or chronic renal failure and its consequences for their closest relatives: the research protocol. BMC Palliative Care. 2008;7(5):1–8. doi: 10.1186/1472-684X-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff B, Burton L, Mader S, Naughton B, Burl J, Inouye S, Greenough WB, Guido S, Langston C, Frick KD, Steinwachs D, Burton JR. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143(11):798–808. doi: 10.7326/0003-4819-143-11-200512060-00008. [DOI] [PubMed] [Google Scholar]
- Upadaya S, Lee FA, Saldarriaga C, Verma S, Sedrakyan A, Nystrom K, Katz SD. Home continuous positive inotropic infusion as a bridge to cardiac transplantation in patients with end-stage heart failure. J Heart Lung Transplant. 2004;23(4):466–472. doi: 10.1016/S1053-2498(03)00203-1. [DOI] [PubMed] [Google Scholar]
- Mair FS, Hiscock J, Beaton SC. Understanding factors that inhibit or promote the utilization of telecare in chronic lung disease. Chronic Illn. 2008;4:110–117. doi: 10.1177/1742395308092482. [DOI] [PubMed] [Google Scholar]
- Quinn C, Dunbar SB, Higgins M. Heart failure symptom assessment and management: Can caregivers serve as proxy? J Cardiovasc Nurs. 2010;25(2):142–148. doi: 10.1097/JCN.0b013e3181bf93a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DM, Ross C, Goodridge D, Davis P. The care needs of community-dwelling seniors suffering from advanced chronic obstructive pulmonary disease. Canadian Journal on Aging/La Revue canadienne du vieillissement. 2008;27(4):347–357. doi: 10.3138/cja.27.4.347. [DOI] [PubMed] [Google Scholar]
- Bennett SJ, Bakas T, Johnson EA, Shaneyfelt T. What about family caregivers of patients with heart failure? J Card Fail. 2004;10(4S):303. [Google Scholar]
- Narsavage GL, Chen K. Factors related to depressed mood in adults with COPD post-hospitalization. Home Healthcare Nurse: The Journal for the Home Care and Hospice Professional. 2008;26(8):474–482. doi: 10.1097/01.NHH.0000335606.45977.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan EA. People with heart failure and home health care resource use and outcomes. J Clin Nurs. 2008;17(7B):253–259. doi: 10.1111/j.1365-2702.2008.02334.x. [DOI] [PubMed] [Google Scholar]
- Warwick M, Gallagher R, Chenoweth L, Stein-Parbury J. Self-management and symptom monitoring among older adults with chronic obstructive pulmonary disease. J Adv Nurs. 2010;66(4):784–793. doi: 10.1111/j.1365-2648.2009.05238.x. [DOI] [PubMed] [Google Scholar]
- Pressler SJ, Gradus-Pizlo I, Chubinski SD, Smith G, Wheeler S, Wu J, Sloan R. Family caregiver outcomes in heart failure. Am J Crit Care. 2009;18(2):149–159. doi: 10.4037/ajcc2009300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglia E, Fulgenzi A, Ferrero ME. Rationale of the combined Use of inspiratory and expiratory devices in improving maximal inspiratory pressure and maximal expiratory pressure of patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2009;90:913–918. doi: 10.1016/j.apmr.2008.12.019. [DOI] [PubMed] [Google Scholar]
- Gullick J, Stainton MC. Living with chronic obstructive pulmonary disease: developing conscious body management in a shrinking life-world. J Adv Nurs. 2008;64(6):605–614. doi: 10.1111/j.1365-2648.2008.04823.x. [DOI] [PubMed] [Google Scholar]
- Harkness KI. Uncertainty and emotional distress in patients with heart failure and their primary caregivers: a novel study. J Card Fail. 2009;15:6S. doi: 10.1016/j.cardfail.2009.06.419. [DOI] [Google Scholar]
- Lundman B, Brännström M, Hägglund L, Strandberg G. Fatigue in elderly with chronic heart failure: an under-recognized symptom. Aging Health. 2009;5(5):619–624. doi: 10.2217/ahe.09.49. [DOI] [Google Scholar]
- Mendoza H, Martín MJ, Garcia A, Arós F, Aizpuru F, De Los Cobos JR, Belló MC, Lopetegui P, Cia JM. ‘Hospital at home’ care model as an effective alternative in the management of decompensated chronic heart failure. Eur J Heart Fail. 2009;11(12):1208–1213. doi: 10.1093/eurjhf/hfp143. [DOI] [PubMed] [Google Scholar]
- Suwanno J, Petpichetchian W, Riegel B, Issaramalai S. A Model predicting health status of patients with heart failure. J Cardiovasc Nurs. 2009;24(2):118–126. doi: 10.1097/JCN.0b013e318197a75c. [DOI] [PubMed] [Google Scholar]
- Law S. Liquid oxygen therapy at home. Montréal, Canada: Agence d’évaluation des technologies et des modes d’intervention en santé (AETMIS); 2005. Retrieved December 2010 at http://www.crd.york.ac.uk/crdweb/ShowRecord.asp?View=Full&ID=32005000094#.UaPvwEqmWIR. [Google Scholar]
- Ågren S, Frisman GH, Berg S, Svedjeholm R, Strömberg A. Addressing spouses’ unique needs after cardiac surgery when recovery is complicated by heart failure. Heart Lung. 2009;38(4):284–291. doi: 10.1016/j.hrtlng.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Tsai B. Feasibility and effectiveness of e-therapy on fatigue management in home-based older adults with congestive heart failure. USA: The State University of New York at Buffalo; 2008. (PhD thesis). [Google Scholar]
- Saunders MM. Factors associated with caregiver burden in heart failure family caregivers. West J Nurs Res. 2008;30:943–959. doi: 10.1177/0193945908319990. [DOI] [PubMed] [Google Scholar]
- Harkness KI, Tranmer JE. Measurement of the caregiving experience in caregivers of persons living with heart failure: a review of current instruments. J Card Fail. 2007;13(7):577–587. doi: 10.1016/j.cardfail.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J Card Fail. 2005;11(6):455–463. doi: 10.1016/j.cardfail.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Luttik ML, Lesman-Leegte I, Jaarsma T. Quality of life and depressive symptoms in heart failure patients and their partners: The impact of role and gender. J Card Fail. 2009;15(7):580–585. doi: 10.1016/j.cardfail.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Shoham V, Cleary AA, Berman JS, Ewy GA. Health consequences of partner distress in couples coping with heart failure. Heart Lung. 2009;38:298–305. doi: 10.1016/j.hrtlng.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Jha AK, Prasopa-Plaizier N, Larizgoitia I, Bates DW. Patient safety research: and overview of the global evidence. Qual Saf Health Care. 2010;19:42–47. doi: 10.1136/qshc.2008.029165. [DOI] [PubMed] [Google Scholar]
- Hirdes J. Because This Is the Rainy Day: A Discussion Paper on Home Care And Informal Caregiving for Seniors with Chronic Health. Toronto: The Change Foundation; 2011. [Google Scholar]
- Sherman H, Castro G, Fletcher M, Hatlie M, Hibbert P, Jakob R, Koss R, Loeb J, Perneger T, Runciman W, Thomson R, Der Schaaf T, Virtanen M. World Alliance for Patient Safety Drafting Group. Towards an international classification for patient safety: the conceptual framework. Int J Qual Health Care. 2009;21(1):2–8. doi: 10.1093/intqhc/mzn054. [DOI] [PMC free article] [PubMed] [Google Scholar]