Abstract
The transcription factors STAT1 and STAT3 appear to play opposite roles in tumorigenesis. While STAT3 promotes cell survival/proliferation, motility and immune tolerance and is considered as an oncogene, STAT1 mostly triggers anti-proliferative and pro-apoptotic responses while enhancing anti-tumor immunity. Despite being activated downstream of common cytokine and growth factor receptors, their activation is reciprocally regulated and perturbation in their balanced expression or phosphorylation levels may re-direct cytokine/growth factor signals from proliferative to apoptotic, or from inflammatory to anti-inflammatory. Here we review the functional canonical and non-canonical effects of STAT1 and STAT3 activation in tumorigenesis and their potential cross-regulation mechanisms.
Keywords: STAT1, STAT3, anti-tumor immune response, apoptosis, inflammation, metastasis, oncogene, proliferation, survival, tumor invasivity, tumor suppressor, tumorigenesis
Introduction
Cross-talk between signaling pathways determines how a cell integrates the environmental signals received, ultimately translating them in transcriptional regulation of specific sets of genes. Transcription factors belonging to the signal transducer and activator of transcription family (STATs), being able to detect a variety of signals at the inner cell membrane and to transduce them to the nucleus directly affecting gene regulation, are ideally suited to play a central role in orchestrating the outcome of this cross-talk.1 Indeed, despite an intriguing convergence of distinct cytokine and growth factor receptors on STAT1 and STAT3 signaling [e.g., type I and II Interferons (IFNs), IL-6-type cytokines, growth factors such as EGF and PDGF], these soluble mediators elicit specific patterns and duration of STATs activation, resulting in distinct and often opposing effects on target cells.2 While STATs activation is typically fast but transient, due to specific negative feedback mechanisms, aberrant activation often leads to pathological conditions such as chronic inflammation, defective immune responses or cancer. Here, we present what is known about the actions of STAT1 and STAT3 in oncogenesis and finally discuss data suggesting reciprocal cross-regulation, likely to impact on different stages of tumor biology.
STAT1 is a central mediator of both type I (alpha and beta) and type II (gamma) IFNs,3 which are involved in cell growth regulation and antiviral and immune defense. IFNγ mainly triggers prolonged STAT1 activation that induces gene expression by binding to gamma-activated sequences (GAS). In contrast, type I IFNs activate both STAT1 and STAT2 triggering the formation of the ISGF3 transcriptional complex. Both IFN types can in addition activate STAT3, albeit to a lesser extent/more transiently.2
The IL-6 family of cytokines acts instead through homo- or hetero-dimerization of a common signal transduction subunit, gp130, with other specific receptors such as the LIFR. This activated receptor complex triggers tyrosine phosphorylation of STAT1/STAT3, which is either prolonged (STAT3) or transient (STAT1).4 Once phosphorylated, these two factors can bind to similar cognate sites both as homo- and as hetero-dimers, at least in vitro. However, the repertoire of target genes is mostly distinct, suggesting the need for specific co-factors for in vivo binding.2 STAT1 and STAT3 are thought to play opposite roles in tumorigenesis. STAT1 exerts a complex array of functions on both tumor cells and the immune system and is usually considered as a tumor suppressor.5 In contrast, STAT3 is considered as an oncogene, being constitutively active in nearly 70% of solid and hematological tumors, which often become dependent on its activity for their growth and survival.6 Accordingly, STAT3 activation can be elicited by a number of oncogenes (e.g., v-Src, v-Fps, v-Sis, Met and polyoma middle T antigen) in addition to the above listed cytokines and growth factors.
Moreover, overexpression of its constitutively active form, STAT3C, is sufficient to transform already immortalized fibroblasts and other non-malignant cell types such as breast and prostate epithelial cell lines (reviewed in ref. 6). Of note, the continued activity of the STAT3C artificial mutant was shown to be at least partly due to slower dephosphorylation rates and increased DNA binding affinity, resulting in prolonged activation and elevated expression of STAT3 target genes.7,8
Both STAT1 and STAT3 can exert their opposing effects on tumorigenesis either directly, through transcriptional regulation of target genes in the neoplastic cell, or indirectly, by modulating tumor angiogenesis, tissue invasion or the anti-tumor immune response.
Direct Effects of STAT1 and STAT3 Activity on Tumor Growth
STAT1 and STAT3 can directly activate targets with functions on proliferation and apoptosis. STAT1 typically promotes apoptosis by inducing the expression of members of the cell surface death receptor family and their ligands, in addition to caspases and iNOS; it can also repress the p53-inhibitor Mdm2 and act as a p53 co-activator.6,9,10 Additionally, STAT1 negatively regulates the cell cycle inducing the expression of IFITM1, the CDK inhibitors p21waf/cip1 and p27Kip1 and the G1/S phase blocker KLF4.6 Conversely, STAT1 activation inhibits the expression of several cyclins and of the oncogenes c-Myc and HER-2.6,11
In contrast, STAT3 constitutive activity is essential for proliferation and/or survival of many established or primary tumor cells, and its inhibition impairs tumor growth.6 STAT3 expression signature, although different in distinct tumor contexts, is indeed consistent with tumor cell growth and survival. Among STAT3 target genes are anti-apoptotic proteins, such as survivin and members of the Bcl family [e.g., Bcl-XL, Bcl-2 and myeloid cell leukemia sequence 1 (Mcl1)] and proteins involved in proliferation and cell cycle progression such as cyclin D1, c-Myc and pim-1/2.6,12,13 STAT3 can also inhibit apoptosis by suppressing Fas transcription and, in the mouse, p53 expression. It must be noted, however, that under physiological conditions STAT3 may act as an inducer of cell death. In particular, STAT3 is required for lysosome-mediated epithelial cell death during mammary gland involution.14
Consistently with its predominant anti-apoptotic role in cancer cells, STAT3 can confer resistance to chemotherapeutic drugs in several tumors. For example, doxorubicin activates STAT3 in a metastatic subline of breast cancer cells, suggesting that STAT3-mediated anti-apoptotic effects may represent one of the protection mechanisms activated in response to chemotherapeutic drugs.15 Indeed, interference with STAT3 activity sensitizes cells to doxorubicin-, taxol- or adriamycine-induced apoptosis in highly metastatic breast cancer cell lines,15 suggesting that STAT3 inhibition coupled to chemotherapeutic treatment might be a valid approach to cancer therapy.
In contrast with its prevalent pro-apoptotic role, STAT1 was recently shown to correlate also with improved resistance to chemotherapeutic drugs, as in the case of ovarian cancer and of cutaneous T-cell lymphoma.16,17
STAT3 can enhance survival and proliferation by acting on tumor glucose metabolism
STAT3 is essential for tumor transformation downstream of several oncogenes including Src18 and Ras.19 Interestingly, while Src induces STAT3 tyrosine phosphorylation and transcriptional activity, Ras elicits phosphorylation of STAT3 on serine 727, recently shown to be required for its localization to mitochondria. In turn, mitochondrial STAT3 enhances the respiratory chain activity under normal or Ras-transformed conditions, thus supporting Ras oncogenic transformation.19,20 In contrast, we have recently shown that constitutively active STAT3 is part of the complex signaling network that shapes the metabolic phenotype of tumor cells and that includes, among others, the PI3K pathway and the transcription factors hypoxia-inducible factor (HIF), p53, Myc and NFκB.21,22 Indeed, constitutively active STAT3 acts as a master regulator of cell metabolism, inducing aerobic glycolysis via HIF-1α transcriptional induction and downregulating mitochondrial activity in a HIF-1α-independent way both in primary fibroblasts and in STAT3-dependent tumor cell lines.23 Cells are thus protected from apoptosis and senescence while becoming highly sensitive to glucose deprivation. This metabolic switch, known as the Warburg effect, is shared by most cancer cells and is believed to lend a metabolic advantage to highly proliferating cells when nutrient supply is not limiting, as it favors the synthesis of essential cellular components required for fast cell duplication.24 In addition, glycolysis generates ATP less efficiently at a higher rate than oxidative phosphorylation and this is an advantageous feature for tumor cells as long as glucose supplies are not limited. Aerobic glycolysis and reduced mitochondrial respiration are important components of STAT3-mediated oncogenesis, as STAT3 inhibition in tumor cell lines downregulates glycolysis and upregulates mitochondrial activity prior to leading to growth arrest and cell death.23 This novel metabolic role is likely at the core of the addiction to STAT3 shown by so many biologically different tumors, and may provide further selective advantages in the hypoxic environment of solid tumors and of the stem cell niche. Of note, IFNγ-induced STAT1 activation was recently shown to negatively regulate HIF-1α-dependent transcription in human glioblastoma cells lines, once more highlighting the opposite effects of STAT1 and STAT3 in tumors.25
Thus, two distinct forms of “active” STAT3 exist: (1) tyrosine phosphorylated STAT3, which is nuclear and transcriptionally active and (2) serine phosphorylated STAT3, which is localized to mitochondria and transcriptionally inactive. Although regulated downstream of different signals under distinct physiological or pathological conditions, and eliciting different effects on cellular respiration, both forms finally converge to enhance cell survival and protection from apoptosis via specific regulation of mitochondrial functions.26
Both STAT1 and STAT3 can support the expansion of cancer stem cells
Cancer stem cells (CSCs), or tumor initiating cells, are a small population of slowly, asymmetrically dividing cells, which are resistant to chemotherapy and thought to be responsible for recurrence. STAT3, prominently involved in maintaining undifferentiated mouse embryonic stem cells, also plays a role in the maintenance of CSCs. Indeed, in head and neck squamous cell carcinoma (HNSCC) cells STAT3 tyrosine phosphorylation levels correlate with high tumorigenicity and the expression of stem cell markers.27 STAT3 activity is also crucial for neurosphere formation in glioblastoma,28 and for tumorsphere formation in human colon cell lines.29 STAT3 inhibition in glioblastoma and HNSCC cells leads to sensitization to chemotherapeutic treatment,27,28 a potential strategy for CSCs eradication. Additionally, several data sets point to a role for STAT3 in breast CSCs. STAT3 is required for the viability of the stem-like side population of MCF-7 cells.30 Moreover, autocrine IL-6 signaling sustains the aggressiveness of hypoxia-selected MCF-7 cells and enhances breast CSCs malignancy in several models.31 Finally, the stem cell-like subpopulation from human breast tumors shows high STAT3 activation and this drives STAT3 phosphorylation in other tumor cells via secretion of IL-6,32 and IL-6 drives the conversion of non-stem cancer cells into CSCs in human breast tumors and in a prostate cell line.33
The data correlating CSCs with STAT1 are more conflicting. In a model of oncogene-driven leukemia, the expansion potential of leukemia initiating cells is severely reduced in the absence of STAT1,34 and STAT1-deficient mice are partially protected from leukemia development.35 In contrast, IFNα treatment triggers proliferative reactivation of dormant hematopoietic stem cells (HSCs).36 This process requires STAT1 activity and sensitizes HSCs to the chemotherapeutic agent 5-fluoro-uracil, providing a potential mechanism for the so far unexplained clinical effects of IFNα on leukemic cells.
STAT3 Enhances Epithelial to Mesenchymal Transition and Cell Migration
Epithelial-mesenchymal transition (EMT), during which epithelial cells lose cell-cell adherence and acquire mesenchymal properties leading to migration, tissue invasion and metastasis, has been linked to the progression of epithelial tumors.37 STAT3 activity is required for EMT during gastrulation in zebrafish via the regulation of the breast-cancer-associated zinc transporter LIV1.38 More recent data suggest a direct link between STAT3 and EMT. Twist1, a major player in EMT, is a direct STAT3 target, and STAT3-mediated Twist-1 induction is involved in EGF-triggered EMT of cancer cells.6,39 Moreover, IL-6 induces EMT in the human breast cancer cell line MCF-7, and constitutive Twist1 expression triggers aberrant IL-6 production and STAT3 activation, suggesting a positive autocrine loop.40 Finally, we have recently shown that the tensin family member Cten, known to play a role in invasive cancer and to mediate EGF-induced migration, is a novel STAT3 target that contributes to disruption of cell-cell contacts and enhances migration and invasion in a model of HER2-mediated breast cancer.41
STAT3 can regulate cell movement also independently of EMT, as suggested by the observation that STAT3 conditional disruption in keratinocytes results in impaired migration and wound healing in response to EGF, TGF-α, HGF and IL-6. Moreover, STAT3 was shown to contribute to the disruption of epithelial adhesion and polarity downstream of ErbB2-Integrin β4 signaling (reviewed in ref. 6).
STAT3 may regulate cell motility also via non-nuclear functions. For example, phosphorylated STAT3 was reported to localize to focal adhesions in ovarian carcinoma cells and to interact with active focal adhesion kinase and paxillin, correlating with cell motility and aggressiveness.42 Interestingly, we could observe a similar localization in cells derived from MMTV-NeuT tumors expressing constitutively active STAT3.41 In addition, non-phosphorylated STAT3 can interact with the microtubule-destabilizing protein stathmin, resulting in enhanced polymerization and cell migration.43
Effects of STAT1 and STAT3 Activity on Tumor Angiogenesis and Metastasis
Both STAT1 and STAT3 can also indirectly control tumor growth by regulating angiogenesis in opposite ways. STAT1 acts as a negative regulator of tumor angiogenesis and, hence, tumor growth and metastasis by suppressing VEGF biological activity and the expression of pro-angiogenic FGF-β, while inducing the antiangiogenic chemokine IP-10 (CXCL10).6 The IFNγ/STAT1 pathway also counteracts pancreatic tumor growth by inhibiting the pro-tumoral fibrosis due to overproduction of extra-cellular matrix proteins by pancreatic stellate cells.44 Similarly, STAT1-mediated inhibition of the urokinase-type plasminogen activator (uPA) gene expression in breast cancer plays an antimetastatic role.45
In contrast, STAT3 enhances angiogenesis by mediating both VEGF expression and signaling, either directly or via HIF-1α.6 In addition, STAT3 can also enhance tissue invasion and metastasis by inducing members of the matrix-metalloproteinases family of proteins including MMP-9 and MMP-2, both of which are instead downregulated by STAT1.6,46 Moreover, STAT3 contributes to initiation and progression of pancreatic ductal adenocarcinoma at least partly by upregulating MMP7, whose serum levels are predictive of metastatic disease.47
Both STAT1 and STAT3 are Important Regulators of Anti-Tumor Immune Responses
Despite some contrasting observations, most data point to STAT1 as an important check-point to control tumor development via activation of the immune system, acting on both tumor and immune cells. Both type I and type II IFNs are crucial in the phenomenon formerly known as immunosurveillance and now defined by the broader concept of cancer immunoediting.48 Indeed, several human melanomas and squamous-cell carcinomas are able to bypass the immune system control by downregulating STAT1 expression.6
Activation of the IFNγ/STAT1/IRF1 axis favors processing and presentation of tumor antigens, in association with MHC class I or class II molecules.6 This function is mediated by direct regulation of MHC class I antigens expression, of the antigen processing-associated transporters (TAP) 1 and 2, and of LMP2 and LMP7.6,49,50 Moreover, the expression of the MHC class II transactivator CIITA, a coactivator essential for MHC class II transcription that is reduced in many tumors, is STAT1-dependent.6 Defective antigen presentation due to impaired IFNγ/STAT1 signaling, including STAT1 gene promoter methylation or de-acetylation, is a frequently observed strategy to escape immunosurveillance.6 These tumors become resistant to the direct anti-proliferative/pro-apoptotic effect of IFNγ released by T and natural killer (NK) cells and fail to overexpress MHC class I in response to IFNγ, thus becoming unable to display tumor associated antigens to effector CD8+ T cells. Of note, intra-tumoral T cells, nuclear STAT1 and strong MHC class I expression correlate with improved survival and identify patients that may benefit from immunotherapy in colorectal cancer.49 In the same vein, STAT1 is one out of five genes predictive of relapse-free and overall survival in non-small cell lung cancer (NSCLC),51 and its activation in immune cells predicts a favorable outcome correlating with activation of the immune response in melanoma.52 Indeed, downregulation of the IFN signaling pathway can also occur in the immune cells, an alternative strategy to escape immunosurveillance observed in T lymphocytes from patients with metastatic melanoma.53 Thus, defects in IFNγ/STAT1 signaling represent novel, dominant mechanisms of immune dysfunction in cancer. These findings might be exploited to design therapies to counteract immune dysfunction and improve cancer immunotherapy. It must however be borne in mind that STAT1 activation can sometimes inhibit rather than favor anti-tumor immune responses. In tumor-associated macrophages (TAMs), for example, STAT1 regulates the expression of arginase and NO, which in turn suppress T cell-mediated immune responses and induce T cell apoptosis, respectively, correlating with an adverse outcome.54,55 In addition, STAT1 can induce indoleamine 2,3-dioxygenase, an enzyme overexpressed in many cancers that blocks T lymphocytes activation,56 it can suppress the IL-12-mediated anti-tumor CTL activity,57 and its expression increases in late stage melanoma.58
STAT1 activity has also an ambiguous role in mammary carcinoma, where it represents a positive prognostic factor when expressed alone,59 but not when associated with phospho-STAT3.60 In agreement with the first observation, three recent papers report both enhanced and spontaneous mammary carcinogenesis in the absence of STAT1.80-82 In contrast, STAT1 co-expression with CD74 and Mx1 or with MUC1, respectively, identifies most aggressive triple negative breast tumors,61 correlating with poor prognosis.62
In contrast to STAT1, STAT3 has a key role in mediating tumor immune-evasion. STAT3 constitutive activity in tumor cells is indeed able to inhibit the maturation of antigen presenting cells (APCs), including dendritic cells (DC) and macrophages, at least partly through the production of soluble anergyzing factors such as VEGF and IL-10 and the reduced secretion of pro-inflammatory mediators.13 This inhibitory effect occurs via STAT3 activation in APCs, which is in turn responsible for impaired DC-mediated induction of T cell responses. Recently, tumor-derived exosome-associated Hsp72 was shown to induce STAT3 activity in myeloid-derived suppressor cells (MDSC) in a TLR2/MyD88-dependent manner.63 STAT3 activation in TAMs triggers a switch between the production of the anti- and pro-tumorigenic cytokines IL-12 or IL-23, respectively, by blocking NFκB-dependent IL-12 production while inducing IL-23 transcription.64 IL-23 in turn triggers the expansion of pro-inflammatory Th17 cells, which require STAT3 for their differentiation and activity, and stimulates the production of IL-10 by regulatory T cells, further inhibiting the immune response. Recently, constitutively active STAT3 in growing tumors and tumor-infiltrating immune cells was shown to facilitate NFκB binding to genes that are important for tumor growth, which contain both NFκB and STAT3 DNA-binding site(s), while inhibiting its binding to Th1 immunostimulatory genes, only carrying NFκB responsive elements.65
Indeed, STAT3 blockade in tumor cells increases the production of chemoattractants and the infiltration of immune cells, resulting in macrophage-mediated cytostatic activity.13 On the other hand, inhibition of STAT3 in macrophages could induce an anti-tumor immune response in several cancer models,13,64 and in vivo deletion of STAT3 in hematopoietic precursor cells resulted in enhanced anti-tumor activity triggered by DC, T cell, NK cells and neutrophils, correlating with a reduction of regulatory T cells.13
STAT3 and Tumor-Associated Inflammation
Tumor-associated inflammation has a crucial role in both initiation and progression of many malignancies.66 Indeed, chronic inflammatory conditions such as inflammatory bowel disease, hepatitis or pancreatitis are well known cancer predisposing factors. Infiltrating immune cells promote chronic inflammation and sustain growth and survival of pre-malignant cells by triggering continuous production of pro-inflammatory cytokines like IL-6. High IL-6 levels are often found in the serum of human patients with colon, breast, prostate, lung, ovary and liver cancer.67 Indeed, STAT3 has emerged as a key player in tumor-associated inflammation. Active STAT3 is often found at the invasive edge of tumors, adjacent to inflammatory cells, suggesting a role in the crosstalk between immune and tumor cells.68 Moreover, mice lacking STAT3 in the intestinal epithelial cells (IECs) are more resistant to the onset of AOM + DSS-induced colon carcinomas, a model of colitis-associated tumorigenesis.69,70 IL-6 produced by myeloid cells infiltrating the pre-cancerous tissue activates STAT3 in IECs, thus triggering survival and proliferation of pre-malignant cells and supporting a persistent inflammatory microenvironment that later will also sustain STAT3-dependent tumor growth. However, we have recently observed that ablation of STAT3 in IECs, although reducing early adenomas multiplicity, promotes tumor progression at later stages, leading to invasive carcinomas and significantly shortened lifespan.71 These data suggest specific functions according to different tumoral contexts, which need to be carefully assessed before resorting to anti-STAT3 therapeutic approaches.
On the other hand, STAT3 has been shown to be essential for the initiation and progression of pancreatic ductal adenocarcinomas.47,72 STAT3 deletion in pancreatic epithelial cells severely affects tumor formation in the KrasG12D mouse model of pancreatic intraepithelial neoplasia.47 In this context, STAT3 mediates the conversion of pancreatic epithelial cells to progenitor-like cells, more susceptible to Kras-mediated transformation, upon cerulein-induced pancreatitis. Furthermore, STAT3 orchestrates tumor-associated inflammation by regulating the production of chemokines able to attract IL-6 and IL-11-producing immune cells, which in turn sustain STAT3 activity.
STAT1:STAT3 Cross-Regulation
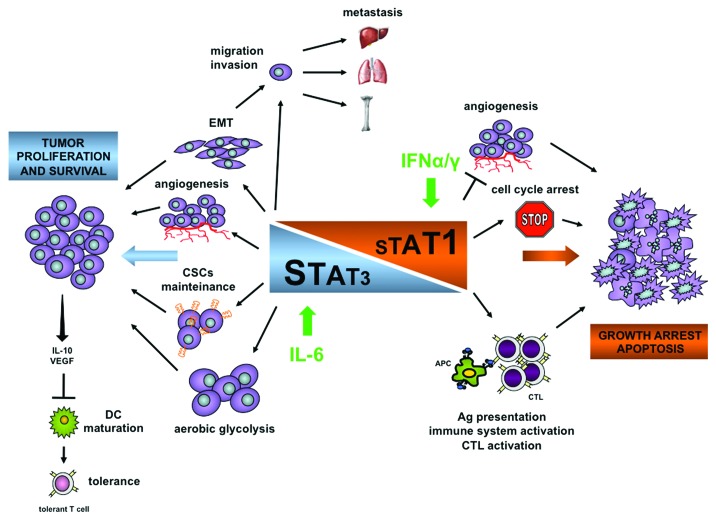
As discussed above and depicted in Figure 1, with some exceptions STAT1 and STAT3 play opposing roles in proliferation, apoptotic death, inflammatory and anti-tumor immune responses. In addition, studies on STAT-deficient cells/animals have revealed the existence of reciprocal STAT1:STAT3 regulatory mechanisms (reviewed in ref. 2). Indeed, STAT3 has recently emerged as a key player in holding the balance not only between the reciprocal STAT3 vs. STAT1 activation levels but also between the STAT vs. the MAPK branches of cytokine signaling. STAT3−/− cells display prolonged STAT1 and MAPK activation downstream of several IL-6 family cytokines both in vitro and in vivo.73,74 As a consequence, IL-6 induces in these cells an IFNγ-like response74 and triggers prolonged induction of immediate early genes such as cFos and Egr1.75 Interestingly, we have recently shown that phosphorylated STAT1 binds to the promoters of the IFN-responsive IRF-1 as well as of the Fos and Egr1 immediate early genes, mediating their aberrant transcriptional activation in the absence of STAT3.75 Increased and prolonged phosphorylation of STAT1 in response to gp130 cytokines occurs in several systems upon STAT3 gene inactivation (reviewed in ref. 2), suggesting that in normal cells one of the functions of STAT3 in response to IL-6 is to downregulate STAT1 activity. In this vein, STAT1 expression was recently shown to be required for cell death induced by treatment with the JAK1 inhibitor AG490, believed to act by abolishing STAT3 activation76 and by a STAT3-decoy oligonucleotide.77 Of note however, Lui et al. have shown STAT1-independent effects of the same decoy.78 Similarly, IFNγ and IFNα trigger proliferative responses correlating with STAT3-mediated transcription in STAT1-deficient bone-marrow-derived macrophages, T lymphocytes or MEFs.6 Thus, the relative abundance of STAT3 or STAT1 may play a role in determining their activation levels in response to activating stimuli. This may be relevant for the development and growth of tumors in the presence of specific tumor microenvironments, where different cytokine/growth factor combinations can modulate the relative levels of STAT1 and STAT3, resulting in their differential activation. Interestingly, many of the inflammatory mediators produced by cancer cells upon STAT3 inactivation are typical STAT1 targets (e.g., CXCL10, CCL5 and ICAM1).
Figure 1. Balanced activation and opposite effects of STAT1 and STAT3 in tumor settings. Prevalent STAT3 activation and/or expression, often downstream of IL-6 production, favors tumor development and maintenance. Tumor cell proliferation and survival are favored not only directly, but also indirectly by the maintenance of cancer stem cells and the switch to aerobic glycolysis. STAT3-dependent tumor-produced soluble factors such as IL-10 and VEGF induce STAT3-dependent tolerance in the immune cells. Moreover, STAT3 activation enhances metastasis formation by inducing EMT and cell migration and by increasing tumor angiogenesis. In contrast, the prevalence of STAT1 activation is fundamental to directly and indirectly block cell cycle progression and induce apoptosis of cancer cells. STAT1 elicits an efficient anti-tumor immune response both by stimulating antigen presentation to the immune system and by stimulating immune cells activity. CSCs, cancer stem cells; DC, dendritic cells; EMT, epithelial to mesenchymal transition (modified from ref. 2).
It is thus tempting to speculate that interfering with the activation of either factor in tumors may result in activation or re-activation of the other. Thus, care should be taken to plan therapeutic intervention using compounds that could unbalance finely tuned equilibria between STAT1 and STAT3. At the same time, the possibility to activate a specific STAT pathway by interfering with the other may under specific conditions provide unique therapeutic opportunities. For example, we have recently shown that interference with STAT3 activity in IFNγ-resistant human T lymphoma cells enhances pro-apoptotic responses to IFNγ while making cells sensitive to IL-6, which under these conditions triggers prolonged activation of STAT1, apoptosis and impaired in vivo growth.79 This strategy might be suitable in other conditions characterized by impaired STAT1 activation.
Acknowledgments
Work in the author’s laboratories was supported by the Italian Ministry of Research (MIUR, PRIN and FIRB), Italian Ministry of Health (Progetto Integrato Oncologia), Piedmont Region and by the Italian Association for Cancer Research (AIRC IG 9272).
Glossary
Abbreviations:
- IFNs
interferons
- GAS
gamma-activated sequences
- CSCs
cancer stem cells
- HNSCC
head and neck squamous cell carcinoma
- HSCs
hematopoietic stem cells
- EMT
epithelial-mesenchymal transition
- NK
natural killer
- NSCLC
non small cell lung cancer
- TAMs
tumor-associated macrophages
- APCs
antigen presenting cells
- DC
dendritic cells
- MDSC
myeloid-derived suppressor cells
- IECs
intestinal epithelial cells
Footnotes
Previously published online: www.landesbioscience.com/journals/jak-stat/article/20045
References
- 1.Schindler C, Levy DE, Decker T. JAK-STAT signaling: from interferons to cytokines. J Biol Chem. 2007;282:20059–63. doi: 10.1074/jbc.R700016200. [DOI] [PubMed] [Google Scholar]
- 2.Regis G, Pensa S, Boselli D, Novelli F, Poli V. Ups and downs: the STAT1:STAT3 seesaw of Interferon and gp130 receptor signalling. Semin Cell Dev Biol. 2008;19:351–9. doi: 10.1016/j.semcdb.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Schindler C, Brutsaert S. Interferons as a paradigm for cytokine signal transduction. Cell Mol Life Sci. 1999;55:1509–22. doi: 10.1007/s000180050391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heinrich PC, Behrmann I, Müller-Newen G, Schaper F, Graeve L. Interleukin-6-type cytokine signalling through the gp130/Jak/STAT pathway. Biochem J. 1998;334:297–314. doi: 10.1042/bj3340297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stephanou A, Latchman DS. STAT-1: a novel regulator of apoptosis. Int J Exp Pathol. 2003;84:239–44. doi: 10.1111/j.0959-9673.2003.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pensa S, Regis G, Boselli D, Novelli F, Poli V. STAT1 and STAT3 in tumorigenesis: two sides of the same coin. In: Stephanou A, ed. JAK-STAT Pathway in Disease. Austin: Landes Bioscience, 2008: 100-121. [Google Scholar]
- 7.Li L, Shaw PE. Elevated activity of STAT3C due to higher DNA binding affinity of phosphotyrosine dimer rather than covalent dimer formation. J Biol Chem. 2006;281:33172–81. doi: 10.1074/jbc.M606940200. [DOI] [PubMed] [Google Scholar]
- 8.Liddle FJ, Alvarez JV, Poli V, Frank DA. Tyrosine phosphorylation is required for functional activation of disulfide-containing constitutively active STAT mutants. Biochemistry. 2006;45:5599–605. doi: 10.1021/bi0525674. [DOI] [PubMed] [Google Scholar]
- 9.Allione A, Bernabei P, Bosticardo M, Ariotti S, Forni G, Novelli F. Nitric oxide suppresses human T lymphocyte proliferation through IFN-gamma-dependent and IFN-gamma-independent induction of apoptosis. J Immunol. 1999;163:4182–91. [PubMed] [Google Scholar]
- 10.Chin YE, Kitagawa M, Kuida K, Flavell RA, Fu XY. Activation of the STAT signaling pathway can cause expression of caspase 1 and apoptosis. Mol Cell Biol. 1997;17:5328–37. doi: 10.1128/mcb.17.9.5328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kominsky SL, Hobeika AC, Lake FA, Torres BA, Johnson HM. Downregulation of neu/HER-2 by interferon-gamma in prostate cancer cells. Cancer Res. 2000;60:3904–8. [PubMed] [Google Scholar]
- 12.Barré B, Avril S, Coqueret O. Opposite regulation of myc and p21waf1 transcription by STAT3 proteins. J Biol Chem. 2003;278:2990–6. doi: 10.1074/jbc.M210422200. [DOI] [PubMed] [Google Scholar]
- 13.Yu H, Kortylewski M, Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumour microenvironment. Nat Rev Immunol. 2007;7:41–51. doi: 10.1038/nri1995. [DOI] [PubMed] [Google Scholar]
- 14.Kreuzaler PA, Staniszewska AD, Li W, Omidvar N, Kedjouar B, Turkson J, et al. Stat3 controls lysosomal-mediated cell death in vivo. Nat Cell Biol. 2011;13:303–9. doi: 10.1038/ncb2171. [DOI] [PubMed] [Google Scholar]
- 15.Gariboldi MB, Ravizza R, Molteni R, Osella D, Gabano E, Monti E. Inhibition of Stat3 increases doxorubicin sensitivity in a human metastatic breast cancer cell line. Cancer Lett. 2007;258:181–8. doi: 10.1016/j.canlet.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 16.Fantin VR, Loboda A, Paweletz CP, Hendrickson RC, Pierce JW, Roth JA, et al. Constitutive activation of signal transducers and activators of transcription predicts vorinostat resistance in cutaneous T-cell lymphoma. Cancer Res. 2008;68:3785–94. doi: 10.1158/0008-5472.CAN-07-6091. [DOI] [PubMed] [Google Scholar]
- 17.Stronach EA, Alfraidi A, Rama N, Datler C, Studd JB, Agarwal R, et al. HDAC4-regulated STAT1 activation mediates platinum resistance in ovarian cancer. Cancer Res. 2011;71:4412–22. doi: 10.1158/0008-5472.CAN-10-4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bromberg JF, Horvath CM, Besser D, Lathem WW, Darnell JE., Jr. Stat3 activation is required for cellular transformation by v-src. Mol Cell Biol. 1998;18:2553–8. doi: 10.1128/mcb.18.5.2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gough DJ, Corlett A, Schlessinger K, Wegrzyn J, Larner AC, Levy DE. Mitochondrial STAT3 supports Ras-dependent oncogenic transformation. Science. 2009;324:1713–6. doi: 10.1126/science.1171721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wegrzyn J, Potla R, Chwae YJ, Sepuri NB, Zhang Q, Koeck T, et al. Function of mitochondrial Stat3 in cellular respiration. Science. 2009;323:793–7. doi: 10.1126/science.1164551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cairns RA, Harris IS, Mak TW. Regulation of cancer cell metabolism. Nat Rev Cancer. 2011;11:85–95. doi: 10.1038/nrc2981. [DOI] [PubMed] [Google Scholar]
- 22.Mauro C, Leow SC, Anso E, Rocha S, Thotakura AK, Tornatore L, et al. NF-κB controls energy homeostasis and metabolic adaptation by upregulating mitochondrial respiration. Nat Cell Biol. 2011;13:1272–9. doi: 10.1038/ncb2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demaria M, Giorgi C, Lebiedzinska M, Esposito G, D’Angeli L, Bartoli A, et al. A STAT3-mediated metabolic switch is involved in tumour transformation and STAT3 addiction. Aging (Albany NY) 2010;2:823–42. doi: 10.18632/aging.100232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324:1029–33. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hiroi M, Mori K, Sakaeda Y, Shimada J, Ohmori Y. STAT1 represses hypoxia-inducible factor-1-mediated transcription. Biochem Biophys Res Commun. 2009;387:806–10. doi: 10.1016/j.bbrc.2009.07.138. [DOI] [PubMed] [Google Scholar]
- 26.Demaria M, Poli V. From the nucleus to the mitochondria and back: the odyssey of a multitask STAT3. Cell Cycle. 2011;10:3221–2. doi: 10.4161/cc.10.19.17379. [DOI] [PubMed] [Google Scholar]
- 27.Chen YW, Chen KH, Huang PI, Chen YC, Chiou GY, Lo WL, et al. Cucurbitacin I suppressed stem-like property and enhanced radiation-induced apoptosis in head and neck squamous carcinoma--derived CD44(+)ALDH1(+) cells. Mol Cancer Ther. 2010;9:2879–92. doi: 10.1158/1535-7163.MCT-10-0504. [DOI] [PubMed] [Google Scholar]
- 28.Sherry MM, Reeves A, Wu JK, Cochran BH. STAT3 is required for proliferation and maintenance of multipotency in glioblastoma stem cells. Stem Cells. 2009;27:2383–92. doi: 10.1002/stem.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin L, Fuchs J, Li C, Olson V, Bekaii-Saab T, Lin J. STAT3 signaling pathway is necessary for cell survival and tumorsphere forming capacity in ALDH⁺/CD133⁺ stem cell-like human colon cancer cells. Biochem Biophys Res Commun. 2011;416:246–51. doi: 10.1016/j.bbrc.2011.10.112. [DOI] [PubMed] [Google Scholar]
- 30.Zhou J, Wulfkuhle J, Zhang H, Gu P, Yang Y, Deng J, et al. Activation of the PTEN/mTOR/STAT3 pathway in breast cancer stem-like cells is required for viability and maintenance. Proc Natl Acad Sci U S A. 2007;104:16158–63. doi: 10.1073/pnas.0702596104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sansone P, Storci G, Tavolari S, Guarnieri T, Giovannini C, Taffurelli M, et al. IL-6 triggers malignant features in mammospheres from human ductal breast carcinoma and normal mammary gland. J Clin Invest. 2007;117:3988–4002. doi: 10.1172/JCI32533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marotta LL, Almendro V, Marusyk A, Shipitsin M, Schemme J, Walker SR, et al. The JAK2/STAT3 signaling pathway is required for growth of CD44⁺CD24⁻ stem cell-like breast cancer cells in human tumors. J Clin Invest. 2011;121:2723–35. doi: 10.1172/JCI44745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iliopoulos D, Hirsch HA, Wang G, Struhl K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc Natl Acad Sci U S A. 2011;108:1397–402. doi: 10.1073/pnas.1018898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heuser M, Sly LM, Argiropoulos B, Kuchenbauer F, Lai C, Weng A, et al. Modeling the functional heterogeneity of leukemia stem cells: role of STAT5 in leukemia stem cell self-renewal. Blood. 2009;114:3983–93. doi: 10.1182/blood-2009-06-227603. [DOI] [PubMed] [Google Scholar]
- 35.Kovacic B, Stoiber D, Moriggl R, Weisz E, Ott RG, Kreibich R, et al. STAT1 acts as a tumor promoter for leukemia development. Cancer Cell. 2006;10:77–87. doi: 10.1016/j.ccr.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 36.Essers MAG, Offner S, Blanco-Bose WE, Waibler Z, Kalinke U, Duchosal MA, et al. IFNalpha activates dormant haematopoietic stem cells in vivo. Nature. 2009;458:904–8. doi: 10.1038/nature07815. [DOI] [PubMed] [Google Scholar]
- 37.Christiansen JJ, Rajasekaran AK. Reassessing epithelial to mesenchymal transition as a prerequisite for carcinoma invasion and metastasis. Cancer Res. 2006;66:8319–26. doi: 10.1158/0008-5472.CAN-06-0410. [DOI] [PubMed] [Google Scholar]
- 38.Yamashita S, Miyagi C, Fukada T, Kagara N, Che YS, Hirano T. Zinc transporter LIVI controls epithelial-mesenchymal transition in zebrafish gastrula organizer. Nature. 2004;429:298–302. doi: 10.1038/nature02545. [DOI] [PubMed] [Google Scholar]
- 39.Cheng GZ, Zhang WZ, Sun M, Wang Q, Coppola D, Mansour M, et al. Twist is transcriptionally induced by activation of STAT3 and mediates STAT3 oncogenic function. J Biol Chem. 2008;283:14665–73. doi: 10.1074/jbc.M707429200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sullivan NJ, Sasser AK, Axel AE, Vesuna F, Raman V, Ramirez N, et al. Interleukin-6 induces an epithelial-mesenchymal transition phenotype in human breast cancer cells. Oncogene. 2009;28:2940–7. doi: 10.1038/onc.2009.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barbieri I, Pensa S, Pannellini T, Quaglino E, Maritano D, Demaria M, et al. Constitutively active Stat3 enhances neu-mediated migration and metastasis in mammary tumors via upregulation of Cten. Cancer Res. 2010;70:2558–67. doi: 10.1158/0008-5472.CAN-09-2840. [DOI] [PubMed] [Google Scholar]
- 42.Silver DL, Naora H, Liu J, Cheng W, Montell DJ. Activated signal transducer and activator of transcription (STAT) 3: localization in focal adhesions and function in ovarian cancer cell motility. Cancer Res. 2004;64:3550–8. doi: 10.1158/0008-5472.CAN-03-3959. [DOI] [PubMed] [Google Scholar]
- 43.Ng DC, Lin BH, Lim CP, Huang G, Zhang T, Poli V, et al. Stat3 regulates microtubules by antagonizing the depolymerization activity of stathmin. J Cell Biol. 2006;172:245–57. doi: 10.1083/jcb.200503021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fitzner B, Brock P, Nechutova H, Glass A, Karopka T, Koczan D, et al. Inhibitory effects of interferon-gamma on activation of rat pancreatic stellate cells are mediated by STAT1 and involve down-regulation of CTGF expression. Cell Signal. 2007;19:782–90. doi: 10.1016/j.cellsig.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 45.Ilkovitch D, Handel-Fernandez ME, Herbert LM, Lopez DM. Antitumor effects of Mucin 1/sec involves the modulation of urokinase-type plasminogen activator and signal transducer and activator of transcription 1 expression in tumor cells. Cancer Res. 2008;68:2427–35. doi: 10.1158/0008-5472.CAN-07-5651. [DOI] [PubMed] [Google Scholar]
- 46.Ugarte-Berzal E, Redondo-Muñoz J, Eroles P, Del Cerro MH, García-Marco JA, Terol MJ, et al. VEGF/VEGFR2 interaction down-regulates matrix metalloproteinase-9 via STAT1 activation and inhibits B chronic lymphocytic leukemia cell migration. Blood. 2010;115:846–9. doi: 10.1182/blood-2009-08-239426. [DOI] [PubMed] [Google Scholar]
- 47.Fukuda A, Wang SC, Morris JP, 4th, Folias AE, Liou A, Kim GE, et al. Stat3 and MMP7 contribute to pancreatic ductal adenocarcinoma initiation and progression. Cancer Cell. 2011;19:441–55. doi: 10.1016/j.ccr.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331:1565–70. doi: 10.1126/science.1203486. [DOI] [PubMed] [Google Scholar]
- 49.Simpson JAD, Al-Attar A, Watson NFS, Scholefield JH, Ilyas M, Durrant LG. Intratumoral T cell infiltration, MHC class I and STAT1 as biomarkers of good prognosis in colorectal cancer. Gut. 2010;59:926–33. doi: 10.1136/gut.2009.194472. [DOI] [PubMed] [Google Scholar]
- 50.Leibowitz MS, Andrade Filho PA, Ferrone S, Ferris RL. Deficiency of activated STAT1 in head and neck cancer cells mediates TAP1-dependent escape from cytotoxic T lymphocytes. Cancer Immunol Immunother. 2011;60:525–35. doi: 10.1007/s00262-010-0961-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen H-Y, Yu S-L, Chen C-H, Chang G-C, Chen C-Y, Yuan A, et al. A five-gene signature and clinical outcome in non-small-cell lung cancer. N Engl J Med. 2007;356:11–20. doi: 10.1056/NEJMoa060096. [DOI] [PubMed] [Google Scholar]
- 52.Simons DL, Lee G, Kirkwood JM, Lee PP. Interferon signaling patterns in peripheral blood lymphocytes may predict clinical outcome after high-dose interferon therapy in melanoma patients. J Transl Med. 2011;9:52. doi: 10.1186/1479-5876-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Critchley-Thorne RJ, Yan N, Nacu S, Weber J, Holmes SP, Lee PP. Down-regulation of the interferon signaling pathway in T lymphocytes from patients with metastatic melanoma. PLoS Med. 2007;4:e176. doi: 10.1371/journal.pmed.0040176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Álvaro T, Lejeune M, Camacho FI, Salvadó MT, Sánchez L, García JF, et al. The presence of STAT1-positive tumor-associated macrophages and their relation to outcome in patients with follicular lymphoma. Haematologica. 2006;91:1605–12. [PubMed] [Google Scholar]
- 55.Kusmartsev S, Gabrilovich DI. STAT1 signaling regulates tumor-associated macrophage-mediated T cell deletion. J Immunol. 2005;174:4880–91. doi: 10.4049/jimmunol.174.8.4880. [DOI] [PubMed] [Google Scholar]
- 56.Uyttenhove C, Pilotte L, Théate I, Stroobant V, Colau D, Parmentier N, et al. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat Med. 2003;9:1269–74. doi: 10.1038/nm934. [DOI] [PubMed] [Google Scholar]
- 57.Torrero MN, Xia X, Henk W, Yu S, Li S. Stat1 deficiency in the host enhances interleukin-12-mediated tumor regression. Cancer Res. 2006;66:4461–7. doi: 10.1158/0008-5472.CAN-05-3554. [DOI] [PubMed] [Google Scholar]
- 58.Schultz J, Koczan D, Schmitz U, Ibrahim SM, Pilch D, Landsberg J, et al. Tumor-promoting role of signal transducer and activator of transcription (Stat)1 in late-stage melanoma growth. Clin Exp Metastasis. 2010;27:133–40. doi: 10.1007/s10585-010-9310-7. [DOI] [PubMed] [Google Scholar]
- 59.Widschwendter A, Tonko-Geymayer S, Welte T, Daxenbichler G, Marth C, Doppler W. Prognostic significance of signal transducer and activator of transcription 1 activation in breast cancer. Clin Cancer Res. 2002;8:3065–74. [PubMed] [Google Scholar]
- 60.Charpin C, Secq V, Giusiano S, Carpentier S, Andrac L, Lavaut M-N, et al. A signature predictive of disease outcome in breast carcinomas, identified by quantitative immunocytochemical assays. Int J Cancer. 2009;124:2124–34. doi: 10.1002/ijc.24177. [DOI] [PubMed] [Google Scholar]
- 61.Greenwood C, Metodieva G, Al-Janabi K, Lausen B, Alldridge L, Leng L, et al. Stat1 and CD74 overexpression is co-dependent and linked to increased invasion and lymph node metastasis in triple-negative breast cancer. J Proteomics. 2012;75:3031–41. doi: 10.1016/j.jprot.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 62.Khodarev N, Ahmad R, Rajabi H, Pitroda S, Kufe T, McClary C, et al. Cooperativity of the MUC1 oncoprotein and STAT1 pathway in poor prognosis human breast cancer. Oncogene. 2010;29:920–9. doi: 10.1038/onc.2009.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chalmin F, Ladoire S, Mignot G, Vincent J, Bruchard M, Remy-Martin JP, et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. J Clin Invest. 2010;120:457–71. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kortylewski M, Xin H, Kujawski M, Lee H, Liu Y, Harris T, et al. Regulation of the IL-23 and IL-12 balance by Stat3 signaling in the tumor microenvironment. Cancer Cell. 2009;15:114–23. doi: 10.1016/j.ccr.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee H, Deng J, Xin H, Liu Y, Pardoll D, Yu H. A requirement of STAT3 DNA binding precludes Th-1 immunostimulatory gene expression by NF-κB in tumors. Cancer Res. 2011;71:3772–80. doi: 10.1158/0008-5472.CAN-10-3304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 67.Heikkilä K, Ebrahim S, Lawlor DA. Systematic review of the association between circulating interleukin-6 (IL-6) and cancer. Eur J Cancer. 2008;44:937–45. doi: 10.1016/j.ejca.2008.02.047. [DOI] [PubMed] [Google Scholar]
- 68.Bromberg J, Wang TC. Inflammation and cancer: IL-6 and STAT3 complete the link. Cancer Cell. 2009;15:79–80. doi: 10.1016/j.ccr.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bollrath J, Phesse TJ, von Burstin VA, Putoczki T, Bennecke M, Bateman T, et al. gp130-mediated Stat3 activation in enterocytes regulates cell survival and cell-cycle progression during colitis-associated tumorigenesis. Cancer Cell. 2009;15:91–102. doi: 10.1016/j.ccr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 70.Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009;15:103–13. doi: 10.1016/j.ccr.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Musteanu M, Blaas L, Mair M, Schlederer M, Bilban M, Tauber S, et al. Stat3 is a negative regulator of intestinal tumor progression in Apc(Min) mice. Gastroenterology. 2010;138:1003–11, e1-5. doi: 10.1053/j.gastro.2009.11.049. [DOI] [PubMed] [Google Scholar]
- 72.Lesina M, Kurkowski MU, Ludes K, Rose-John S, Treiber M, Klöppel G, et al. Stat3/Socs3 activation by IL-6 transsignaling promotes progression of pancreatic intraepithelial neoplasia and development of pancreatic cancer. Cancer Cell. 2011;19:456–69. doi: 10.1016/j.ccr.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 73.Maritano D, Sugrue ML, Tininini S, Dewilde S, Strobl B, Fu X, et al. The STAT3 isoforms alpha and beta have unique and specific functions. Nat Immunol. 2004;5:401–9. doi: 10.1038/ni1052. [DOI] [PubMed] [Google Scholar]
- 74.Costa-Pereira AP, Tininini S, Strobl B, Alonzi T, Schlaak JF, Is’harc H, et al. Mutational switch of an IL-6 response to an interferon-gamma-like response. Proc Natl Acad Sci U S A. 2002;99:8043–7. doi: 10.1073/pnas.122236099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schiavone D, Avalle L, Dewilde S, Poli V. The immediate early genes Fos and Egr1 become STAT1 transcriptional targets in the absence of STAT3. FEBS Lett. 2011;585:2455–60. doi: 10.1016/j.febslet.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 76.Shim SH, Sung MW, Park SW, Heo DS. Absence of STAT1 disturbs the anticancer effect induced by STAT3 inhibition in head and neck carcinoma cell lines. Int J Mol Med. 2009;23:805–10. doi: 10.3892/ijmm_00000196. [DOI] [PubMed] [Google Scholar]
- 77.Souissi I, Najjar I, Ah-Koon L, Schischmanoff PO, Lesage D, Le Coquil S, et al. A STAT3-decoy oligonucleotide induces cell death in a human colorectal carcinoma cell line by blocking nuclear transfer of STAT3 and STAT3-bound NF-κB. BMC Cell Biol. 2011;12:14. doi: 10.1186/1471-2121-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lui VWY, Boehm AL, Koppikar P, Leeman RJ, Johnson D, Ogagan M, et al. Antiproliferative mechanisms of a transcription factor decoy targeting signal transducer and activator of transcription (STAT) 3: the role of STAT1. Mol Pharmacol. 2007;71:1435–43. doi: 10.1124/mol.106.032284. [DOI] [PubMed] [Google Scholar]
- 79.Regis G, Icardi L, Conti L, Chiarle R, Piva R, Giovarelli M, et al. IL-6, but not IFN-gamma, triggers apoptosis and inhibits in vivo growth of human malignant T cells on STAT3 silencing. Leukemia. 2009;23:2102–8. doi: 10.1038/leu.2009.139. [DOI] [PubMed] [Google Scholar]
- 80.Raven JF, Williams V, Wang S, Tremblay ML, Muller WJ, Durbin JE, et al. Stat1 is a suppressor of ErbB2/Neu-mediated cellular transformation and mouse mammary gland tumor formation. Cell Cycle. 2011;10:794–804. doi: 10.4161/cc.10.5.14956. [DOI] [PubMed] [Google Scholar]
- 81.Schneckeleithner C, Bago-Horvath Z, Dolzing H, Neugebauer N, Kollmann, Kolbe T, et al. Putting brakes on mammary tumorigenesis: Loss of STAT1 predisposes to intraepithelial neoplasias. Oncotarget. 2011;2:1043–1054. doi: 10.18632/oncotarget.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chan SR, Vermi W, Luo J, Lucini L, Rickert C, Fowler AM, et al. STAT1-deficient mice spontaneously develop estrogen receptor alpha-positive luminal mammary carcinomas. Breast Cancer Res. 2012;14:R16. doi: 10.1186/bcr3100. [DOI] [PMC free article] [PubMed] [Google Scholar]