Abstract
Intramural gas in stomach is a rare finding, but differential diagnosis of this condition into gastric emphysema and emphysematous gastritis is clinically important because of vastly different aetiologies and prognosis. Emphysematous gastritis is caused by gas producing micro-organisms inside the stomach wall and is a potentially fatal condition, while, on the other hand, gas enters stomach wall through mucosal breach in the case of gastric emphysema and prognosis is usually good with complete resolution. To date, no case has been reported in the literature showing gas in the stomach wall in a patient with acute calculus cholecystitis. We present a case of a young man with upper abdominal pain, and who, upon diagnostic work up was diagnosed with acute calculus cholecystitis with associated intramural gas in the stomach with no known aetiological factors to be positive. Conservative management with close observation resulted in complete symptomatic resolution.
Background
Intramural gas is a rare entity; there is no case in the literature to date reporting spontaneous intramural air of the stomach and its association with acute calculus cholecystitis.
Case presentation
The patient was a 31-year-old gentleman with no previously known comorbid conditions, who presented to us with upper abdomen pain of 6 h duration. It was acute onset, sharp pain, more towards right hypochondrium with no association. History was unremarkable regarding upper gastrointestinal symptoms or any upper gastrointestinal medical procedures. There was no history of trauma to the upper abdomen. On examination, blood pressure was 140/80 mm Hg, pulse was 100 beats/min, respiratory rate was 20 breath/min, afebrile and was maintaining 100% oxygen saturation on room air. General physical examination, as well as systemic examination, was unremarkable except that the patient had right hypochondrium tenderness with positive Murphy's sign. The patient's medical, surgical and family histories were unremarkable.
Investigations
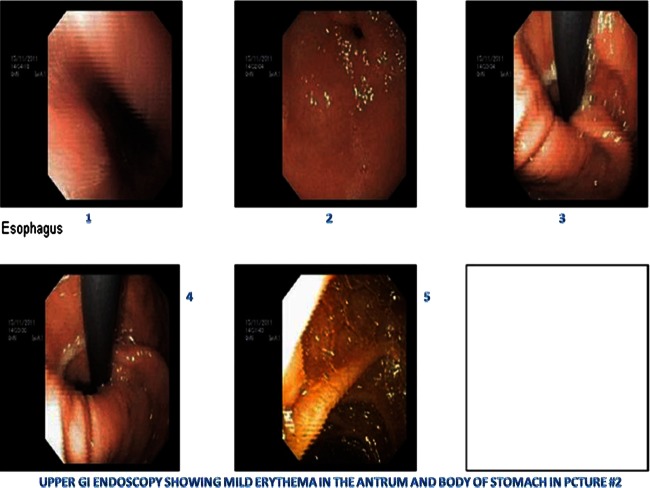
A laboratory workup showed thin-layer chromatography (TLC) of 11.1×109/l with neutrophil count of about 79%. Liver function tests (LFTs) reveal a total bilirubin of 1.4 mg/dl with direct component of 1 mg/dl, alanine transaminase/ aspartate aminotransferase was normal, alkaline phosphate was slightly higher with 100 IU/l and γ GT was 40 IU/l. Ultrasound abdomen showed a slightly thick-walled gallbladder with a gallstone near the neck. Otherwise, ultrasonographic findings were unremarkable. The ultrasound was inconclusive to rule out cholecystitis. A CT scan of the abdomen was done to further evaluate the cause of pain. It showed mildly enhancing thick-walled gallbladder with minimal peri-cholecystic fluid. Two calculi measuring 16 and 5 mm were seen in the lumen of gallbladder. These radiological appearances were suggestive of acute cholecystitis. Incidental finding was thin streaks of air specks in non-dependent fundal region of stomach, representing intramural air (Figures 1–3). On delay images and prone cuts, air specks persist. Otherwise, stomach appeared unremarkable with no evidence of mass lesion or abnormal thickening as shown in figure 1. Oesophagogastroduodenoscopy (EGD) done to further evaluate intramural gastric air was unremarkable except mild erythema of body and antrum of stomach (Figures 4–8). Histopathology of the biopsy specimen taken at the time of endoscopy revealed mild chronic non-specific inflammation.
Figure 1.
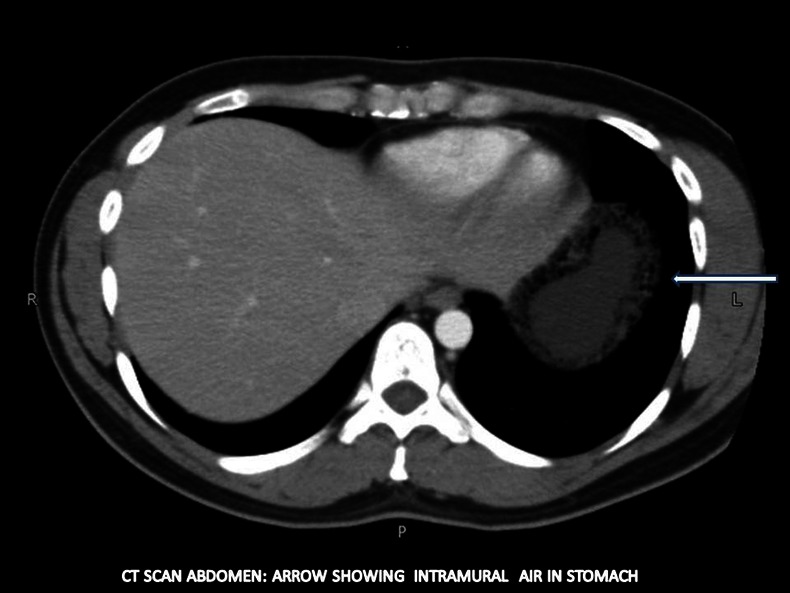
CT scan abdomen: (arrow) showing intramural air in stomach.
Figure 2.

CT scan abdomen: showing intramural air in the fundal part (dependent and non-dependent) of the stomach.
Figure 3.
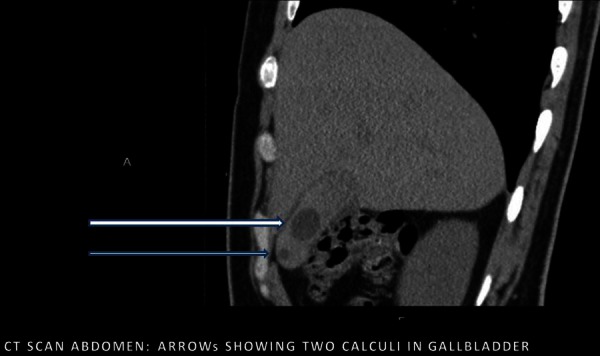
CT scan abdomen: (arrows) showing two calculi in gallbladder.
Figure 4.
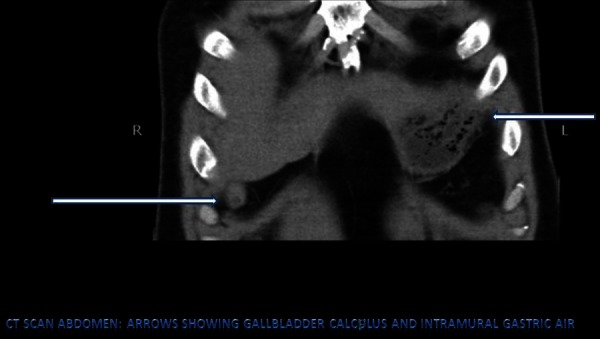
CT scan abdomen: (arrows) showing gallbladder calculas and intramural gastric air.
Figure 5.
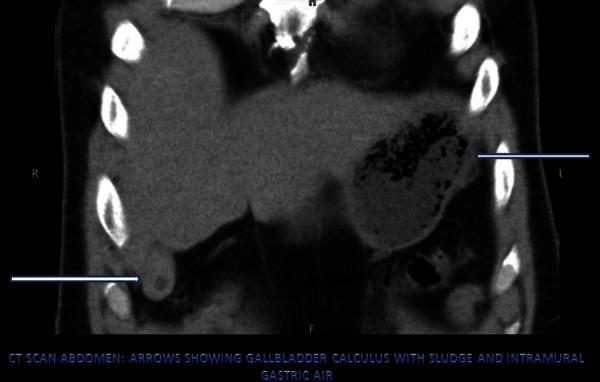
CT scan abdomen: (arrows) showing gallbladder calculas with sludge and intramural gastric air.
Figure 6.

CT scan abdomen: (arrows) showing gallbladder calculas with sludge and intramural gastric air.
Figure 7.
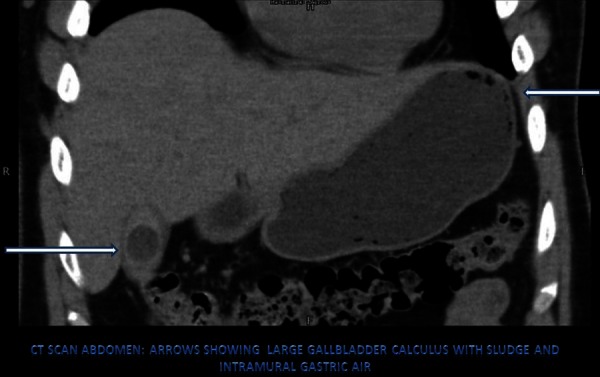
CT scan abdomen: (arrows) showing large gallbladder calculas with sludge and intramural gastric air.
Figure 8.
Upper gastrointestinal endoscopy showing mild erythema in the antrum and body of the stomach.
Differential diagnosis
Acute cholecystitis
Gastric emphysema
Emphysematous gastritis
Treatment
The patient was kept NPO; intravenous fluids along with intravenous antibiotics were started. The patient was advised for laparoscopic cholecystectomy, but the patient refused and preferred to be managed conservatively. The patient also underwent EGD to further evaluate intramural gastric air, and biopsy was taken at the time of endoscopy.
Outcome and follow-up
Pain resolved in 24 h, with the normalisation of TLC (5.4×109/l) and LFT's. He was discharged home on antibiotics and proton pump inhibitors. Clinical follow-up showed complete resolution of symptoms.
Discussion
Intramural air in the stomach is a relatively rare radiological finding, as stomach is reported to be least common site to have intramural gas.1 Differential diagnosis includes two conditions, viz emphysematous gastritis and gastric emphysema. Pathogenesis of the two conditions is different. Emphysematous gastritis is a potentially fatal condition that results from gas-producing micro-organisms in the stomach wall. The patients suffering from this condition are toxic and may have signs of systemic involvement.2 On the other hand, gastric emphysema also known as gastric pneumatosis results from air entering the stomach wall from outside.2 It may be intraluminal air entering the stomach wall from gastric lumen through the disruption of mucosa. This disruption may be caused by either iatrogenic injury during upper gastrointestinal procedures like endoscopy3 or nasogastric tube placement4 or by increased intraluminal pressure secondary to pyloric or enteral stenosis.5 Gastric paresis is also known to be associated with gastric emphysema.6 Forceful vomiting and chest wall injuries can also result in this condition. To date, there is no case in literature reporting gastric emphysema associated with acute cholecystitis. Differential diagnosis of intramural gas in the stomach is important because of completely different management and prognosis of the two conditions. These two conditions can be distinguished on the basis of clinical picture and radiographical appearances; those who suffer from emphysematous gastritis usually have very sick look, while gastric emphysema is usually asymptomatic or causes mild symptoms like dyspepsia and epigastric discomfort. Plain radiographs usually pick up intramural gas of the stomach as linear small gas bubbles in gastric wall. Gastric emphysema has more linear and streak-like gas bubbles. Emphysematous gastritis may be associated with gas in the portal venous system as well.7 Different radiological appearances on CT scan can help differentiate the two conditions. Gastric emphysema usually has a characteristic linear pattern of lucent areas in thin-walled gastric wall, while on the other hand lucent areas in the form of bubbles are found in emphysematous gastritis along with thickened gastric mucosa and gas in portal venous system.7 CT abdomen is the most commonly used investigation for the differential diagnosis.8 EGD and biopsy for histopathology and culture of the tissue help in finding out the aetiology of the condition.9 Gastric emphysema can be managed conservatively with close observation.10 Complete resolution with conservative management has been reported in literature11 as in our case. There is no case in the literature to date reporting spontaneous intramural air of the stomach or its association with acute calculus cholecystitis.
In our case, the patient was clinically stable with no signs of systemic involvement. A CT scan of the abdomen demonstrated thin streaks of intramural air in stomach. Based on these features, diagnosis of gastric emphysema was made. Complete symptomatic resolution on clinical follow-up after conservative management also favour's our diagnosis. Thorough clinical evaluation and aetiological work up including EGD did not show any known risk factor association so it was labelled as idiopathic intramural gastric air.
Learning points.
Intramural air can be associated with acute cholecystitis.
Thorough workup should be done before labelling it as benign condition, that is, gastric emphysema.
It can be managed conservatively.
Footnotes
Contributors: ZGN conceptualised this case report and also contributed to the writing of the manuscript. NS did the literature search and added to the discussion part. ARA contributed by writing down the management part and supervised the overall activity. MSE reviewed and finalised the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Arezzo A, Famiglietti F, Garabello D, et al. Complete resolution of emphysematous gastritis after conservative management. Clin Gastroenterol Hepatol 2011;2013:e30. [DOI] [PubMed] [Google Scholar]
- 2.Nasr D, Bernard P, Basile N. [Emphysematous gastritis]. J Chir (Paris) 2007;2013:439–40 [DOI] [PubMed] [Google Scholar]
- 3.Hyun YS, Han DS, Lee HL, et al. Gastric emphysema after endoscopic submucosal dissection. Endoscopy 2011;2013(Suppl 2 UCTN):E83–4 [DOI] [PubMed] [Google Scholar]
- 4.Zenooz NA, Robbin MR, Perez V. Gastric pneumatosis following nasogastric tube placement: a case report with literature review. Emerg Radiol 2007;2013:205–7 [DOI] [PubMed] [Google Scholar]
- 5.Lim RK, McKillop S, Karanicolas PJ, et al. Massive gastric pneumatosis from pyloric stenosis. CMAJ 2010;2013:E227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gutiérrez Andreu M, Otero Perpiñá B, Muñoz C, et al. [Gastric pneumatosis secondary to a pyloric stenosis of peptic origin]. Cir Esp 2011;2013:188. [DOI] [PubMed] [Google Scholar]
- 7.Paul M, John S, Menon MC, et al. Successful medical management of emphysematous gastritis with concomitant portal venous air: a case report. J Med Case Rep 2010;2013:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson PT, Horton KM, Edil BH, et al. Gastric pneumatosis: the role of CT in diagnosis and patient management. Emerg Radiol 2011;2013:65–73 [DOI] [PubMed] [Google Scholar]
- 9.Krier M, Jeffrey R Brooke, Jr, Banerjee S. Troubles with stomach bubbles? Or not? Dig Dis Sci 2009;2013:919–21 [DOI] [PubMed] [Google Scholar]
- 10.McLaughlin SA, Nguyen JH. Conservative management of nongangrenous esophageal and gastric pneumatosis. Am Surg 2007;2013:862–4 [PubMed] [Google Scholar]
- 11.Iqbal M, Ishtiaq O, Akhtar A, et al. Empysematous gastritis Shifa College of Medicine, Islamabad. J Pak Med Assoc 2006;2013:605–7 [PubMed] [Google Scholar]