Abstract
Desmoplastic ameloblastoma (DA) is a newly recognised, rare odontogenic neoplasm that is a histological variant of ameloblastoma. In this type, the islands of ameloblastoma are surrounded and often compressed by a dense and sometimes hyalinised fibrous connective tissue. Although ameloblastomas are usually located in the mandible, this variant often occurs in the anterior maxilla. In view of the paucity of DA case series and only limited understanding of its biological behaviour and prognosis, proper treatment strategies for DA are not entirely defined so far. The purpose of this paper was to review the literature and to demonstrate a rare case for an improved understanding of the behaviour and prognosis of DA.
Background
Desmoplastic ameloblastomas (DAs) are rare, accounting for approximately 4–13% of ameloblastomas.1 Their radiographic appearance as a mixed radiolucent-radio-opaque lesion is commonly confused with fibro-osseous lesions as in the present case. The fact that recurrences have been documented by many authors suggests that the tumour has a potentially aggressive biological behaviour. In view of the paucity of DA case series, it continues to remain as one of nature's secrets. Up until now, less than 150 patients have been reported in the literature. A painless swelling or bony expansion is the most conspicuous clinical manifestation in most of the cases.2
This report gives a comprehensive knowledge regarding the epidemiology, classification, occurrence, diagnosis, behaviour and treatment of DA.
Case presentation
A 47-year-old female patient presented with swelling on the front and right side of the upper jaw for 6 months. It was insidious in onset and gradually progressive in nature. On clinical examination, a bony hard swelling of the right maxillary alveolar ridge was observed extending from the upper right central incisor (11) to the mesial surface of the upper right second molar (17) (figure 1). Loss of vitality was noted with upper-right central incisor, lateral incisor and canine. A clinical diagnosis of a fibro-osseous lesion was made. Maxillary occlusal radiograph and incisional biopsy were planned for further confirmation.
Figure 1.

Intraoral photograph showing a swelling of the right maxillary alveolar ridge extending from 11 to mesial surface of 17.
Investigations
Maxillary occlusal radiograph
Radiograph revealed a multilocular, mixed radiolucent-radio-opaque lesion with ill-defined borders causing an expansion of the buccal and palatal cortical plates and erosion of the buccal cortex (figure 2).
Figure 2.
Multilocular, mixed radiolucent-radio-opaque lesion with ill-defined borders causing expansion of the buccal and palatal cortical plates and erosion of the buccal cortex.
Histopathology
The histopathological examination of the incisal biopsy showed irregular, bizarre-shaped odontogenic epithelial islands and cords in a moderately cellular fibrous connective tissue with abundant thick collagen fibres compressing the odontogenic islands giving them a stellate or an ‘animal-like’ configuration. The epithelial cells showed hyperchromatic nuclei. The centre of the islands appeared to be hypercellular with mainly spindle-shaped cells and few squamoid cells. A few islands showed peripheral tall columnar cells. The biopsy findings were suggestive of DA (figures 3 and 4).
Figure 3.
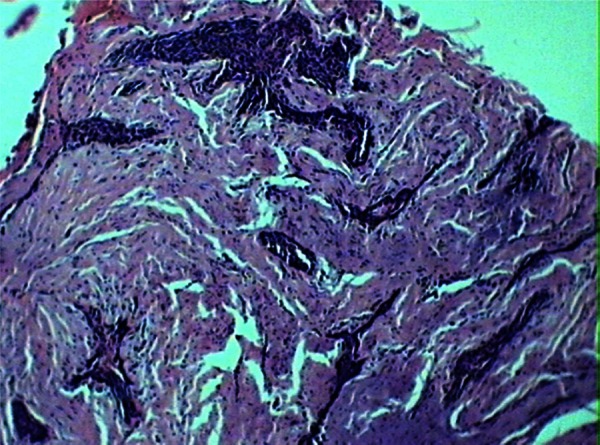
H&E, ×40, photomicrograph showing bizarre-shaped hypercellular odontogenic epithelial islands with pronounced desmoplastic stroma.
Figure 4.

H&E, ×400×, high-power photomicrograph confirming the features seen in figure 3.
The histopathological examination of the excisional biopsy revealed findings identical to the incisional biopsy. In addition, the decalcified sections showed irregular, bizarrely shaped, large, hypercellular, odontogenic epithelial islands in a moderately cellular, dense fibrous connective tissue. Numerous irregular bony trabaculae were seen in close approximation of the tumour islands (figures 5 and 6).
Figure 5.

Gross specimen of the excised maxilla.
Figure 6.

H&E, ×40×, photomicrograph showing findings identical to incisional biopsy (figures 3 and 4).
Differential diagnosis
Squamous odontogenic tumour and ameloblastic fibroma could be considered as a histological differential diagnoses, whereas fibro-osseous lesions are the most likely diagnoses on imaging. Accurate diagnosis of the desmoplastic variant of ameloblastoma depends on the identification of the typical ameloblastic areas, and this may require the examination of more tissues or a repeated biopsy.3
Treatment
A partial maxillectomy for tumour resection was performed (figure 7) under general anaesthesia with reconstruction and prosthetic rehabilitation planned at a later stage.
Figure 7.

H&E, ×400 photomicrograph showing a focal ameloblastic island showing peripheral tall columnar ameloblast-like cell.
Outcome and follow-up
The patient is under observation for any complication or recurrence.
Discussion
DA was first described by Eversole et al in 1984.4 Although ameloblastomas are usually located in the mandible, this variant often occurs in the anterior maxilla and shows unique radiographic features that appear as a mixed radiolucent-radio-opaque lesion similar to a benign fibro-osseous lesion.5
Epidemiology and prevalence
DA constitutes 0.9–12.1% of all ameloblastomas. The mean age at initial presentation is 42.3 years (range 17–70 years) with age and gender predilection similar to that of other ameloblastomas. Data from different geographical regions seem to suggest a biogeographical pattern in which the relative frequency of DA is slightly higher in Asian population. However, more systematic studies on DA are needed to prove such suggestions.6
Aetiology
It is suggested that DA develops from the periodontal membrane of the related tooth. Moreover, some suggest that DA might arise from epithelial rests of Malassez in the periodontal membrane.7
Classification
WHO classifies ameloblastomas into four variants:
Solid/multicystic;
Extraosseous or peripheral;
Desmoplastic;
Unicystic.
A combination of DA with solid/multicystic ameloblastoma is known and has been termed as ‘hybrid lesion’.8
Clinical features
The WHO classification of odontogenic tumours has classified it as a separate type of ameloblastoma and quoted that the incidence ratio in maxilla:mandible is 1:1, with a predilection for the anterior mandibular region. A painless swelling of the jaw bone represents the chief initial complaint. The size of the tumour varies between 1.0 and 8.5 cm in diameter.8
Radiographic features
Radiographically, about 50% show a mottled, mixed radiolucency/radio-opacity with diffuse margins, suggesting a fibro-osseous lesion. Resorption of tooth roots and bone formation may occur. The ill-defined borders make high-resolution CT and MRI helpful in treatment planning.4 8 Similar clinical and radiographic presentations of the present case lead to an initial diagnosis of a fibro-osseous lesion.
Histopathology
The lesional tissue has a gritty consistency; the cut surface is solid in most cases. The stromal component dominates (ie, dense collagenous stroma—desmoplasia), compressing the odontogenic epithelial components. The epithelial tumour islands are very irregular or bizarre in shape with a pointed, stellate appearance. The epithelial cells at the periphery of the islands are cuboidal with occasional hyperchromatic nuclei. Columnar cells with nuclear polarity are rarely conspicuous. The islands have a swirled, hypercellular centre with spindle-shaped or squamous epithelial cells. Microcysts may occur centrally. Myxoid changes of the juxtaepithelial stroma are often found. The formation of metaplastic osteoid trabeculae (osteoplasia) may be present. A fibrous capsule is not present corresponding to the radiographically poorly defined tumour margin. A combination of DA with solid multicystic ameloblastoma is known and has been termed as ‘hybrid lesion’.6 8 9
Immunoprofile
In contrast to SMAs, marked immunoexpression of transforming growth factor (TGF-β) is observed in DA cases.8 The authors suggested that TGF-β produced by DA tumour cells plays a prominent part in the desmoplastic matrix formation.9
Furthermore, along with regular investigations, such as radiographic, histopathology and immunoprofiling, CT and/or MRI are very helpful in diagnosing rare lesions like this. Since our patient was poor, to reduce the financial burden on him, we could not perform these investigations.
Recurrence
Concerning the biological behaviour of DA, it is mentioned in the WHO classification of odontogenic tumours that DA, like unicystic ameloblastoma and peripheral ameloblastomas, possibly has a lower recurrence rate than other ameloblastomas.8 In contrast to that statement of WHO, a review of the literature provided the information that DA showed a similar recurrence rate (15.9%) as that of with the other types of ameloblastomas.1 Even Keszler et al10 reported a higher recurrence rate (21.4%) than the other type (10.1%) of ameloblastoma. The reason for this may be somewhat hypothetical: first, radiographically, DAs are apt to be mismatched with fibro-osseous lesions. The accurate diagnosis of a DA is hard to achieve before the operation; second, DA is frequently present with ill-defined border making the exact interface of the lesion with normal bone difficult to investigate. Third, the more common location in the maxilla may produce an early invasion of the adjacent structures.
Learning points.
Rare odontogenic neoplasm with unusual clinical, radiographic and histological presentation.
The definite diagnosis requires histopathological examination.
With the potential for recurrence, such cases should always be treated by complete resection.
In view of the paucity of such case series and limited understanding of its biological behaviour and prognosis, proper treatment strategies are not entirely defined so far. Hence, such cases need to be identified and reported.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zhi S. Desmoplastic ameloblastoma—a review. Oral Oncol 2009;2013:752–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soheyl S, Shambulingappa P, Isha S, et al. Desmoplastic ameloblastoma: a case report. J Dent Res Dent Clin Dent Prospects 2011;2013:27–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lam KY, Chan AC, Wu PC, et al. Desmoplastic variant of ameloblastoma in Chinese patients. Br J Oral Maxillofac Surg 1998;2013:129–34 [DOI] [PubMed] [Google Scholar]
- 4.Mamoru W, Takuya H, Takashi I. Follicular/desmoplastic hybrid ameloblastoma with radiographic features of concomitant fibro-osseous and solitary cystic lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;2013:774–80 [DOI] [PubMed] [Google Scholar]
- 5.Hirota M. Desmoplastic ameloblastoma featuring basal cell ameloblastoma: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;2013:160–4 [DOI] [PubMed] [Google Scholar]
- 6.Marx. R, Stern D. Oral and maxillofacial pathology. Illinois: Quintessence Publishing Co Ltd, 2002:650 [Google Scholar]
- 7.Katsura K, Maruyama S, Suzuki M, et al. A case of desmoplastic ameloblastoma arising in the maxillary alveolus: the origin and time-course changes in the early stage of tumor development observed on dental radiographs. Dentomaxillofac Radiol 2011;2013:126–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gardner DG, Helkinheimo K, Shear M, et al. Ameloblastomas. In: Barnes L, Eveson JW, Reichart P, Sidransky D, eds. World Health Organization Classification of Tumours, Pathology & Genetics, Head and Neck Tumors. Lyon: IARC Press; 2005;296–300 [Google Scholar]
- 9.Reichart P, Philipsen H. Desmoplastic ameloblastoma in Odontogenic tumors and allied lesions. London: Quintessence Publishing Co Inc, 2004 [Google Scholar]
- 10.Keszler A, Paparella ML, Dominguez FV. Desmoplastic and non-desmoplastic ameloblastoma: a comparative clinicopathological analysis. Oral Dis 1996;2013:228–31 [DOI] [PubMed] [Google Scholar]



