Abstract
One of the rare side effects of chronic usage of non-steroidal anti-inflammatory drugs is colopathy, which is characterised by colonic inflammation, ulceration and formation of diaphragms in late stages. We treated a case of colonic diaphragm disease with similar findings in our unit recently. We present the case herewith, followed by a discussion of the management of this interesting rare but benign condition.
Background
With increasing use of slow release non-steroidal anti-inflammatory drugs (NSAIDs), the incidence of colonic diaphragms is on the rise. Recognition of this benign condition would aid in timely and satisfactory management of this group of patients. We wrote this article to share our experience with all medical professionals dealing with gastrointestinal (GI) pathologies.
Case presentation
A 63-year-old female patient presented to the hospital physicians with incidental finding of anaemia (haemoglobin 8.5 g/dl). She had morbid obesity with a body mass index of 50, and multiple comorbidities for which she was on extensive medication. These include diclofenac sodium which she has been taking for many years for symptomatic relief from osteoarthritis of knees. In recent times, she had switched onto a modified release preparation 150 mg/day and did not experience any overt side effects from this.
Investigations
She had oesophago-gastro-duodenoscopy that showed mild erosive prepyloric gastritis. Colonoscopy showed a non-passable stricture at hepatic flexure of colon with fibrotic edges and normal looking mucosa. There was no macroscopic appearance of a neoplastic process (figure 1). Few sigmoid diverticulae also were detected. Multiple biopsies were obtained from the stricture and this area was tattooed. A repeat colonoscopy showed similar findings. Histology showed area of ulceration covered by granulation tissue with active chronic organising inflammation. A panel of immunoperoxidase stains has confirmed these cells to be of epithelial in nature. These pathological changes were of non-specific in nature and were felt could be related to a variety of conditions including inflammation, ischaemia or diverticulitis.
Figure 1.
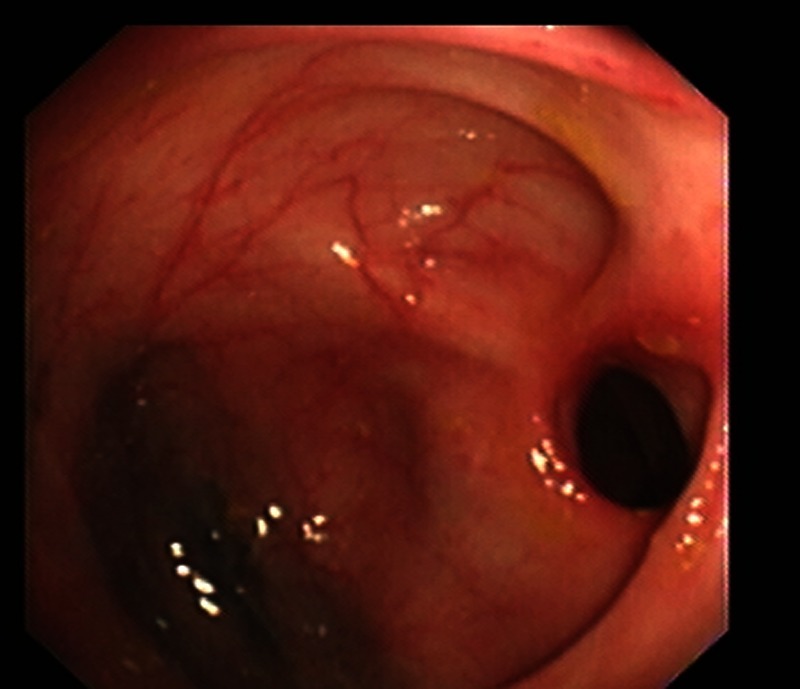
Endoscopic appearance of the diaphragm (case 1).
CT scan of her abdomen and chest demonstrated a 4 cm long stricture of her hepatic flexure, with some subcentimetre mesenteric lymph nodes and distension of ascending colon. No evidence of any metastatic disease was discovered (figure 2). She underwent CT colonogram which showed persistent abnormal wall thickening at the hepatic flexure suspicious of malignancy (figure 3).
Figure 2.
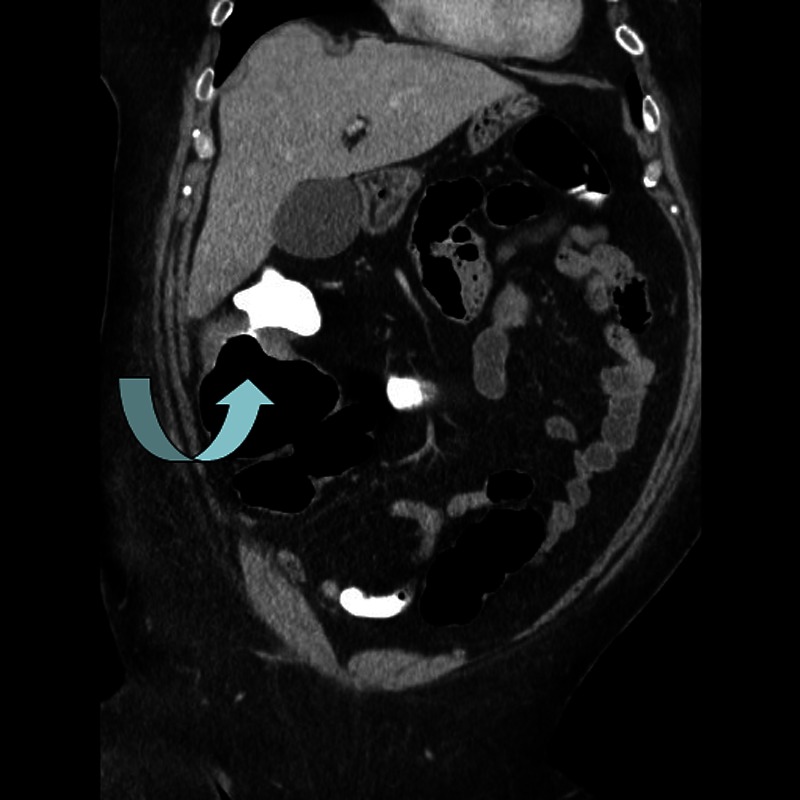
CT scan image of the diaphragm.
Figure 3.
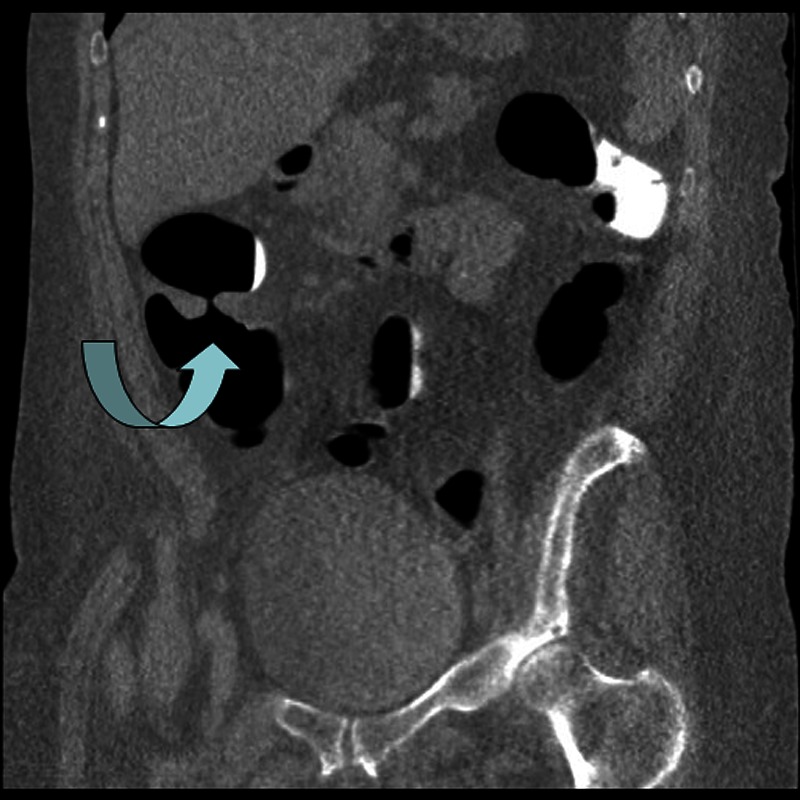
Reconstructed image of the diaphragm on CT colonogram.
Differential diagnosis
Malignancy, inflammatory bowel disease.
Treatment
Her case was discussed in our multidisciplinary team meeting. In view of the indeterminate nature of the lesion and with evidence of impending bowel obstruction as demonstrated by distended ascending colon, she has been offered a laparoscopic right hemicolectomy which she underwent successfully. She had uneventful postoperative recovery in high-dependence unit followed by on the ward. She was discharged on fourth postoperative day.
The resected stricture demonstrated a ‘diaphragm’ with a central narrow aperture (figure 4). On histological analysis, the diaphragm was shown to be formed by fibrosis of the submucosa, possibly as a reparative response to previous ulceration. This was supported by the presence of ulceration of the surrounding bowel surface, along with surface granulation tissue and fibrosis of the lamina propria (figure 5).
Figure 4.
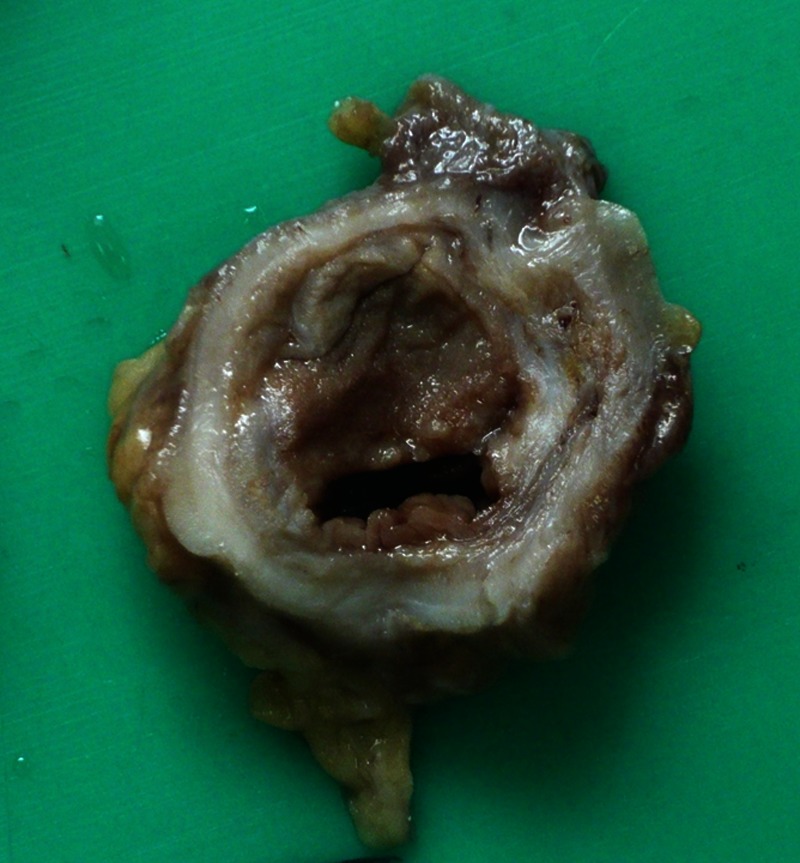
Cross-section of operative specimen showing diaphragm.
Figure 5.
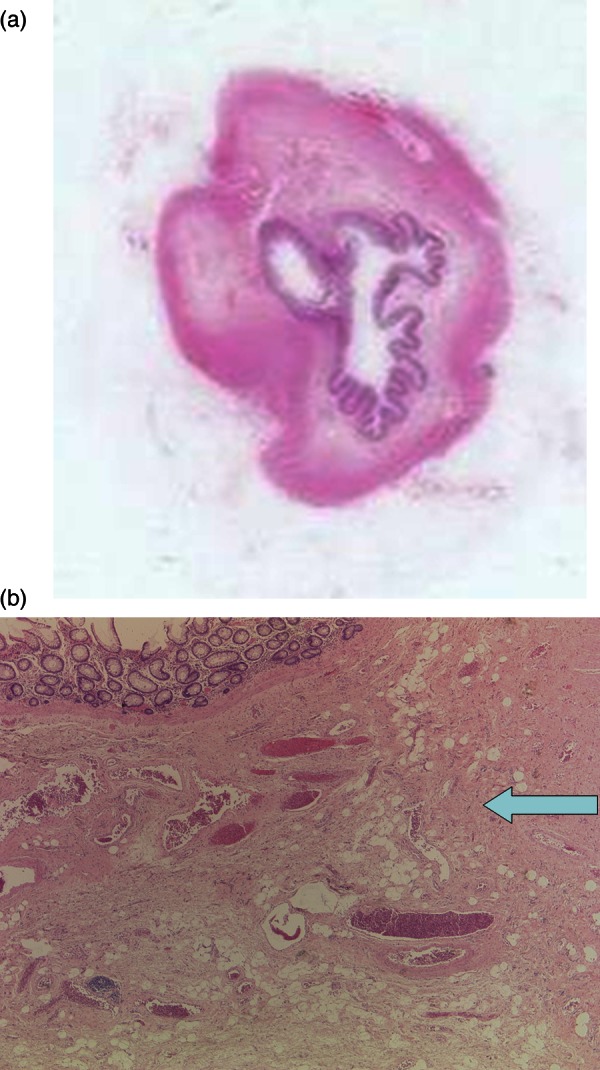
Histology of the diaphragm—H&E stain: (A) macroscopic (×1.5); (B) microscopic (×50)—arrow points to submucosal fibrosis.
Outcome and follow-up
She is symptom free in the follow-up period of 9 months.
Discussion
Slow release NSAIDs are a common form of medication prescribed for musculo-skeletal conditions. While the other GI side effects of these preparations are well known,1 diaphragm disease resulting from colopathy was first described in 1988.2 So far only 45 such cases were reported in English literature. The active ingredients of the NSAIDs are believed to be causing local effects in the distal small bowel and proximal large bowel, manifested as ulceration and ‘healing by fibrosis’ resulting in diaphragm formation. Systemic role of NSAIDs is also implicated in the pathogenesis of this condition.
The symptoms of colonic diaphragms are generally insidious and could be variable. These include abdominal pain, bleeding, obstruction, diarrhoea, anaemia, etc. History of patient's medication along with macroscopically benign looking proximally located diaphragms could alert the physicians/surgeons to the possibility of NSAID-induced disease. Colonoscopic biopsies aided by imaging would be the diagnostic modalities of choice. The differential diagnosis would include colitis of various aetiology (infectious, inflammatory or ischaemic) or neoplasms. The histological characteristic feature of the diaphragms is submucosal fibrosis as observed in our case, with associated inflammatory infiltrate and usually normal mucosa.
Discontinuation of NSAIDs alone has been observed to be effective in resolving the inflammation underlying the colopathy; however, diaphragm disease itself is not reversed by this treatment strategy.3 Surgical resection of the affected segment of colon4 or endoscopic/fluoroscopic dilation of the diaphragms5 is the only option that provides satisfactory treatment of this condition. In those patients treated by conservative means, follow-up is important for timely identification and treatment of the recurrent disease.
Learning points.
We believe awareness of this increasingly common condition is essential among the gastrointestinal surgeons and physicians.
Meticulous history taking and appropriate investigations in the form of colonoscopy would aid in identification of this condition.
Treatment depends on the extent and severity of the colonic diaphragms.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bjarnason DN, Macpherson AJ. Intestinal toxicity of non-steroidal anti-inflammatory drugs. Pharmacol Ther 1994;2013:145–57 [DOI] [PubMed] [Google Scholar]
- 2.Lang J, Price AB, Levi AJ, et al. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol 1988;2013:516–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hakeem A, Subramonia S, Badrinath K, et al. NSAID-induced diaphragm-like colonic strictures: a case report. BMJ Case Rep 2009. doi:10.1136/bcr.02.2009.1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gargot D, Chaussade S, d'Alteroche L, et al. Nonsteroidal anti-inflammatory drug-induced colonic strictures: two cases and literature review. Am J Gastroenterol 1995;2013:2035–8 [PubMed] [Google Scholar]
- 5.Smith JA, Pineau B. Endoscopic therapy of NSAID-induced colonic diaphragm disease: two cases and a review of published reports. Gastrointest Endosc 2000;2013:120–5 [DOI] [PubMed] [Google Scholar]


