Abstract
A woman presented with 75% stenosis of the right internal carotid artery (ICA) with extension to the origin of a persistent hypoglossal artery (PHA). The PHA is a rare fetal variant of carotid–basilar anastomosis that elevates the risk of ischemia and embolic infarction within the posterior cerebral circulation in patients with carotid disease proximal to the anastomosis. Our case is highly unique because of the extremely rare nature of the PHA with associated ICA stenosis that extended to the PHA. Additionally, a novel treatment approach was employed by stenting and angioplasty while protecting both the anterior and posterior cerebral circulations.
Keywords: Atherosclerosis, Embolic, Intervention, Stent
Background
The persistent hypoglossal artery (PHA) is one of the five carotid anastomoses that develop between the embryonic internal carotid arteries (ICAs) of the anterior cerebral circulation and bilateral longitudinal neural arteries of the posterior cerebral circulation. It rarely persists at birth.1 If the anastomosis fails to regress during embryonic development, normal formation of the posterior communicating arteries and the vertebral arteries is impaired. Therefore, a PHA can serve as the major supplier of the posterior cerebral territories.
The current case satisfies all of the diagnostic criteria,2 3 and therefore the presence of a PHA was an important factor in planning treatment for the severe right ICA stenosis.
In this report, we present the unique case of a patient with a symptomatic severe ICA stenosis extending to involve the origin of the ipsilateral PHA. Although there are a few reports describing the use of carotid endarterectomy (CEA) for the treatment of stenoses extending into the PHA,4 5 this is the first reported case of treatment using carotid artery stenting (CAS), with placement of two distal protection devices within the distal ICA and distal PHA. Here we discuss our strategy and its benefit in the treatment of high risk ICA stenoses in the presence of a PHA.
Case presentation
A 63-year-old woman with a past medical history significant for hyperlipidemia and tobacco abuse presented to our hospital with left upper extremity parasthesia. She had a 13 year history of intermittent numbness and weakness involving the left upper extremities but her symptoms had increased in frequency in the 2 weeks prior to her hospitalization. Additionally, the patient reported a 7 year history of right-sided pulsatile tinnitus but denied additional symptoms and was neurologically intact on admission.
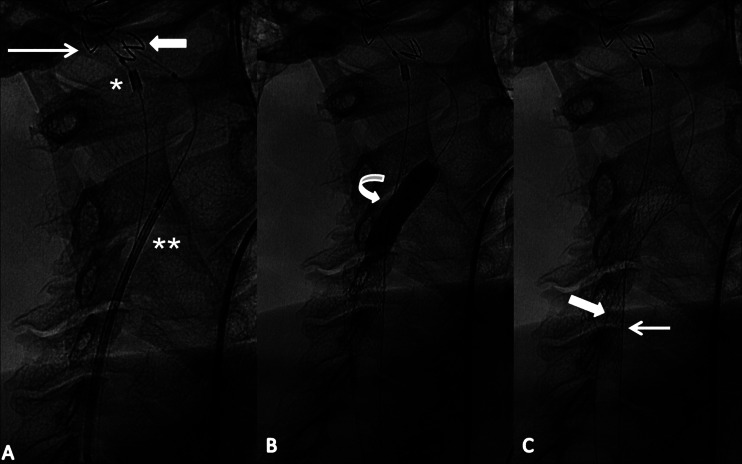
Carotid duplex ultrasonography indicated a right ICA stenosis that was further characterized using CT angiograms of the head and neck and digital subtraction angiography (DSA). The examinations showed a calcified atherosclerotic plaque in the right ICA and the right carotid bifurcation causing 75% stenosis (measured according to North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria). The stenosis extended 1.8 cm above the carotid bifurcation to the origin of a PHA. The PHA arose from the ICA at the C2 vertebral body level and continued to the intracranial cavity anterior to the right occipital condyle (figure 1). It merged with the left vertebral artery to form the basilar artery, and formed the dominant supply to the posterior circulation.
Figure 1.
(A) Cone beam CT image shows a persistent right hypoglossal artery (arrow) arising from the internal carotid artery (block arrow) at the level of C2 which merges with the left vertebral artery to form the basilar artery (small arrows). (B) Digital subtraction angiography shows a 75% symptomatic stenosis of the right internal carotid artery in the setting of persistent hypoglossal artery (curved arrow).
Due to the high location of the stenosis at the skull base and the finding of the PHA, CAS was chosen over a surgical intervention. CAS was seen as more technically feasible and safer because it allowed for protection of the anterior and posterior circulations using distal protection devices.
Treatment
CAS using two distal protection devices was performed under general anesthesia. Bilateral groins were prepped and draped in a sterile fashion, and accessed using a modified Seldinger technique.
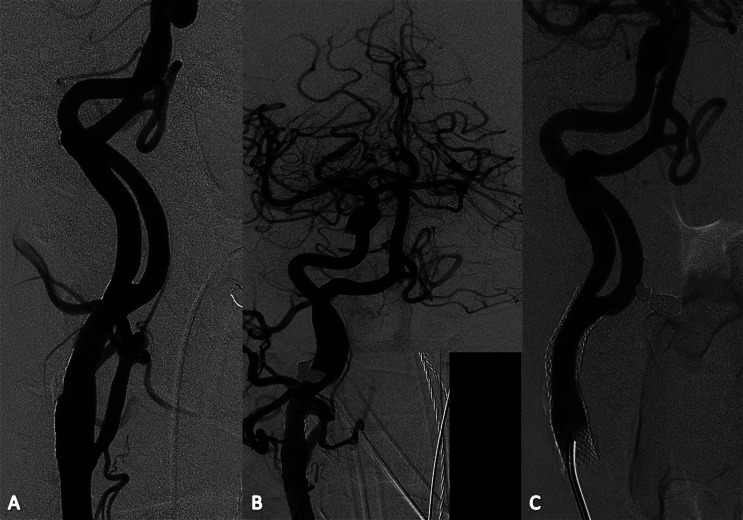
Following the diagnostic angiography, 5 F and 6 F Envoy catheters were both advanced into the right common carotid artery. Two Emboshield protective devices (Abbott, Abbott Place, Illinois, USA) were placed in the right ICA and PHA, respectively. Following proper device placement, the Emboshield re-sheathing catheter was introduced proximal to the protection device in the PHA. An 8×40 mm Precise stent (Cordis, Miami Lakes, Florida, USA) was deployed in the right ICA, thereby jailing the re-sheathing catheter of the distal protection device in the PHA (figure 2).
Figure 2.
(A) Fluoroscopic spot image shows the position of both cerebral embolic protection devices within the hypoglossal artery (arrow) and the right internal carotid artery (block arrow) distal to the stenosis. The catheter to re-capture the first embolic protection device has already been advanced close to the tip (*) while the wire of the second embolic protection device is used for advancing the stent delivery system (**). (B) Balloon angioplasty was performed following stent placement to treat the remaining waste within the stent (curved arrow). (C) Fluoroscopic spot image following angioplasty shows a fully open stent. The wire carrying the embolic protection device and the re-capture catheter has been jailed by the stent within the hypoglossal artery (arrow). The wire of the second embolic protection device used for the delivery of the stent passes through the lumen of the deployed stent (block arrow).
A follow-up angiogram following stent placement revealed residual narrowing and thus balloon angioplasty was performed using a Sterling Monorail balloon dilation catheter (Boston Scientific, Natick, Massachusetts, USA). After completing the procedure, the first protection device behind the stent was removed from the PHA after re-sheathing followed by removal of the second embolic protection device through the stent. A final angiogram of the stented ICA and the intracranial circulation was obtained. Catheters were removed and hemostasis was achieved at the common femoral artery access sites. The two distal protection devices were submitted for pathological analysis to determine if any emboli were shed during the procedure.
Outcome and follow-up
Stent revascularization was successfully performed without complications. A repeat angiogram following balloon angioplasty showed complete opening of the high grade stenosis (figure 3). There was excellent blood flow observed within the stented right ICA and distal to the stented vessel segment.
Figure 3.
(A) Carotid artery follow-up angiography shows complete revascularization and (B) excellent intracranial blood flow to the right hemisphere and posterior circulation. (C) Six month follow-up angiography shows smooth intimal coverage of the stent and no re-stenosis.
The distal protection devices were placed in formalin and microscopically examined for emboli. There was no material identified in the protection device placed in the PHA. Analysis of the device placed in the right ICA showed that multiple 0.2×0.1×0.1 cm fragments and a blood clot were collected by the protection device.
The patient tolerated the procedure well, and the hospital course was uneventful. She had no complaints and remained neurologically and physically intact. After 6 months, the patient was seen for follow-up digital subtraction angiography (figure 3). No significant intimal hyperplasia or major residual stenosis could be detected. The stented vessel segment remained entirely patent.
The patient has been asymptomatic since the intervention.
Discussion
Previously, the successful use of a single distal protection device was reported in a patient with sufficient length between the ICA stenosis and the PHA origin.6 Although there are reports that find no statistically significant difference in the efficacy of flow arrest using proximal balloon occlusion versus the use of distal filter embolic protection devices,7 flow arrest by use of balloon occlusion devices does so at the expense of constant procedural cerebral perfusion and may not be tolerated in patients with decreased cerebral vascular reserve, incomplete circle of Willis and/or high grade stenosis of the contralateral ICA.8 There are a few reports in which emboli traveling through the PHA have been noted to cause infarctions.9 10
Current treatment options for ICA stenoses extending near or beyond the bifurcation into the PHA or for stenoses of the PHA itself include balloon angioplasty, CEA and CAS, with the use of proximal flow arrest or distal filter embolic protection devices.6 11 12
CEA in our case would have involved plaque removal from both the ICA and PHA and the risks of complications to a hemodynamically sensitive area. Unlike CEA, treatment with CAS has been shown to be an appropriate choice for patients in surgically difficult areas, such as high located plaques.13 The use of CEA may require difficult shunt placement and lengthy occlusion times, while CAS with proximal flow arrest reduces occlusion time, offering protection against ischemic events.11 In cases such as ours, in which the vertebrobasilar system is dependent on the blood flow from the ICA, CEA with flow arrest may interfere with the blood flow to the posterior circulation from the ICA.14 In addition, CAS allows for the use of protection devices to prevent emboli from entering the posterior cerebral circulation.
Currently, the use of distal filter embolic protection devices is the preferred method of distal embolic protection.7 However, in cases in which the stenosis is immediately proximal to the origin of the PHA, the use of a distal embolic protection device may be difficult because of the tortuousity of the vessels.6 15
Learning points.
CAS involving the ICA and the origin of the PHA presented a challenge for distal embolic protection and the necessity to protect both vessels from emboli.
The significant decrease in carotid blood flow associated with a stenotic carotid artery potentially places both the ipsilateral anterior and posterior circulations under ischemia.9
The inadequate hemodynamic flow to the posterior circulation due to the presence of a PHA results in poor collateral circulation, further increasing the risk of ischemia.
By jailing one of the protection devices during stent deployment, it was possible to protect the anterior and posterior cerebral circulations.
Footnotes
Contributors: AKW: design and concept, and critical revision of the manuscript for important intellectual content. CFS, SYH and ALK: writing the first draft of the manuscript. CFS, SYH and ALK: literature research. All authors approved the final version of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Padget DH. The development of the cranial arteries in the human embryo. Contrib Embryol 1948;2013:205–62 [Google Scholar]
- 2.Lie A. Congenital anomalies of the carotid arteries. Amsterdam: Excerpta Medica Foundation, 1968:70–5 [Google Scholar]
- 3.Brismar J. Persistent hypoglossal artery, diagnostic criteria. Acta Radiol Diagn 1976;2013:160–6 [DOI] [PubMed] [Google Scholar]
- 4.Megyesi JF, Findlay JM, Sherlock RA. Carotid endarterectomy in the presence of a persistent hypoglossal artery: case report. Neurosurgery 1997;2013:669–72 [DOI] [PubMed] [Google Scholar]
- 5.Cartier R, Cartier P, Hudan G, et al. Combined endarterectomy of the internal carotid artery and persistent hypoglossal artery: an unusual case of carotid revascularization. Can J Surg 1996;2013:159–62 [PMC free article] [PubMed] [Google Scholar]
- 6.Nii K, Aikawa H, Tsutsumi M, et al. Carotid artery stenting in a patient with internal carotid artery stenosis and ipsilateral persistent primitive hypoglossal artery presenting with transient ischemia of the vertebrobasilar system. Neurol Med Chir 2010;2013:921–4 [DOI] [PubMed] [Google Scholar]
- 7.Zahn R, Ischinger T, Mark B, et al. Embolic protection devices for carotid artery stenting. J Am Coll Cardiol 2005;2013:1769–74 [DOI] [PubMed] [Google Scholar]
- 8.MacDonald S. Is there any evidence that cerebral protection is beneficial? J Cardiovasc Surg 2006;2013:127–36 [PubMed] [Google Scholar]
- 9.Pyun HW, Lee DH, Kwon SU, et al. Internal carotid artery stenosis with ipsilateral persistent hypoglossal artery presenting as a multiterritorial embolic infaraction: a case report. Acta Radiol 2007;2013:116–18 [DOI] [PubMed] [Google Scholar]
- 10.Conforto AB, Souza M, Puglia P, et al. Bilateral occipital infarcts assoaciated with carotid atherosclerosis and persistent hypoglossal artery. Clin Neurol Neurosurg 2007;2013:364–7 [DOI] [PubMed] [Google Scholar]
- 11.Kanazawa R, Ishihara S, Okawara M, et al. A successful treatment with carotid arterial stenting for symptomatic internal carotid artery severe stenosis with ipsilateral persistent primitive hypoglossal artery: case report and review of the literature. Minim Invas Neurosurg 2008;2013:298–302 [DOI] [PubMed] [Google Scholar]
- 12.Polo M, Chiu D, Klucznik R, et al. Intracranial stenting of a persistent primitive artery in a patient presenting with acute bilateral posterior circulation infarcts. J Neurointervent Surg 2011;2013:A38–9 [Google Scholar]
- 13.Yadav JS, Wholey MH, Kuntz RE, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004;2013:1493–501 [DOI] [PubMed] [Google Scholar]
- 14.Paraskeva GK, Tsitsopoulos PP, Papaziogas B, et al. Persistent primitive hypoglossal artery: an incidental autopsy finding and its significance in clinical practice. Folia Morphol 2007;2013:143–7 [PubMed] [Google Scholar]
- 15.Al-Mubarak N, Colombo A, Gaines PA, et al. Multicenter evaluation of carotid artery stenting with a filter protection system. J Am Coll Cardiol 2002;2013:841–6 [DOI] [PubMed] [Google Scholar]