Abstract
A case of an immunocompetent 51-year-old healthy man with chronic recurrent disciform corneal oedema and hypertensive anterior uveitis in the right eye for 2 years was unresponsive to topical corticosteroid and systemic acyclovir. Diagnostic anterior chamber tapping was performed and viral DNA PCR was positive for both cytomegalovirus and herpes simplex virus. The patient was treated with both oral valganciclovir for 3 months and long-term oral acyclovir. His condition improved significantly after the treatment; intraocular pressure and anterior chamber inflammation were controlled and the remaining keratic precipitates in the cornea started to clear up.
Background
We believe this is the first case of concomitant infection with herpes simplex virus (HSV) and cytomegalovirus (CMV) endotheliitis in a healthy patient. Apart from the brain and the skin, there are limited data on concomitant infection of these two viruses in immunocompetent patients.1 This patient was presented with disciform endotheliitis which is the most common presentation of HSV endotheliitis. He was misdiagnosed as having only HSV endotheliitis and was treated with systemic acyclovir and topical corticosteroid for 2 years. After PCR, HSV and CMV were both positive. As a result of this, systemic valganciclovir was combined with acyclovir and the patient's clinical condition significantly improved.
Lessons learnt from this case are that when both the clinical and the treatment failure for corneal endotheliitis with topical corticosteroid and systemic acyclovir cannot explain the causes of the disease, the additional investigation is necessary such as aqueous tapping for CMV and in vivo confocal microscopy. Accurate and prompt treatment should be ensued immediately after a confirmed diagnosis to prevent deleterious results.
Case presentation
A 51-year-old healthy man had a chronic recurrent corneal oedema with hypertensive anterior uveitis in the right eye since 2007. Topical steroids and mydriatics were started. Oral acyclovir and topical antiglaucoma treatment were given with initial good clinical response. For approximately 2 years, the patient continued to use steroids periodically and prophylactic dose of oral acyclovir. Despite this, the inflammation did not resolve and the intraocular pressure (IOP) started to increase. The condition became difficult to control with the maximal antiglaucoma medications. A cataract developed. He received trabeculectomy in the right eye in October 2008 at another hospital. But corneal oedema and anterior uveitis continued after the operation and did not respond to oral acyclovir, topical corticosteroid and 3% NaCl eye drop. He was eventually referred to us in February 2009. There was nothing contributory in his left eye.
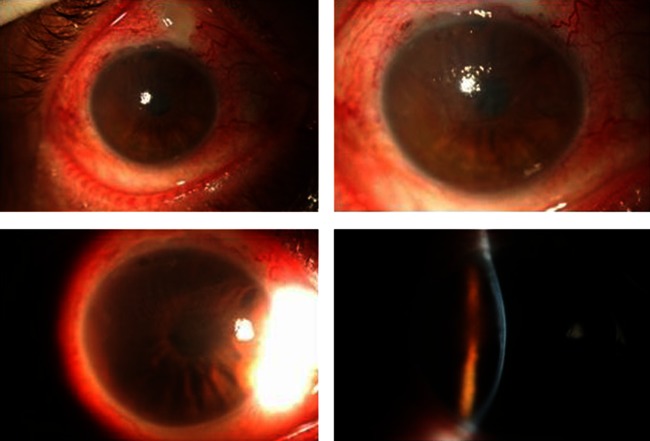
He complained of photophobia and mild ocular discomfort. The BCVA was hand-motion in the right eye and 20/20 in the left eye. Slit-lamp examination showed ciliary injection. The conjunctival bleb was high and avascular in the upper quadrant of the nasal passage. The IOP was 10 mm Hg in the right eye. There was a round area of stromal oedema overlying the keratic precipitates (KPs) in the superior paracentral cornea. The oedematous area spanned the entire stromal thickness with a ground-glass appearance. The stroma was void of infiltrate and neovascularisation. The epithelium showed microcystic oedema overlying the areas of the stromal oedema. The anterior chamber had a 1+ inflammatory reaction without flare. No iris atrophy or posterior synechiae was detected. The fundus appeared normal (figure 1).
Figure 1.
Right eye shows disciform corneal endotheliitis with multiple small keratic precipitates in a circumferential pattern with associated localised corneal edema.
Investigations
Diagnostic anterior chamber tapping was performed and followed by real-time quantitative PCR to detect herpes viridae DNA including HSV I and II, varicella zoster virus (VZV), CMV and Epstein-Barr virus (EBV). The aqueous viral DNA PCR was positive for CMV and HSV but negative for EBV. The blood test was negative for HIV, tuberculosis and syphilis, and the HLA-B27 allele was negative.
In vivo confocal microscopy of the right eye showed an owl's eye appearance of the corneal endothelium (figure 2). Pachymetry was 710 µm at the oedematous area.
Figure 2.
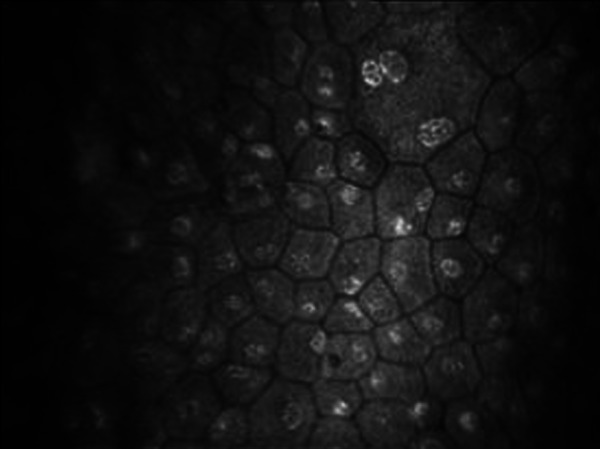
Confocal microscope showed the owl's eye appearance (a group of large cells whose nuclei have a high reflection area surrounded by a halo of low reflection), a pathognomonic sign of CMV infection in the corneal endothelium.
Differential diagnosis
Localised round corneal oedema with KPs was present only under the area of the oedema which supports the notion that the inflammation is closely related to the endothelial decompensation. Endotheliitis is the primary diagnosis.
The differential diagnosis for corneal endotheliitis with chronic refractory hypertensive anterior uveitis was concomitant infections with HSV, VZV and CMV infection. For this patient, disciform endotheliitis was unresponsive to systemic acyclovir and the owl's eye pattern from confocal microscopy led the physicians to the diagnosis of CMV endotheliitis.
Treatment
The results from the PCR confirmed the diagnosis of concomitant HSV and CMV endotheliitis.
The patient received oral valganciclovir 900 mg twice a day for 6 weeks as the loading dose and then 450 mg twice daily for 6 weeks. Topical corticosteroid was slowly tapered from every 2 h to EOD depending on the severity of the anterior chamber inflammation. At 6 weeks after the start of oral valganciclovir, the corneal oedema gradually improved. Oral acyclovir 400 mg was also administered five times a day for 2 weeks after HSV was positive from the PCR test, then followed by 800 mg once daily as a prophylaxis.
Outcome and follow-up
After a complete course of treatment with oral valganciclovir and acyclovir, the cornea cleared up but multiple small KPs persisted (figures 3 and 4). Anterior chamber inflammation had subsided. Post-treatment aqueous viral DNA obtained on June 2010 for the PCR test continued to yield a positive result for only HSV. As a result of this, long-term oral acyclovir 800 mg was administered once daily as a prophylactic dose. The aqueous viral DNA PCR was repeated again on January 2011 which yielded negative results for both HSV and CMV.
Figure 3.
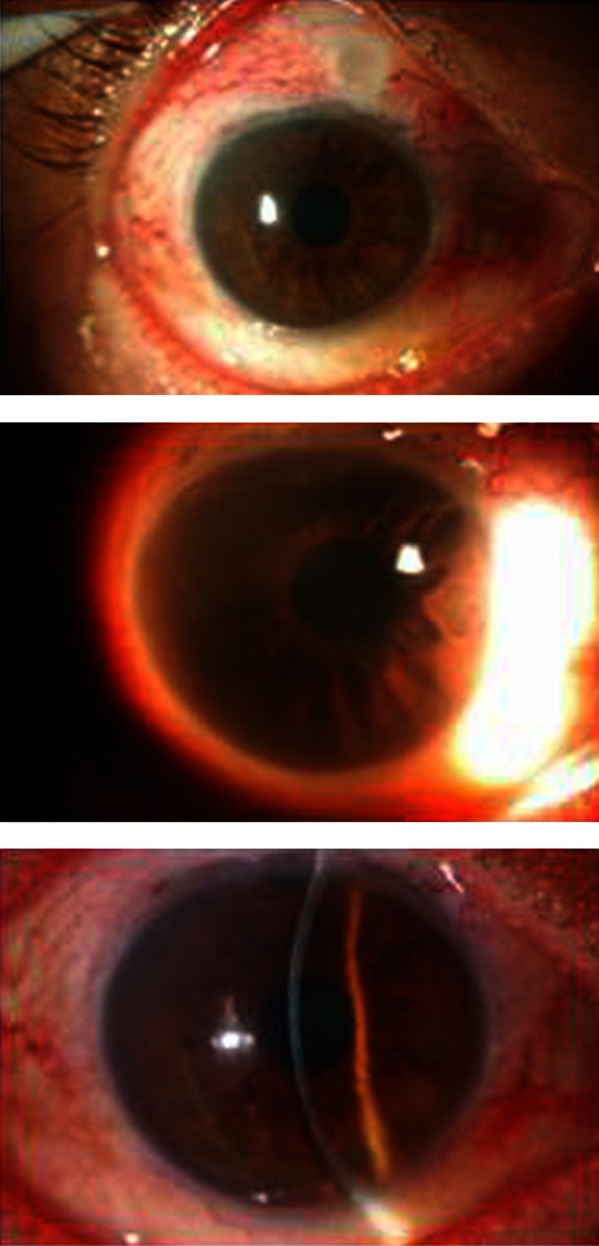
Right eye at 6 weeks after treatment with oral valganciclovir and acyclovir, corneal edema gradually subsided but keratic precipitates still existed.
Figure 4.
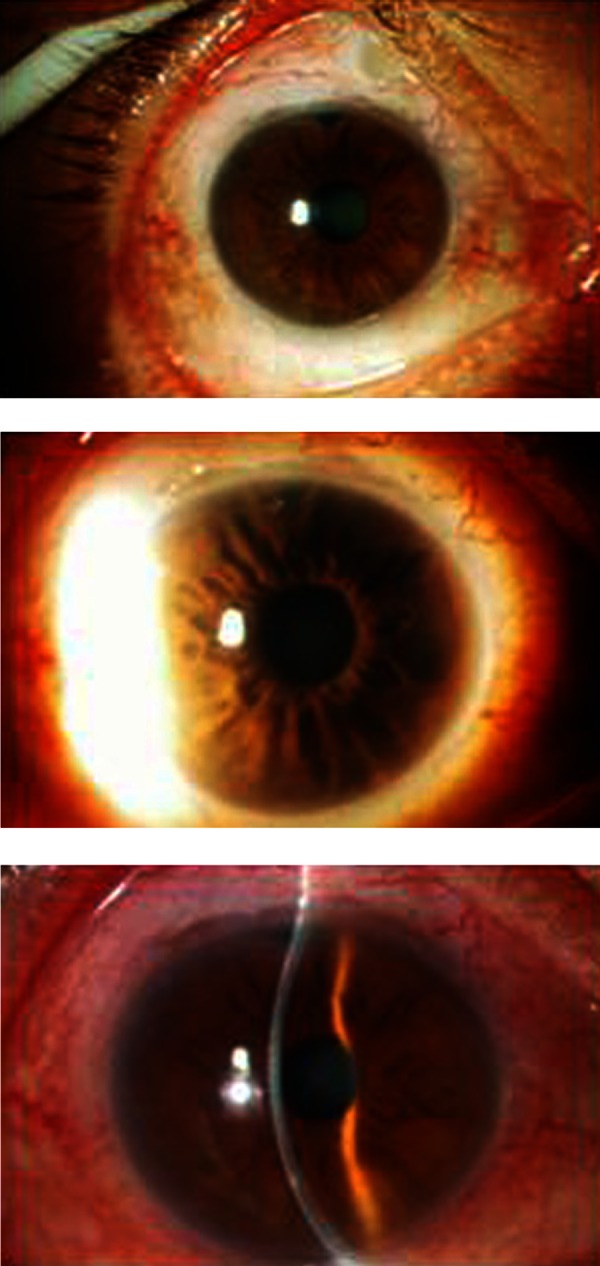
Right eye at 12 weeks after treatment with oral valganciclovir and acyclovir, no corneal edema seen and anterior chamber was quiet.
The cornea remained clear and the best-corrected visual acuity in March 2011 was the Finger count for 2 feet in the right eye due to dense posterior subcapsular cataract. The last IOP was 11 mm Hg. The pachymetry was 537 um. Unfortunately, the affected eye had only 558 corneal endothelial cells/mm2 which indicated that there was a significant cell loss compared with the normal fellow eye (2586 cells/mm2). Owing to the low endothelial cell count, two additional treatments of choice were recommended and administered to improve the patient's vision: Phacoemulsification with IOL followed by penetrating keratoplasty or triple procedure depending on the availability of the donated eye.
Discussion
Corneal endotheliitis is an intriguing clinical entity manifested by corneal oedema, KPs, and mild anterior chamber reaction, and can be defined as a spectrum of the disorder in which the corneal endothelium is the primary site of the inflammation. Corneal endotheliitis can be classified clinically into four forms: linear, sectorial, disciform and diffuse, based on the distribution of the KPs and configuration of the overlying stromal and epithelial oedema.2 3 A mild-to-moderate iritis accompanies endotheliitis with occasional elevation of IOP.
This patient had disciform endotheliitis, the most common manifestation of the corneal endotheliitis, forming a round or disc-shaped stromal oedema in superior paracentral region of the cornea with a definite boundary between affected and unaffected areas. There were numerous KPs on the corneal endothelium inside the oedematous area. There is increased evidence that the disease aetiology is composed of various viral infections including HSV, VZV and CMV. This is the first report of concomitant infections with HSV and CMV in the corneal endothelium of a healthy patient. Concomitant infections of these two viruses in the brain and skin have been reported. There is one report on concomitant infection of CMV and HSV encephalitis in a healthy person4 and three in patients with AIDS.1
CMV is a member of the herpes family which also includes HSV 1 and 2, VZV and EBV. Herpes viruses are well known for their ability to cause unilateral chronic or recurrent anterior uveitis including corneal endotheliitis associated with elevation of IOP.4–7 This have been reported recently in immunocompetent patients.8 CMV endotheliitis is characterised by mild iritis and corneal oedema associated with coin-shaped and/or linear KPs. Koizumi et al7 thought coin-shaped KPs were a characteristic sign of CMV endotheliitis. Shiraishi et al9 also identified a group of large endothelial cells with owl’s morphology as another pathognomonic sign of CMV infections.
The diagnosis of herpetic eye disease is challenging, even though there are certain clinical features that may be useful in the diagnosis, such as the presence of linear or coin-shaped KPs in eyes with endotheliitis and the Owl's eyes lesions which are considered as characteristic of CMV infection.10 In case of chronic recurrent corneal oedema with hypertensive anterior uveitis and resisted to the treatment, more sensitive and specific test should be performed to find the aetiologies for proper management.
The traditional cultivation method is a standard technique to detect the aetiological agents of infectious keratitis. However, the isolation of the virus is time-consuming, low sensitivity and requires a special laboratory for virological processing. Nowadays, the majority of clinical laboratories have significantly reduced the use of this method. Recently, the PCR, a highly sensitive and specific method, has been used in a variety of biomedical research studies including viral detection of many ocular inflammatory diseases.11–14 There has been a changeover from a common PCR with a sensitivity of approximately 100 genomic DNAs to nested PCR methods with a sensitivity of 1–10 genomic DNAs. Nowadays, clinical laboratories proceed generally to real-time PCR methods, which have, if a correct design is used, same or even better sensitivity than the nested PCR.15 Indeed, real-time PCR has successfully been used to diagnose HSV,11 CMV retinitis16 and VZV retinitis.17
This patient suffered from an intractable disciform corneal oedema and had a poor response to systemic acyclovir and topical corticosteroid for 5 months. HSV and CMV were both positive when the real-time PCR test was done. Systemic valganciclovir was later combined with acyclovir and the patient showed a significant clinical improvement. Hence, it is important that clinicians are aware of the possibility of concomitant infection with HSV and CMV endotheliitis whenever there is treatment failure with systemic acyclovir because the two diseases share common features. Therefore additional investigations such as aqueous tapping should be conducted.18 Generally, the aqueous humour is free of any pathogens as far as the sensitivity of the custom PCR is concerned; thus a positive result obtained from the PCR is quite reliable. In this regard, the real-time PCR is a useful tool in distinguishing between the aetiological and bystander virus.
We recommend that patients with concomitant HSV and CMV anterior segment infection should receive treatment when morbidity, such as corneal oedema or glaucomatous change, develops. Oral valganciclovir, intravenous ganciclovir, topical ganciclovir and intravitreal injection of the ganciclovir have been suggested to suppress CMV endotheliitis.5 7 19 20 Chee et al recommended that the patients are initially treated with intravenous systemic ganciclovir 5 mg/kg twice daily for 6 weeks followed by oral ganciclovir 1 g three times daily for another 6 weeks. Intravenous ganciclovir can replace oral valganciclovir 900 mg twice daily for 6 weeks, followed by 450 mg twice daily for another 6 weeks as shown with this case.21
In general, patients with pure CMV endotheliitis will start to show improvement of the corneal oedema within 4–6 weeks after initiating therapy.21 But this case showed that systemic valganciclovir was insufficient to combat against HSV. Therefore we recommend adding systemic acyclovir 400 mg five times a day for 2 weeks followed by 800 mg once daily until the next follow-up PCR result is negative. For this patient, 2 weeks after oral acyclovir, the uveitis and corneal oedema became quiescent. Topical steroid was tapered off.
Antiviral treatment in combination with topical corticosteroids is generally effective in suppressing the inflammation. However, irreversible corneal endothelial dysfunction may develop in some cases. Severe pretreatment corneal oedema, older age and previous corneal graft are associated with a poor visual outcome.21 Koizumi et al7 reported two patients with CMV endotheliitis who experienced persistent bullous keratopathy because there were no or delayed ganciclovir treatment whereas Hwang et al22 reported additional four similar cases with clinical corneal remission after anti-CMV treatment. Thus it is important that patients receive accurate and prompt treatment immediately after a confirmed diagnosis to prevent deleterious results.
After treatment, patients should be reviewed at weekly intervals during the first month and every month thereafter, with more frequent reviews as necessary. Full blood count and serum creatine should be monitored every 2 weeks during the entire course of treatment. If myelosuppression or pancytopenia occurs during the use of systemic ganciclovir, the treatment should be discontinued. However, many have reported the recurrence of CMV endotheliitis after discontinuation of systemic ganciclovir. Post-treatment aqueous viral DNA PCR should be done to determine whether prophylactic dose of antiviral agents should be continued or not.
Learning points.
Herpes virus and cytomegalovirus are well known for their ability to cause unilateral chronic or recurrent anterior uveitis including corneal endotheliitis associated with elevation of IOP. Concomitant herpes simplex virus (HSV) and CMV endotheliitis can occur in immunocompetent host.
Non-HSV/varicella zoster virus corticosteroid-recalcitrant IOHS (corticosteroid-recalcitrant inflammatory ocular hypertensive syndrome) and corneal endotheliitis with specific coin-shaped keratic precipitates demonstrated by confocal microscopy may be used as a screening tool for CMV anterior segment intraocular infection.
When clinical or treatment failure for corneal endotheliitis cannot be explained by only HSV, then additional investigations such as aqueous tapping for CMV and in vivo confocal microscopy should be conducted. Aqueous humour analysis is important in distinguishing between CMV and other herpes viruses and in making a definite diagnosis for corneal endotheliitis as well as estimate the efficacy of the treatment.
Accurate and prompt treatment should be ensued immediately after a confirmed diagnosis to prevent deleterious results.
Therapy with valganciclovir for 3 months combined with oral acyclovir and topical corticosteroid may be very effective in improving concomitant infections with HSV and CMV endotheliitis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Laskin OL, Stahl-Bayliss CM, Morgello S. Concomitant herpes simplex virus type 1 and cytomegalovirus ventriculoencephalitis in acquired immunodeficiency syndrome. Arch Neurol 1987;2013:843–47 [DOI] [PubMed] [Google Scholar]
- 2.Holland EJ, Mozayeni RM, Schwartz GS. Herpes simplex keratitis. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. Vol. 2. Cornea and external disease: clinical diagnosis and management. St. Louis: Mosby, 1997:1191–223 [Google Scholar]
- 3.Liesegang TJ. Classification of herpes simplex virus keratitis and anterior uveitis. Cornea 1999;2013:127–43 [DOI] [PubMed] [Google Scholar]
- 4.Yanagisawa N, Toyokura Y, Shiraki H. Double encephalitis with herpes simplex virus and cytomegalovirus in an adult. Acta Neuropathol 1975;2013:153–64 [DOI] [PubMed] [Google Scholar]
- 5.Suzuki T, Ohashi Y. Corneal endotheliitis. Semin Ophthalmol 2008;2013:235–40 [DOI] [PubMed] [Google Scholar]
- 6.Heiligenhaus A, Helbig H, Fiedler M. Herpesviruses. In: Foster CS, Vitale AT, eds. Diagnosis and treatment of uveitis. Philadelphia: W.B. Saunders, 2002:315–32 [Google Scholar]
- 7.Koizumi N, Suzuki T, Uno T, et al. Cytomegalovirus as an etiologic factor in corneal endotheliitis. Ophthalmology 2008;2013:292–7 [DOI] [PubMed] [Google Scholar]
- 8.Chee SP, Bacsal K, Jap A, et al. Clinical features of cytomegalovirus anterior uveitis in immunocompetent patients. Am J Ophthalmol 2007;2013:834–40 [DOI] [PubMed] [Google Scholar]
- 9.Shiraishi A, Hara Y, Takahashi M, et al. Demonstration of “owl's eye” morphology by confocal microscopy in a patient with presumed cytomegalovirus corneal endotheliitis. Am J Ophthalmol 2007;2013:715–17 [DOI] [PubMed] [Google Scholar]
- 10.Chee SP, Jap A. Cytomegalovirus-associated anterior segment infection. Expert Rev Ophthalmol 2011;2013:517–28 [Google Scholar]
- 11.Fox GM, Crouse CA, Chuang EL, et al. Detection of herpes virus DNA in vitreous and aqueous specimens by the polymerase chain reaction. Arch J Ophthalmol 1991;2013:266–71 [DOI] [PubMed] [Google Scholar]
- 12.Ohashi Y, Yamamoto S, Nishida K, et al. Demonstration of herpes simplex virus DNA in idiopathic corneal endotheliopathy. Am J Ophthalmol 1991;2013:419–23 [DOI] [PubMed] [Google Scholar]
- 13.Nishi M, Hanashiro R, Mori S, et al. Polymerase chain reaction for the detection of the varicella-zoster genome in ocular samples from patients with acute retinal necrosis. Am J Ophthalmol 1992;2013:603–9 [DOI] [PubMed] [Google Scholar]
- 14.Biswas J, Mayr AJ, Martin WJ, et al. Detection of human cytomegalovirus in ocular tissue by polymerase chain reaction and in situ DNA hybridization. Graefes Arch Clin Exp Ophthalmol 1993;2013:66–70 [DOI] [PubMed] [Google Scholar]
- 15.Hlinomazová Z, Loukotová V, Horáčková M, et al. The treatment of HSV1 ocular infections using quantitative real-time PCR results. Acta Ophthalmol 2012;2013:456–60 [DOI] [PubMed] [Google Scholar]
- 16.McCann JD, Margolis TP, Wong MG, et al. A sensitive and specific polymerase chain reaction-based assay for the diagnosis of cytomegalovirus retinitis. Am J Ophthalmol 1995;2013:219–26 [DOI] [PubMed] [Google Scholar]
- 17.Short GA, Margolis TP, Kuppermann BD, et al. A polymerase chain reaction based assay for the diagnosis of varicella-zoster virus retinitis in patients with AIDS. Am J Ophthalmol 1997;2013:157–164 [DOI] [PubMed] [Google Scholar]
- 18.Kandori M, Inoue T, Takamatsu F, et al. Prevalence and features of keratitis with quantitative polymerase chain reaction positive for cytomegalovirus. Ophthalmology 2010;2013:216–22 [DOI] [PubMed] [Google Scholar]
- 19.Chee SP, Bacsal K, Jap A, et al. Corneal endotheliitis associated with evidence of cytomegalovirus infection. Ophthalmology 2007;2013:798–803 [DOI] [PubMed] [Google Scholar]
- 20.Hwang YS, Lin KK, Lee JS, et al. Intravitreal loading injection of ganciclovir with or without adjunctive oral valganciclovir for cytomegalovirus anterior uveitis. Graefes Arch Clin Exp Ophthalmol 2010;2013:263–9 [DOI] [PubMed] [Google Scholar]
- 21.Chee SP, Jap A. Treatment outcome and risk factors for visual loss in cytomegalovirus endotheliitis. Graefes Arch Clin Exp Ophthalmol 2012;2013: 383–9 [DOI] [PubMed] [Google Scholar]
- 22.Hwang YS, Shen CR, Chang SH, et al. The validity of clinical feature profiles for cytomegaloviral anterior segment infection. Graefes Arch Clin Exp Ophthalmol 2011;2013:103–10 [DOI] [PubMed] [Google Scholar]