Description
A 32-year-old woman with idiopathic congenital moderate mental retardation was being followed because of presumed primary central nervous system lymphoma (previous clinical evolution and investigation summarised in table 1)
Table 1.
Previous clinical evolution and investigation
| Year | Clinical and imagiological findings | Investigation | Treatment/evolution | Presumed diagnosis |
|---|---|---|---|---|
| 2000 | Somnolence, progressive right-sided hemiparesis brain magnetic resonance: left-sided hypointense on T2-weighted with homogeneous gadolinium-enhancing lenticulo-thalamo-capsular lesion (tumour? inflammatory?) | Negative extensive blood* and CSF** testing; normal EEG; biopsy postponed : deep location of the lesions, disappearance with corticotherapy | Corticotherapy/clinical and radiological remission | Primary CNS*** vasculitis? Primary CNS lymphoma? |
| 2000(3 weeks later) | Right-sided central facial paresis, spastic paretic gait resurgence of prior lesion brain magnetic resonance | Negative extensive blood and CSF testing; normal EEG; HLA typing: A24; B07, DRB1 11:04, 11:07; DQB1 03:01, 03:03 | Corticotherapy/partial clinical and radiological remission | Primary CNS vasculitis? |
| 2011 | Headache, confusional state, residual right crural paresis brain magnetic resonance: multiple nodular hypointense on T2-weighted with homogeneous T1 gadolinium-enhancing supratentorial lesions | Inconclusive biopsy (encephalitis? lymphoma?): presence of reactive astrocytes and microgliosis, perivascular mononuclear infiltrates; atypical T and B lymphocytes on immunohistochemical staining—negative extensive blood and CSF investigation; normal EEG | Corticotherapy/clinical and radiological remission | Primary CNS lymphoma? |
| 2013 | Tetraparesis, worsening of the pre-existing cognitive impairment brain magnetic resonance: hypointense on T2-weighted a with T1 gadolinium-enhancing lesions in the dorsal midbrain tegmentum and periaqueductal area | Negative extensive blood and CSF testing; normal EEG | Corticotherapy | Primary CNS lymphoma? |
*antineutrophilic cytoplasmic antibodies, antinuclear antibody, antiphospholipid antibodies, C-reactive protein, haemosedimentation rate, renal function, hepatic function, electrolites, lactate, pyruvate, arylsulfatase A, thyroid function, adrenal function, HIV, hepatitis B and C virus. **neurotropic virus, John Cunningham virus, immunophenotyping. ***Central nervous system.
CSF, cerebrospinal fluid; CNS, central nervous system; HLA, human leucocyte antigen.
She was admitted for clinical re-evaluation because of motor and cognitive deterioration. She was bedridden, tetraparetic, with severe cognitive impairment preventing any verbal communication, apart from elementary responses. During the first week of hospitalisation she developed persistent elementary vocal tics and swallowing disturbance, often showing facial signs of discomfort. Oropharyngeal examination revealed the presence of continuous rhythmic movement of the soft palate typical of palatal tremor (video 1) which was also present during sleep. No repetitive audible clicks were noticed. Brain magnetic resonance disclosed the presence of lesions involving the dorsal midbrain tegmentum and periaqueductal area without hypertrophy of the inferior olive (figures 1 and 2). Baclofen was introduced with slight symptomatic relief. Palatal tremor, also called palatal myoclonus, is a rare movement disorder characterised by brief, rhythmic involuntary movements of the soft palate. It is presumably caused by dysfunction (essential palatal tremor) or a lesion (symptomatic palatal tremor), involving the Guillain-Mollaret triangle also known as ‘myoclonic triangle’ (dentate nucleus, red nucleus, inferior olivary nucleus and central tegmental tract). Brainstem or cerebellar disorders such as stroke, demyelinating diseases, trauma and tumours are often identified.1There is no established treatment for palatal tremor. Palatal botulinum toxin injections, and other drugs such as clonazepam, flunarizine, baclofen or sumatriptan are used, but these interventions are often unsuccessful.2 3
Figure 1.
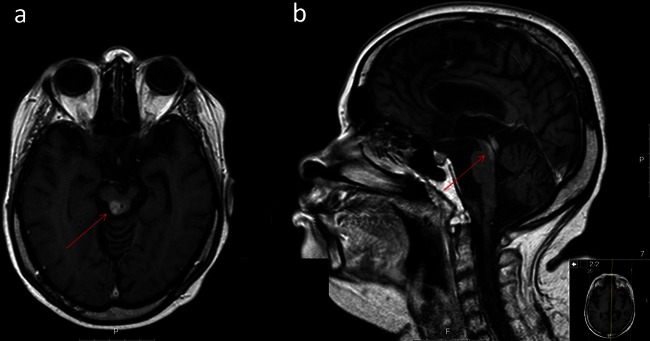
Brain MRI showing lesions involving the dorsal midbrain tegmentum and periaqueductal area in axial fluid-attenuated inversion recovery (A) and sagital T1 with gadolinium (B) weighted images.
Figure 2.

Lesion within Guillain Mollaret triangle (yellow triangle) on coronal T1 with gadolinum.
Continuous rhythmic movement of the soft palate.
Learning points.
Palatal tremor is a rare movement disorder; when symptomatic (secondary) is usually described in association with lesions involving the Guillain-Mollaret triangle.
Brain magnetic resonance is mandatory to identify an underlying lesion, particularly in cases of central nervous system tumours.
Footnotes
Contributors: HN designed the study. JM wrote the manuscript; AA collected the data and drafted the manuscript; DS wrote and revised the manuscript. All authors read and approved the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Deuschl G, Mischke G, Schenck E, et al. Symptomatic and essential rhythmic palatal myoclonus. Brain 1990;2013:1645–72 [DOI] [PubMed] [Google Scholar]
- 2.Penney SE, Bruce IA, Saeed SR. Botulinum toxin is effective and safe for palatal tremor: a report of five cases and a review of the literature. J Neurol 2006;2013:857–60 [DOI] [PubMed] [Google Scholar]
- 3.Campistol-Plana J, Majumdar A, Fernández-Alvarez E. Palatal tremor in childhood: clinical and therapeutic considerations. Dev Med Child Neurol 2006;2013:982–4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Continuous rhythmic movement of the soft palate.


