Abstract
A 25-year-old lady presented with hypertensive encephalopathy. She also had chronic refractory hypertension for the past 7 years. Workup revealed persistent hypokalaemia with metabolic alkalosis suggesting hyperaldosteronism. Hyperaldosteronic states such as renal artery stenosis, Conn's syndrome and Liddle's syndrome were ruled out. Her plasma renin activity was high. Contrast-enhanced CT of the abdomen showed a 1.9×2 cm heterogeneously enhancing lesion in the anterior aspect of the right kidney suggesting a possibility of reninoma. The benign tumour was resected by a nephron-sparing surgery. Histopathology suggested a juxtaglomerular cell tumour. Anti-hypertensive drugs were completely withdrawn postoperatively.
Background
Refractory hypertension in young is often secondary and potentially curable. The triad of hypokalaemia, metabolic alkalosis and refractory hypertension act as clues to hyperaldosteronic state. When plasma renin activity (PRA) is high in the absence of renal artery stenosis (RAS), a renin-secreting tumour (RST) (Reninoma) should be considered and carefully looked for in imaging. Our patient was found to have this rare tumour, which on surgical resection resulted in a complete cure of hypertension.
Case presentation
A 25-year-old woman presented with hypertensive encephalopathy and weakness of limbs to the emergency services after a brief period of drug default. Her blood pressure at admission was 220/120 mm Hg. A CT of the brain at admission showed diffuse cerebral oedema. Ophthalmic fundus examination revealed bilateral papilloedema. Hence, she was managed as a case of hypertensive emergency and blood pressure was controlled with sodium nitroprusside infusion. Subsequently, her blood pressure was partially controlled with antihypertensives of four different classes. When her sensorium improved, she came out with a history of receiving antihypertensives from 18 years of age. She had four similar episodes of hypertensive emergencies in the past 6 years.
Differential diagnosis
Initially, secondary hypertension was considered in view of the young age at presentation, absence of family history, repeated episodes of hypertensive emergencies and a refractory hypertension. Aortic interruption was unlikely as there was no radio-femoral delay and all peripheral pulses were palpable. There was no renal bruit. Overt clinical features of hyperthyroidism, hypothyroidism, pheochromocytoma or Cushingoid features were absent. Obstructive sleep apnoea is unlikely in view of normal body mass index and no day time somnolence.
Serum creatine was normal. Hypokalaemia was persistent with urinary excretion of potassium in the normal range (45 mmol/l per day). Arterial blood gas analysis revealed metabolic alkalosis. Owing to the presence of hypokalaemia with metabolic alkalosis in the setting of severe hypertension, hyperaldosteronic states were considered. The causes of hyperaldosteronism are given in figure 1. Since the clinical presentation of RAS due to fibromuscular dysplasia usually occurs in a young female with features of hyperaldosteronism, ultrasound Doppler and MR angiography to rule out RAS were done initially and was found to have no evidence for RAS.
Figure 1.
Causes of hyperaldosteronism.
Liddle's syndrome was also suspected, but there was no response in blood pressure to a therapeutic trial of Tab. Amiloride. Contrast-enhanced CT (CECT) scan was done to rule out the possibility of adrenal adenoma or hyperplasia. There was no evidence of any adrenal involvement. There is no history of liquorice intake (11β HSD-2 deficiency). The absence of virilisation and growth retardation rule out 11β hydroxylase deficiency. There is no amenorrhoea to suggest 17α hydroxylase deficiency.
On close examination of the CECT of the abdomen, a well-circumscribed heterogeneously enhancing lesion of about 2×2 cm was seen in the anterior pole of the right kidney, suggesting a possibility of reninoma (figure 2). Hence, PRA and plasma aldosterone (PA) levels were measured. PRA was 9 ng/ml/h (normal: 0.16–2.33 ng/ml/h) and the PA was 5.2 ng/dl (normal: 6–25 ng/dl). Bilateral renal vein sampling for the estimation of PRA could not be done.
Figure 2.

Contrast-enhanced CT scan of the abdomen showing a heterogeneously enhancing mass in the anterior cortex of the right kidney (arrow).
Treatment
Since imaging showed a well-defined lesion in renal cortex along with an increased PRA, reninoma was strongly considered. The patient was taken up for a nephron-sparing surgery after obtaining an informed consent. The surgery was uneventful. Postoperatively, she required a daily dose of 5 mg of amlodipine to control her blood pressure, which was tapered and stopped in 2 weeks time.
Outcome and follow-up
The tumour was well circumscribed with a soft fleshy pale pink appearance, measuring 2 cm in its maximum dimension (figure 3A).
Figure 3.
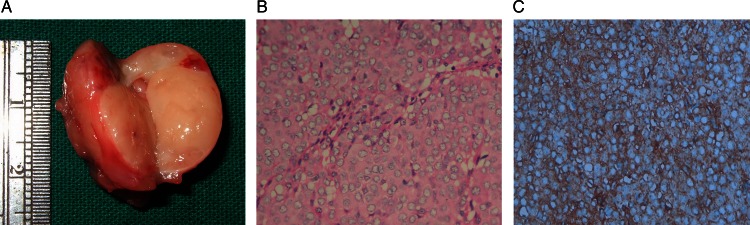
(A) Cut section showing a well-circumscribed tumour with a soft fleshy pale pink appearance measuring 2 cm in the maximum dimension. (B) Islands of monomorphic tumour cells with vesicular nucleus, arranged in an organoid pattern (H&E ×400). (C) Tumour cells showing positivity for CD34 (IHC ×400).
Histology showed monomorphic polygonal cells with moderate ill-defined cytoplasm and vesicular nucleus (figure 3B). These cells were arranged in islands and surrounded by blood vessels which showed arteriosclerosis. On immune-histochemical staining, tumour cells were positive for CD34 (figure 3C), but were negative for HMB-45, melanin A, cytokeratin and smooth muscle actin. The features were compatible with a juxtaglomerular cell tumour.1 Electron microscopy to demonstrate the renin secretory granules could not be done.
She was off antihypertensive drugs at discharge and remained normotensive at 1 year follow-up.
Discussion
RST or reninoma was first reported by Robertson et al. in 1967.2 Since then, less than 100 cases of RST has been reported so far.3 4 Reninoma is a benign functional tumour of the juxtaglomerular apparatus, characterised by the excess secretion of renin, thus causing secondary hypertension.1
In our case, imaging techniques and the level of PRA suggested the presence of a RST, and histopathology confirmed it to be a reninoma. With tumour resection, she had a complete resolution of hypertension.
Though renin is a preformed hormone and the tumour is highly vascular, blood pressure fluctuations were not noted during surgery. Mild hypertension persisted for about 2 weeks in the postoperative period. This is not explained by the half-life (∼15 min) of renin.
Although PA estimation was done with necessary precautions, the level was low and did not correlate with our clinical diagnosis. It has been reported in the literature that the levels of aldosterone are subject to diurnal variation and are affected by volume status, potassium levels, emotional stress and posture. Also, the measurement of aldosterone level requires withholding spironolactone and diuretics for 6 weeks, withholding beta blockers and calcium channel blockers for a week, unrestricted salt intake for 4 days and standing for 2 h prior to blood sampling.5 6 Since our patient presented to us in hypertensive crisis with resistant hypertension requiring four different classes of antihypertensive drugs for control of hypertension, withholding the drugs for the estimation of PA was difficult, and hence the PA estimation could not be repeated.
Renal vein catheterisation and sampling for PRA, which is the ideal means of diagnosing reninoma, could not be done in our patient. However, this was not performed in all the cases of reninoma reported in the literature. Moreover, in some case reports, the renal vein catheterisation failed to provide adequate localisation of the tumour7; in one study,8 CT scan has remained more useful than lateralisation of renin activity in renal vein sampling.
It is distressing to note that the patient had gone undiagnosed for many years even though she had many clinical reasons to suspect secondary causes of hypertension. Hypokalaemia could have been masked by the ACE inhibitors she received earlier. But, her drug default prior to this admission helped in revealing hypokalaemia and metabolic alkalosis which helped us in unmasking the aetiology and curing hypertension.
Learning points.
Refractory hypertension and persistent hypokalaemia could be clues to a hyper-reninemic state.
In patients without an established cause of hypertension, the use of ACE inhibitors could mask the hypokalaemia and detection of hyper-reninism.
In the absence of imaging evidence for renal artery stenosis or adrenal involvement, one should carefully look for a well-defined mass in the cortex of kidney.
Nephron-sparing surgical excision of tumour offers complete cure.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Martin SA, Mynderse LA, Lager DJ, et al. Juxtaglomerular cell tumour: a clinicopathologic study of four cases and review of the literature. Am J Clin Pathol 2001;2013:854–63 [DOI] [PubMed] [Google Scholar]
- 2.Robertson PW, Klidjian A, Harding LK, et al. Hypertension due to a renin-secreting renal tumour. Am J Med 1967;2013:963. [DOI] [PubMed] [Google Scholar]
- 3.Wong L, Hsu THS, Perlroth MG, et al. Reninoma: a case report and literature review. J Hypertens 2008;2013:368–73 [DOI] [PubMed] [Google Scholar]
- 4.Gottardo F, Cesari M, Morra A, et al. A kidney tumor in an adolescent with severe hypertension and hypokalemia: an uncommon case—case report and review of the literature on reninoma. Urol Int 2010;2013:121–4 [DOI] [PubMed] [Google Scholar]
- 5.Helena AG, Amal FF. Evaluation of endocrine function. In McPherson RA, Pincus MR, eds. Henry's clinical diagnosis and management by laboratory methods. 22nd edn Philadelphia: WB Saunders Elsevier, 2011:397–400 [Google Scholar]
- 6.William FY. Endocrine hypertension. In Shlomo M, Kenneth SP, Larsen PR, Henry MK, eds. Williams textbook of endocrinology. 12th edn Philadelphia: WB Saunders Elsevier, 2011:562–9 [Google Scholar]
- 7.Baruch D, Corvol P, Alhenc-Gelas F, et al. Diagnosis and treatment of renin-secreting tumors. Report of three cases. Hypertension 1984;2013:760–6 [DOI] [PubMed] [Google Scholar]
- 8.Corvol P, Pinet F, Plouin PF, et al. Renin-secreting tumours. Endocrinol Metab Clin North Am 1994;2013:255–70 [PubMed] [Google Scholar]



