Abstract
Objectives
Patients with advanced cancer are often admitted to hospital as emergency cases. This may not always be medically indicated. Study objectives were to register the reasons for the emergency admissions, to examine interventions performed during hospitalisation and self-reported symptom intensity at admission and discharge, and to assess patients’ opinions about the admission.
Design
This was a descriptive before-and-after study. Participating patients completed the Edmonton Symptom Assessment System (ESAS) twice, upon hospital admission and prior to discharge. All patients underwent a structured interview assessing their opinion about the emergency admission. Medical data were obtained from the hospital records.
Setting
The study was performed in two Norwegian acute care secondary hospitals with urban catchment areas.
Participants
44 patients with cancer (men 27 and women 17; mean age 69.2, SD 9.2) representing 50 emergency admissions were included.
Results
Median length of stay was 7 days (95% CI 7.4 to 11.4). Median survival was 50 days (95% CI 51 to 115). 90% were admitted from home, and 46% had been hospitalised less than 1 month earlier. Lung and gastrointestinal symptoms and pain were the most frequent reasons for admissions. Mean pain scores on ESAS were reduced by 50% from admission to discharge (p<0.01). Simple interventions such as hydration, bladder catheterisation and oxygen therapy were most frequent. Nearly one-third would have preferred treatment at another site, provided that the quality of care was similar. Home visits by the family doctor and specialised care teams were perceived by patients as important to prevent hospitalisation.
Conclusions
In most emergency admissions, relatively simple medical interventions are necessary. Specialised care teams with palliative care physicians, easier access to the family doctor and better lines of cooperation between hospitals and the primary care sector may make it possible to perform more of these procedures at home, thereby reducing the need for emergency admissions.
Keywords: Oncology, Palliative care
Article summary.
Article focus
Investigate the reasons for emergency admissions of palliative care patients with cancer.
Register interventions performed in the hospital.
Examine symptom intensity before and after medical interventions by a standardised self-report tool (Edmonton Symptom Assessment System).
Key messages
Palliative care emergency admissions were not always necessary or strictly medically indicated.
Simple medical procedures in the home care setting may reduce the need for emergency admissions.
Increased level of competence and more specialised palliative care skills in the primary healthcare sector is necessary to prevent emergency admissions.
Strengths and limitations of this study
-
▪
All potentially eligible patients were assessed.
-
▪
Registrations were performed prospectively, with a thorough examination of the charts after discharge/death, and the latter were also assessed retrospectively.
-
▪
Patients’ own experiences were registered.
-
▪
Small study in two hospitals only, with a limited number of variables, may reduce overall generalisability.
-
▪
No registration of the Eastern Cooperative Oncology Group (ECOG)/Karnofsky score upon admission.
Introduction
Thanks to modern multimodal therapy, survival has improved for many cancer diagnoses. Slightly less than 50% of patients will die from their cancer1 while the remaining half will live with the disease for shorter or longer periods of time.2 This accentuates the need for optimal symptom management and maintenance of quality of life throughout the disease trajectory.
Admissions to the intensive care unit (ICU) and the number of visits to the emergency room (ER) are quality indicators in end-of-life care.3 Although this may be necessary in many cases, it is not always so. A British study examined emergency admissions of patients with cancer in an acute care hospital and concluded that close to 50% neither needed nor wanted to be admitted as an emergency.4 This is in line with a Canadian study examining administrative data on admissions, concluding that many visits to the emergency department by patients with cancer near the end of life may be avoidable.5 Studies have documented that patients with incurable cancer frequently use acute care hospitals for acute problems and symptomatic treatment,6 –8 particularly older patients with cancer during their last month of life.7 A study from Ontario published in 20068 showed that 27% of patients with cancer paid a visit to the ER in the last 2 weeks of life, corresponding to 34% in a subsequent report (2010),5 in line with other reports demonstrating increasing trends over time.6 9 10
A closer collaboration between oncology and palliative care has been recommended.11 12 One study reported that systematic implementation of a palliative care integration project resulted in significantly better documentation of pain, fewer visits to the ER, and fewer admissions to acute care hospitals.13 This was consistent with a review showing that home, hospital and inpatient specialist palliative care significantly improved symptom control, pain and anxiety, and reduced hospital admissions.14 Similar findings were reported from a randomised controlled trial (RCT) in a mixed sample of terminally ill patients who received specialised in-home palliative care.15 However, another RCT, comparing a multicomponent intervention and follow-up, found no reduction in ER visits but a significantly better quality of life and mood.16
Emergency admissions often represent stressful events for the patients and their families because of anxiety, a feeling of discontinuity and logistic problems in an emergency setting that may increase the waiting time. Having to go to the ER for admission may also conflict with patients’ wishes. On the basis of our experience in palliative medicine, and our interest in continuity of care in patients with advanced disease, we have conducted a small descriptive study aiming to aid in the planning of palliative care in two Norwegian acute care local hospitals. The aims of the study were to register the reasons for the emergency admissions, to examine symptom intensity upon admission and discharge and to register the interventions performed during hospitalisation. Patients’ opinions about the emergency admission were also assessed.
Material and methods
Patients
The two hospitals were the Østfold Hospital Trust (SØF) and the Lovisenberg Diakonale Hospital (LDS). SØF is the district general hospital for approximately 277 000 inhabitants in the south-eastern part of Norway. The hospital has specialist healthcare services in most medical specialties, including oncology and palliative care. LDS is located in the capital, Oslo, Norway. It serves as the general hospital for psychiatry and internal medicine including emergency admissions, in one of four city sectors with a catchment area of about 156 000 inhabitants. LDS has a specialised palliative care unit.
The Norwegian healthcare system is organised with university, regional and local hospitals and widespread community healthcare services. In the catchment areas of these two hospitals, the home care services had nurses with special training in palliative care, supplemented by experienced physicians who were available on request. Also, all palliative care patients who have had previous contact with the hospitals receive special follow-up from the hospital directly or through the hospitals’ ambulant palliative care teams, as necessary. The update is normally adapted and updated according to the changing needs. Nevertheless, unplanned hospital admissions in Norway are normally routed though the emergency department, even if the patients have a previous affiliation with the hospital. Formal advanced care planning is not routinely applied in Norway, but elements from such plans are often part of the discussion with patients and their relatives.
A consecutive sample of patients with cancer who were admitted through the emergency departments was included between October 2009 and May 2010. Inclusion criteria were a verified diagnosis of cancer in the palliative phase of the disease, documented in the patient chart, anticipated survival less than 1 year and cognitive and physical capacity to complete the study as evaluated by the attending oncologist prior to inclusion, age >18 years, fluency in Norwegian and provision of signed informed consent. Exclusion criteria were treatment with curative or adjuvant intent, a psychiatric diagnosis and language problems/illiteracy.
Instruments
Medical and sociodemographic data
The case report forms encompassed sociodemographic variables (marital and living situation), use of etc and details about the admission (date, time, reason for and organisation of the admission). One dichotomous question (yes/no) asked about the use of different home care services such as specialised palliative care, generalist home care teams, contact with community cancer nurse, etc, as well as help from family/friends in the last 3 months. Medical data, for example, cancer diagnosis (International Classification of Diseases, 10th edition (ICD-10)),17 metastases, ongoing or previous tumour-directed treatment (chemotherapy, radiotherapy, biological agents and hormonal therapy), and recent hospital discharges were recorded, as were medical interventions during hospitalisation and details about the discharge. This information was updated during the stay and after discharge by the study nurses/physicians through double checking of the hospitals’ patient records and the electronic/written charts. Date of death was recorded retrospectively based on automatic updates in the hospital records from the Cause of Death Registry.18
Symptom assessment
The Edmonton Symptom Assessment System (ESAS) is one of the most frequently used symptom assessment tools in palliative cancer care,19 and was developed to monitor the most common cancer symptoms with minimal patient burden.20 A Norwegian version of ESAS was used. A numerical rating scale, ranging from 0 to 10 (0=no symptom, normal/good and 10=worst possible symptom), was used for the following symptoms; pain at rest, pain at movement, tiredness, nausea, shortness of breath, dry mouth (xerostomia), appetite, anxiety/uneasiness, depression/sadness and the question “Overall, how are you feeling today (well-being)?” Patients were asked to rate their symptoms at the present time.
Structured patient interview
A short structured interview (nine questions) was developed in order to assess patients’ perceptions about emergency admission. First, the patients were asked to give the two most important reasons for the emergency admission from a list of 16 frequent symptoms/problem areas, supplemented by one open category. They were also asked about the duration of symptom development, how the admission was organised, whom they contacted to get help, who organised the admission and how they were transported to the hospital. Four questions were asked to assess if the admission was in accordance with their desires, if they would have preferred to receive treatment somewhere else, and if so, where: at home, in another hospital, in a nursing home or palliative care unit, and finally, if they could identify certain interventions that could have prevented the emergency admission: among others, extended nursing home care, specialised palliative care teams and regular visits from the family doctor. Free comments were encouraged.
Methods for data collection
Patients were approached shortly after admission, and informed about the study by the study nurses. If the patient consented to participate, ESAS was used at the earliest convenience. The second ESAS was completed as close to discharge as practically possible. The structured interviews were undertaken 1–3 days after admission. These were performed by two designated specialist nurses in palliative medicine.
Ethical considerations
The protocol was approved by the Regional Committee for Medical and Health Research Ethics, the Norwegian Social Science Data Services (NSD), the institutional review boards at the two hospitals and was conducted according to the rules of the Helsinki declaration. All participants provided written informed consent prior to study start.
Statistics
Sample size estimations and power calculations were not performed due to the descriptive nature of the study. Standard descriptive statistics were used and few subgroup comparisons were performed due to the small sample size. Each admission and its related interventions were regarded as independent events. A p value ≤0.05 was considered to be statistically significant. The PASW 18 statistical package was used (SPSS Inc, Chicago, Illinois, USA).
Results
Patients
A total of 44 patients (27 men and 17 women) were included, accounting for 50 emergency admissions. Median age was 66 years (53–89) and 16 (36%) of the patients were >70 years old. Forty (91%) patients had metastatic disease. The remaining four had lung (n=2) and gastrointestinal cancer (n=2) and were receiving palliative cancer care because of their complex symptom burden.
One patient was still alive at the time of data analyses. Median survival for the remaining 43 patients was 50 days (range 1–500, 95% CI 51 to 115) from the first day of study entry, table 1. Five patients died during their hospitalisation, while median survival for the 38 patients who were discharged was 56 days (range 16–500, 95% CI 58 to 128). Nine of these died within the first month. Sixteen patients lived for more than 90 days after discharge, six beyond 180 days, while two patients lived longer than the estimated life expectancy of 1 year.
Table 1.
Sociodemographic and medical characteristics of the patients*
| N | Per cent | |
|---|---|---|
| Sex | ||
| Male | 27 | 61 |
| Female | 17 | 39 |
| Marital status | ||
| Married/cohabiting | 32 | 73 |
| Single/widowed/divorced | 11 | 44 |
| Missing | 1 | 2 |
| Living situation | ||
| With others | 32 | 73 |
| Alone | 12 | 27 |
| Education | ||
| Compulsory or less | 17 | 39 |
| High school graduate | 15 | 34 |
| College/university | 11 | 25 |
| Missing | 1 | 2 |
| Diagnoses | ||
| Gastrointestinal | 18 | 41 |
| Lung | 11 | 25 |
| Urological | 7 | 16 |
| Other† | 8 | 18 |
| Metastatic disease‡ | ||
| Presence of metastases | 40 | 91 |
| Site of metastases | ||
| Liver | 21 | 48 |
| Lymph nodes | 17 | 39 |
| Bone | 13 | 30 |
| Lung | 12 | 27 |
| Brain | 7 | 16 |
| Tumour-directed treatment, ongoing upon admission | ||
| Chemotherapy | 14 | 32 |
| Hormones | 3 | 6 |
| Median | Range | |
| Age | 66 | 53–89 |
| Survival | ||
| Overall survival§, days from first study entry | 50 | 1–500, 95% CI 51 to 115 |
*N=44, the number of individual patients accounting for the 50 emergency admissions.
†Breast (3), malignant melanoma (2), gynaecological (2) and unspecified (1).
‡Percentages exceed 100 because of the multiple sites per patient.
§N=43, one patient was still alive at follow-up.
The emergency admissions
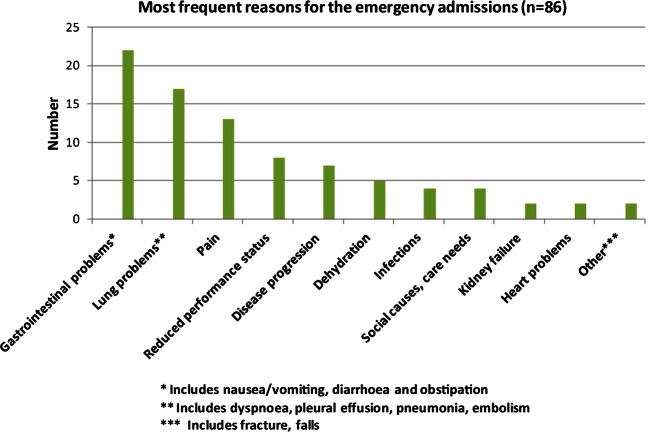
Information about the reason for the emergency admission was captured from the registrations in the medical charts by the attending doctors in the emergency department. In the majority of the cases (n=36, 72%) two reasons were listed, while a single symptom/condition was given in 14 (28%) of the admissions; there were 86 indications in total. Overall, the most frequent indications were gastrointestinal problems such as nausea/vomiting, diarrhoea and obstipation (n=22/86, 26%), lung problems such as dyspnoea, pleural effusion, pneumonia, embolism (n=17/86, 20%), pain (n=13/86, 15%) and reduced performance status (n=8/86, 9%) (figure 1).
Figure 1.
Most frequent reasons for the emergency admissions.
Fifty per cent (n=25) of the emergency admissions were administered by a hospital doctor, and 24% (n=12) by the patient's general practitioner (GP) or a GP on call. In 45 (90%) cases, patients were admitted from home, four patients came from the hospitals’ outpatient clinic, and one from a nursing home. Forty-eight per cent (n=24) were transported by ambulance. In seven cases, an ‘open return’ was established as part of the patient's care plan. However, only two patients were admitted directly to the appropriate hospital unit, while the remaining had to wait in the ER for up to 7 h. Twenty-three (46%) patients had been discharged from the hospital less than 1 month prior to the actual admission.
The highest number of emergencies, 18 of 50, occurred on Mondays. Overall, 19 (38%) of the admissions took place outside regular working hours, that is, 20:00 to 5:00 on weekdays. Fourteen (74%) of these occurred from Friday night through Sunday.
Median length of stay was 7 days (1–35). Most discharges, 28/45 (62%), were to the patient's home, 8 (18%) discharges were to a nursing home and 5 (11%) were transferred to another hospital or a specialised palliative care unit.
Examinations and interventions
x-Ray, CT scans, ultrasound examinations and MRIs were performed in 66 (n=33), 48 (n=24), 24% (n=12) and 8% (n=4) of the cases, respectively. Six patients had none of these procedures performed, three patients went through three of these, while one patient had all four performed, prior to abdominal surgery. Seven patients had an ECG taken during their stay. Four patients went through surgical procedures: abdominal surgery (n=1), insertion of stents (n=2) and a central venous catheter (n=1). None of the patients went directly to the ICU upon admission. One patient, however, experienced severe complications related to dialysis during hospitalisation, was admitted to the ICU after 2 days and subsequently died.
Several standard procedures were performed during hospitalisation, with hydration (n=39, 78%), antibiotics (n=21, 42%), and oxygen therapy (n=15, 30%) being the ones most frequently employed (figure 2). The maximum number of registered procedures per patient was twelve, while the minimum was three. About one-third of the patients (n=15) were seen by an oncologist, while more than 50% (n=26) were approached by the hospital palliative team.
Figure 2.
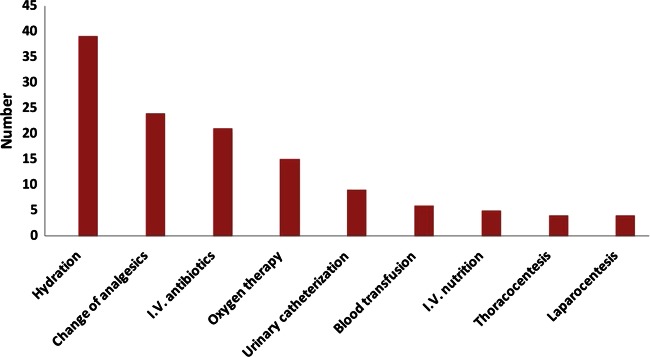
Most frequent interventions during hospitalisation.
Pain was prominent, and pain-related procedures were performed in all but seven cases. The main reasons for admission in these seven cases were dyspnoea (n=3), reduced performance status (n=2) and problems in swallowing (n=2). Two-thirds used strong analgesics such as morphine, fentanyl or oxycodon upon admission, mostly as slow release tablets or patches.
The most frequent pain-related interventions were changes in the analgesic regimen (n=24) such as opioid switch, adding a coanalgesic or increasing the dosage. Two patients had an epidural catheter inserted; one of these also had a coeliacus blockage and a spinal catheter.
Symptom assessment, ESAS scores
Both ESAS forms were completed in 76% of the cases. Missing forms were a result of death (n=5), discharge earlier than planned and administrative failure (n=7).
The median number of days from admission to the first ESAS was 1 (0–3), with a median of 5 days between assessments (1 and 20). ESAS number 2 was completed shortly before discharge on the same day (48%) or the day before (12%). Table 2 displays the ESAS mean scores at inclusion and at discharge. Pain at rest and pain at movement were significantly reduced during the stay, with a reduction of 1.7 for both between assessments (p<0.01). The highest mean intensity scores at inclusion were found with tiredness (6.1), appetite (5.6) and oral dryness/xerostomia (5.1). Upon discharge, 6 patients reported a score above 3 for pain at rest, while 11 patients had a pain score exceeding 3 for pain at movement.
Table 2.
ESAS scores at inclusion and prior to discharge of patients*
| Symptoms | First assessment† | Second assessment† | Difference in mean scores of first and second ESAS | p Value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Pain at rest | 3.2 (2.8) | 1.5 (1.9) | 1.7 | <01 |
| Pain at movement | 4.4 (3.1) | 2.7 (2.7) | 1.7 | <01 |
| Tiredness | 6.1 (2.5) | 5.5 (2.6) | 0.6 | NS |
| Nausea | 1.7 (2.5) | 1.3 (2.0) | 0.4 | NS |
| Shortness of breath | 3.0 (2.9) | 2.8 (3.2) | 0.2 | NS |
| Oral dryness (xerostomia) | 5.1 (2.7) | 5.2 (2.6) | −0.1 | NS |
| Appetite | 5.6 (2.9) | 5.0 (2.4) | 0.6 | NS |
| Anxiety/uneasiness | 1.9 (2.5) | 2.3 (2.7) | −0.4 | NS |
| Depression/sadness | 2.3 (2.7) | 2.9 (3.0) | −0.6 | NS |
| “Overall, how are you feeling today?” | 4.5 (2.3) | 4.2 (2.1) | 0.3 | NS |
*Numerical rating scale (0–10) with higher scores implying higher symptom intensity.
†N varies between 38 and 34 because of missing items on some of the forms.
NS, not significant.
The mean ESAS scores at inclusion in the 12 cases in which the second form was not completed were compared with the scores from those who completed both. No significant differences were found.
Patients’ interviews
Patients were asked to mention the two most bothersome symptoms leading to hospitalisation. Gastrointestinal symptoms including nausea/vomiting, diarrhoea and appetite loss (n=24, 48%), fatigue (n=19, 38%), pain (n=18, 38%) and dyspnoea (n=10, 20%) were the most frequent reasons according to the patients. In most cases (n=32, 64%), patients said the symptoms had developed over several days, and this was reported by all the 18 patients who were admitted on a Monday. Six (12%) patients reported a more acute onset with symptoms developing during a few hours. Four of these patients came to the hospital outside normal working hours. Nineteen (38%) patients received regular medical care at home from the community health system, such as nursing services and domestic assistance, or both. When asked about preference for care, the majority of patients (n=33, 66%) preferred hospital admission to other places in the actual situation. Nine (18%) patients said they would have liked to have received medical treatment at home, given that necessary resources and equipment were available, while four (8%) would have preferred a nursing home.
Free comments were provided in 44 interviews. Seven (16%) patients perceived the delays in the emergency unit as tiring and unnecessary, while another seven (16%) found them acceptable. Two (5%) patients specifically stated that they would have preferred direct admission to the appropriate hospital unit, while another two (5%) had a desire to go directly to the palliative care unit. In 10 (23%) interviews, patients said they felt safer at hospital than at home given the actual situation. Seven (70%) of them were 65 years or older, but only one was living alone. Four (10%) patients expressed concerns about the caregiver burden imposed on their partner. The most frequently raised comments in the interviews (n=11, 25%) were related to doubts whether the home care services had the required competence and expertise to handle the situation.
Nevertheless, 10 (23%) patients said they would have preferred to have got simple procedures such as intravenous nutrition and hydration at home. In their opinion, specialised care teams and home visits by their GP were the most important actions to prevent emergency admissions.
Discussion
This small, descriptive study from two acute-care Norwegian hospitals serving local, urban areas shows that relatively simple procedures were performed in most of the emergency cases. Standard interventions such as hydration, antibiotics and oxygen therapy were most common, corresponding well with the most frequent reasons for admission. In many cases, these procedures may well be administered in the primary healthcare sector.
Pain, gastrointestinal and respiratory problems were prominent, well in line with other studies of emergency admissions.4 5 21 22 These are frequent symptoms in advanced patients with cancer, and may indicate disease progression. One study demonstrated a significant relationship between signs of disease progression and short-term mortality (<90 and <180 days) in symptomatic patients with cancer coming to the ER,22 in line with other reports.23 24 Although the present study was too small to perform valid analyses of a possible relationship between symptoms and survival, our sample consisted of patients with cancer in the palliative phase of the disease, and more than 50% were dead 90 days after discharge. This suggests that standard medical procedures were indicated for most of the patients, and more advanced procedures in some cases only.
Thirty-eight per cent of the admissions were outside normal working hours, a lower proportion than that reported elsewhere.21 In most cases, patients said that symptoms had developed over time. Monday had the highest percentage of emergency admissions as found by others,21 which corresponds to a gradual onset of symptoms, as reported by all the patients admitted on Mondays. It may also be that patients tried to avoid going on weekends and waited until Monday before contacting the hospital or the GP.
Many common symptoms are bothersome and distressing and known to cause considerable anxiety in patientsand in relatives. Thus, it should be remembered that causes other than strict medical, somatic indications may lead to hospital admissions, for example, reduced performance status, frailty, loneliness and psychological distress that often coexist. Some patients commented that they felt safer at hospital than at home, and that they wanted to reduce the burden imposed on their family by the disease. Causes like this may be more common in smaller hospitals serving a well-defined area compared with larger university clinics. In our opinion, maybe the most important issue raised by this study is not whether hospital admission was indicated per se, but if hospital admission as an emergency case was most appropriate for getting necessary medical care. However, we also believe that a higher level of specialist palliative care competence in the home care services and closer collaboration between these services and the hospital may reduce the need for emergency admissions.
This also relates to the fact that about 50% of the admissions were administered by a hospital doctor, twice as many as by GPs (24%). The standard pathway for hospital admissions in Norway is through the family GP, unless there is an emergency. The fact that our sample consisted of palliative care patients with an affiliation to the local hospital may explain why the hospital doctors were so frequently contacted. It is noteworthy, however, that a home visit by a medical doctor was mentioned as the most wanted intervention that could possibly have prevented the emergency admission. Shorter hospital stays, and more people living longer at home with advanced disease, represent a challenge for the primary healthcare sector, specifically so for the GPs25 26 as they are crucial in the follow-up and care for patients with advanced cancer outside hospital.27 One study found that a higher number of visits to the family doctor was inversely associated with the number of visits to the ER in patients dying from cancer.28
In our opinion, this points to two important aspects related to palliative care, namely that it is misconstrued as end-of-life care only,11 and that it should be integrated into standard oncology on the diagnosis of metastatic or advanced cancer. WHO emphasises that palliative care is applicable early in the course of illness29 owing to a systematic approach to symptom relief, enhanced quality of life of patient and caregivers, less use of emergency care services and a timelier referral to specialised palliative care, which often takes place too late.12 21 30
The fact that many patients with advanced cancer see acute-care providers makes systematic follow-up less common, and means that collaborative care plans across organisational levels are not available, even if needed. Home care of patients with advanced cancer should be taken care of by specialist teams with easy access to hospital-based palliative care specialists, in close collaboration with the family doctor. Pain-related interventions were performed in almost all patients, and there was a significant decline in the mean pain scores (mean 1.7) on ESAS from admission to discharge. A recent study in more than 200 patients showed that a decrease of 1.2 units in the ESAS pain score constituted a clinically relevant improvement.31 A change in the analgesic regimen was the most frequent procedure, and it is reason to believe that this and other simple procedures could have been performed at home, if the resources in the form of necessary competence were available. This may reduce the dependency on the local hospital and reduce the number of emergency admissions.
One limitation is the lack of information about performance status and current disease status at admission, both important predictors of survival and disease progression.22 This might have provided more valid information about the necessity of being admitted as an emergency case. The majority of patients had metastatic disease and few received tumour-directed treatment upon admission, indicating that the majority were in the late stages of the disease. Additionally, lung symptoms, reported as an independent predictor of death within 90 and 180 days,22–24 were among the most frequent reasons for admission. Although some patients needed more advanced procedures (surgery, CT scans and MRIs), relatively simple procedures like hydration, antibiotics and change in analgesics were most common. This may be taken to indicate that an emergency hospital admission was necessary for some patients, but not for all. To perform a valid investigation of the ‘true’ proportion of patients needing emergency admissions, a larger study with thorough objective examinations and detailed registrations of all interventions and a close follow-up is necessary, which was beyond the scope of this descriptive study. This is also related to the limitation caused by the small sample size and the fact that the study was confined to two hospitals only. The first does not allow for advanced statistics and subgroup comparisons, while the second may limit the generalisability. On the other hand, there are many relatively small acute-care hospitals in Norway serving a limited catchment area with a well-organised primary healthcare sector. It could be argued that more knowledge about the extent and quality of the home care nursing services, as well as the amount of patients’ contact with the GP, would have provided important information about the need for an emergency admission. This is true, but we also believe that a small study like this makes the findings relevant to consider in discharge planning and palliative care follow-up, as was our intention with the present study. Also, the fact that all consecutive emergency cases in the actual time period were considered for inclusion is a major strength, in our opinion. Furthermore, quantitative registrations combined with interviews give a better picture of the patients’ experiences than registry-based studies alone.
The fact that close to 50% of our patients had been discharged from hospital less than 1 month prior to the actual admission emphasises the need to improve the continuity of care through a systematic follow-up and treatment plan, which are the cornerstones of palliative care. This may actually have a double effect, preventing a rapid development in symptom intensity and improving the feeling of safety for patients and their families, thereby reducing the need for emergency admissions.
Conclusion
Emergency admissions may represent stressful events for patients and relatives. This study showed that many patients needed simple procedures only. About two-thirds preferred hospital admission to other places of care, and about one-fourth expressed that they felt safe in the hospital in the actual situation. Higher levels of expertise, easier access to medical doctors outside hospital and better lines of cooperation between hospitals and the primary healthcare services may reduce the need for emergency admissions.
Supplementary Material
Acknowledgments
The authors would like to thank Marit S Jordhøy, Norway, who gave valuable advice on the protocol and manuscript writing, and Irmelin Bergh who helped out in the initial phase of study planning. The authors also thank the study coordinators at the participating centres and the patients who took part in the study.
Footnotes
Contributors: MJH, JK, NA and SBH conceived the idea of the study and were responsible for the design of the study. SBH, AN and AOL were responsible for data collection, quality assurance and data compilation. MJH, NA and JK were responsible for undertaking the data analysis and produced the tables and graphs. All the coauthors contributed to the interpretation of the results and provided input into the data analysis. The initial draft of the manuscript was prepared by MJH, JK and NA and then circulated among all the authors who provided input and comments on multiple occasions.
Funding: This project was supported in part by a grant from the Department of Research at Østfold Hospital Trust, Norway.
Competing interests: None.
Ethics approval: Regional Committee for Medical and Health Research Ethics, Norwegian Social Science Data Services (NSD), the institutional review boards at the two hospitals.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Kreftregisteret, Cancer Registry of Norway. 2011. http://www.kreftregisteret.no/en/ (accessed Nov 2012)
- 2.Verdecchia A, Francisci S, Brenner H, et al. Recent cancer survival in Europe: a 2000–02 period analysis of EUROCARE-4 data. Lancet Oncol 2007;9:784–96 [DOI] [PubMed] [Google Scholar]
- 3.Earle CC, Park ER, Lai B, et al. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol 2003;21:1133–8 [DOI] [PubMed] [Google Scholar]
- 4.Yates M, Barrett A. Oncological emergency admissions to the Norfolk and Norwich University Hospital: an audit of current arrangements and patient satisfaction. Clin Oncol (R Coll Radiol) 2009;3:226–33 [DOI] [PubMed] [Google Scholar]
- 5.Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CAMJ 2010;182:563–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Earle CC, Neville BA, Landrum MB, et al. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 2004;2:315–21 [DOI] [PubMed] [Google Scholar]
- 7.Huang J, Boyd C, Tyldesley S, et al. Time spent in hospital in the last six months of life in patients who died of cancer in Ontario. J Clin Oncol 2002;6:1584–92 [DOI] [PubMed] [Google Scholar]
- 8.Barbera L, Paszat L, Chartier C. Indicators of poor quality end-of-life cancer care in Ontario. J Palliat Care 2006;1:12–17 [PubMed] [Google Scholar]
- 9.Ho TH, Barbera L, Saskin R, et al. Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada. J Clin Oncol 2011;12:1587–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Earle CC, Landrum MB, Souza JM, et al. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol 2008;23:3860–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith TJ, Temin S, Alesi ER, et al. American society of clinical oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 2012;8:880–7 [DOI] [PubMed] [Google Scholar]
- 12.Bruera E, Hui D. Integrating supportive and palliative care in the trajectory of cancer: establishing goals and models of care. J Clin Oncol 2010;25:4013–17 [DOI] [PubMed] [Google Scholar]
- 13.Dudgeon DJ, Knott C, Eichholz M, et al. Palliative Care Integration Project (PCIP) quality improvement strategy evaluation. J Pain Symptom Manage 2008;6:573–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higginson IJ, Evans CJ. What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J 2010;5:423–35 [DOI] [PubMed] [Google Scholar]
- 15.Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 2007;7:993–1000 [DOI] [PubMed] [Google Scholar]
- 16.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009;7:741–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.2010. International Classification of Diseases ICD-10. http://www.who.int/classifications/icd/en/ (accessed Nov 2012)
- 18.Norwegian Cause of Death Registry. 2010. http://www.ssb.no/english/subjects/03/01/10/dodsarsak_en/ (accessed Nov 2012)
- 19.Nekolaichuk C, Watanabe S, Beaumont C. The Edmonton Symptom Assessment System: a 15-year retrospective review of validation studies (1991–2006). Palliat Med 2008;2:111–22 [DOI] [PubMed] [Google Scholar]
- 20.Bruera E, Kuehn N, Miller MJ, et al. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 1991;2:6–9 [PubMed] [Google Scholar]
- 21.Mayer DK, Travers D, Wyss A, et al. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 2011;19:2683–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geraci JM, Tsang W, Valdres RV, et al. Progressive disease in patients with cancer presenting to an emergency room with acute symptoms predicts short-term mortality. Support Care Cancer 2006;10:1038–45 [DOI] [PubMed] [Google Scholar]
- 23.Escalante CP, Martin CG, Elting LS, et al. Identifying risk factors for imminent death in cancer patients with acute dyspnea. J Pain Symptom Manage 2000;5:318–25 [DOI] [PubMed] [Google Scholar]
- 24.Vigano A, Dorgan M, Bruera E, et al. The relative accuracy of the clinical estimation of the duration of life for patients with end of life cancer. Cancer 1999;1:170–6 [PubMed] [Google Scholar]
- 25.Menten J, De Lepeleire J. Emergency hospital admission for pain in palliative patients: a crucial role for general practitioners. Eur J Gen Pract 2006;3:133–4 [DOI] [PubMed] [Google Scholar]
- 26.Wiese CH, Bartels UE, Ruppert D, et al. Treatment of palliative care emergencies by prehospital emergency physicians in Germany: an interview based investigation. Palliat Med 2009;4:369–73 [DOI] [PubMed] [Google Scholar]
- 27.Wiese CH, Bartels UE, Marczynska K, et al. Quality of out-of-hospital palliative emergency care depends on the expertise of the emergency medical team—a prospective multi-centre analysis. Support Care Cancer 2009;12:1499–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burge F, Lawson B, Johnston G. Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care 2003;41:992–1001 [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. 2011. http://www.who.int/cancer/palliative/definition/en/ (accessed Nov 2012)
- 30.Daugherty CK, Steensma DP. Overcoming obstacles to hospice care: an ethical examination of inertia and inaction. J Clin Oncol 2003;21(9 Suppl):42s–5s [DOI] [PubMed] [Google Scholar]
- 31.Bedard G, Zeng L, Zhang L, et al. Minimal clinically important differences in the Edmonton Symptom Assessment System in patients with advanced cancer. J Pain Symptom Manage 2012. Epub ahead of print, Nov 21. doi: 10.1016/j.jpainsymman.2012.07.022 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.