Abstract
A 27-year-old woman presented to her primary care doctor's office with left flank pain. CT of the abdomen showed an isolated left renal vein thrombus. The clot was initially attributed to her oral contraceptive use; however, closer inspection of CT images revealed nutcracker phenomenon (compression of the renal vein between the superior mesenteric artery and abdominal aorta). Intravascular ultrasound imaging confirmed the diagnosis. Nutcracker syndrome is a rare condition, which if left untreated may cause damage to the left kidney. Although under diagnosed, there are several treatment options available ranging from simple surveillance to surgical resolution.
Background
The case describes an under-reported disorder, nutcracker syndrome (NCS), which presents with non-specific symptoms and predisposes patients to developing renal vein thrombosis. Such patients have a higher likelihood of being misdiagnosed owing to low levels of awareness among providers about the condition.
Case presentation
A 27-year-old woman presented to her primary care physician's (PCP) office with constant, left flank pain for 5 days, which she attributed to a muscle strain. She denied prior such episodes and reported no known medical history other than anxiety for which she was taking citalopram and alprazolam. Her PCP ordered an abdominal CT to look for renal stones. CT (figure 1) however showed left renal vein thrombosis. The patient was sent to the emergency room for further management.
Figure 1.

CT image showing left renal vein thrombus. Closer inspection demonstrates left renal vein compression as it passes between the superior mesenteric artery and abdominal aorta.
The patient had also been on oral contraceptives for 11 years and was using a combination pill containing ethinyl estradiol and desogestrel. She had switched from another combination pill (containing ethinyl estradiol and levonorgestrel) a year prior. She denied any personal history of thrombosis. She was a non-smoker and denied any history of recent immobilisation, recent prolonged travel, recent surgery, trauma to her abdomen or back, or known malignancy. She was not pregnant. In terms of her family history, she seemed to remember that her grandmother might have had a blood clot when she was pregnant.
Investigations
The patient's vitals were stable and exam revealed isolated left costovertebral angle tenderness. She had no other complaints or findings. Her labs were unremarkable including a normal complete blood count and urinalysis (no haematuria).
Differential diagnosis
Differential diagnosis for renal vein thrombosis includes renal malignancy, nephrotic syndrome, hypovolaemia, extrinsic compression of renal vein, hypercoagulable conditions of the blood, oral contraceptive use and myeloproliferative disorders.
Treatment
The patient was advised to stop combination oral contraceptive pill (OCP) and started on a low-molecular weight heparin bridge to warfarin. Owing to the atypical location of her thrombus, however, haematology was consulted. A hypercoagulable panel was sent prior to starting anticoagulation and this came back only showing low antithrombin III levels. Haematologist suspected that this was likely due to patient being on an OCP. The haematology attending reviewed the CT scan (figure 1) with the radiologist and noted that there was a potential for compression of the left renal vein (nutcracker phenomenon). However, the initial CT was not diagnostic since it was a static study (hence failing to establish whether the renal vein compression was haemodynamically significant). To confirm the diagnosis by some form of dynamic study, interventional radiology (IR) was consulted. A renal ultrasound was performed and was unable to establish the diagnosis. IR then performed an intravascular ultrasound (IVUS). IVUS confirmed the diagnosis of nutcracker syndrome (figures 2 and 3). The patient was informed of her diagnosis and there was a discussion about possible treatment options. Since she was young, it was decided to initially bridge her to warfarin with plans for 6 months of anticoagulation followed by repeat imaging. Need for additional management would be decided at that time.
Figure 2.
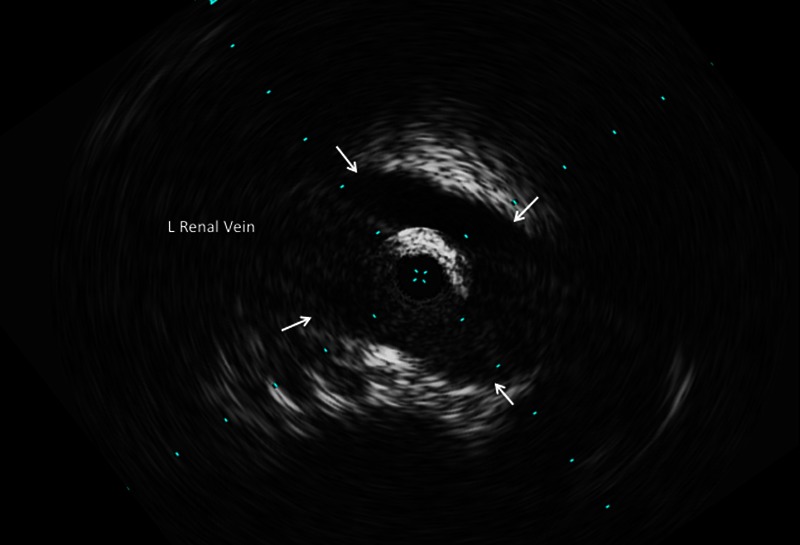
Intravascular ultrasound showing widely open left renal vein at the prestenotic area. Arrows demonstrate vessel walls.
Figure 3.
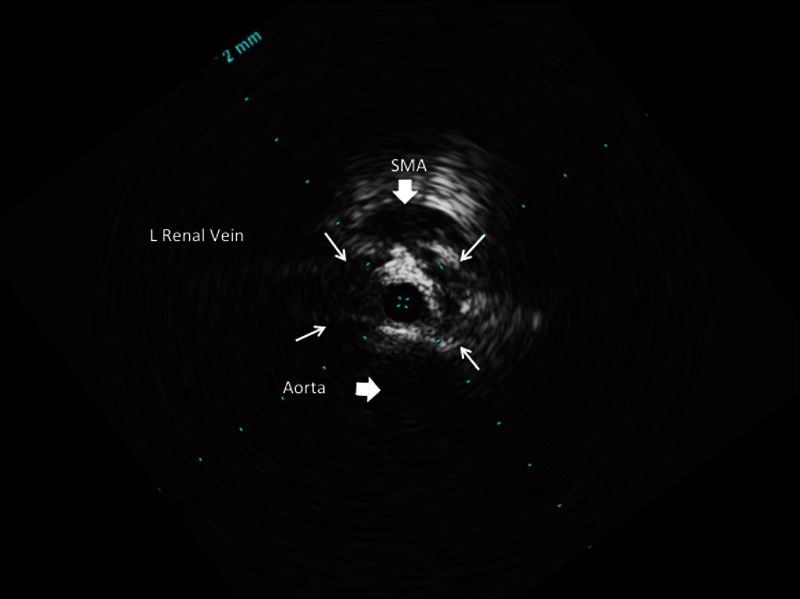
Intra vascular ultrasound showing point of compression of the left renal vein (small white arrows demonstrating vessel walls).
Outcome and follow-up
The patient was discharged to follow with haematology and radiology as outpatient. She was also seen by ObGyn, who switched her to a progestin only contraceptive.
Discussion
Left renal vein (LRV) compression, which is also known as nutcracker phenomenon or renal vein entrapment syndrome, refers to the extrinsic narrowing of the LRV between the abdominal aorta and proximal superior mesenteric artery (SMA). El Sadr and Mina first described this anomaly in 1950 and the term ‘nutcracker syndrome’ was coined in 1972 by de Schepper.1 Notably, symptomatic cases are called ‘nutcracker syndrome’ NCS whereas non-symptomatic patients may be described as having the ‘nutcracker phenomenon’ (NCP).1
There are two anatomical variants. Anterior nutcracker syndrome refers to compression of the LRV as described above. However, another variant, posterior nutcracker syndrome (figure 4) has also been described and refers to the retroaortic position of the LRV with compression of the vessel between the aorta and the vertebral column.1 2
Figure 4.
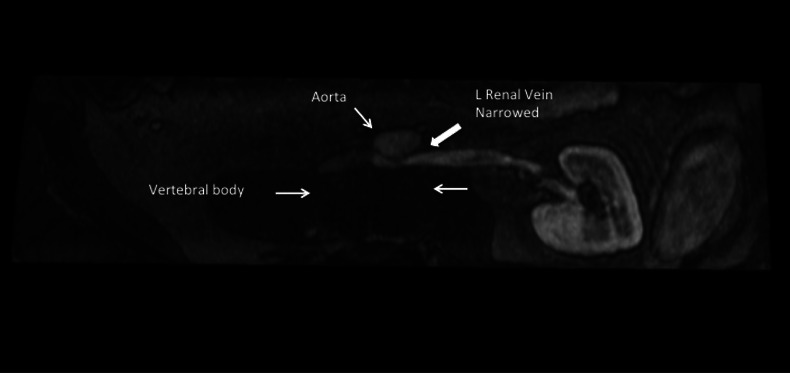
Magnetic resonance venography showing example of posterior nutcracker syndrome (different patient than the one described in case). Left renal vein is narrowed between the abdominal aorta and the vertebral body.
There is some lack of consensus on the prevalence of the disease. Studies note bimodal peak with most cases identified in adolescence to young adulthood and then again in the third to fourth decades of life with a slightly higher prevalence in women.2 3
Symptoms occur due to compression of the LRV and include haematuria, gonadal varices, varicocele, ovarian vein syndrome and back pain.4 Common presenting complaints include left flank pain and haematuria.5 Haematuria is hypothesized to occur due to rupture of the thin walled septum separating the veins from the collecting system.5 The patient may also present with anaemia, which is a result of haematuria. Some patients also present with asymptomatic proteinuria.5 Male patients may present with a left-sided varicocele. Women may present with symptoms of pelvic congestion (pelvic congestion syndrome), which may include dysmenorrhoea, dysuria, dyspareunia and pelvic pain.6 Finally, in some cases, vulvar, gluteal and lower extremity varices have been noted.7
NCS is a radiological diagnosis though a clinical presentation of left flank pain with haematuria, varicocele and orthostatic proteinuria should raise suspicion of the condition.8 Since this is an under diagnosed problem, imaging of the kidneys with CT or ultrasound (US) should be performed when suspected. CT imaging showing the ‘beak sign’ (abrupt narrowing of the LRV with a triangular shape at the aortomesenteric portion) should suggest the presence of NCS.9 Cystoscopy may sometimes be able to identify left ureteral haematuria although this test is unreliable owing to possibility of lack of haematuria at time of exam.9
Since static images will not be able to confirm haemodynamic significance or differentiate between NCP and NCS, dynamic studies are necessary. Doppler US or venography (CT or MR) may be considered. Reno-caval pull back gradient is helpful in establishing the diagnosis.10 Normal reno-caval pullback mean gradient pressure ranges from 0 to 1 mm Hg and a gradient >3 mm Hg has been used as the reference standard for the diagnosis of NCS.10 Our centre has the ability to perform IVUS, which secured the diagnosis in case described above.
In the setting of NCS, some conditions may exacerbate risk for thrombus in the renal vein (differential diagnosis above). Patients who present with no obvious cause should be worked up for these conditions. In some cases, however, cause may be idiopathic. The predicted pathophysiology includes decrease in AT III, decreased plasminogen (likely secondary to urinary loss), platelet activation, hyperfibrinogenaemia and plasminogen activator inhibition.
Learning points.
Patients presenting with left flank pain and haematuria should have nutcracker syndrome (NCS) on their list of differential diagnoses.
NCS is an under detected cause of isolated left renal vein thrombosis.
Untreated NCS may lead to kidney damage.
There are several treatment options available for treating NCS, ranging from simple surveillance to surgical therapy.
Footnotes
Contributors: SKM, GPO and RPR have written the manuscript. This name order reflects contribution. GPO provided radiology images. SKM is the guarantor of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc 2010;2013:552–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhanji A, Malcolm P, Karim M. Nutcracker syndrome and radiographic evaluation of loin pain and hematuria. Am J Kidney Dis 2010;2013:1142–5 [DOI] [PubMed] [Google Scholar]
- 3.Chi YW, Ehrensing C. Images in vascular medicine. Nutcracker syndrome . Vasc Med 2007;2013:251–3 [DOI] [PubMed] [Google Scholar]
- 4.Zhang H, Li M, Jin W, et al. The left renal entrapment syndrome: diagnosis and treatment. Ann Vasc Surg 2007;2013:198–203 [DOI] [PubMed] [Google Scholar]
- 5.Venkatachalam S, Bumpus K, Kapadia SR, et al. The nutcracker syndrome. Ann Vasc Surg 2011;2013:1154–64 [DOI] [PubMed] [Google Scholar]
- 6.Marone EM, Psacharopulo D, Tshomba Y, et al. A typical case of nutcracker phenomenon. J Vasc Surg 2011;2013:219. [DOI] [PubMed] [Google Scholar]
- 7.Scultetus AH, Villavicencio JL, Gillespie DL. The nutcracker syndrome: its role in the pelvic venous disorders. J Vasc Surg 2001;2013:812–19 [DOI] [PubMed] [Google Scholar]
- 8.Rudloff U, Holmes RJ, Prem JT, et al. Mesoaortic compression of the left renal vein (nutcracker syndrome): case reports and review of the literature. Ann Vasc Surg 2006;2013:120–9 [DOI] [PubMed] [Google Scholar]
- 9.Kim KW, Cho JY, Kim SH, et al. Diagnostic value of computed tomographic findings of nutcracker syndrome: correlation with renal venography and renocaval pressure gradients. Eur J Radiol 2011;2013:648–54 [DOI] [PubMed] [Google Scholar]
- 10.Ahmed K, Sampath R, Khan MS. Current trends in the diagnosis and management of renal nutcracker syndrome: a review. Eur J Vasc Endovasc Surg 2006;2013:410–16 [DOI] [PubMed] [Google Scholar]


