Abstract
This is a case of a 69-year-old man with a history of asbestos exposure who presented with acute shortness of breath. His chest x-ray showed bilateral hydropneumothorax. Further investigations including CT chest and video-assisted thoracoscopic surgery revealed bilateral pleural thickening and histology confirmed epithelioid mesothelioma. This case highlights the need for clinicians to be aware of atypical presentations of malignant pleural mesothelioma as well as the importance of considering underlying secondary causes such as malignancy in the older patient presenting with spontaneous pneumo/hydropneumothorax.
Background
Malignant pleural mesothelioma (MPM) is a rare malignancy with a poor prognosis. It typically presents in patients with a history of asbestos exposure in the fifth to seventh decades of life with symptoms of dyspnoea, non-pleuritic chest pain or both. The most common radiographical presentation is unilateral pleural effusion with or without ipsilateral pleural thickening or mass.
Case presentation
A previously fit and healthy 69-year-old man presented with a 6-day history of shortness of breath on exertion and fleeting non-pleuritic pain in his chest. He denied any symptoms of cough, haemoptysis, fever or weight loss, and had no orthopnoea or ankle swelling. He had a history of long-haul air travel 3 weeks previously, but no symptoms of calf pain or swelling. He was a lifelong non-smoker and was an electrician by trade, with a history of asbestos exposure between the age of 15 and 30 years.
On examination he was neither tachycardic nor tachypnoeic and had oxygen saturations of 94% at room air. Chest auscultation revealed reduced breath sounds bilaterally.
Investigations
A chest radiograph revealed bilateral hydropnuemothorax (figures 1 and 2). A CT chest with pulmonary angiography was performed to look for potential secondary causes of pneumothorax.
Figure 1.
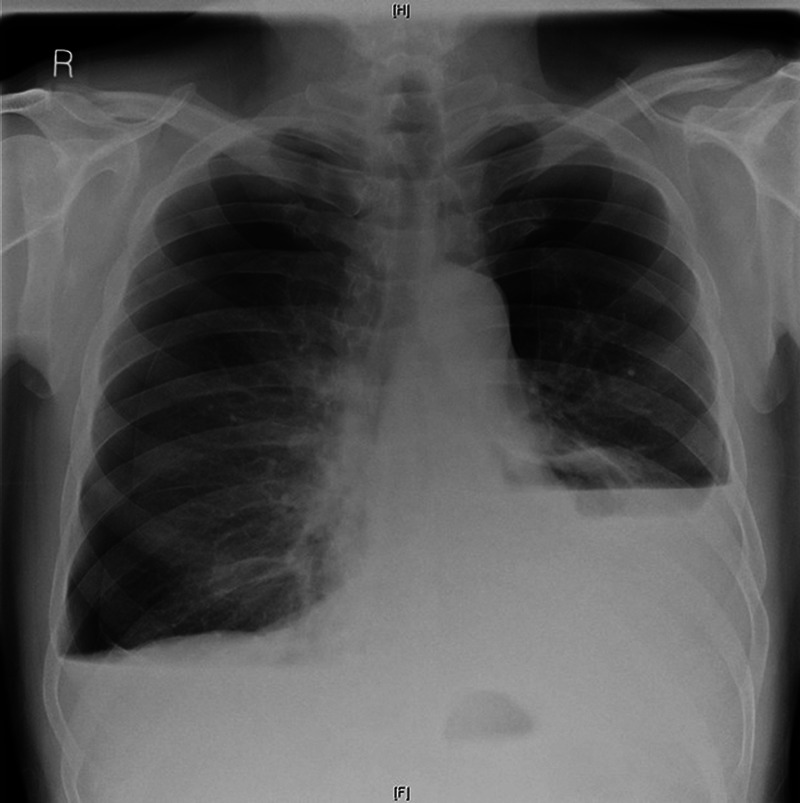
Anteropostrrior view of chest radiograph showing bilateral hydro pneumothorax.
Figure 2.
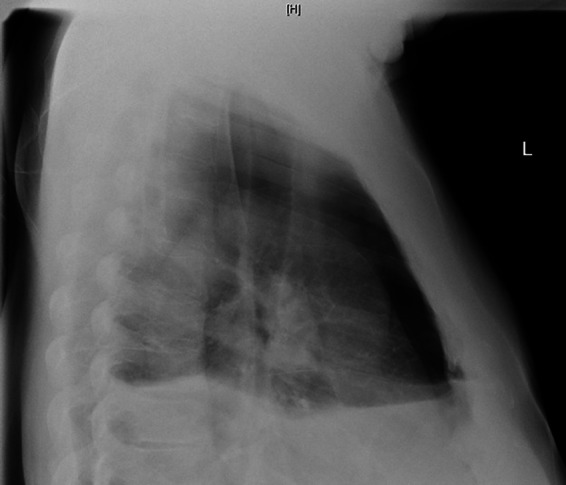
Lateral view of chest radiograph showing bilateral hydropneumothorax.
The CT chest showed large bilateral hydropneumothorax with significant collapse of the underlying lungs (figure 3). There was a very small amount of mediastinal free gas and a 10 mm superior mediastinal, 12 mm right hilar and 15 mm subcarinal node. There was bilateral thickening more marked on the left.
Figure 3.
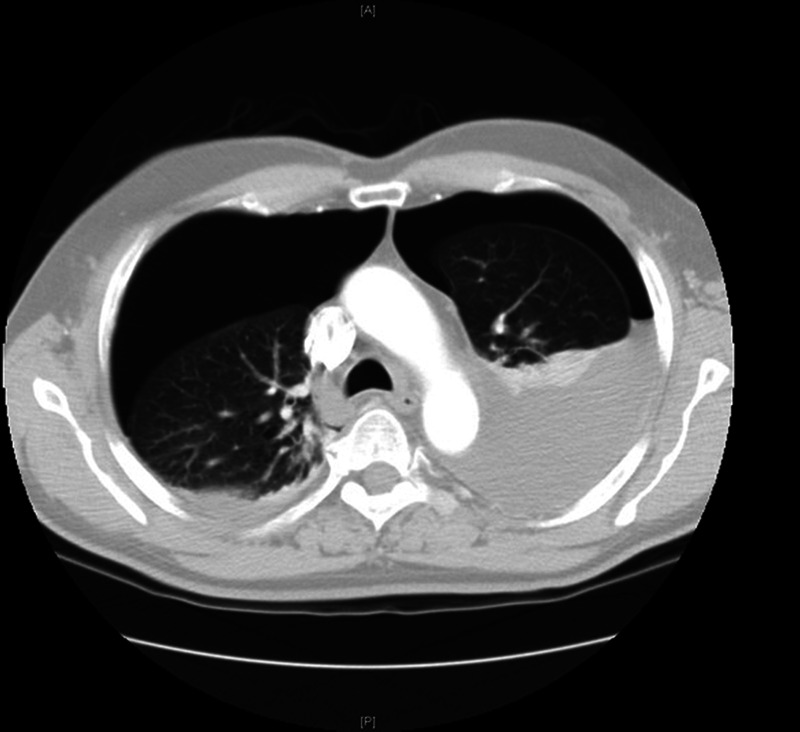
CT chest showing bilateral hydropneumothorax and pleural thickening.
Treatment
The patient had bilateral chest drains inserted. Diagnostic cytology of the pleural fluid showed moderate numbers of reactive mesothelial cells, many polymorphs, some lymphocytes and red blood cells but no malignant cells. The patient underwent video-assisted thoracoscopic surgery (VATS) which showed pleural nodules and fibrinous deposits, more on the left than on the right. Talc pleurodesis was performed in the same setting. Pleural biopsies revealed epithelioid mesothelioma.
Outcome and follow-up
The patient was referred to oncology and underwent four cycles of cisplatin and pemetrexed chemotherapy, for which he responded well both clinically and radiologically on follow-up imaging. However, 11 months after his diagnosis, further imaging showed left-sided circumferential pleural thickening and progression of the disease. (figure 4). Unfortunately, the patient died 4 months later.
Figure 4.
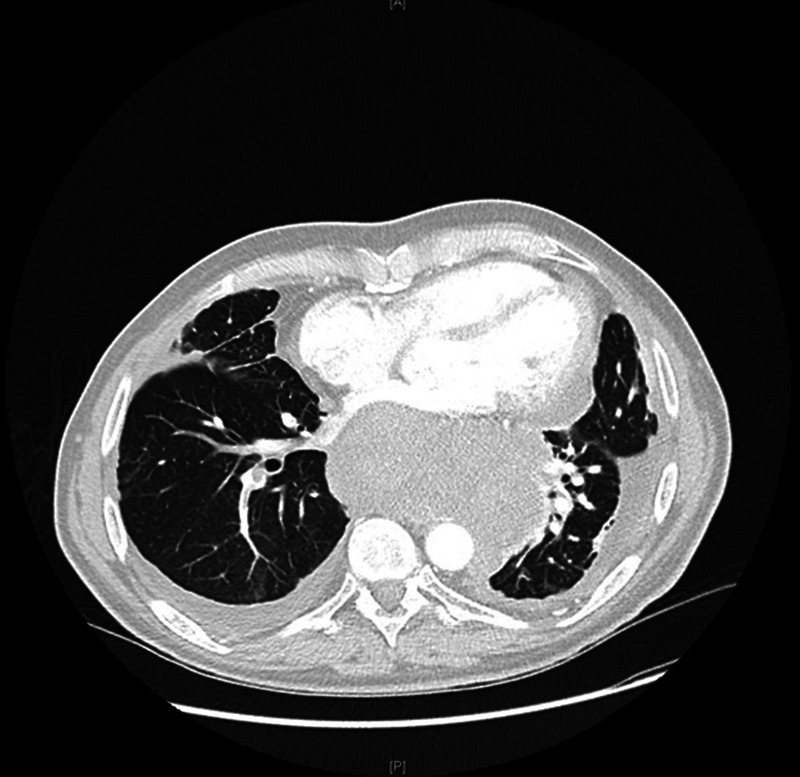
CT chest showing bilateral progression of the mesothelioma.
Discussion
Radiologically, MPM typically presents with pleural effusion and pleural thickening. Although uncommon, spontaneous pneumothorax is a recognised presentation.1 Hydropneumothorax secondary to MPM is also uncommon with descriptions of this phenomenon limited to a handful of case reports.2–5 The mechanism underlying such presentations is uncertain but may be related to rupture of necrotic tumour nodules.
Bilateral presentations of pneumothorax and hydropneumothorax are even more unusual.
On review of literature we were able to find only one case report describing bilateral spontaneous pneumothorax as the primary presentation of malignant pleural mesothelioma.6 We were unable to find any cases describing bilateral hydropnuemothorax in mesothelioma, and indeed there appear to be only two documented cases of bilateral hydropneumothorax because of other causes. Steeghs et al7 reported a case in a patient with pulmonary rheumatoid nodules during treatment with methotrexate, while Daoud8 reported a similar case in pulmonary sarcoidosis.
Given that the number of mesothelioma cases in the UK has risen in the past 50 years, with deaths predicted to peak between 2011 and 2015,9 recognition of atypical presentation is increasingly important to facilitate timely diagnosis and appropriate management. In a recent case series Saleh et al2 suggest performing CT scans of the chest in all patients over the age of 50 presenting with spontaneous pneumothorax so as to rule out an underlying malignant cause or visualise big bullae. Although there are currently no recommendations to this effect in the UK BTS10 or American College of Chest Physicians11 guidelines on management of spontaneous pneumothorax, this case would certainly seem to support the utility of such an approach, especially in patients with a history of environmental asbestos exposure.
Learning points.
Malignant pleural mesothelioma can present in unusual ways such as spontaneous pneumothorax or hydropneumothorax.
Consideration should be given to CT scanning in older patients presenting with spontaneous hydropnuemothorax or pneumothorax to identify potential underlying malignancy, particularly when there is a history of environmental asbestos exposure.
Footnotes
Contributors: HEF and JG had the idea of writing this case report. They were both involved at looking after the patient. HEF and VKW performed literature search and wrote the article. JG reviewed the article before submission. HEF is the guarantor for this article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.British Thoracic Society Standards of Care Committee BTS statement on malignant mesothelioma in the United Kingdom. Thorax 2007;2013:ii1–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saleh HZ, Fontaine E, Elsayed H. Malignant pleural mesothelioma presenting with a spontaneous hydropneumothorax: a report of 2 cases. Rev Port Pneumol 2012;2013:93–5 [DOI] [PubMed] [Google Scholar]
- 3.Guha K, Jones D, James HK, et al. Recurrent hydropneumothorax as a presenting feature of malignant mesothelioma. Eur J Intern Med 2008;2013(Pt1):63–4 [DOI] [PubMed] [Google Scholar]
- 4.Serap H, Hanta I, Karatash M. Spontaneous hydrpneumothorax: an unusual presentation of malignant pleural mesothelioma. Turk Resp J 2002;2013:127–9 [Google Scholar]
- 5.Wu H, Tino G, Gannon FH, et al. Lepidic intrapulmonary growth of malignant mesothelioma presenting as recurrent hydropneumothorax. Hum Pathol 1996;2013:989–92 [DOI] [PubMed] [Google Scholar]
- 6.6.Margery J, Regnard JF, Chompret A, et al. Malignant mesothelioma of the pleura revealed by bilateral spontaneous pneumothorax. Rev Pneumol Clin 2005;2013(5 Pt 1):332–3 [DOI] [PubMed] [Google Scholar]
- 7.Steehs N, Huizinga TW, Dik H. Bilateral hydropnuemothoraces in a patient with pulmonary rheumatoid nodules during treatment with methotrexate. Ann Rheum Dis 2005;2013:1661–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daoud BT, Patel RG. Pulmonary sarcoidosis: presentation as bilateral spontaneous hydropneumothorax and pulmonary infiltrates. Southern Med J 2000;2013:494–6 [PubMed] [Google Scholar]
- 9.Hodgson JT, McElvenny DM, Darnto AJ, et al. The expected burden of mesothelioma mortality in Great Britain from 2002 to 2050. Br J Cancer 2005;2013:587–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;2013(Suppl. 2):ii18–31 [DOI] [PubMed] [Google Scholar]
- 11.American college of Chest Physicians Management of spontaneous pneumothorax. Chest 2001;2013:590–602 [DOI] [PubMed] [Google Scholar]


