Abstract
We present a 46-year-old Somalian woman, who attended our hospital, with 1 week history of worsening epigastric pain and vomiting, worse after eating on a background of 3 months history of four stones loss of weight, malaise and decreased appetite. CT scan of the abdomen revealed an annular 10 cm long mass of the right transverse colon with a second mass of the caecum raising concerns of a synchronous colonic cancer. She underwent an extended right hemi-colectomy due to the development of obstruction from the transverse colon lesion. The histology revealed caseating, transmural granulomatous inflammation consistent with tuberculosis. She had an uneventful recovery and was discharged on the tenth postoperative day on antituberculosis (anti-TB) medications. She reports complete resolution of her symptoms 4 months after discharge.
Background
Gastrointestinal tuberculosis (GITB) is an uncommon encounter in clinical practice especially in the UK. However, with the increase of influx of immigrants and the rising numbers of HIV-positive patients it is becoming a more frequent phenomenon. Clinicians need to have a high index of suspicion in the above two groups of people as early treatment with anti-TB medications can successfully treat the majority of the patients.
Case presentation
A 46-year-old Somalian woman presented with 1 week history of worsening epigastric pain, more severe after meals, associated with vomiting and loose, non-bloody stools. This was on a background of a 3 months history of four stones of weight loss, malaise and decrease appetite.
She had a medical history of haemorroids and peptic ulcer disease and was taking lanzoprazole.
She had a strong family history of gastric carcinoma with her father, sister and brother all died of the disease.
She was born is Somalia but was living and working in the UK since the age of 32.
On examination she had a blood pressure of 134/98, heart rate 90 and temperature 37.1°C. Abdominal examination revealed a soft but tender epigastrium with no guarding or rebound tenderness and a normal digital rectal examination.
Investigations
Haematological investigations revealed a haemoglobin value of 13.8 g/dl, white cell count 6.1×109/l and platelets 548×109/l. Her U+E's and liver function tests were within normal limits and C reactive protein was 105 mg/l. Tumour markers of carcino-embryonic antigen and cancer antigen 19-9 were also normal.
CT with contrast revealed a 10 cm long segment stricture of the hepatic flexure of transverse colon (figure 1) and a second annular wall thickening of the caecum (figure 2). There was also moderate dilation involving the proximal colon and few subhepatic lymph nodes, appearances suggesting synchronous colonic carcinoma. CT chest was normal.
Figure 1.

The 10 cm longitudinal lesion of the transverse colon.
Figure 2.
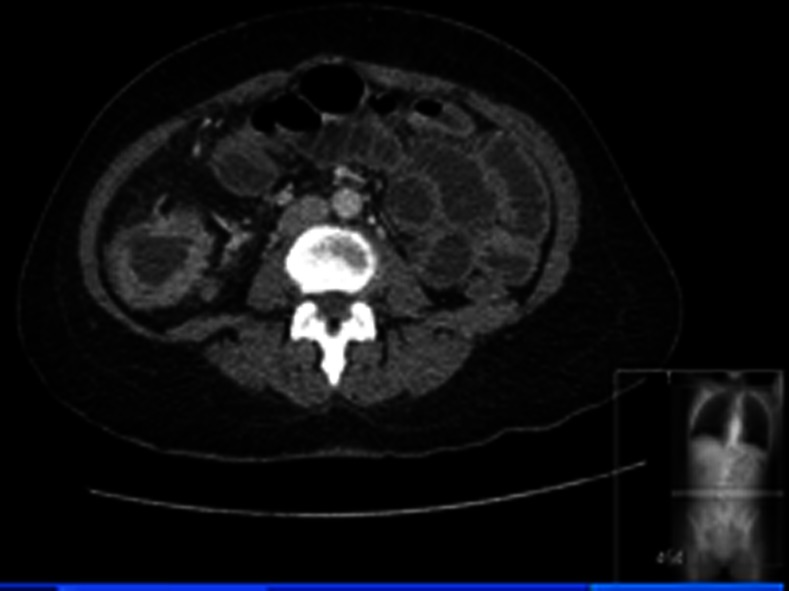
CT abdomen showing an annular caecal lesion.
Differential diagnosis
The two main differentials to consider from the history and examination are inflamatory bowel disease (IBD) and bowel cancer as both of them can have similar systemic and bowel symptoms. However, strong family history of gastrointestinal cancer along with the CT findings pointed initially towards colonic cancer. It is important to note that even though she was from a group of people with high prevalence of TB, the absence of any lung lesions and the absence of rigors and night sweats made it difficult at this point to suspect TB of the colon due to the rarity of this phenomenon.
Treatment
She was taken for a laparotomy 2 days after admission.
A midline incision was done and the right colon was mobilised safeguarding the duodenum. An extended right hemi-colectomy was performed taking down the ileocolic, right colic and right branch of middle colic arteries. Proximal half of the transverse colon and 10 cm of the terminal ileum were resected. Splenic flexure and left colon were mobilised for tension-free anastomosis. Air/water-tight anastomosis was achieved with a stapler and suture line over-run with 3-0 polydioxanon suture material (PDS). Peritoneal cavity was washed with 1 litre of warm normal saline. A 24 F-Robinson drain was placed in the right para-colic gutter. The skin was closed with loop PDS × 2 and skin clips.
Outcome and follow-up
Histology report revealed appearances suggestive of tuberculosis with severe caseating, transmural granulomatous colitis in both caecum and transverse colon and also caseating granuloma within the lymph nodes. There was no evidence of malignancy.
She had an uneventful postoperative recovery and was discharged home on the tenth postoperative day with anti-TB medications. She remains asymptomatic 4 months following treatment with resolution of her symptoms.
Discussion
TB is one of the commonest infections affecting poor socioeconomic groups in high-income and developing countries. In 2011, there were 8.7 million new cases of TB worldwide of which 13% involved co-infection with HIV.1 The majority of the infections in countries like the UK occur in foreign-born residents and immigrants. This is something that the clinician has to keep in mind when dealing with this group of patients especially in those with long-term non-specific symptoms.
GITB is the sixth commonest extra-pulmonary site. It is not entirely known if the bacteria colonise the bowel by penetrating through the wall or enter that site through the arterial circulation. Our patient had both lesions in the distribution of superior mesenteric artery (SMA), but the fact that no other disease were found in the rest of the body makes the possibility of haematogenous spread less likely. The ileo-caecal area is the commonest site affected and is thought to be due to the abundant lymphoid tissue and the stasis of the stools around that segment. The rest of the colon is affected with decreasing frequency further away from ileo-caecal area with recto-sigmoid less frequent.
The symptoms are not specific and can mimic diseases like Crohn's disease and colon cancer. Commonest complains are abdominal pain 80.6%, weight loss 74.63%, loss of appetite 62.69%, fever 40.3%, loose stools 16.42% and alternate constipation and diarrhoea 25.37%.2
Our patient had no evidence of pulmonary TB and this is the case for about 75–80% of patients with GITB. It is not clear why some are affected by extra-pulmonary TB and some not, but it is shown that race, age, underlying disease, the genotype of the bacteria and the immune status are factors that are related to the pathogenesis.3 The immune status is also found to affect manifestation of bowel TB. The ulcerative form (60%) tends to be more common in the immunocompromised individuals and the hypertrophic form (10%) in immunocompetent patients. Our patient had a negative HIV test and her CT image showed the hypertrophic form.
In our case we were unable to identify the acid-fast bacilli with the Ziehl-Neelsen stain (ZN), but she responded well on anti-TB medications. PCR which is the test with the higher sensitivity and specificity is not usually performed as it is expensive, it takes time for the results to be available and it does not alters the management of the patient as the treatment will be started before the results. Demonstration of caceating granuloma and response to anti-TB medications are adequate to make the diagnosis of TB.4 Crohn's disease can have similar features as it can also present with skip lesions in two different part of the bowel and have transmural granulomatous inflammation in histology. However, in Crohn's disease the granulomas do not show caceation and there are no hypertrophic lesions of the colon but rather strictures, fistulas and deep ulcers.
It is important to differentiate Crohn's disease from TB as misdiagnosing Crohn's disease instead of TB, can have deleterious effects for the patient due to the immunosuppressive medications given for Crohn's disease.
Successful treatment of colonic TB can be achieved with conservative management with oral anti-TB medications unless a surgical emergency like perforation or obstruction occurs. In a prospective study 69 patients, confirmed to have colonic TB by either histological evidence of caseating granuloma and/or acid-fast bacilli, were followed up. Five of them required an emergency operation at some point but 48 patients who were successfully followed up by endoscopy 4 weeks after treatment, 75–86% showed resolution of the lesions.2
Therefore, in cases of high-risk patients for TB presenting with non-specific symptoms with colonic thickening on imaging, it is important to successfully biopsy the lesion during endoscopy as this can save the patient from undergoing an operation. However, close monitoring of the patient's response to medical treatment is required as failure of symptoms to regress and the lesions to decrease in size might be a hint of a more sinister underlying pathology, like carcinoma. In a paper by Falagas et al,5 where they studied all patients in literature found to have TB and cancer together, it was shown that there is evidence of coexistence of TB and malignancy. There is the possibility of development of cancer on the background of previous TB infection and the concurrent existence of TB and malignancy in the same patient. This can be explained by the fact than on a cellular level chronic TB infection is capable of inducing DNA damage and therefore carcinogenesis. This is thought to be due to production of nitric oxide and oxygen-free radicals and the increased synthesis of B-cell lymphoma 2 (BCL-2), which leads to increased antiapoptotic activity.
We encountered many cases of colonic TB in literature but we have not come across a case similar to this in which there is a concurrent colonic TB in two different regions of the large bowel.
Learning points.
Clinicians need to have gastrointestinal tuberculosis (TB) in their top diagnosis when dealing with patients with chronic gastrointestinal symptoms who are HIV-positive or coming from countries of high prevalence of TB.
Gastrointestinal TB is one of the known causes of hypertrophic lesions on the bowel wall mimicking malignancy.
Conservative management is successful in the majority of cases.
Footnotes
Contributors: RN and MN operated on the patient and GAD was the main writer of the manuscript and MN and RN supervised the whole process.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zumla A, Raviglione M, Hafner R, et al. Tuberculosis. N Engl J Med 2013;2013:745–55 [DOI] [PubMed] [Google Scholar]
- 2.Mukewar S, Mukewar S, Ravi R, et al. Colon tuberculosis: endoscopic features and prospective endoscopic follow-up after anti-tuberculosis treatment. Clin Transl Gastroenterol 2012;2013:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caws M, Thwaites G, Dunstan S, et al. The influence of host and bacterial genotype on the development of disseminated disease with Mycobacterium tuberculosis. PLoS Pathog 2008;2013:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radzi M, Rihan N, Vijayalakshmi N, et al. Diagnostic challenge of gastrointestinal tuberculosis: a report of 34 cases and overview of literature. Southeast Asian J Trop Med Public Health 2009;2013:505–10 [PubMed] [Google Scholar]
- 5.Falagas ME, Kouranos VD, Korterides P. Tuberculosis and malignancy. Q J Med 2010;2013:461–87 [DOI] [PubMed] [Google Scholar]


