Description
A 22-year-old Bangladeshi man presented to a London district general hospital with a 2 month history of abdominal pain, weight loss, fever and difficulty in walking. His medical history was significant for cervical tuberculous lymphadenitis and he had recently been stepped-down from quadruple therapy with rifampicin, isoniazid, ethambutol and pyrazinamide to dual therapy with rifampicin and isoniazid. On admission, he was febrile and tachycardic. Examination revealed generalised abdominal tenderness with a palpable, fluctuant right flank mass. Inflammatory markers were raised (C reactive protein 287 mg/l, erythrocyte sedimentation rate 121 mm/h) with a normal white cell count (9.4×109/l) and normocytic anaemia (haemoglobin 9.3 g/dl). An abdominal CT was performed which demonstrated a large right-sided psoas abscess measuring 110×190×80 mm with superior displacement of the right kidney (figure 1). No vertebral disease was seen.
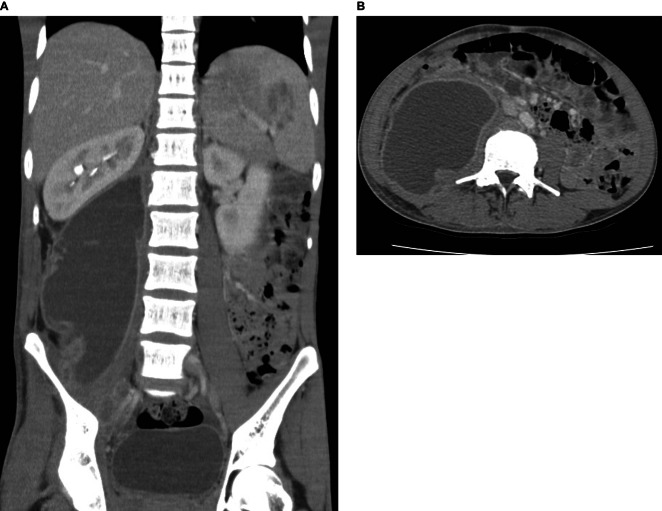
Figure 1.
Contrast-enhanced CT scans in (A) the coronal plane and (B) the transverse plane, demonstrating a large right-sided psoas abscess measuring 110×190×80 mm. There is superolateral displacement of the ipsilateral kidney, obliterating the hepato-renal recess. There is no evidence of lumbar involvement and the contralateral psoas major muscle is unaffected. Low attenuation lesions within the spleen may represent splenic abscesses.
The patient was treated with ultrasound-guided percutaneous drainage and was restarted on quadruple therapy, with a good symptomatic relief. A total volume of 1200 ml was drained.
Mycobacterial psoas abscess is typically associated with spinal tuberculosis due to the extension of infection from lumbar vertebrae. However, as in this patient, a psoas abscess may occur in the absence of spinal disease. This is either secondary to direct invasion from other adjacent structures or from haematogenous spread.1 Abdominal CT is the principal imaging modality for the diagnosis of psoas abscess,2 but ultrasound is also useful for drain insertion and for monitoring resolution. Percutaneous drainage combined with antituberculous therapy is usually sufficient for treatment; patients rarely require open surgical drainage.3
Learning points.
Presentations of mycobacterial psoas abscess are increasing in incidence and may occur in the absence of vertebral disease.
Treatment of large, symptomatic mycobacterial psoas abscess hinges on antituberculous medication with percutaneous drainage.
Caution should be used when reducing to dual therapy before mycobacterial culture and sensitivity results are available, owing to the risk of disease spread and complications.
Footnotes
Contributors: LWT and AJS designed and drafted the article. HB revised the article and approved the final version.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Vaz AP, Gomes J, Esteves J, et al. A rare cause of lower abdominal and pelvic mass, primary tuberculous psoas abscess: a case report. Cases J 2009;2013:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tonolini M, Campari A, Bianco R. Common and unusual diseases involving the iliopsoas muscle compartment: spectrum of cross-sectional imaging findings. Abdom Imaging 2012;2013:118–39 [DOI] [PubMed] [Google Scholar]
- 3.Yacoub WN, Sohn HJ, Chan S, et al. Psoas abscess rarely requires surgical intervention. Am J Surg 2008;2013:223–7 [DOI] [PubMed] [Google Scholar]