Description
A 40-year-old gentleman presented to emergency department (ED) with sudden onset of right-sided chest pain, largely subsided on admission. He was an ex-smoker with a history of basal cell carcinoma and patella fracture. Trachea was central on examination, with absence of right-sided breath sounds. Observations were normal.
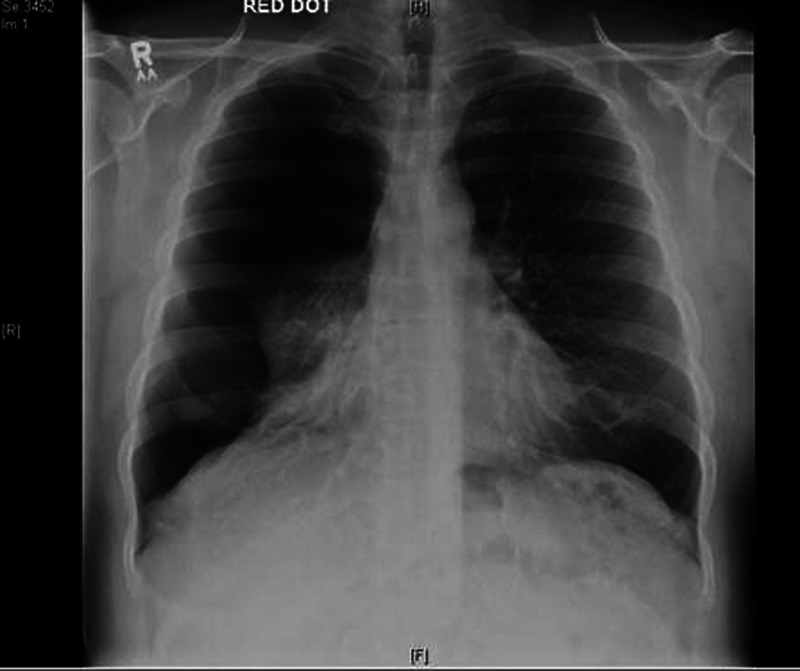
Chest radiograph revealed a large right-sided primary spontaneous pneumothorax (PSP) (figure 1), which was aspirated unsuccessfully. A chest drain was inserted with uneventful recovery (figure 2).
Figure 1.
Erect anteroposterior chest radiograph showing large right-sided pneumothorax with almost complete right lung collapse with loss of right lung markings. There is no tracheal deviation. Pneumothorax defined as ‘large’ by the presence of greater than 2 cm rim between lung margin and chest wall.1
Figure 2.
Erect posteroanterior chest radiograph showing lung fields after chest drain removal. There is no pneumothorax present; however, there is some persistent atelectasis in the right lung. The left lung is clear.
Global occurrence is greater in men, at 0.018–0.028% versus 0.0012–0.006%, with 54% risk of another pneumothorax within 4 years.1 Smoking poses a further 12% risk.1 Alveoli of taller subjects are also prone to greater distension pressure and development of subpleural blebs as negative pleural pressure gradient increases towards the lung apex.1
If present, signs include reduced lung expansion, absent breath sounds and hyper-resonance on the affected side. Although diagnosis and management should be guided clinically, an inspiratory chest x-ray is recommended.1 CT scanning, ‘gold standard’ for size estimation and detection of small pneumothoraces, is advised for uncertain cases.1
Treatment depends on:
Previous lung pathology.
Breathlessness.
- Pneumothorax size.
- Insert chest drain if bilateral or haemodynamically unstable spontaneous pneumothoraces.
- If age >50, clinical/radiological lung pathology or significant smoking history, treat as secondary pneumothorax.1
- If PSP >2 cm or shortness of breath, aspirate less than 1.5 l. If aspiration fails, insert chest drain.
- If <2 cm with no shortness of breath, or successful aspiration, consider discharge with 2–4 week follow-up.1
Learning points1.
Spontaneous pneumothorax should always be considered in a young, tall, male patient who presents with sudden onset chest pain. Delayed presentation comes with the risk of re-expansion pulmonary oedema.
Size of pneumothorax does not necessarily correlate with severity of symptoms—symptoms may even be absent in primary spontaneous pneumothorax and thus a high level of clinical diagnostic suspicion is required. If there are signs of cardio-respiratory compromise, do not delay treatment to perform imaging. Treat as a tension pneumothorax.
Smoking increases the risk of primary spontaneous pneumothorax by a further 12% compared with 0.1% of non-smokers. There is no evidence to suggest development of pneumothorax is associated with physical exertion. However, in view of increased risk of recurrence of pneumothorax in an affected individual, controllable risk factors such as smoking and progression to chronic obstructive pulmonary disease should be addressed.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Reference
- 1.MacDuff A, Arnold A, Harvey J, on behalf of the BTS Pleural Disease Guidelines Group Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline. BTS Guidelines. Thorax 2010;2013(Suppl 2):ii18–31 [DOI] [PubMed] [Google Scholar]