Summary
Carotid artery pseudoaneurysm is a rare complication from placement of an internal jugular triple lumen catheter. Endovascular stenting is the favored treatment option in the setting of traumatic carotid injury. In other parts of the body, specifically the femoral artery, thrombin injection has become the standard of care. We intend to show that effective management of carotid pseudoaneurysms can also be achieved with thrombin injection after placement of a distal embolic protection device.
Key words: percutaneous thrombin injection, common carotid artery pseudoaneurysm, distal embolic protection device
Introduction
Arterial puncture of the carotid artery is a known complication in placement of internal jugular triple lumen catheters (IJ TLC) with low reported rates of occurrence 1.
Carotid artery pseudoaneurysm is a rare complication. Endovascular therapy, specifically carotid stenting, is the favored treatment option in the setting of traumatic carotid artery injury 2,3. With femoral artery pseudoaneurysms, thrombin injection has become the standard of care 4. We intend to show that effective management of carotid pseudoaneurysms can also be achieved with thrombin injection after placement of a distal protection device.
Case Report
A 78-year-old man with a medical history of congestive heart failure, coronary artery disease status-post stenting, and chronic obstructive pulmonary disease was undergoing outpatient evaluation for gross hematuria when he was found to be acutely anemic. He was admitted to our institution and urgent workup revealed a renal cell carcinoma.
The patient's antiplatelet therapy for his coronary artery stent was discontinued. Prior to radical nephrectomy, the patient developed acute respiratory distress requiring emergent placement of an IJ TLC.
An Arrow 7-Fr IJ TLC catheter (Teleflex Medical. Research Triangle Park, North Carolina, USA) was placed without ultrasound guidance. The catheter remained in place for several hours until it was noted on routine blood draw that the catheter was inadvertently placed in the right common carotid artery (CCA). The catheter was immediately removed and direct pressure was held for 20 minutes. Over the next 48 hours, the patient developed right-sided neck swelling at the puncture site.
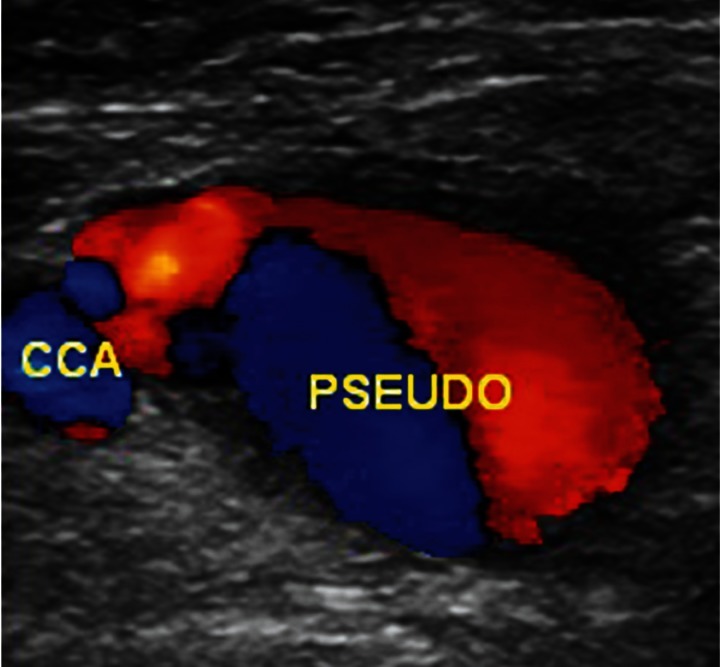
CT scan without contrast demonstrated an enlarged soft tissue density at the base of the right neck (Figure 1). Doppler ultrasound demonstrated a narrow neck 5cm pseudoaneurysm in the proximal right CCA (Figure 2).
Figure 1.
Non-contrast axial CT image demonstrates an enlarging soft tissue mass in the right neck.
Figure 2.
Doppler ultrasound demonstrates a right common carotid artery pseudoaneurysm with a 5-mm narrow neck.
Treatment
Institutional Review Board approval is not required for case reports detailing a single patient. Informed consent for diagnostic angiography and percutaneous treatment was obtained.
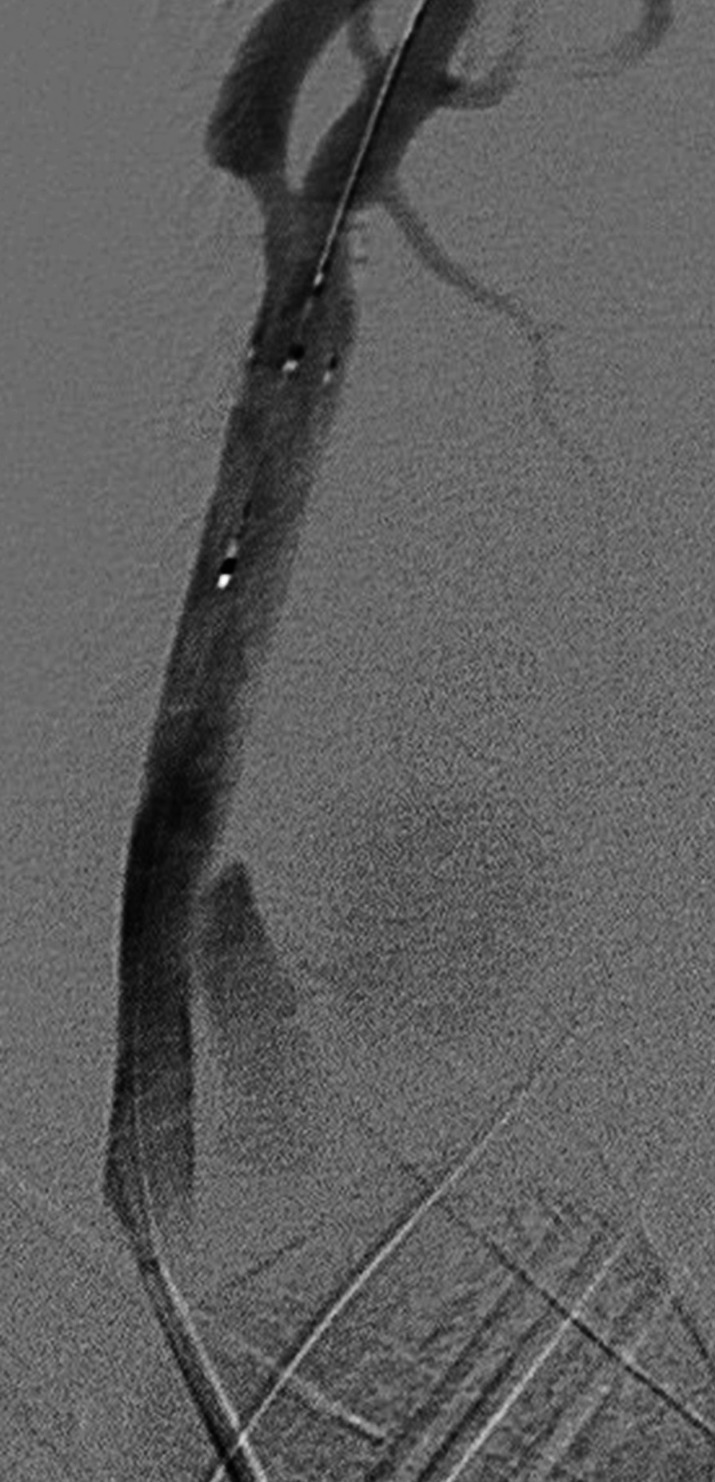
An angiogram was performed to further evaluate the pseudoaneurysm. The right CCA was selected and angiography demonstrated a 5 cm pseudoaneurysm with a narrow neck (Figure 3). The intracranial portion of the injection showed predominant supply to the right middle cerebral artery with an incomplete circle of Willis.
Given the small pseudoaneurysm neck, percutaneous thrombin injection was decided as the preferred treatment option and placement of a distal protection device was deemed necessary to prevent distal thromboembolism. An Acculink 6.5 mm embolic protection device (Abbott Laboratories. Abbott Park, Illinois, USA) was deployed distal to the pseudoaneurysm neck (Figure 4).
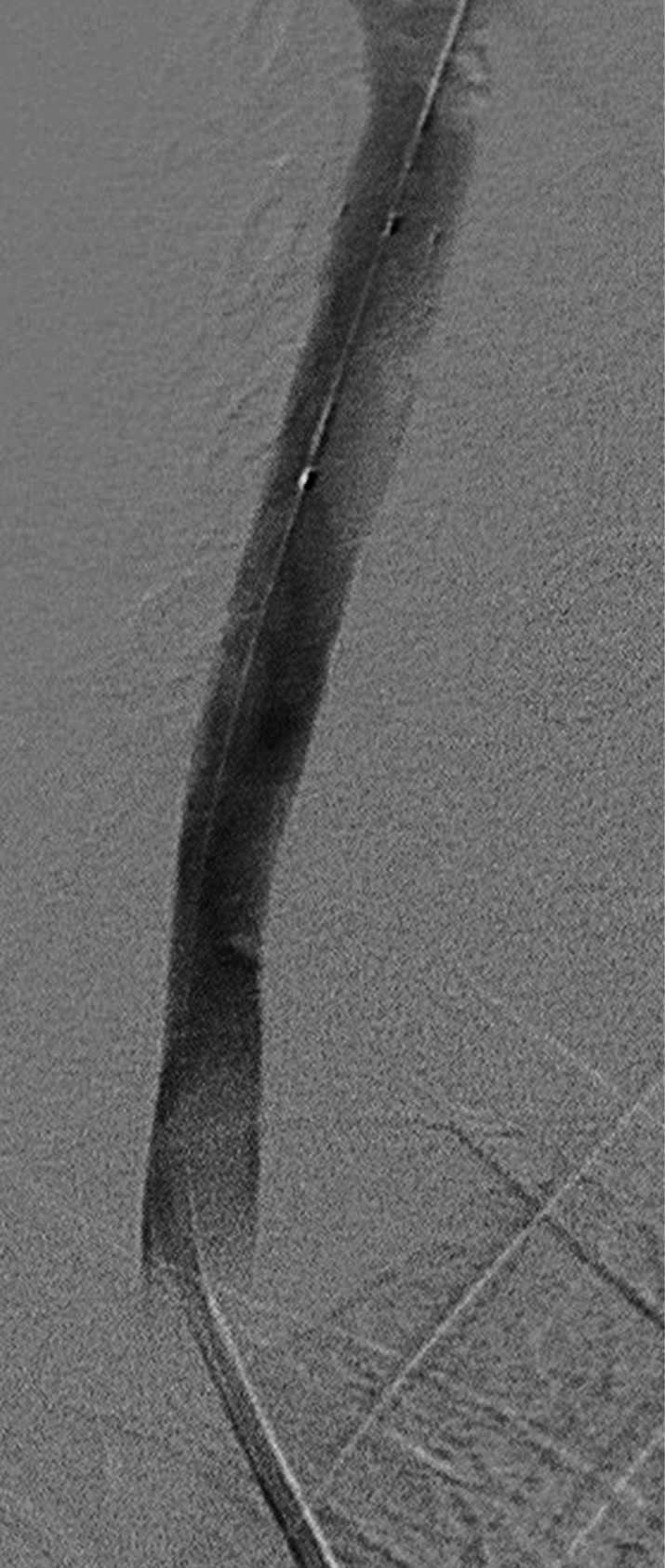
After sterile preparation and under ultrasound guidance, a 25-gauge needle was used to directly puncture into the medial aspect of the right CCA pseudoaneurysm. A total of 200 U of thrombin was slowly injected into the pseudoaneurysm under duplex imaging and complete thrombosis was instantaneously achieved. Subsequent angiogram demonstrated complete occlusion of the pseudoaneurysm and patency of the right carotid system (Figure 5). The distal protection device was closed and retrieved revealing capture of a 2 mm thrombus.
The patient tolerated the procedure well and follow-up ultrasound three days following the procedure again demonstrated complete occlusion of the pseudoaneurysm. There were no symptoms of stroke or complications from either the pseudoaneurysm or the procedure during the patient's month long hospitalization. The patient was maintained on short-term two-week anti-platelet therapy without evidence of recurrent hematuria or bleeding. The patient passed away one year later secondary to his metastatic disease and other comorbidities.
Figure 3.
Selective angiogram demonstrates a narrow neck 5-cm pseudoaneurysm projecting medially from the proximal right common carotid artery.
Figure 4.
Status post deployment of distal embolic protection device distal to the pseudoaneurysm.
Figure 5.
Selective angiogram demonstrating complete occlusion of the pseudoaneurysm with preservation of patency of the right carotid system.
Discussion
Carotid artery punctures are a known complication of IJ TLC placement with an occurrence rate of 3% 1. However, effective hemostasis after arterial puncture can be adequately achieved with manual compression if identified upon initial puncture. Therefore, pseudoaneurysm of the CCA is a rare complication after placement of an IJ TLC. In our case, the arterial puncture was not noticed prior to placement of the IJ TLC.
Two options are available for treatment of carotid pseudoaneurysms: open surgery and endovascular surgery. Open surgery for traumatic injuries of the internal carotid artery has reported mortality rates up to 22% and postoperative stroke rates up to 21% 2. For internal carotid artery pseudoaneurysms, increased mortality rates are observed in up to 30% of cases in open surgery and there is a high incidence of reported cerebral complications.
In contrast, endovascular treatment is relatively safe with most treatment performed using stent placement. The reported mortality rates with stent placement are 0.9% and the postoperative stroke rates are between 3.5 and 4.7% 2,3. While there is no consensus on the need and type of adjunctive anticoagulation, patients are generally maintained on anti-platelet therapy for several months following the procedure. There has also been reported inherent loss of intraluminal vessel diameter following stent placement 2,3. Maintenance anti-platelet therapy was not ideal for our patient given the presence of acute anemia secondary to hematuria. Furthermore, the patient's anti-platelet regimen for his coronary artery stent had already been discontinued earlier in his admission. The potential for inherent loss of intraluminal vessel diameter was also a concerning complication given the insufficient collateral vascular supply from the contralateral internal carotid artery. Therefore, an alternate treatment method, in our case percutaneous thrombin injection, was considered.
Thrombin injection has become the preferred treatment method of femoral artery pseudoaneurysms 4. With percutaneous treatment of iatrogenic femoral pseudoaneurysms after thrombin injection there is a positive correlation between successful treatment of pseudoaneurysms and size smaller than 6 cm but there is no correlation with pseudoaneurysm neck size 6. Our patient's 5cm pseudoaneurysm was well within the range of treatable size. While there was no correlation between neck size and success rates, the small pseudoaneurysm neck promoted our usage of thrombin. Furthermore, given that thrombin injection results in almost instantaneous thrombus formation under real-time ultrasound visualization, the risk of significant thrombin escape into the distal circulation is rare 6. This is especially important given the potential devastating consequences if distal embolization were to occur into the cerebral circulation.
Holder et al. reported successful treatment of a carotid pseudoaneurysm with percutaneous thrombin injection 5. In their case, an occlusion balloon was used to prevent distal embolization. In our case, the circle of Willis was incomplete and did not provide sufficient collateral supply to the right middle cerebral artery from the contralateral internal carotid artery. Given this fact, occlusion of the right internal carotid artery was not considered a viable option and so a distal embolic protection device was favored over an occlusion balloon.
Distal carotid protection devices are used during carotid stent deployment 7. In a recent study regarding carotid and vertebral artery stenting for treatment of pseudoaneurysms, distal protection devices were not used. While the pseudoaneurysms were successfully treated, a patient developed thromboembolic occlusion of the left M1 segment despite loading anticoagulation 8. Another case of a superior mesenteric artery pseudoaneurysm was treated with thrombin after distal protection device deployment and a thrombus was successfully retrieved 9. In our case, a thrombus was also successfully retrieved after thrombin injection, and intracranial thromboembolism was avoided. The distal protection device would also address protection from the rare potential complication of distal thrombin escape.
Conclusion
Carotid artery pseudoaneurysm is a rare complication from placement of an internal jugular triple lumen catheter. Percutaneous thrombin injection with the aid of a distal embolic protection device is a viable method to treat this rare condition.
Acknowledgments
The report is dedicated to the memory of the late, great, Dr Randall Siegel, who performed the thrombin injection.
References
- 1.Ruesch S, Walder B, Tramer MR. Complications of central venous catheters: internal jugular versus subclavian access – A systemic review. Crit Care Med. 2002;30(2):454–460. doi: 10.1097/00003246-200202000-00031. [DOI] [PubMed] [Google Scholar]
- 2.DuBose J, Recinos G, Teixeira PGR, et al. Endovascular stenting for the treatment of traumatic internal carotid injuries: expanding experience. J Trauma. 2008;65:1561–1566. doi: 10.1097/TA.0b013e31817fd954. [DOI] [PubMed] [Google Scholar]
- 3.Agid R, Simons M, Casaubon LK, et al. Salvage of the carotid artery with covered stent after perforation with dialysis sheath. Interv Neuroradiol. 2012;18(4):386–390. doi: 10.1177/159101991201800404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tisi PV, Callam MJ. Surgery versus non-surgical treatment for femoral pseudoaneurysms. Cochrane Database of Systematic Reviews. 2006;(1) doi: 10.1002/14651858.CD004981.pub2. Art. No.: CD004981. DOI: 10.1002/14651858.CD004981.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Holder R, Hilton D, Martin J, et al. Percutaneous thrombin injection of carotid artery pseudoaneurysm. J Endovasc Ther. 2002;9:25–28. doi: 10.1177/152660280200900105. [DOI] [PubMed] [Google Scholar]
- 6.Vlachou PA, Karkos CD, Bains S, et al. Percutaneous ultrasound-guided thrombin injection for the treatment of iatrogenic femoral artery pseudoaneurysms. Eur J Radiol. 2011;77:172–174. doi: 10.1016/j.ejrad.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 7.Metzger DC. Embolic protection in carotid artery stenting: new options. Tech Vasc Interv Radiol. 2011;14(2):86–94. doi: 10.1053/j.tvir.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Yi AC, Palmer E, Luh GY, et al. Endovascular treatment of carotid and vertebral pseudoaneurysms with covered stents. Am J Neuroradiol. 2008;29:983–987. doi: 10.3174/ajnr.A0946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Juszkat R, Karsinski Z, Wykretowicz M, et al. Transarterial thrombin injection secured with an embolic protection device as a treatment for a superior mesenteric artery pseudoaneurysm. Cardiovasc Intervent Radiol. 2011;34:198–201. doi: 10.1007/s00270-009-9791-4. [DOI] [PubMed] [Google Scholar]