Abstract
The occurrence of an acute myocardial infarction (MI) following a scorpion sting has been very rarely reported in the previous literature. Possible pathogenetic mechanisms include severe hypotension due to hypovolaemic shock and coronary spasm with subsequent thrombosis of coronary vessels developed after the release of vasoactive, inflammatory and thrombogenic substances contained in the scorpion venom. All of the previously reported cases had normal coronary angiogram. We report a case of a 65-year-old woman who presented with severe scorpion sting and was treated with prazosin. But a few hours later, she developed acute anterior wall MI. Coronary angiogram revealed the presence of significant stenosis in coronary arteries. As acute MI owing to significant coronary artery disease can be evident after severe scorpion envenomation, so every case of acute coronary syndrome following scorpion sting needs early diagnosis, thorough cardiovascular evaluation and appropriate treatment.
Background
Scorpion stings are common in tropical and subtropical regions of the world.1 Scorpion bites are common in our country, particularly in the rural areas.2 Among 86 species of scorpions present in India, Mesobuthus tumulus (Indian red scorpion) and Heterometrus swammerdami are of medical importance.2 In western India most cases of envenomation are following stings from M tamulus, while Heterometrus bengalensis is common in eastern India.1 Though local symptoms including severe pain and burning sensation at the site of sting are the most common manifestations, systemic complications can ensue.3 Cardiovascular manifestations are particularly prominent following stings by Indian red scorpion.2 Such bites infrequently have serious clinical sequelae, including myocardial infarction (MI), acute pulmonary oedema, cardiogenic shock and even death.3 Though all of the previous cases with MI following scorpion envenomation had normal coronary artery2–4 but we are reporting a case where obstructive coronary artery disease (CAD) with MI was evident following an episode of severe scorpion bite.
Case presentation
A 65-year-old woman presented in the emergency department with cold sweating and acute pain in her left ring finger a half an hour after being stung by a red scorpion. Her history was not significant and she had no predisposing cardiac risk factors like hypertension or diabetes. On examination, her blood pressure was 170/84 mm Hg, heart rate 130/min, regular and respiratory rate 18/min. She was treated with α-blocker prazosin. But 3–4 hours after treatment with prazosin, she developed chest discomfort and tightness and ECG showed sinus tachycardia with ST elevation in the anterior chest leads (figure 1). She was referred to our hospital for the management of acute anterior wall MI (AWMI). She was asymptomatic when she was admitted in our hospital and ECG showed features of evolved AWMI (figure 2). Serum cardiac enzymes were increased, and the level of creatine kinase (CK)-MB was 105 U/l and that of troponin-T was 0.628 ng/ml. Echocardiography demonstrated hypokinesia of interventricular septum and anterior and lateral wall and left ventricular ejection fraction (LVEF) 44%. Finally, coronary angiogram (CAG) was performed which revealed significant stenosis in left anterior descending (LAD) coronary artery (figure 3) and right coronary artery (RCA) (figure 4). She was treated with medications including dual antiplatelet drug, β-blockers, atorvastatin, sorbitrate and ramipril. Her admission course was smooth and she was discharged uneventfully 5 days later. She was planned to be on optimum medical management and if she becomes symptomatic then percutaneous coronary intervention to LAD/RCA was planned.
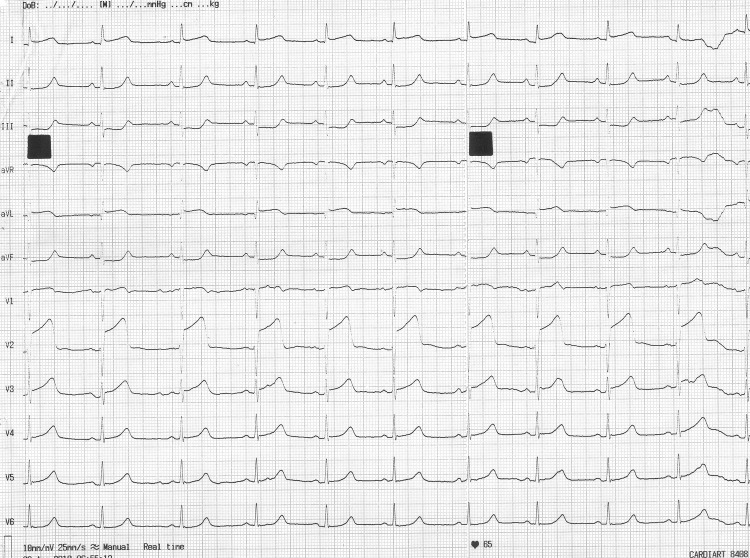
Figure 1.
ECG showed ‘ST’ elevation in the lead I, aVL, V2–V5.
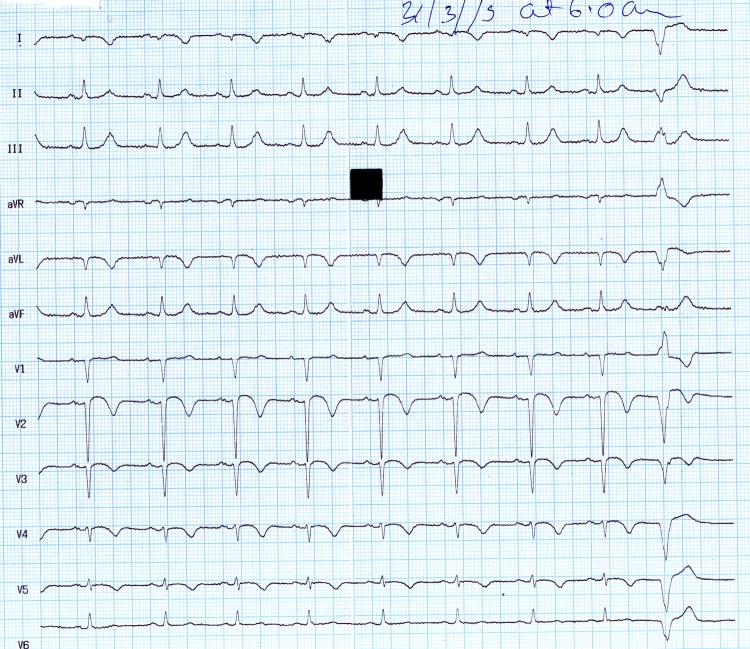
Figure 2.
ECG showed ‘ST’ elevation and ‘T’ inversion in the lead I, aVL, V2–V5.
Figure 3.
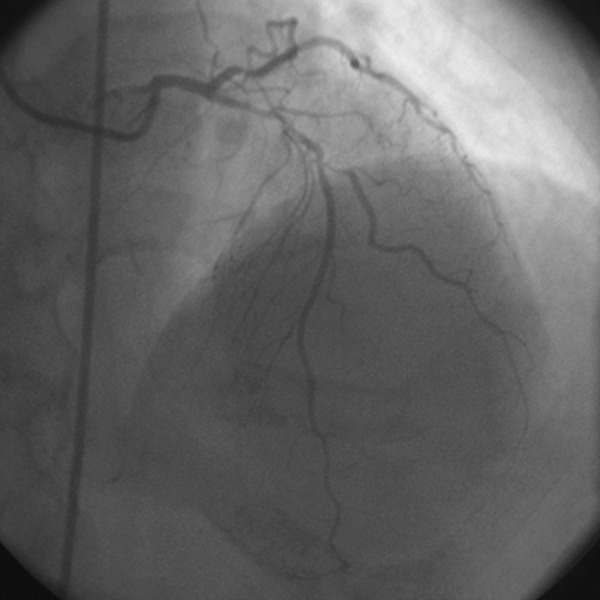
Coronary angiogram showed 70% stenois in the mid left anterior descending.
Figure 4.
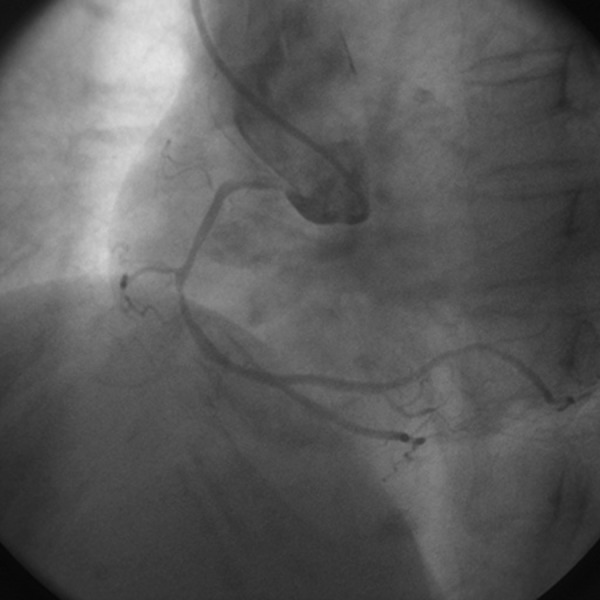
Coronary angiogram revealed 80% stenosis in the mid right coronary artery.
Outcome and follow-up
Patient was asymptomatic on medical treatment since her last visit after 1 month from the episode.
Discussion
The scorpion venom is a water soluble antigenic complex mixture of neurotoxin, cardiotoxin, nephrotoxin, haemolysins, phosphodiesterases, phospholipase, hyaluronidases, histamine and other chemicals.5 The venom can cause myocardial damage by several pathogenetic mechanisms.2 First, myocardial ischaemia caused by coronary spasm because of the release of vasoactive, inflammatory and thrombogenic peptides and amine constituents (histamine, serotonin, bradykinin, leukotrienes, thromboxane), which act on the coronary vasculature and induce coronary artery vasospasm and facilitate platelet aggregation as well as thrombosis.6 Second, direct cardiotoxic effect of the venom can cause toxic myocarditis by reduction of Na-K-ATPase and adrenergic myocarditis by releasing epinephrine and norepinephrine from neurons, ganglia and adrenals, thereby increasing myocardial oxygen demand by direct inotropic and chronotropic effect on the already compromised myocardial blood supply and third, the anaphylactic reaction caused by the release of allergenic proteins causes anaphylactic shock leading to hypotension with vasodilation and decrease of intravascular volume with reduced myocardial perfusion.7 8 Scorpion venom inhibits ACE, resulting in accumulation of bradykinin, which is implicated in the development of pulmonary oedema2 but it was not seen in our case. In our patient, the findings suggestive of AWMI (including clinical symptoms, dynamic changes of ECG, elevated cardiac enzymes and regional wall motion abnormality) was due to obstructive CAD with plaque rupture being the most probable mechanism rather than coronary vasospasm as CAG demonstrated significant lesion in the coronary artery. Acute myocardial infarction occurs very rarely after a scorpion envenomisation.2–8 There are a few cases of AMI due to bee or scorpion bites reported in the literature.1–8 Most of those cases had normal coronary artery. But in our case, acute MI was due to significant CAD which was evident following scorpion sting reaction. The most possible mechanism for MI in our case could be atherosclerotic plaque rupture following sympathetic over activity owing to scorpion bite. So every case with features of acute coronary syndrome following scorpion sting, thorough cardiological evaluation and CAG is to be performed to rule out the presence of any significant CAD.
Learning points.
Prazocin is the drug of choice following scorpion bite especially if patient had symptoms like accelerated hypertension, profuse sweating due to excessive adrenergic surge.
Underlying obstructive coronary artery disease can be evident after scorpion bite as acute myocardial infarction.
Any patient of scorpion bite who presents with acute coronary syndrome, a thorough cardiological evaluation including coronary angiogram is needed.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cvetković-Matić D, Asanin M, Matić D, et al. Acute myocardial infarction following a hornet sting. Vojnosanit Pregl 2009;2013:333–7 [DOI] [PubMed] [Google Scholar]
- 2.Maheshwari M, Tanwar CP. Scorpion bite induced myocardial damage and pulmonary edema. Heart Views 2012;2013:16–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korantzopoulos P, Kountouris E, Voukelatou M, et al. Acute myocardial infarction after a European hornet sting–a case report. Angiology 2006;2013:383–6 [DOI] [PubMed] [Google Scholar]
- 4.Wagdi P, Mehan VK, Bürgi H, et al. Acute myocardial infarction after wasp stings in a patient with normal coronary arteries. Am Heart J 1994;2013:820–3 [DOI] [PubMed] [Google Scholar]
- 5.Karnad DR. Haemodynamic patterns in patients with scorpion envenomation. Heart 1998;2013:485–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bahloul M, Kallel H, Rekik N, et al. Cardiovascular dysfunction following severe scorpion envenomation. Mechanisms and physiopathology. Presse Med 2005;2013:115–20 [DOI] [PubMed] [Google Scholar]
- 7.Lombardi A, Vandelli R, Cerè E, et al. Silent acute myocardial infarction following a wasp sting. Ital Heart J 2003;2013:638–41 [PubMed] [Google Scholar]
- 8.Calveri G, Bertelli Y, Caico SI, et al. Acute myocardial infarction after wasp sting. Ital Heart J Suppl 2002;2013:555–7 [PubMed] [Google Scholar]