Summary
Bow hunter's syndrome is an uncommon cause of vertebrobasilar insufficiency resulting from rotational compression of the extracranial vertebral artery. While positional compression of any portion of the extracranial vertebral artery has been reported to result in bow hunter's syndrome, the most common site of compression is the V2 segment as it passes through the foramen transversarium of the subaxial cervical spine. A 43-year-old woman presented with increasingly frequent pre-syncopal and syncopal episodes upon leftward head rotation. Pre-operative angiographic studies with the neck rotated to the left demonstrated occlusion of the left vertebral artery by a C4-5 osteophyte arising from the C4 uncinate process. The patient underwent microsurgical decompression of the vertebral artery at C4-5 through a standard anterior transcervical retropharyngeal approach. Selective vertebral artery intraoperative angiography performed with the head passively rotated to the left before and after left vertebral artery decompression showed marked improvement in the luminal diameter and blood flow. The patient's symptoms resolved post-operatively. This case illustrates the second instance of intraoperative angiography used to confirm adequate vertebral artery decompression for bow hunter's syndrome. Intraoperative angiography can be safely used to decrease the extent of vertebral artery decompression in order to minimize the risk of operative complications.
Key words: vertebrobasilar insufficiency, stroke, endovascular procedures, vertebral artery, spondylosis
Introduction
Vertebrobasilar insufficiency resulting from vertebral artery compression during head rotation is an uncommon cause of posterior circulation ischemia 1. Ever since Sorensen et al. coined ‘bow hunter's stroke' after a bow-wielding patient developed a medullary infarct following head rotation, the constellation of position-dependent symptoms, typically syncope or pre-syncope, diplopia, and vertigo, has since been referred to as bow hunter's syndrome (BHS) 2. While the classic site of vertebral artery compression in BHS is the V3 segment in the C1-2 region, BHS is more commonly caused by compression of the V2 segment in the subaxial cervical spine 3. We describe our experience with a case of BHS caused by compression of the vertebral artery by an osteophyte in the subaxial cervical spine, which was treated by microsurgical decompression complemented by intraoperative angiography (IOA).
Case Report
A 43-year-old woman presented with increasingly frequent pre-syncopal and syncopal episodes occurring only during leftward head rotation. CT angiography with the patient's head rotated left showed a C4-5 osteophyte originating from the C4 uncinate process causing complete occlusion of the left vertebral artery with normal flow through the right vertebral artery (Figure 1). A pre-operative diagnostic angiogram showed normal flow through the left vertebral artery when the head was in the neutral position, rotated to the right in any degree, and rotated to the left up to 45 degrees. However, with the head actively rotated 90 degrees to the left, the patient became symptomatic and there was complete cessation of flow through the left vertebral artery at the C4-5 level and retrograde filling of the V2 segment distal to the occlusion via the contralateral vertebral artery (Figure 2).
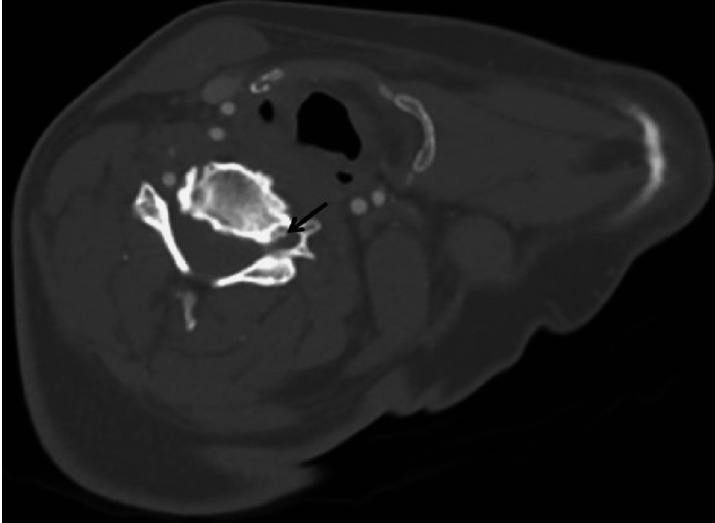
Figure 1.
Pre-operative CT angiogram with the patient's head turned to the left. A C4-5 osteophyte arising from left C4 uncinate process (arrow) causes complete occlusion of the left vertebral in the left C4 foramen transversarium. There is normal flow through the co-dominant right vertebral artery at the same level.
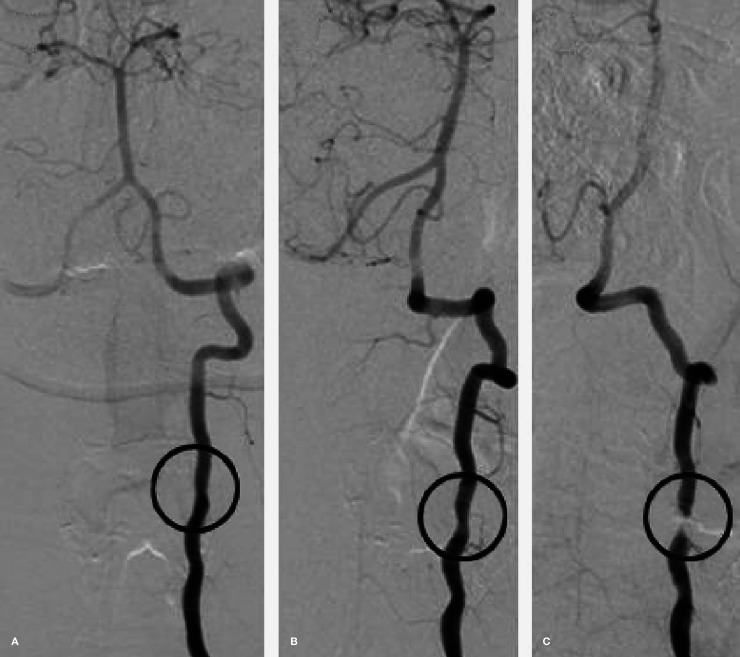
Figure 2.
Pre-operative diagnostic angiogram demonstrating normal flow through the left vertebral artery with the neck in the neutral position (A) and turned 45 degrees to the left (B). However, with the neck turned 90 degrees to the left (C), there is occlusion of the vertebral artery at the C4-5 level (circle) due to compression from an osteophyte. Retrograde flow distal to the obstruction via the contralateral vertebral artery is visualized. Also notice good filling of the intracranial vertebrobasilar circulation in the neutral (A) and 45-degree (B) positions which is greatly diminished in the 90-degree position (C). While not seen in this figure, it is important to note the patient had bilateral hypoplastic posterior communicating arteries.
The patient was taken to the operating room for microsurgical decompression of the left vertebral artery at C4-5. The patient was positioned supine on a radiolucent horseshoe. A selective left vertebral artery angiogram was then performed with the neck passively rotated to the left re-demonstrating the site of the occlusion at C4-5. (Figure 3A). A standard transcervical retropharyngeal approach was used to access the anterior cervical spine. After subperiosteally mobilizing the longus colli laterally, the C4-5 interspace, identified by fluoroscopy, was used as a guide to follow the vertebral body laterally until the anterior tubercle of the left C4 transverse process was encountered. A relaxing incision was made in the medial one-third of the left longus colli in order to adequately expose the anterolateral C4-5 bony anatomy overlying the vertebral artery.
After developing a plane between the C4 foramen transversarium and the vertebral venous plexus, the anterior ring of the foramen was resected with a Kerrison rongeur. A diamond burr was used to remove the large medial osteophyte arising from the C4 uncinate process. Ligamentous tissue in the lateral C4-5 region and the laterally herniated C4-5 disc were in close proximity to the vertebral artery and removed as well. A post-decompression selective IOA was performed with the head again passively rotated to the left which showed a significant increase in the luminal diameter of the vertebral artery and the arterial flow through the vessel (Figure 3B). The patient's BHS resolved completely following surgery and she experienced an uncomplicated post-operative course.
Figure 3.
Intraoperative angiography performed before (A) and after (B) microsurgical decompression of the left vertebral artery at the C4-5 level with the patient's head turned to the left. Prior to decompression (A), there is obstruction of flow through left vertebral artery at the caudal aspect of the C4 foramen transversarium (circle). Following decompression (B), including resection of the C4-5 osteophyte, partial C4-5 discectomy, and removal of a fibrous band overlying the vertebral artery, the luminal diameter of the vertebral artery at the C4-5 level is significantly improved with the neck in the left rotated position.
Discussion
Vertebrobasilar ischemia due to BHS is a rare clinical presentation that must be recognized as primarily a surgically managed pathology. Neurosurgeons, who are rigorously trained to manipulate both the osseous and vascular structures of the neck, are uniquely poised to address BHS. However, one must ensure the attainment of adequate pre-operative imaging with the neck rotated to identify the precise area of flow limitation 3. Additionally, delineation of the intracranial vasculature is crucial to fully understanding the composition of the vertebrobasilar circulation. In BHS, there is typically poor collateral circulation which exacerbates vertebrobasilar insufficiency upon vertebral artery occlusion.
Due to the prevalence of cervical spondylosis, positional compression of the vertebral artery most often occurs in the subaxial cervical spine. Degenerative ossification of the uncinate process results in osteophytes which, when enlarged posterolaterally, may impinge upon the vertebral artery as it courses through the foramen transversarium. Decompression of these osteophytes can be readily achieved through the standard anterior transcervical approach previously described and illustrated by Vilela et al. 3. Intraoperative assessment of arterial flow restoration confirms definitively that the decompression is adequate and allows for further bony or soft tissue resection if flow remains limited. While intraoperative ultrasonography is commonly used to achieve this goal, the use of IOA for the treatment of BHS has only been reported once before 4.
While a direct comparison of the two methods is currently unavailable, IOA may carry distinct advantages, including visualization of the affected arterial segment and the ability to evaluate unexposed portions of the artery. The additional risks incurred by the use of IOA are not negligible although compared to the reported complication rate in intracranial aneurysm surgery, the risk of adverse events should theoretically be lower for catheterization of a more proximal, larger diameter vessel such as the vertebral artery 5. Ultimately, we believe IOA is an effective adjunct which may prevent overaggressive vertebral artery decompression thereby minimizing potential operative and postoperative complications.
Conclusion
There is a paucity of literature describing the utility of IOA in the surgical management of bow hunter's syndrome (BHS). This case reinforces the unrivaled ability of IOA to assess flow restoration following vertebral artery decompression for BHS. We stress the importance of collaboration between neurosurgeons and neurointerventionalists when encountering cerebrovascular pathology, especially when its manifestation is rare.
References
- 1.Tissington Tatlow WF, Bammer HG. Syndrome of vertebral artery compression. Neurology. 1957;7:331–340. doi: 10.1212/wnl.7.5.331. [DOI] [PubMed] [Google Scholar]
- 2.Sorensen BF. Bow hunter’s stroke. Neurosurgery. 1978;2:259–261.. doi: 10.1227/00006123-197805000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Vilela MD, Goodkin R, Lundin DA, et al. Rotational vertebrobasilar ischemia: hemodynamic assessment and surgical treatment. Neurosurgery. 2005;56:36–43 discussion 43-45. doi: 10.1227/01.neu.0000146441.93026.ce. [DOI] [PubMed] [Google Scholar]
- 4.Velat GJ, Reavey-Cantwell JF, Ulm AJ, et al. Intraoperative dynamic angiography to detect resolution of Bow Hunter’s syndrome: Technical case report. Surg Neurol. 2006;66:420–423. doi: 10.1016/j.surneu.2006.03.040. discussion 423. [DOI] [PubMed] [Google Scholar]
- 5.Lopez KA, Waziri AE, Granville R, et al. Clinical usefulness and safety of routine intraoperative angiography for patients and personnel. Neurosurgery. 2007;61:724–729. doi: 10.1227/01.NEU.0000298900.84720.D0. discussion 729-730. [DOI] [PubMed] [Google Scholar]