Abstract
A 55-year-old woman presented with features of gastric outlet obstruction not responding to conservative treatment at a peripheral hospital. She had gastric surgery 15 years before. On examination, there was a globular mass palpable in the epigastrium. Ultrasound and endoscopy findings were suggestive of retrograde jejunogastric intussusception. After initial resuscitation, emergency laparotomy was undertaken which revealed a jejunogastric intussusception at the previous retrocolic gastrojejunostomy site. After manual reduction of the intussuscepted loop by gentle traction, another segment of the jejunum was seen to be telescoping within this loop. On reduction, this jejunal loop was seen to measure around 20 cm and the apex of the intussusceptum was found to be gangrenous and perforated. Resection of the involved segment was done followed by a Roux-en-y anastomosis to restore the continuity.
Background
Retrograde jejunogastric intussusception is a rare but potentially serious complication of gastrectomy or gastrojejunostomy. Even rarer is an associated jejunojunal telescoping into this segment and it has not been reported previously to the best of our knowledge. We report an interesting case of jejunojejunal intussusception within gastrojejunal stomal herniation into the gastric lumen in a 55-year-old woman.
Case presentation
A 55-year-old woman was admitted with complaints of pain in the abdomen and vomiting since 3 days. Fifteen years earlier, she had undergone surgery for acid peptic disease, the details of which were not known. On physical examination, the patient was dehydrated with a pulse rate of 120/min and a blood pressure of 100/70 mm Hg. An upper midline abdominal scar of a previous laparotomy was seen. A tender ill-defined lump was palpable in the epigastric region with signs of localised peritonitis. It was mobile from side to side and moved with respiration. Ryle's tube aspiration revealed a coffee-ground aspirate. By correlating the history and examination findings, a provisional diagnosis of gastric outlet obstruction probably due to retrograde intussusception was made. Accordingly, she was sent for an ultrasound abdomen and upper gastrointestinal (GI) endoscopy.
Investigations
Laboratory investigations showed haemoglobin 8 g%, white cell count 18 500 with 80% polymorphs and 20% lymphocytes.
Ultrasound showed jejunojejunal intussusception with? gastrojejunal stomal herniation into the gastric lumen.
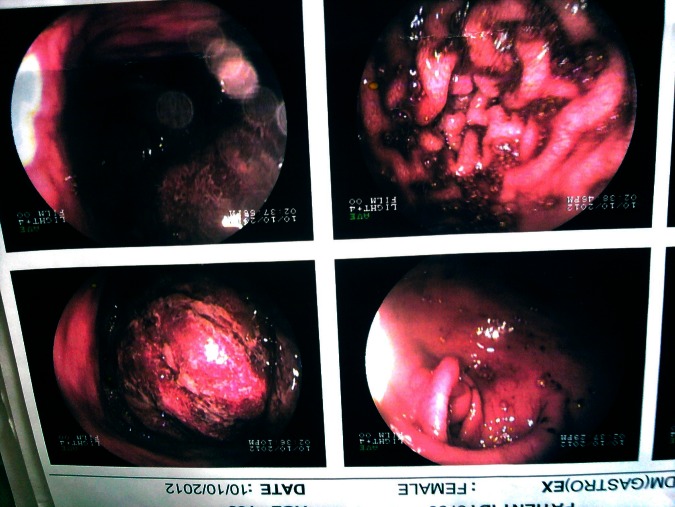
Upper GI endoscopy revealed jejunogastric intussusception with gangrene (figure 1).
Figure 1.
Close view of the endoscopic picture showing the intussusceptum (top right). Gastric mucosa with altered blood is seen below.
Treatment
After initial resuscitation, emergency laparotomy was undertaken using a midline incision which revealed a mass palpable within the stomach with evidence of a posterior gastrojejunostomy. On further exploration, a retrograde jejunogastric intussusception (efferent loop in the stomach) was found. After manual reduction of the intussuscepted loop by gentle traction, to our surprise we noticed that this loop was harbouring another segment of an efferent loop of the jejunum which was telescoping inside it (figures 2 and 3). On slowly reducing this jejunal loop, it was seen to measure around 20 cm and the apex of the intussusceptum was found to be gangrenous and perforated (figure 4 and 5). Resection of the gangrenous segment with Roux-en-Y anastomosis was done.
Figure 2.

Reduced jejunal loop showing telescoping of the efferent loop of the jejunum within it.
Figure 3.

Intussuscepted loop of the distal jejunum seen telescoping within the oedematous proximal jejunum which was herniating through the gastrojejunostomy site and was reduced. Note that the transverse colon is lifted up to have a better view.
Figure 4.
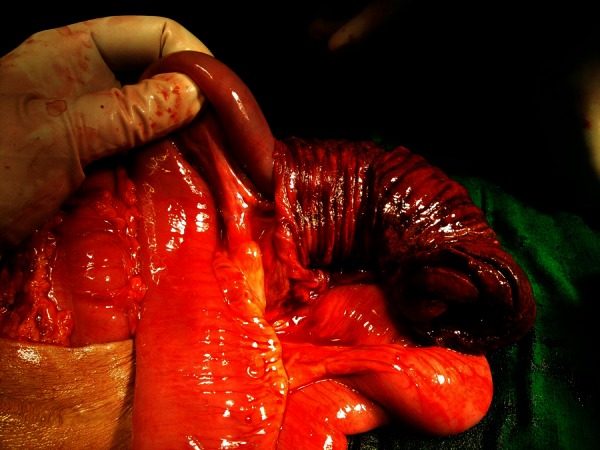
Efferent loop of the jejunum being reduced.
Figure 5.

After reduction, the efferent loop of the jejunum is found to be gangrenous and perforated.
Outcome and follow-up
The postoperative period was uneventful. The patient was discharged on the 11th postoperative day. There was no anastomotic leak or wound infection. She presented to us again with features of subacute intestinal obstruction 1 month postsurgery and was relieved by conservative management.
The patient reported for review a month later and was doing well.
Discussion
Retrograde jejunogastric intussusception is a rare acute abdominal condition where the small bowel loops get incarcerated and strangulated inside the stomach. It is a rare complication after gastric surgery1 (<0.1% incidence) with around 200 cases reported in the world literature2 since the first case of jejunogastric intussusception after gastrojejunostomy was reported by Bozzi3 in 1914.
Three anatomical types of jejunogastric intussusception have been described by Shackman4: type I concerns the afferent loop (ANTEGRADE), type II concerns the efferent loop (RETROGRADE), type III represents a combined form.
It has been stated that type II or retrograde efferent loop intussusception is the most common (80%) with the two other types accounting for 10% each.5
However, ours was a unique case and could not be categorised as per the above classification.
Another classification by Brynitz and Rubinstein (1986)6 classified jejunogastric intussusceptions in greater detail into five types as follows:
Type 1: with afferent loop intussusception (5.5%)
Type 2a: with efferent loop intussusceptions (70%)
Type 2b: with efferent-efferent loop intussusceptions (6.5%)
Type 3: a combination of type 1 and type 2 (10%)
Type 4: with an intussusception through a Braun's side-to-side jejuno-junal anastomosis (8%)
As per this classification, our case can be classified as category 2b, which has an incidence of 6.5% of all the retrograde intussusceptions, but we could not find any similar case in the literature even after an extensive search.
The cause(s) of jejunogastric intussusception is (are) poorly understood.7 Various factors have been incriminated such as hyperacidity, long afferent loop, jejunal spasm with abnormal motility, increased intra-abdominal pressure, retrograde peristalsis, etc. Probably, retrograde peristalsis, which can occur in normal people prior to gastric surgery, seems to be accepted as the cause of type II jejunogastric intussusception by most authors.7 8
If not suspected, the clinical picture can be quite non-specific and the possibility of intussusception may not even be considered. The dominant symptom is pain, occasionally associated with nausea and vomiting. Patients may present with high intestinal obstruction or severe haematemesis from secondary ulceration.9 A firm mass may be palpable in the epigastrium. A water-soluble upper GI contrast study may reveal a ‘coiled-spring’ appearance within the stomach. Upper GI endoscopic examination is often diagnostic and may visualise the jejunal segments as they migrate in and out of the stomach.
Treatment of jejunogastric intussusception consists mainly of surgery using several approaches depending on the intraoperative findings7: (a) manual reduction of the intussusception, (b) revision of the anastomosis, (c) anchoring of the efferent limb to the parietal peritoneum or suturing together of the efferent and afferent limbs after reduction of intussusception and (d) a new gastrojejunostomy, ideally using a Roux-en-Y reconstruction can be fashioned.10 (e) If the intussusception is gangrenous, resection and revision of anastomosis provides the correct treatment.11
Endoscopic reduction of the jejunogastric intussusceptions has been suggested in a few selected cases12; however, this is associated with a significant risk of recurrence.13
Treatment should be initiated early as the reported death rate ranges from 10% for treatment within the first 48 h to 50% with a 96 h delay.14
Learning points.
Presence of a mobile epigastric mass in association with pain and vomiting in a patient who has had a previous gastric surgery is considered virtually pathognomic of acute retrograde intussusception.
Most of the reported cases have not been diagnosed preoperatively; this requires high index of suspicion.
Upper GI endoscopic examination is often diagnostic.
The treatment of acute jejunogastric intussusception is prompt surgery.
The abdomen is a magic box, always full of surprises, as we had one here!!
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Conklin EF, Markowitz AM. Intussusception, a complication of gastric surgery. Surgery 1965;2013:480–8 [PubMed] [Google Scholar]
- 2.Kim KH, Jang MK, Kim HS, et al. Intussusception after gastric surgery. Endoscopy 2005;2013:1237–43 [DOI] [PubMed] [Google Scholar]
- 3.Bozzi E. Annotation. Bull Acad Med 1914;2013:3–4 [Google Scholar]
- 4.Shackman R. Jejunogastric intussusception. Br J Surg 1940;2013:475–80 [Google Scholar]
- 5.Reyelt WP, Jr, Anderson AA. Retrograde jejunogastric intussusception. Surg Gynecol Obstet 1964;2013:1305–11 [PubMed] [Google Scholar]
- 6.Brynitz S, Rubinstein E. Hematemesis caused by jejunogastric intussusceptions. Endoscopy, 1986;2013:162–4 [DOI] [PubMed] [Google Scholar]
- 7.Waits JO, Beart RW, Jr, Charboneau JW. Jejunogastric intussusception. Arch Surg 1980;2013:1449–52 [DOI] [PubMed] [Google Scholar]
- 8.Irons HS, Lipin RJ. Jejuno-gastric intussusception following gastroenterostomy and vagotomy. Ann Surg 1955;2013:541–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menezes LT, D'Cruz A. Retrograde jejunogastric intussusception following gastric surgery. J Indian Med Assoc 1986;2013:310–1 [PubMed] [Google Scholar]
- 10.Soybel DI, Zinner MJ. Complications following gastric operation. In: Zinner MJ, ed. Maingot's abdominal operations. 10th edn. Connecticut: Appleton & Lange, 1997:1046 [Google Scholar]
- 11.Archimandritis AJ, Hatzopoulos N, Hatzinikolaou P, et al. Jejunogastric intussusception presented with haematemesis: a case presentation and review of the literature. BMC Gastroenterol 2001;2013:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kochhar R, Saxena R, Nagi B, et al. Endoscopic management of retrograde jejunogastric intussusception. Gastrointest Endosc 1988;2013:56–7 [DOI] [PubMed] [Google Scholar]
- 13.Guadagni S, Pistoia M, Catarci M, et al. Retrograde jejunogastric intussusception: is endoscopic or surgical management more appropriate? Surg Today 1992;2013:269–72 [DOI] [PubMed] [Google Scholar]
- 14.Walstad P, Ritter J, Arroz V. Delayed jejunogastric intussusception after gastric surgery: an ever-present threat. Am Surg 1972;2013:172–75 [PubMed] [Google Scholar]