Abstract
Rheumatoid arthritis (RA) is a multisystem inflammatory disease characterised by destructive synovitis and varied extra-articular involvement. Rheumatoid lung nodules are the most common pulmonary manifestations of RA. Rheumatoid nodules in mediastinal lymph nodes are extremely uncommon. We describe a male patient with long-standing RA and subcutaneous rheumatoid nodules presenting with multiple lung nodules and mediastinal lymphadenopathies. Definite histopathology of a lymph node was consistent with necrobiotic granuloma due to RA. Clinicians should be aware of rheumatoid nodules as a potential cause of mediastinal lymphadenopathies, mainly in advanced rheumatoid arthritis.
Background
Rheumatoid arthritis (RA) is a systemic inflammatory disease with varied extra-articular manifestations. The most frequent extra-articular organ involvement is the subcutaneous rheumatoid nodule1; however, rheumatoid nodules also occur in the lung, heart and upper airway.2 Rheumatoid nodules are more common in men than in women and are closely associated with rheumatoid factor seropositivity.2 In this paper, we describe the rare occurrence of rheumatoid nodules in mediastinal lymph nodes.
Case presentation
A 72-year-old Caucasian man presented with complaints of bright red blood per rectum over the course of 2 days and 40 pounds unintentional weight loss over the last several months. He had seropositive deforming RA diagnosed 20 years ago, currently on a tumor necrosis factor-α inhibitor (adalimumab) and low-dose prednisone. His other medical problems included subcutaneous rheumatoid nodules, iron deficiency anaemia, hypertension and hyperlipidaemia. He worked at International Harvester for many years. He smoked for 10 years from the age of 13 to 23. In the last 5 years he started smoking two packs per day. He denied recent travels or unusual exposures.
On examination his vital signs were stable and his oxygen saturation was 95% on room air. He appeared tired but not in any distress. Lungs were clear bilaterally. He had swann-neck deformities of his fingers, without active synovitis. Skin examination showed multiple subcutaneous skin nodules over the second and third metacarpophalangeal joints and bilateral elbows.
Investigations
He underwent a colonoscopy which showed a colonic polyp that was excised. As part of the malignancy work-up, a CT scan of the chest showed multiple mediastinal adenopathies and lung nodules. The adenopathies measured between 1.1 and 6.5 cm, and were distributed in the superior pretrachea, subhilum and subcarina; the largest nodal mass was subcarinal and measured 6.5×2.5 cm (figure 1). The lung nodules measured between 0.2 and 0.9 cm, and were located throughout the lungs. Many of these nodules had cavitations within them. Some of these nodular entities were seen endobronchially. The prominent entity was seen in the left lower lobe, was relatively thin-walled, cavitary and immediately subpleural (figure 2).
Figure 1.

Subcarinal adenopathy on CT scan.
Figure 2.

CT of the chest showing a lung nodule in the left lower lobe, cavitary and immediately subpleural.
Differential diagnosis
Patient had a bronhoscopy with bronchoalveolar lavage (BAL) that was negative for opportunistic infections such as tuberculosis and fungal infections and negative for malignant cells. His quantiferon test was negative. He had a biopsy of the subcarinal node measuring 6.5×2.5 cm via endoscopic ultrasound. The node biopsy showed central fibrinoid necrosis with surrounding palisading histiocytes and an outer layer of inflammatory cells and granulomatous inflammation consisting with a necrobiotic granuloma (figure 3). The stains for mycobacteria and fungi did not reveal organisms and acid-fast bacilli culture was negative. The histological appearance was not suggestive of metastatic carcinoma, lymphoma or sarcoidal granulomas, but was most suggestive of necrobiotic granuloma due to RA.
Figure 3.
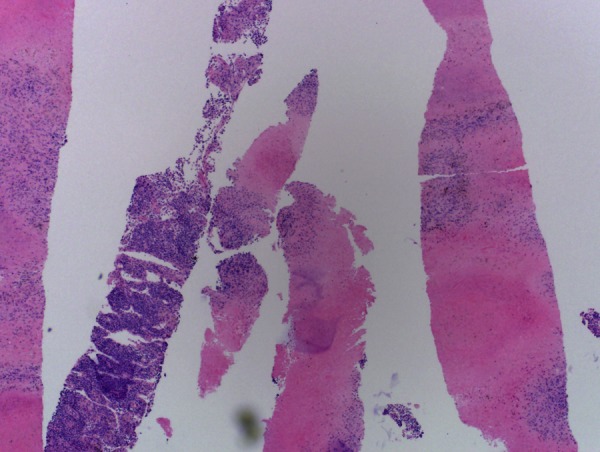
Photomicrograph showing a necrobiotic granuloma.
Treatment
Patient was discharged home on the same medications with instructions to schedule a follow-up CT chest within 6 weeks.
Outcome and follow-up
Patient was discharged home on the same medications with instructions to schedule a follow-up CT chest within 6 weeks.
Discussion
Rheumatoid nodules, also called necrobiotic nodules, are common in patients with RA. Most nodules are clinically asymptomatic; however, subcutaneous nodules on pressure points or adherent to periosteum or tendons may become painful. Nodules typically occur in patients with long-standing disease, but their time of onset varies and may even precede the diagnosis of RA.2 On pathological examination, the nodules consist of a central area of irregular fibrinoid necrosis surrounded by palisading mononuclear cells, with a peripheral area of chronic inflammatory cells and granulation tissue; the so-called necrobiotic granuloma.2 The exact same histopathology is found in certain cutaneous diseases such as necrobiosis lipoidica and the subcutaneous variant of granuloma annulare.3 These granulomas are different than sarcoidal granulomas which lack the central area of necrosis.4 The pathogenesis of rheumatoid nodules is incompletely understood, but the inciting events are thought to include repetitive trauma or immune complex deposition, leading to focal vasculitis, complement activation and cytokine release by local monocytes. Proteinases, collagenases and macrophage chemotactic factors contribute to the central necrosis and surrounding array of macrophages. Complex immunological processes including both B and T lymphocytes contribute to further inflammation.2
RA has varied pleuroparenchymal manifestations, which includes organising pneumonia, interstitial fibrosis, rheumatoid nodules, airway disorders such as bronchiectasis and pulmonary vasculitis.5 Rheumatoid lung nodules are more common in men than in women and are usually asymptomatic. They are detected on chest radiograph in about 0.2% of unselected patients with RA and more frequently on high resolution CT scan (4%).6 The clinical course of pulmonary nodules is variable. The nodules may precede the clinical manifestation of RA or be concurrent. They may increase in size, resolve spontaneously or appear at new sites as older nodules resolve.6 They usually present more of a diagnostic than a therapeutic challenge, particularly when they precede the articular disease.6 7 In the lung, multiple nodules are usually present, although solitary nodules are also found. The nodules tend to be subpleural or septal and peripheral, although they may appear on the pleural surface. Their size varies from less than 1 cm and up to 7 cm in diameter. Cavitation may occur and occasionally leads to haemoptysis. Due to their typical subpleural distribution, complications can include pneumothorax, empyema, pleural effusions and bronchopleural fistulas.2 8 9 Rheumatoid nodules usually require no treatment unless they become quite large, infected or cavitate with bronchopleural fistulas.8 Rituximab, tocilizumab and other immunosuppressives have been used with variable results.1 10
The differential diagnosis of lung nodules with mediastinal lymph nodes would include infections such as tuberculosis and fungual, sarcoidosis, septic emboli such as endocarditis, malignancies including lymphoma or metastatic cancer, lymphomatoid granulomatosis, vasculitides such as granulomatosis with polyangiitis, amyloidosis, drug reactions and rheumatoid nodules.2 8 11 Therefore, histopathological confirmation is usually necessary. The histological hallmark of sarcoidosis is a non-caseating granuloma with giant cells, epithelioid cells and some lymphocytes without a central area of necrosis. The finding of a necrobiotic granuloma in the lymph node biospy specimen in our patient made sarcoidosis less likely. The negative culture for tuberculosis and negative stains for malignancies indicated a rheumatoid nodule. Mediastinal lymphadenopathy is a common finding at autopsy in systemic lupus erythematosus and rheumatoid arthritis, but has seldom been mentioned in reports of rheumatic diseases except in Sjogren's syndrome.12 Rheumatoid nodules in mediastinal lymph nodes are extremely uncommon; however, they are nowadays more recognised thanks to the emergency of new technologies with better sampling such as endobronchial ultrasound-guided transbronchial needle aspiration and endoscopic ultrasound.13 Clinicians should be aware of rheumatoid nodules as a potential cause of mediastinal lymphadenopathies, mainly in advanced long-standing RA.
Learning points.
The histological hallmark of a rheumatoid nodule is a necrobiotic granuloma.
Necrobiotic granulomas are different than sarcoidal granulomas which lack the central area of necrosis.
The differential diagnosis of lung nodules with mediastinal lymph nodes in a patient on tumor necrosis factor-α inhibitor should include tuberculosis.
Acid-fast bacilli culture on the biospy specimen is the most sensitive test to rule out tuberculosis.
Clinicians should be aware of rheumatoid nodules as a potential cause of mediastinal lymphadenopathies, mainly in advanced long-standing rheumatoid arthritis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Turesson C. Extra-articular rheumatoid arthritis. Curr Opin Rheumatol 2013;2013:360–6 [DOI] [PubMed] [Google Scholar]
- 2.Antin-Ozerkis D, Evans J, Rubinowitz A, et al. Pulmonary manifestations of rheumatoid arthritis. Clin Chest Med 2010;2013:451–78 [DOI] [PubMed] [Google Scholar]
- 3.Magro CM, Crowson AN, Regauer S. Granuloma annulare and necrobiosis lipoidica tissue reactions as a manifestation of systemic disease. Hum Pathol 1996;2013:50–6 [DOI] [PubMed] [Google Scholar]
- 4.Gal AA, Koss MN. The pathology of sarcoidosis. Curr Opin Pulm Med 2002;2013:445–51 [DOI] [PubMed] [Google Scholar]
- 5.Schneider F, Gruden J, Tazelaar HD, et al. Pleuropulmonary pathology in patients with rheumatic disease. Arch Pathol Lab Med 2012;2013:1242–52 [DOI] [PubMed] [Google Scholar]
- 6.Nannini C, Ryu JH, Matteson EL. Lung disease in rheumatoid arthritis. Curr Opin Rheumatol 2008;2013:340–6 [DOI] [PubMed] [Google Scholar]
- 7.Perez T, Dansin E, Wallaert B, et al. Pleuro-pulmonary manifestations of rheumatoid polyarthritis. Rev Mal Respir 1991;2013:169–89 [PubMed] [Google Scholar]
- 8.Patel R, Naik S, Amchentsev A, et al. A rare cause of multiple cavitary nodules. Chest 2009;2013:306–9 [DOI] [PubMed] [Google Scholar]
- 9.Jolles H, Moseley PL, Peterson MW. Nodular pulmonary opacities in patients with rheumatoid arthritis. A diagnostic dilemma. Chest 1989;2013:1022–5 [DOI] [PubMed] [Google Scholar]
- 10.Orme ME, Macgilchrist KS, Mitchell S, et al. Systematic review and network meta-analysis of combination and monotherapy treatments in disease-modifying antirheumatic drug-experienced patients with rheumatoid arthritis: analysis of American College of Rheumatology criteria scores 20, 50, and 70. Biologics 2012;2013:429–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karadag F, Polatli M, Senturk T, et al. Cavitary necrobiotic nodule imitating malignant lung disease in a patient without articular manifestations of rheumatoid arthritis. J Clin Rheumatol 2003;2013:246–52 [DOI] [PubMed] [Google Scholar]
- 12.Gordonson J, Quinn M, Kaufman R, et al. Mediastinal lymphadenopathy and undifferentiated connective tissue disease: case report and review. AJR Am J Roentgenol 1978;2013:325–8 [DOI] [PubMed] [Google Scholar]
- 13.Nakajima T, Yasufuku K, Yoshino I. Current status and perspective of EBUS-TBNA. Gen Thorac Cardiovasc Surg. Published Online First: 26 Feb 2013. doi:10.1007/s11748-013-0224-6 [DOI] [PubMed] [Google Scholar]


