Abstract
A 55-year-old man was admitted with a 2-year history of pseudoexfoliation glaucoma. The best-corrected visual acuities were 10/10 in both eyes. Pseudoexfoliation material was noted on the iris and the lens capsule. Fundus examination evidenced cup-to-disc ratio of 0.7 OD and 0.9 OS with peripapillary atrophy. Gonioscopy revealed open angles. Optical coherence tomography demonstrated peripapillary retinoschisis extending to the nasal macula in the left eye and optic nerve head was almost fully excavated. Coexisting retinoschisis in a patient with glaucoma may interfere with the reliability of retinal nerve fibre layer and ganglion cell complex analysis and may change the treatment plan and follow-up intervals.
Background
Peripapillary and macular retinoschisis have historically been linked to X-linked retinoschisis, optic nerve pits and colobomas.1 2 Few cases of peripapillary retinoschisis associated with advanced glaucoma have been reported recently.3–7 Although the exact aetiology of retinoschisis in these eyes are uncertain, there are two hypotheses proposed by the authors; one states increased intraocular pressure (IOP) and fluctuations in IOP may cause structural defect in the retinal nerve fibre layer and liquid vitreous may enter into the retina. The second is the formation of microhole in the thin tissue of a glaucomatous optic disc and hereby vitreous fluid enter into the retina.
Peripapillary retinoschisis associated with open angle glaucoma, narrow angle glaucoma and normal tension glaucoma have been reported previously.3 4 6 7 However, to the best of our knowledge, there is no report of macular and peripapillary retinoschisis associated with pseudoexfoliation glaucoma.
Case presentation
A 55-year-old man admitted to us with a 2-year history of pseudoexfoliation glaucoma. As far as we learned from his medical records, the patient had severe IOP fluctuations in the left eye. He received brimonidine/timolol fixed combination, travoprost and brinzolamide ophthalmic suspensions. On admission, best-corrected visual acuities were 10/10 in both eyes. His IOP measurements were 13 mm Hg OD and 14 mm Hg OS.
Investigations
Ultrasound pachymetry readings revealed average corneal thickness measurements of 533 µm OD and 540 µm OS. Pseudoexfoliation material was noted on the iris and the lens capsule in both eyes. Fundus examination evidenced cup-to-disc ratio of 0.7 OD and 0.9 OS with peripapillary atrophy (figure 1). Gonioscopy examination revealed open angles in both eyes. The axial length was 23.81 mm OD and 23.72 mm OS. Standard automated perimetry showed generalised reduction of sensitivity in the right eye and preservation of a small central and upper temporal island of vision in the left eye.
Figure 1.
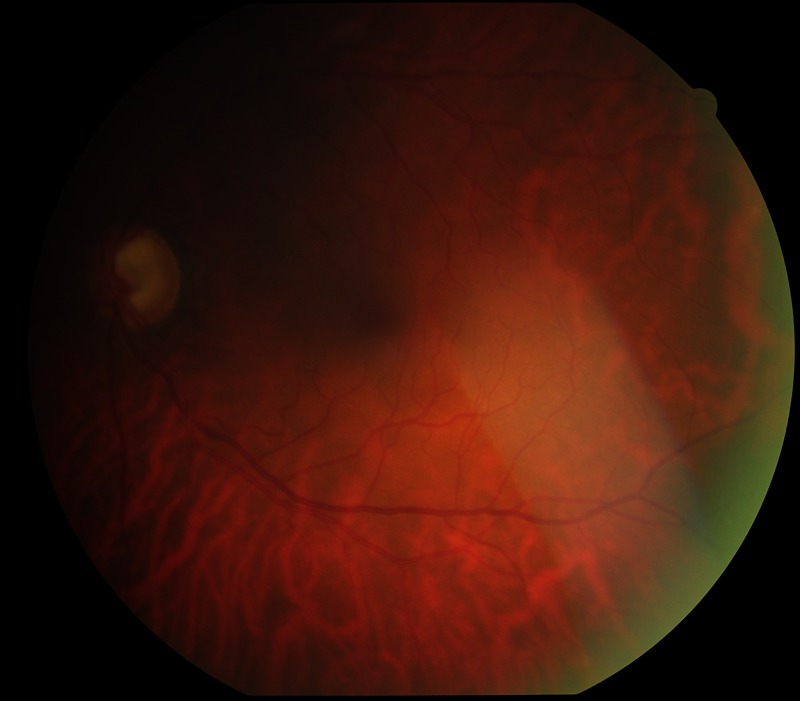
Cup-to-disc ratio of 0.9 in the left eye with a normal macular area.
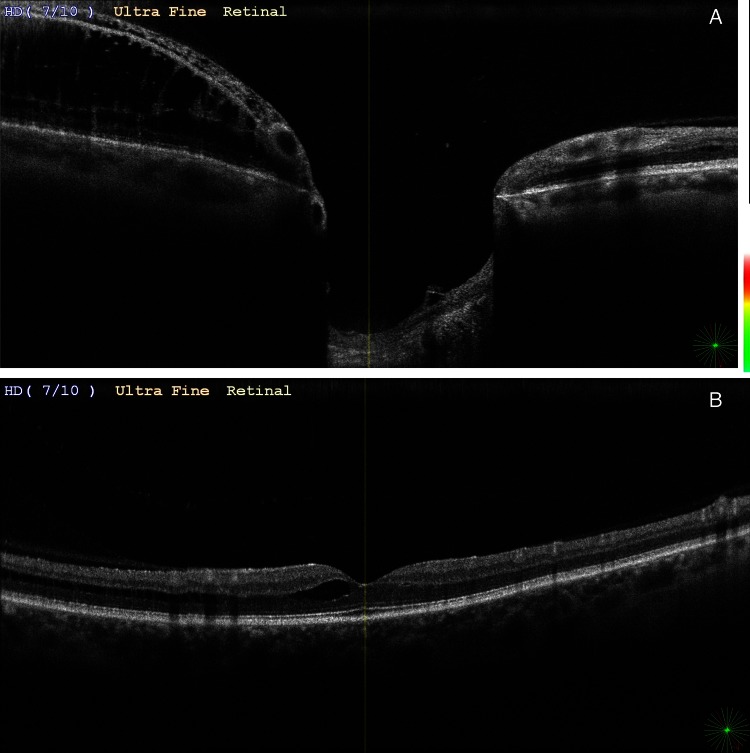
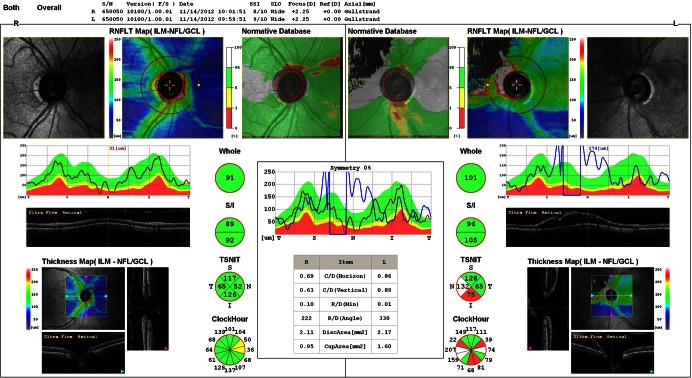
Optical coherence tomography demonstrated peripapillary retinoschisis extending to the nasal macula in the left eye and optic nerve head was almost fully excavated (figure 2A,B). Ganglion cell complex was significantly thinner on the left and slightly reduced in the right eye. Retinal nerve fibre layer () analysis showed thickening in all areas with retinoschisis while it was within normal limits on the right (figure 3). There was no optic disc coloboma, congenital, or acquired optic nerve head pit and vitreomacular traction. Fundus florescein angiography did not show any leakage.
Figure 2.
(A and B): Optical coherence tomography of left eye showing peripapillary and macular schisis cavities.
Figure 3.
Optic nerve head and retinal nerve fibre layer (RNFL) imaging using optical coherence tomography demonstrating RNFL thickening in areas with retinoschisis and high cup-to-disc ratio in the left eye.
Outcome and follow-up
During the course, the patient had no complaints of visual loss and had a well-controlled IOP with medical treatment. In addition, there were no signs of retinal detachment. Therefore, we decided to examine the patient at frequent intervals.
Discussion
Peripapillary retinoschisis associated with primary open angle glaucoma or narrow angle glaucoma and macular retinoschisis associated with angle closure glaucoma have been reported previously.3 4 6 7 The common characteristics of all these patients are large cup-to-disc ratio (thin rim), high IOP together with fluctuations and liquefied vitreous. Retinoschisis in patients with glaucoma may be related with advanced stage of the glaucoma, but the type of the glaucoma does not seem to have a role in the pathogenesis.
Learning points.
Coexisting retinoschisis in a patient with glaucoma may interfere with the reliability of retinal nerve fibre layer and ganglion cell complex analysis and may change the treatment plan and follow-up intervals.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Madjarov B, Hilton GF, Brinton DA, et al. A new classification of the retinoschisis. Retina 1995;2013:282–5 [DOI] [PubMed] [Google Scholar]
- 2.Lincoff H, Lopez R, Kreissig I, et al. Retinoschisis associated with optic nerve pits. Arch Ophthalmol 1988;2013:61–7 [DOI] [PubMed] [Google Scholar]
- 3.Hubschman JP, Reddy S, Kaines A, et al. Nasal retinoschisis associated with glaucoma. Ophthalmic Surg Lasers Imaging 2010;2013:1–4 [DOI] [PubMed] [Google Scholar]
- 4.Kahook MY, Noecker RJ, Ishikawa H, et al. Peripapillary schisis in glaucoma patients with narrow angles increased intraocular pressure. Am J Ophthalmol 2007;2013:697–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zumbro DS, Jampol LM, Folk JC, et al. Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol 2007;2013:70–4 [DOI] [PubMed] [Google Scholar]
- 6.Hollander DA, Barricks ME, Duncan JL, et al. Macular schisis detachment associated with angle closure glaucoma. Arch Ophthalmol 2005;2013:270–2 [DOI] [PubMed] [Google Scholar]
- 7.Zhao M, Li X. Macular retinoschisis associated with normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol 2011;2013:1255–8 [DOI] [PubMed] [Google Scholar]