Abstract
Human monocytic ehrlichiosis (HME) is a tick-born disease that presents predominantly as a mild to moderate acute illness. Severe life-threatening disease has been reported with a case death rate of approximately 3%, often in immunosuppressed persons. A delay in therapy initiation has been proven to increase the morbidity of the disease. We report a case of an elderly immunocompetent man with severe HME disease and multiorgan failure to emphasise on the severity of this disease in the elderly, as well as the importance of early therapy for overall favourable prognosis.
Background
Human monocytic ehrlichiosis (HME) can progress rapidly to severe multisystem disease with toxic shock-like syndrome, meningitis, or acute respiratory distress syndrome, mainly in the elderly. Early diagnosis and treatment is crucial for an overall favourable prognosis.
Case presentation
A 72-year-old man with a history of hypertension, aortic stenosis and benign prostatic hyperplasia was admitted with a 2 day history of fever, chills, headache, myalgias, diarrhoea and confusion. After admission, he had respiratory failure requiring intubation and rapid atrial fibrillation.
Investigations
Laboratory data revealed: white cell count of 5.7 (70% neutrophils, 6% bands and 20% lymphocytes), haemoglobin of 8.0, platelet count of 90, international normalised ratio of 1.2, aspartate aminotransferase 65 U/L, alanine transaminase 71 U/L, alkaline phosphatase 119 U/L, bilirubin 1.3 mg/dl, blood urea nitrogen 86 mg/dl, creatine 5.8 mg/dl. Chest x-ray, blood and urine cultures and lumbar puncture were all negative.
Differential diagnosis
The patient was started on broad spectrum antibiotics cefepime and vancomycin as well as doxycycline (starting day 1). Serologies for influenza A and B, Rickettsia typhi IgM, Rocky Mountain spotted fever, Lyme PCR, Babesia smear and Anaplasmosis PCR were negative.
Ehrlichia PCR came back positive and confirmed the diagnosis of HME. His blood smear showed the typical dispersed intracytoplasmic inclusions of HME seen in monocytes (figure 1). His acute kidney injury was attributed to acute tubular necrosis which required dialysis.
Figure 1.
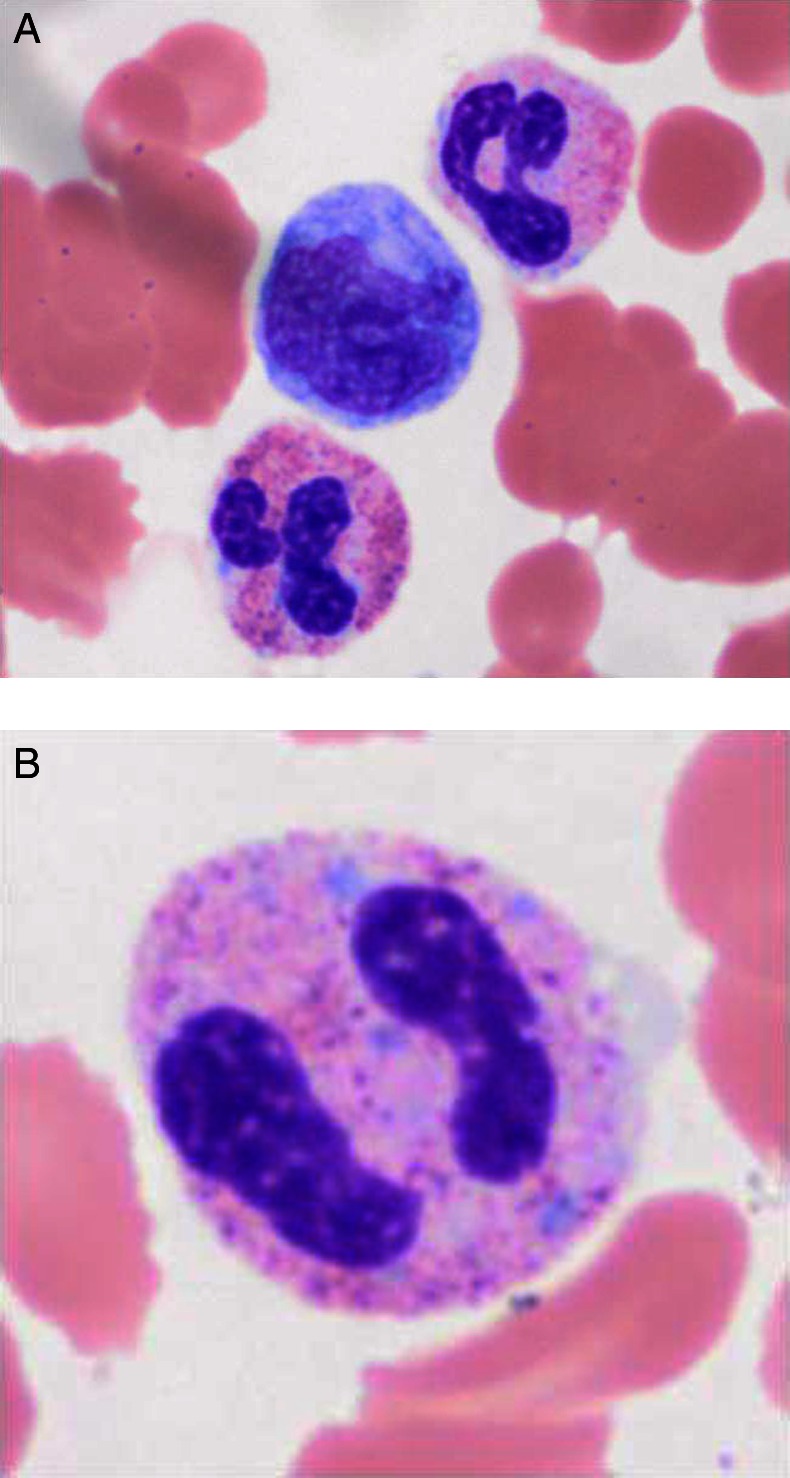
(A) Blood smear showing monocytes with intracytoplasmic inclusions (morulae), characteristic of human monocytic ehrlichiosis (HME). (B) Blood smear showing monocytes with intracytoplasmic inclusions (morulae), characteristic of HME.
Outcome and follow-up
Fever abated after 3 days; he improved gradually and was discharged home 10 days after his admission.
Discussion
The annual incidence of HME in the USA is around 0.7 cases per million population. Military studies suggested that HME can be asymptomatic in up to two-third of cases. When symptomatic, patients frequently present with fever (>95%), headache (60 –75%), myalgias (40–60%), nausea (40–50%), arthralgias (30–35%) and malaise (30–80%). Rash is reported in 30%, although it is reported frequently among adult persons infected with HIV.1
A variety of laboratory abnormalities occur in HME infection. The most common (50–90%) are leucopaenia, thrombocytopaenia and elevated plasma levels of aminotransferases, lactate dehydrogenase and alkaline phosphatase.2 HME can be diagnosed by reporting a single elevated (IgG) immunofluorescent antibody (IFA) Ehrlichia titre or demonstration of a four-fold or greater increase between acute and convalescent IFA Ehrlichia titres. A thorough peripheral smear examination can identify about 40% of infections. Intracytoplasmic inclusions (morulae) are characteristic and diagnostic. PCR has been newly used for diagnosis of HME with a very good correlation with serological results.3
In untreated patients, the disease may progress to death. The death rate cases in untreated patients were reported to be approximately 3%, and death is generally attributed to multisystem organ failure, catastrophic haemorrhage or secondary bacterial or fungal infections. Factors described to be associated with severe disease are: older patients (median age of 51) and patients debilitated by underlying disease or immunodeficiencies including HIV infection, malignancy, asplenia, chronic ethanol abuse and corticosteroid therapy.4
The diagnosis of ehrlichiosis is often delayed because of its non-specific clinical and laboratory manifestations. Early therapy is very important in the course of the disease and appropriate antibiotic treatment with doxycycline in the first 24 h of admission has proved to have a major impact on the morbidity of the disease.5
In this case scenario, doxycycline was started 24 h after the initial presentation given the unexplained fever presentation and the triad of anaemia, thrombocytopaenia and elevated transaminases. Our case highlights the importance of early clinical suspicion of HME and early empirical therapy in any patient living in an endemic area with unexplained fever, transaminase elevations and new-onset thrombocytopaenia or leucopaenia. It also emphasises that clinical manifestations in elderly hosts can be severe and can include neurological deterioration and multiorgan failure.
Learning points.
Human monocytic ehrlichiosis can progress rapidly to multiorgan failure, especially in the elderly.
Early therapy has a major impact on the morbidity of the disease.
The response to doxycycline is dramatic.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fishbein DB, Dawson JE, Robinson LE. Human ehrlichiosis in the United States, 1985 to 1990. Ann Intern Med 1994;2013:736. [DOI] [PubMed] [Google Scholar]
- 2.Dumler JS, Bakken JS. Ehrlichial diseases of humans: emerging tick-borne infections. Clin Infect Dis 1995;2013:1102. [DOI] [PubMed] [Google Scholar]
- 3.Standaert SM, Yu T, Scott MA, et al. Primary isolation of Ehrlichia chaffeensis from patients with febrile illnesses: clinical and molecular characteristics. J Infect Dis 2000;2013:1082. [DOI] [PubMed] [Google Scholar]
- 4.Paddock CD, Childs JE. Ehrlichia chaffeensis: a prototypical emerging pathogen. Clin Microbiol Rev 2003;2013:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamburg BJ, Storch GA, Micek ST, et al. The importance of early treatment with doxycycline in human ehrlichiosis. Medicine 2008;2013:53. [DOI] [PubMed] [Google Scholar]


