Abstract
Aim:
The primary aim was to determine the prognostic significance of apoptosis in colorectal tumour cells and tumour-associated stroma. A secondary aim was to determine whether apoptosis was related to immune surveillance.
Methods:
Immunohistochemistry was performed using monoclonal antibodies recognising cleaved caspase-3 (CC3), cleaved poly (ADP-ribose) polymerase (PARP), p53, Bcl2, MHC-II, B cells (CD16), macrophages (CD68) and T cells (CD3), on a tissue microarray of 462 colorectal tumours.
Results:
Kaplan–Meier analysis demonstrated that patients with high expression of CC3 in the tumour or CC3 or cleaved PARP in tumour-associated stroma have a good prognosis. This suggests that tumour stroma is promoting tumourigenesis and that high levels of death within the stroma breaks this link. CC3 levels in the tumour correlated with cleaved PARP and MHC-II expression but not with CD16, CD68, CD3, p53 or Bcl2 expression. CC3 levels on tumour-associated stroma also correlated with cleaved PARP and MHC-II expression but not with CD16, CD68, CD3, p53 or Bcl2 expression. Tumour cells express MHC-II in response to IFN-γ, suggesting that this may be one of the initiators of apoptosis within the good prognosis tumours. Although 73% of the MHC-II-positive tumour had high levels of apoptosis, many tumours had high levels of apoptosis in the absence of MHC-II, implying that this is only one of many causes of apoptosis within tumours. On multivariate analysis, using Cox's proportional hazards model, tumour stage, vascular invasion and expression of CC3 in tumour-associated stroma were shown to be independent markers of prognosis.
Conclusion:
This study shows that a high level of apoptosis within colorectal tumour-associated stroma is an independent marker of good prognosis.
Keywords: Apoptosis, cleaved caspase-3, cleaved PARP, MHC-II, colorectal cancer, tumour-associated stroma
One of the hallmarks of cancers is their ability to accumulate mutations that provides progressive and survival advantages as well as resistance to cell death mechanisms. (O'Connell et al, 2000; Mild et al, 2002; Mazelin et al, 2004; Watson et al, 2005; Dyer et al, 2007; Ullenhag et al, 2007; Krajewska et al, 2008; Hector and Prehn, 2009; Yang et al, 2009). The interplay between the tumour and its associated stroma is complex. Recent studies have suggested that there is an autocrine link between the two promoting and driving tumourigenesis. In brief, cancer cells induce oxidative stress in adjacent fibroblasts and other stromal cells resulting in the production of reactive oxygen species (Balliet et al, 2011). Excessive reactive oxygen species drives an anti-oxidant defence in the adjacent tumour cells protecting them from apoptosis and also induces DNA damage and aneuploidy. Reactive oxygen species also induces autophagy leading to over production of recycled nutrients which then further drive anabolic growth of tumour cells. Heterotypic signalling in cancer-associated fibroblasts activates HIF1α and NF-κB potentiating the autophagic cycle in the stroma (Lisanti et al, 2010). It is therefore unclear whether apoptosis within either the tumour or the associated stroma will confer either a good or bad prognosis.
Furthermore, tumours express a range of stress-related molecules that alert the immune system to the danger, a process termed immune surveillance and one of the key mediators is interferon-gamma (IFN-γ; Dunn et al, 2005; Nausch and Cerwenka, 2008; Waldhauer and Steinle, 2008). MHC-II expression is induced on epithelial, endothelial and fibroblast cells and is upregulated on macrophages by IFN-γ. MHC-II expression on tumour cells and within stroma may therefore be a good marker of immune surveillance. There is then a period of immune equilibrium where the transformed cells acquire further mutations and the immune system continuously adapts to combat this progression. Ultimately, during the process of ‘immune editing' where the immune system is sculpting the tumour phenotype, the immune-resistant clones of tumour may emerge. One other consequence of immune editing is alteration of the tumour microenvironment, which becomes increasingly immunosuppressive (Watson et al, 2006b; Jordanova et al, 2008; Sica et al, 2008; McGilvray et al, 2009).
Apoptosis mediated by either the intrinsic or extrinsic pathways results in cleavage of caspase-3 (CC3). Caspase-3 is rarely mutated in colorectal cancer (Soung et al, 2004) and is therefore an ideal marker for measuring apoptosis in these tumours. Furthermore, studies have validated the use of active caspase-3 staining as a marker for apoptosis (Sabine et al, 2012) The CC3 mAb used in this study has previously been shown to bind specifically to the cleaved fragment of capase-3 and not to the full-length protein by western blot (Cheong et al, 2003; Garnier et al, 2003; Thome et al, 2012), as well as being validated for use with paraffin-embedded immunohistochemistry (Gown and Willingham, 2002; Patel and Krimm, 2010). Caspase 3 can also be cleaved by other proteases, and this does not always lead to activation. To further validate apoptosis within the tumour, cleavage of the caspase 3 substrate poly (ADP-ribose) polymerase (PARP), was also measured. This study aims to measure the level of apoptosis both within the stroma and in tumour cells and to correlate this with immune surveillance in a large cohort of colorectal cancers utilising high-throughput tissue microarray technology.
Materials and methods
Patient study and design
The study population comprised a series of 462 consecutive patients undergoing elective surgical resection of a histologically proven sporadic primary colorectal cancer at the University Hospital, Nottingham, UK (Table 1; Durrant et al, 2003; Watson et al, 2005; Watson et al, 2006a; Duncan et al, 2007; Ullenhag et al, 2007; McGilvray et al, 2009; Simpson et al, 2010). These patients were treated between 1 January 1994 and 31 December 2000; this time period allowed meaningful assessment of the prognostic markers studied. All patients treated during this time-frame were considered eligible for inclusion in the study. Tumours were classified as mucinous carcinoma, when >50% of tumour volume consisted of mucin (Kakar et al, 2004).
Table 1. Numbers of tumour specimens negative and positive for CC3 expression.
| Marker | Level of expression | Number of specimens (%) |
|---|---|---|
|
CC3 | ||
|
Tumour | ||
| |
Low (0–60 cells mm−2) |
43 (13) |
| |
High (61–max cells mm−2) |
314 (87) |
| |
Total |
334 (100) |
| |
Tumour-associated stroma |
|
| |
Low (0–104 cells mm−2) |
178 (56) |
| |
High (105–max cells mm−2) |
142 (44) |
| |
Total |
320 (100) |
|
MHC-II | ||
|
Tumour | ||
| |
Negative |
386 (94) |
| |
Positive |
27 (6) |
| |
Total |
413 (100) |
| |
Tumour-associated stroma |
|
| |
Negative |
213 (51) |
| |
Positive |
202 (49) |
| |
Total |
415 (100) |
|
Cleaved PARP | ||
|
Tumour | ||
| |
Low |
183 (90) |
| |
High |
23 (10) |
| |
Total |
206 |
| |
Tumour-associated stroma |
|
| |
Low |
189 (92) |
| |
High |
16 (8) |
| Total | 205 | |
Abbreviations: CC3=cleaved caspase-3; MHC-II=major histocompatibility class II; PARP=poly (ADP-ribose) polymerase.
Clinicopathological variables for the patient cohort (n=462)
Only cases where the relevant pathological material was unavailable were excluded from the study. Follow-up was calculated from the time of resection of the original tumour with all surviving cases being censored for data analysis at 31 December 2003, this produced a median follow-up of 37 months (range 0–116) for all the patients and 75 months (range 36–116) for survivors.
A prospectively maintained database was used to record relevant clinicopathological data, with data provided from the UK Office for National Statistics; this was available in >99% of cases. The information collected was independently validated through case note review of deceased patients. Disease-specific survival (DSS) was used as the primary end point. Data were also collected on the various other relevant clinical and histopathological parameters (Supplementary Table S1). Adjuvant chemotherapy consisting of 5-FU and folinic acid was reserved for those patients with positive lymph nodes, although surgical and adjuvant treatment was at the discretion of the supervising physician. Sixteen (3%) patients received pre-operative radiotherapy treatment. Previous ethical review of the study was conducted by the Nottingham Local Research and Ethics Committee, who granted approval for the study.
The median age at the time of surgery was 72 years, consistent with a median age at diagnosis of colorectal cancer of 70–74 years in the UK (Quinn et al., 2001). Sixty-nine (15%) tumours arrayed were TNM stage 1, 174 (38%) stage 2, 155 (34%) stage 3 and 54 (11%) stage 4; there were 3 cases of in situ disease. These figures are comparable with national figures for distribution of stage 1–4 at diagnosis of 11, 35, 26 and 29%, respectively (NICE, 2004). In all, 52% of tumours were of colonic origin and 39% were of rectal origin, and in 9% of cases the site was not recorded. The majority of tumours (392, 85%) were adenocarcinomas and were most frequently of a moderate histological grade (353, 77%). Also, 128 (28%) tumours were noted to have histological evidence of extramural vascular invasion, 224 (48%) had no evidence of vascular invasion and this information was not available in 110 (24%) cases.
Patients had a median follow-up of 37 months (range 0–116). At the time of censoring for data analysis, 228 (49%) patients had died from their disease, 64 (14%) were deceased from all other causes and 169 (37%) were alive. The median 5-year DSS for the cohort was 58 months, comparable with a national average of approximately 45% 5-year survival for colorectal cancer in the UK (NICE, 2004). The size of the TMA allows illustration of survival differences of 10%.
Specimen characteristics
All following resection were incised, fixed immediately in 10% neutral-buffered formalin and were embedded in paraffin wax, ensuring optimal tissue fixation and preservation for histological examination. Tissue microarrays were constructed as described previously (Kononen et al, 1998).
Immunohistochemistry
Immunohistochemical analysis of CC3, cleaved PARP and MHC-II expression was performed using a routine streptavidin–biotin peroxidase method. Staining of the slides was carried out as described previously (Watson et al, 2006a). The mouse monoclonal antibody specifically recognising the Asp175 residue of CC3 (diluted 1 : 200 overnight at 4 °C; Cell Signalling Technology, Danvers, MA, USA), anti-cleaved PARP antibody recognising Asp214 residue (diluted 1 : 100 for 1 h at room temperature; Cell Signalling) or anti-MHC-II mAb (diluted 1 : 100 for 1 h at room temperature, HLA DP DQ DR clone WR18; AbD Serotec, Oxford, UK) were used after heat-mediated antigen retrieval with pH 9.0 EDTA buffer.
Evaluation of CC3, cleaved PARP and MHC-II staining
The tumour cores were first imaged at × 20 (0.46 μm pixel−1) using a NanoZoomer 2.0-HT slide scanner (Hamamatsu, Bridgewater, NJ, USA). The cores were then assessed by two independent observers (PN and MV both with experience in the analysis of TMAs) in the Nanozoomer Digital Pathology viewer (Hamamatsu). CC3 and cleaved PARP expression in tumours were classified by measuring the area of tumour and tumour-associated stroma per core and counting the number of positively stained cells, giving a number of positively stained cells per mm2 area. Cells positive for CC3 or cleaved PARP showed homogenous staining and were considered positive when staining was observed. In cases of discrepancy, the cores were reassessed. Determination of the optimal cutoff points for CC3 and cleaved PARP-positive cells mm−2 against DSS were performed by using X-tile bioinformatics software version 3.4.7 (Camp et al, 2004). To avoid the problem of multiple cut point selection, the software performs standard Monte Carlo cross-validation to produce corrected P-values (Camp et al, 2004). MHC-II staining was classified into negative and positive staining in both tumour and tumour-associated cells, where any staining was considered as positive. Both observers were blinded to the clinical and pathological parameters.
Statistical analysis
Statistical analysis of the study data was performed using the SPSS package (version 16 for Windows, SPSS Inc., Chicago, IL, USA). Pearson's χ2 test was used to determine the significance of associations between categorical variables. DSS calculations included all patients whose death related to colorectal cancer. By contrast, patients whose deaths resulted from non-colorectal cancer-related causes were censored at the time of death. Kaplan–Meier curves were used to assess factors that influenced survival. The statistical significance of differences in DSS between groups with differing CC3 and MHC-II expression was estimated using the log-rank test. The Cox's proportional hazards model was used for multivariate analysis in order to determine the relative risk and independent significance of individual factors. In all the cases, P-values <0.05 were considered as statistically significant.
Results
Clinical and pathological data
The clinicopathological features of the 462 cases included in the present study are shown in Supplementary Table S1. Examination of the standard clinicopathological features identified the expected associations between DSS and TNM stage (log-rank=211.37, P<0.0001), DSS with extramural vascular invasion (log-rank=44.30, P<0.0001) but not with differentiation (log-rank=5.75, P=0.12).
CC3 and cleaved PARP expression
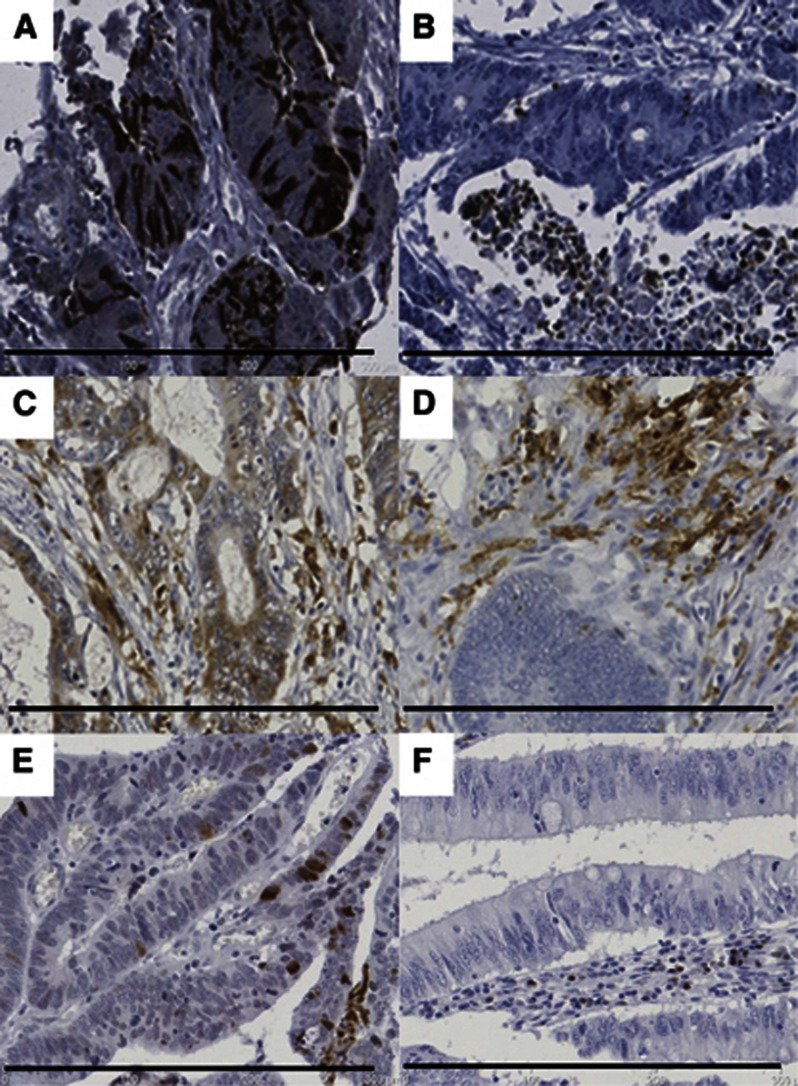
Analysis of CC3 was possible in 334 of the total 462 cores (72%), with the remainder being lost during antigen retrieval or not demonstrating viable tumour cells in the core. Due to the large loss of cores, the clinicopathological data for the 334 samples was confirmed to be similar to the original cohort (Supplementary Table S1). Examples of CC3 staining of tumour and tumour-associated stroma are demonstrated in Figure 1. The majority of staining was seen in the nucleus of both tumour and tumour-associated stromal cells. The majority of tumours had <1000 cells mm−2 of CC3-positive tumour cells and <2000 cells mm−2 in tumour-associated stroma. There were 43 (13%) samples that had a low level of CC3 in tumour cells (0–60 cells mm−2) and 178 (56%) of samples that had a low level of CC3 expression in the tumour-associated stroma (0–104 cells mm−2; Table 1).
Figure 1.
Representations of staining with CC3, cleaved PARP and MHC-II.Samples depicting (A) CC3 staining of tumour, (B) CC3 staining of stroma (C) MHC-II staining of tumour (D) MHC-II staining of stroma (E) cleaved PARP staining of tumour, (F) cleaved PARP staining of stroma. Resolution of images is 0.46 μm pixel−1. Embedded scale bar represents 300 μm.
The anti-CC3 monoclonal antibody recognises the Asp175 residue of cleaved caspase 3 but does not discriminate between active caspase 3 and cleaved caspase-3 generated by other proteases, such as calpains. To try and confirm that it was active caspase-3 that was being measured, the TMA was also stained for cleaved PARP. Examples of cleaved PARP staining of tumour and tumour-associated stroma are demonstrated in Figure 1. The majority of staining was seen in the nucleus of both tumour and tumour-associated stromal cells. The mean number of cleaved PARP-positive cells was 45 cells mm−2 in the tumour and 18 cells mm−2 in the stroma. This was lower than the mean levels of CC3 observed (277 cells mm−2 in the tumour and 257 cells mm−2 in the stroma), supporting the idea that CC3 was generated by a variety of proteases. There were 92% of samples that had a low level of cleaved PARP in tumour cells (CC3 expression was 13%) and 70% of samples (CC3 expression was 56%) had a low level of PARP expression in the tumour-associated stroma (Table 1).
Markers of apoptosis and inflammation: Bcl2, p53, CD3, CD68, CD16 and MHC-II expression
This array has previously been stained for the presence of stromal and intratumoural T, NK and macrophages cells using the CD3, CD68 and CD16 markers, with an increased level of intratumoural T cells correlating with a good survival (Simpson et al, 2010). Expression of Bcl2 and p53 have previously been reported (Watson et al, 2005). As a marker of IFN-γ-induced activation, expression of MHC-II on tumour cells and stroma-associated cells was measured. It was possible to measure MHC-II expression in 413 of the total 462 cores (89%), with the remainder being lost during antigen retrieval or not demonstrating viable tumour cells in the core. Examples of MHC-II staining of tumour and tumour-associated stroma are demonstrated in Figure 1. The majority of cores were negative for MHC-II expression in tumour cells (386 negative, 27 positive); 213 cores were negative for tumour-associated stroma staining, with 202 showing positive staining for MHC-II (Table 1).
Relationship between CC3, cleaved PARP and MHC-II expression and standard clinicopathological variables
The relationship between CC3, cleaved PARP and MHC-II expression in tumour and tumour-associated stroma and standard clinicopathological variables and markers of immune activation was measured using the Pearson's χ2 test (Table 2). Expression of CC3 and MHC-II in the tumour associated significantly with TNM stage (P=0.047 and 0.007, respectively) and the presence of distant metastases (P=0.047, 0.005, respectively). Cleaved PARP in both the tumour and stroma correlated with TNM stage (P>0.001 for both) and cleaved PARP within stroma, with distant metastases (P=0.005). There was no correlation between the expression of CC3, cleaved PARP or MHC-II in tumour-associated stroma with any standard clinicopathological variables, including stage (Table 2).
Table 2. Univariate analysis of patient and tumour in relationship to active caspase 3 expression in tumour and tumour-associated stroma.
| χ2 test (P value) | ||||||
|---|---|---|---|---|---|---|
| |
CC3 expression | Cleaved PARP | MHC-II expression | |||
| Variable | Tumour | Tumour-associated stroma | Tumour | Tumour-associated stroma | Tumour | Tumour-associated stroma |
| Gender |
0.832 |
0.579 |
0.427 |
0.524 |
0.116 |
0.656 |
| Tumour site |
0.729 |
0.364 |
0.884 |
0.410 |
0.757 |
0.058 |
| Tumour grade |
0.196 |
0.266 |
1.000 |
0.255 |
0.036 |
0.190 |
| Duke's stage |
0.026 |
0.298 |
0.288 |
0.844 |
0.157 |
0.706 |
| TNM stage |
0.047 |
0.462 |
>0.001 |
>0.001 |
0.007 |
0.969 |
| Distant metastases |
0.005 |
0.188 |
1.000 |
0.005 |
0.237 |
0.989 |
| Extramural vascular invasion |
0.775 |
0.368 |
0.392 |
0.604 |
0.249 |
0.049 |
| Stromal MHC-II expression |
0.151 |
0.020 |
0.005 |
0.011 |
— |
— |
| Tumoural MHC-II expression |
0.008 |
0.347 |
0.959 |
1.000 |
— |
— |
| CD3—intratumoural |
0.557 |
0.525 |
0.525 |
0.297 |
0.002 |
0.002 |
| CD3—tumour-associated stroma |
0.821 |
0.569 |
0.569 |
0.651 |
0.001 |
0.001 |
| CD16 |
0.762 |
0.490 |
0.490 |
0.522 |
0.002 |
0.004 |
| CD68 |
0.631 |
0.313 |
0.313 |
1.000 |
0.865 |
<0.001 |
| p53 |
0.616 |
0.919 |
0.919 |
0.379 |
0.069 |
0.394 |
| Bcl-2 |
0.681 |
0.290 |
0.290 |
0.486 |
0.362 |
0.145 |
| CC3 tumour |
— |
0.221 |
>0.001 |
>0.001 |
— |
— |
| CC3 tumour-associated stroma |
0.221 |
— |
0.218 |
>0.001 |
— |
— |
| Cleaved PARP tumour |
— |
— |
— |
>0.001 |
— |
— |
| Cleaved PARP tumour-associated stroma | — | — | >0.001 | — | — | — |
Abbreviations: CC3=cleaved caspase-3; MHC-II=major histocompatibility class II; PARP=poly (ADP-ribose) polymerase; TNM=Tumor, Node, Metastasis. P values <0.05 are indicated in bold.
Relationship between CC3, cleaved PARP and MHC-II expression and markers of immune activation and apoptosis
The immune system, and in particular the presence of T cells, has been shown to have strong prognostic significance in colorectal cancer. IFN-γ, produced by immune cells, has been shown to have a central role in immune surveillance. It induces MHC-II expression on tumour cells and upregulates expression on stromal cells. The relationship between CC3 and MHC-II expression in tumour and tumour-associated stroma and markers of immune activation was therefore measured using the Pearson's χ2 test. Expression of CC3 in the tumour associated significantly with MHC-II expression in tumour cells (P=0.008; Table 2) but not with the number of CD68-, CD16- or CD3-positive cells or Bcl2 or p53. There was no correlation between the expression of CC3 in tumour-associated stroma with the number of CD68-, CD16- or CD3-positive cells or Bcl2 or p53. However, there was a significant correlation with stromal expression of MHC-II (P=0.020; Table 2).
Expression of MHC-II in the tumour associated significantly with the expression of CD3 T cells either within the tumour (P=0.002; Table 2) or within the stroma (P=0.001; Table 2) and the expression of CD16-positive cells (macrophage and NK cells: P=0.002; Table 2) but not with the number of CD68-positive cells or Bcl2 or p53. Expression of MHC-II in the tumour-associated stroma was significantly associated with the expression of CD3 T cells either within the tumour (P=0.002; Table 2) or within the stroma (P=0.001; Table 2), the expression of CD16-positive cells (macrophage and NK cells; P=0.004; Table 2) and with the number of CD68-positive cells (macrophages; P=0.001; Table 2) but not with Bcl2 or p53. No correlation between CC3 or MHC-II in tumour or tumour-associated stroma was observed with microsatellite instability.
Expression of cleaved PARP in the tumour correlated significantly with CC3 within the tumour (P=0.001; Table 2), MHC-II (P=0.005) and CD68 (P=0.001) but not with Bcl2, p53, CD3 or CD16. Expression of PARP in tumour-associated stroma associated significantly with CC3 in the stroma (P=0.001) and with MHC-II in tumour-associated stroma (P=0.011) but not with Bcl2, p53, MHC-II, CD3, CD68 or CD16.
Relationship between CC3, cleaved PARP and MHC-II expression and survival
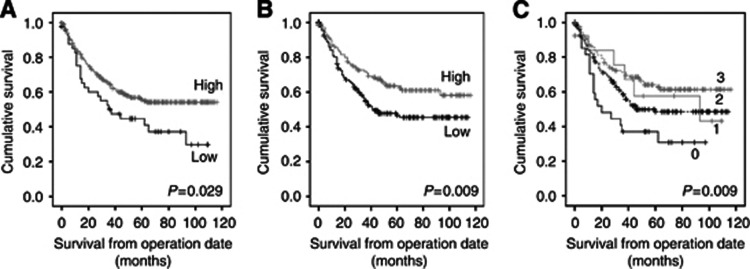
Kaplan–Meier plots were used to analyse the relationship between the expression of CC3, cleaved PARP and MHC-II with DSS. Figure 2A and Table 3 demonstrate that patients with a higher level of tumour CC3 expression have a greater mean survival (P=0.029; 73 months) than those with a lower level of CC3 expression (53 months). This is echoed in tumour-associated stroma with a higher expression having a greater mean survival (P=0.009, 79 mean months vs 63 months; Figure 2B). When tumour cell expression of CC3 cells was compared with tumour-associated stromal cell expression, patients who showed low CC3 expression in tumour and tumour-associated stroma had the worst survival (43 months), whereas patients with high CC3 expression in tumour and tumour-associated stroma displayed the best survival (80 months; P=0.009). Patients with high tumour and low tumour-associated stromal CC3 expression or patients with low tumour and high tumour-associated stromal CC3 expression had similar survival rates (66 and 71 months, respectively; Figure 2C).
Figure 2.
Kaplan–Meier plot for disease-specific survival relative to CC3.(A) Low CC3 expression in tumour cells (Low) vs high CC3 expression in tumour cells (High; P=0.029). (B) Low CC3 expression in tumour-associated stroma (Low) vs high CC3 high expression in tumour-associated stroma (High; P=0.009). (C) Groups of low CC3 expression in both tumour and tumour-associated stroma (0), low CC3 expression in tumour, high expression in tumour-associated stroma (1), high CC3 expression in tumour, low expression in tumour-associated stroma (2) and high CC3 expression in both tumour and tumour-associated stroma (3); P=0.009. Where tumour low/high=0–60/61–max cells mm−2 and tumour-associated stroma low/high=0–104/105–max cells mm−2.
Table 3. Mean survival of patients.
| Marker | Level of expression | Mean survival (months) |
|---|---|---|
|
CC3 | ||
|
Tumour | ||
| |
Low |
53 |
| |
High |
73 |
| |
Tumour-associated stroma |
|
| |
Low |
63 |
| |
High |
79 |
| |
Tumour
vs
tumour-associated stroma |
|
| |
Low tumour/low tumour-associated stroma (0) |
43 |
| |
Low tumour/high tumour-associated stroma (1) |
71 |
| |
High tumour/low tumour-associated stroma (2) |
66 |
| |
High tumour/high tumour-associated stroma (3) |
80 |
|
MHC-II | ||
|
Tumour | ||
| |
Negative |
71 |
| |
Positive |
85 |
| |
Tumour-associated stroma |
|
| |
Negative |
69 |
| |
Positive |
75 |
|
Cleaved PARP | ||
|
Tumour | ||
| |
Low |
70 |
| |
High |
79 |
| |
Tumour-associated stroma |
|
| |
Low |
69 |
| High | 84 | |
Abbreviations: CC3=cleaved caspase-3; MHC-II=major histocompatibility class II; PARP=poly (ADP-ribose) polymerase.
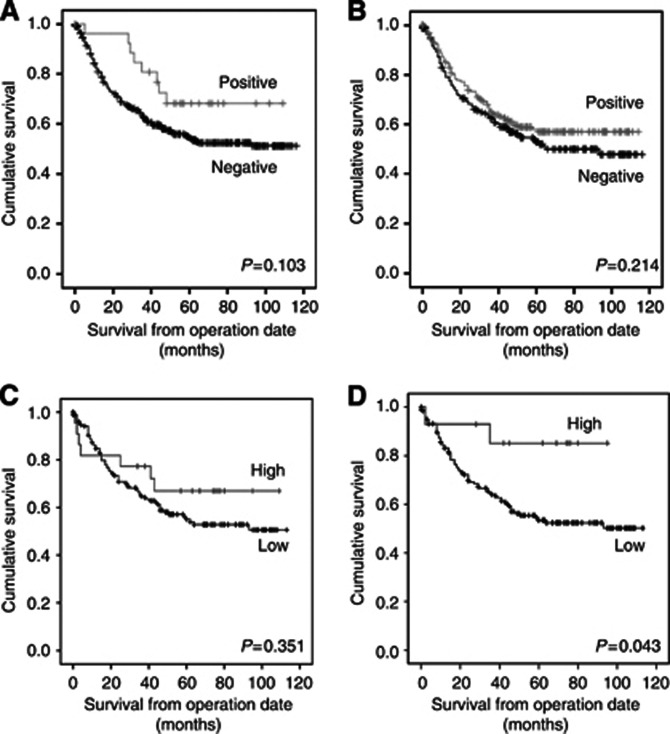
To confirm that the improved prognosis with high levels of CC3 related to active caspase 3 and apoptosis, cleaved PARP was measured and correlated with DSS. Although not significant (P=0.351; Figure 3C, Table 3) levels of cleaved PARP in the tumour showed a similar trend to CC3 expression, with patients with higher levels of cleaved PARP having an improved prognosis. As with CC3 expression, patients with high levels of cleaved PARP in tumour-associated stroma had a significantly (P=0.043; Figure 3D, Table 3) better survival than patients with low levels of cleaved PARP in tumour-associated stroma (survival of 84 and 69 months, respectively).
Figure 3.
Kaplan–Meier plot for disease-specific survival relative to MHC-II and cleaved PARP.(A) MHC-II-negative expression in tumour cells (Negative) vs MHC-II-positive expression in tumour cells (Positive; P=0.103). (B) Negative MHC-II expression in tumour-associated stroma (Negative) vs positive MHC-II expression in tumour-associated stroma (Positive; P=0.214). (C) Low cleaved PARP expression in tumour cells (Low) vs high cleaved PARP expression in tumour cells (High; P=0.315). (D) Low cleaved PARP expression in tumour-associated stroma (Low) vs high cleaved PARP expression in tumour-associated stroma (High; P=0.043).
A sub-analysis of colon vs rectal cancer cases revealed that the survival advantage was predominantly in the rectal cancer group, with high expression of CC3 in either the tumour (P=0.026) or tumour-associated stroma (P=0.01) correlating with a good prognosis (data not shown). By contrast, most of the colonic tumours had low CC3 levels. This may have been related to pre-operative radiotherapy for rectal cancer but 13 out of 181 rectal tumours were irradiated in this historic series of rectal tumours. If the irradiated tumours were excluded, the high expression of CC3 in rectal tumour-associated stroma still correlated with good prognosis (P=0.007); however, the high expression of CC3 in colorectal tumour, although showing the same trend, just failed to reach significance (P=0.064).
Figures 3C and D and Table 3 demonstrate that the level of MHC-II expression in either the tumour or tumour-associated stromal cells had no significant influence on patient survival (P=0.103 and 0.214).
Multivariate analysis of CC3 expression and standard clinicopathological variables
In order to determine the relative influences of CC3 and cleaved PARP and other variables known to affect prognosis, a multivariate analysis was performed using the Cox's proportional hazards model. The variables included were those that have been shown to be significantly related to DSS on univariate analysis (extramural vascular invasion and TNM stage). In combination with CC3, cleaved PARP and MHC-II in both the tumour and stroma, only TNM stage (95% CI 1.496–4.196; P>0.001) and low expression of CC3 in tumour-associated stroma (95% CI 0.229–1.003, P=0.05) retained independent prognostic significance (Table 4A). Previous studies in our group have shown that both the presence of intratumoural T cells and reduced MHC-I expression are independent prognostic factors (Simpson et al, 2010). Multivariate analysis was therefore performed to see whether tumour-associated stroma CC3 expression was independent of these factors and TMN stage and vascular invasion. Analysis showed that only tumour-associated stroma CC3 expression (P=0.005) and TNM stage (P<0.001) retained their independent prognostic significance (Table 4B).
Table 4. Cox multivariate regression analysis of variables in relation to disease-specific survival.
| (A) | |||
|---|---|---|---|
| Variable | Hazard ratio | 95% CI | P value |
|
Vascular invasion status | |||
| Negative | 1 | ||
| Positive |
1.191 |
0.764–2.885 |
0.244 |
|
TNM stage | |||
| 0–II | 1 | ||
| III–IV |
2.506 |
1.496–4.196 |
<0.001 |
|
CC3 tumour | |||
| Low | 1 | ||
| High |
0.808 |
0.341–1.917 |
0.629 |
|
CC3 tumour-associated stroma expression | |||
| Low | 1 | ||
| High |
0.479 |
0.229–1.003 |
0.051 |
|
Cleaved PARP tumour | |||
| Low | 1 | ||
| High |
1.205 |
0.394–3.687 |
0.744 |
|
Cleaved PARP tumour-associated stroma expression | |||
| Low | 1 | ||
| High |
0 |
0 |
0.975 |
|
MHC-II tumour | |||
| Negative | 1 | ||
| Positive |
0.464 |
0.104–2.079 |
0.315 |
|
MHC-II tumour-associated stroma expression | |||
| Negative | 1 | ||
| Positive |
1.110 |
0.716–1.722 |
0.640 |
| (B) | |||
|
Vascular invasion status | |||
| Negative | 1 | ||
| Positive |
0.638 |
0.394–1.034 |
0.068 |
|
TNM stage | |||
| 0–II | 1 | ||
| III–IV |
3.733 |
2.141–6.506 |
<0.001 |
|
ITTC | |||
| Low | 1 | ||
| High |
1.310 |
0.825–2.080 |
0.253 |
|
MHC-I | |||
| Low | 1 | ||
| High |
0.549 |
0.219–1.376 |
0.201 |
|
CC3 tumour-associated stroma expression | |||
| Low | 1 | ||
| High | 0.490 | 0.299–0.804 | 0.005 |
Abbreviations: CC3=cleaved caspase-3; CI=confidence interval; ITTC=intratumoural T cells; MHC=major histocompatibility class ; PARP=poly (ADP-ribose) polymerase; TNM=Tumor, Node, Metastasis.
Discussion
Cancer involves a complex interaction between tumour cells, surrounding stromal cells and immune cells. Perturbation of this complex relationship can lead to tumour cell apoptosis. However, resistance to apoptosis has been shown to be a key factor in tumour progression.
It may be logical to consider that higher levels of apoptosis in a tumour could lead to a better prognosis. However, the properties of apoptotic cells and their ability to affect the inflammatory nature of the tumour microenvironment can also provide a drive towards tumourigenesis (Gregory and Pound, 2010). This, and contradictory results from previous studies, means the value of apoptosis as a prognostic marker remains unclear (Koornstra et al, 2003). The majority of early studies used transferase-mediated nick end labelling (TUNEL) to detect fragmented DNA in apoptotic cells. The TUNEL method has two main disadvantages: first the labelling of DNA fragments also marks necrotic and autolytic cells (Gown and Willingham, 2002), and second, the method requires pre-treatment steps, which can be a source of variation between studies.
In this study, we have shown that high levels of CC3 both within tumour and surrounding stromal cells correlates with good prognosis. Furthermore, CC3 expression within stromal cells was an independent prognostic marker. These findings are in concurrence with other studies. A low level of CC3 activity in the tumour correlated with a greater risk of recurrence in 117 stage III rectal cancer patients (de Heer et al, 2007). A lower level of caspase-3 activation, measured by western blots, in the tumours of 60 colorectal cancer patients significantly correlated with a greater risk of recurrence (Jonges et al, 2001). Increase in caspase-3 activity with cancer progression has also been suggested (Leonardos et al, 1999). In their study, Koelink et al (2009) measured the caspase-3-degraded antigen M30 and found that a greater than median level of caspase activity in tumour-associated stroma correlated with increased survival in 211 colorectal cancer patients (Koelink et al, 2009). Procaspase 3 can be cleaved by proteases such as calpains that generate similar cleavage products but which do not activate caspase 3 (Blomgren et al, 2001). To determine whether the CC3 measured was active caspase, we also stained for cleavage of a caspase 3 substrate PARP. The level of PARP cleavage was lower than CC3, suggesting that perhaps some of the CC3 cleavage was related to other protease activity. However, there was a strong correlation between the two products, suggesting that there was a correlation with apoptosis. Furthermore, high cleaved PARP within tumour stroma also correlated with a good prognosis.
In our study, we also found that CC3 expression in the tumour and tumour-associated stroma correlates with the level of MHC-II. This may be related to the expression of IFN-γ as this is the only agent that can upregulate expression of MHC-II on epithelial cells (Giroux et al, 2003). It has been shown that transformation induces stress-related molecules, which are recognised by innate immune cells with the subsequent release of IFN-γ (Dunn et al, 2005). The strong correlation between MHC-II on tumours and CD3, CD16 and CD68 expression suggests that IFN-γ may be produced by T cells, NK cells and M1 macrophages. The correlation between CC3 and MHC-II suggests that IFN-γ may be responsible for some of the tumour cell apoptosis and good prognosis. This is supported by previous studies showing that the stress-related protein MICA (Watson et al, 2006b) and intratumoural T cells are markers of good prognosis in colorectal cancer (Simpson et al, 2010). Although 73% of the MHC-II-positive tumours and tumour-associated stroma expressed high levels of CC3/cleaved PARP, there were many tumours with high levels of apoptosis that did not express MHC-II suggesting other factors were key drivers of apoptosis in these tumours.
Cancer-associated fibroblasts have been shown to facilitate colorectal tumour progression by secreting growth factors and proteases that stimulate tumour growth, migration and angiogenesis (Olumi et al, 1999; Adegboyega et al, 2002; Tsujino et al, 2007; Schoppmann et al, 2012; Servais and Erez, 2013). More recent studies have suggested that stromal and tumour cells co-operate to promote each other's survival (Lisanti et al, 2010; Balliet et al, 2011). Thus, cancers that express low levels of CC3 in both the tumour itself and its associated stroma are most aggressive and lead to a poor prognosis (median survival 43 months). However, if the tumour grows too rapidly, it could compete with the stroma for nutrients and oxygen resulting in stromal death and consequently tumour death. Thus, tumours with high CC3 levels in both their tumour and stroma have less aggressive tumours and better prognosis (median survival 80 months).
The independent significance of apoptosis in tumour-associated stroma in colorectal cancer suggests that tumour microenvironment-targeted therapy may be beneficial. The anti-VEGFA mAb bevacizumab is approved for treatment of colorectal cancer (Van Meter and Kim, 2010) and the DNA vaccine targeted at the cancer-associated fibroblast marker fibroblast-activation protein has shown promising results in a murine model (Wen et al, 2010).
In conclusion, our study has shown that high expression of CC3 in tumours correlates with good prognosis. High expression of CC3 in tumour-associated stroma also resulted in good prognosis and is an independent prognostic factor in colorectal cancer. This may be because apoptosis in the tumour-associated stroma reduces tumour-promoting signals and therefore limits cancer progression. This study further highlights the importance of tumour-associated stroma in colorectal cancer as a possible new therapeutic target.
Acknowledgments
We are grateful for funding from the MRC and Lewis Trust.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Material
References
- Adegboyega PA, Mifflin RC, DiMari JF, Saada JI, Powell DW. Immunohistochemical study of myofibroblasts in normal colonic mucosa, hyperplastic polyps, and adenomatous colorectal polyps. Arch Pathol Lab Med. 2002;126 (7:829–836. doi: 10.5858/2002-126-0829-ISOMIN. [DOI] [PubMed] [Google Scholar]
- Balliet RM, Capparelli C, Guido C, Pestell TG, Martinez-Outschoorn UE, Lin Z, Whitaker-Menezes D, Chiavarina B, Pestell RG, Howell A, Sotgia F, Lisanti MP. Mitochondrial oxidative stress in cancer-associated fibroblasts drives lactate production, promoting breast cancer tumor growth: understanding the aging and cancer connection. Cell Cycle. 2011;10 (23:4065–4073. doi: 10.4161/cc.10.23.18254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blomgren K, Zhu C, Wang X, Karlsson JO, Leverin AL, Bahr BA, Mallard C, Hagberg H. Synergistic activation of caspase-3 by mm-calpain after neonatal hypoxia-ischemia: a mechanism of ‘pathological apoptosis'. J.Biol Chem. 2001;276 (130:10191–10198. doi: 10.1074/jbc.M007807200. [DOI] [PubMed] [Google Scholar]
- Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10 (21:7252–7259. doi: 10.1158/1078-0432.CCR-04-0713. [DOI] [PubMed] [Google Scholar]
- Cheong JW, Chong SY, Kim JY, Eom JI, Jeung HK, Maeng HY, Lee ST, Min YH. Induction of apoptosis by apicidin, a histone deacetylase inhibitor, via the activation of mitochondria-dependent caspase cascades in human Bcr-Abl-positive leukemia cells. Clin Cancer Res. 2003;9 (13:5018–5027. [PubMed] [Google Scholar]
- de Heer P, de Bruin EC, Klein-Kranenbarg E, Aalbers RI, Marijnen CA, Putter H, de Bont HJ, Nagelkerke JF, van Krieken JH, Verspaget HW, van de Velde CJ, Kuppen PJ. Caspase-3 activity predicts local recurrence in rectal cancer. Clin Cancer Res. 2007;13 (19:5810–5815. doi: 10.1158/1078-0432.CCR-07-0343. [DOI] [PubMed] [Google Scholar]
- Duncan TJ, Watson NF, Al-Attar AH, Scholefield JH, Durrant LG. The role of MUC1 and MUC3 in the biology and prognosis of colorectal cancer. World J Surg Oncol. 2007;5:31. doi: 10.1186/1477-7819-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn GP, Bruce AT, Sheehan KC, Shankaran V, Uppaluri R, Bui JD, Diamond MS, Koebel CM, Arthur C, White JM, Schreiber RD. A critical function for type I interferons in cancer immunoediting. Nat Immunol. 2005;6 (7:722–729. doi: 10.1038/ni1213. [DOI] [PubMed] [Google Scholar]
- Durrant LG, Chapman MA, Buckley DJ, Spendlove I, Robins RA, Armitage NC. Enhanced expression of the complement regulatory protein CD55 predicts a poor prognosis in colorectal cancer patients. Cancer Immunol Immunother. 2003;52 (10:638–642. doi: 10.1007/s00262-003-0402-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer MJ, MacFarlane M, Cohen GM. Barriers to effective TRAIL-targeted therapy of malignancy. J Clin Oncol. 2007;25 (28:4505–4506. doi: 10.1200/JCO.2007.13.1011. [DOI] [PubMed] [Google Scholar]
- Garnier P, Ying W, Swanson RA. Ischemic preconditioning by caspase cleavage of poly(ADP-ribose) polymerase-1. J Neurosci. 2003;23 (22:7967–7973. doi: 10.1523/JNEUROSCI.23-22-07967.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giroux M, Schmidt M, Descoteaux A. IFN-gamma-induced MHC class II expression: transactivation of class II transactivator promoter IV by IFN regulatory factor-1 is regulated by protein kinase C-alpha. J Immunol. 2003;171 (8:4187–4194. doi: 10.4049/jimmunol.171.8.4187. [DOI] [PubMed] [Google Scholar]
- Gown AM, Willingham MC. Improved detection of apoptotic cells in archival paraffin sections: immunohistochemistry using antibodies to cleaved caspase 3. J Histochem Cytochem. 2002;50 (4:449–454. doi: 10.1177/002215540205000401. [DOI] [PubMed] [Google Scholar]
- Gregory CD, Pound JD. Microenvironmental influences of apoptosis in vivo and in vitro. Apoptosis. 2010;15 (9:1029–1049. doi: 10.1007/s10495-010-0485-9. [DOI] [PubMed] [Google Scholar]
- Hector S, Prehn JH. Apoptosis signaling proteins as prognostic biomarkers in colorectal cancer: a review. Biochim Biophys Acta. 2009;1795 (2:117–129. doi: 10.1016/j.bbcan.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Jonges LE, Nagelkerke JF, Ensink NG, van der Velde EA, Tollenaar RA, Fleuren GJ, van de Velde CJ, Morreau H, Kuppen PJ. Caspase-3 activity as a prognostic factor in colorectal carcinoma. Lab Invest. 2001;81 (5:681–688. doi: 10.1038/labinvest.3780277. [DOI] [PubMed] [Google Scholar]
- Jordanova ES, Gorter A, Ayachi O, Prins F, Durrant LG, Kenter GG, van der Burg SH, Fleuren GJ. Human leukocyte antigen class I, MHC class I chain-related molecule A, and CD8+/regulatory T-cell ratio: which variable determines survival of cervical cancer patients. Clin Cancer Res. 2008;14 (7:2028–2035. doi: 10.1158/1078-0432.CCR-07-4554. [DOI] [PubMed] [Google Scholar]
- Kakar S, Aksoy S, Burgart LJ, Smyrk TC. Mucinous carcinoma of the colon: correlation of loss of mismatch repair enzymes with clinicopathologic features and survival. Mod Pathol. 2004;17 (6:696–700. doi: 10.1038/modpathol.3800093. [DOI] [PubMed] [Google Scholar]
- Koelink PJ, Sier CF, Hommes DW, Lamers CB, Verspaget HW. Clinical significance of stromal apoptosis in colorectal cancer. Br J Cancer. 2009;101 (5:765–773. doi: 10.1038/sj.bjc.6605220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP. Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med. 1998;4 (7:844–847. doi: 10.1038/nm0798-844. [DOI] [PubMed] [Google Scholar]
- Koornstra JJ, de Jong S, Hollema H, de Vries EG, Kleibeuker JH. Changes in apoptosis during the development of colorectal cancer: a systematic review of the literature. Crit Rev Oncol Hematol. 2003;45 (1:37–53. doi: 10.1016/s1040-8428(01)00228-1. [DOI] [PubMed] [Google Scholar]
- Krajewska M, Kitada S, Winter JN, Variakojis D, Lichtenstein A, Zhai D, Cuddy M, Huang X, Luciano F, Baker CH, Kim H, Shin E, Kennedy S, Olson AH, Badzio A, Jassem J, Meinhold-Heerlein I, Duffy MJ, Schimmer AD, Tsao M, Brown E, Sawyers A, Andreeff M, Mercola D, Krajewski S, Reed JC. Bcl-B expression in human epithelial and nonepithelial malignancies. Clin Cancer Res. 2008;14 (10:3011–3021. doi: 10.1158/1078-0432.CCR-07-1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonardos L, Butler LM, Hewett PJ, Zalewski PD, Cowled PA. The activity of caspase-3-like proteases is elevated during the development of colorectal carcinoma. Cancer Lett. 1999;143 (1:29–35. doi: 10.1016/s0304-3835(99)00176-7. [DOI] [PubMed] [Google Scholar]
- Lisanti MP, Martinez-Outschoorn UE, Chiavarina B, Pavlides S, Whitaker-Menezes D, Tsirigos A, Witkiewicz A, Lin Z, Balliet R, Howell A, Sotgia F. Understanding the ‘lethal' drivers of tumor-stroma co-evolution: emerging role(s) for hypoxia, oxidative stress and autophagy/mitophagy in the tumor micro-environment. Cancer Biol Ther. 2010;10 (6:537–542. doi: 10.4161/cbt.10.6.13370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazelin L, Bernet A, Bonod-Bidaud C, Pays L, Arnaud S, Gespach C, Bredesen DE, Scoazec JY, Mehlen P. Netrin-1 controls colorectal tumorigenesis by regulating apoptosis. Nature. 2004;431 (7004:80–84. doi: 10.1038/nature02788. [DOI] [PubMed] [Google Scholar]
- McGilvray RW, Eagle RA, Watson NF, Al-Attar A, Ball G, Jafferji I, Trowsdale J, Durrant LG. NKG2D ligand expression in human colorectal cancer reveals associations with prognosis and evidence for immunoediting. Clin Cancer Res. 2009;15 (22:6993–7002. doi: 10.1158/1078-0432.CCR-09-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mild G, Bachmann F, Boulay JL, Glatz K, Laffer U, Lowy A, Metzger U, Reuter J, Terracciano L, Herrmann R, Rochlitz C. DCR3 locus is a predictive marker for 5-fluorouracil-based adjuvant chemotherapy in colorectal cancer. Int J Cancer. 2002;102 (3:254–257. doi: 10.1002/ijc.10711. [DOI] [PubMed] [Google Scholar]
- Nausch N, Cerwenka A. NKG2D ligands in tumor immunity. Oncogene. 2008;27 (45:5944–5958. doi: 10.1038/onc.2008.272. [DOI] [PubMed] [Google Scholar]
- NICE . Improving Outcomes in Colorectal Cancers: Manual Update. National Institute for Clinical Excellence: London, UK; 2004. [Google Scholar]
- O'Connell J, Bennett MW, Nally K, Houston A, O'Sullivan GC, Shanahan F.2000Altered mechanisms of apoptosis in colon cancer: Fas resistance and counterattack in the tumor-immune conflict Ann N Y Acad Sci 910178–192.; discussion 193–5 [DOI] [PubMed] [Google Scholar]
- Olumi AF, Grossfeld GD, Hayward SW, Carroll PR, Tlsty TD, Cunha GR. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res. 1999;59 (19:5002–5011. doi: 10.1186/bcr138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel AV, Krimm RF. BDNF is required for the survival of differentiated geniculate ganglion neurons. Dev Biol. 2010;340 (2:419–429. doi: 10.1016/j.ydbio.2010.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn MJBP, Brock A, Kirby EA, Jones J. Stationery Office: London, UK; 2001. Cancer Trends in England and Wales, 1950–1999; pp. 206–207. [Google Scholar]
- Sabine VS, Faratian D, Kirkegaard-Clausen T, Bartlett JM. Validation of activated caspase-3 antibody staining as a marker of apoptosis in breast cancer. Histopathology. 2012;60 (2:369–371. doi: 10.1111/j.1365-2559.2011.04024.x. [DOI] [PubMed] [Google Scholar]
- Schoppmann SF, Berghoff A, Dinhof C, Jakesz R, Gnant M, Dubsky P, Jesch B, Heinzl H, Birner P. Podoplanin-expressing cancer-associated fibroblasts are associated with poor prognosis in invasive breast cancer. Breast Cancer Res Treat. 2012;134 (1:237–244. doi: 10.1007/s10549-012-1984-x. [DOI] [PubMed] [Google Scholar]
- Servais C, Erez N. From sentinel cells to inflammatory culprits: cancer-associated fibroblasts in tumour-related inflammation. J Pathol. 2013;229 (2:198–207. doi: 10.1002/path.4103. [DOI] [PubMed] [Google Scholar]
- Sica A, Larghi P, Mancino A, Rubino L, Porta C, Totaro MG, Rimoldi M, Biswas SK, Allavena P, Mantovani A. Macrophage polarization in tumour progression. Semin Cancer Biol. 2008;18 (5:349–355. doi: 10.1016/j.semcancer.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Simpson JA, Al-Attar A, Watson NF, Scholefield JH, Ilyas M, Durrant LG. Intratumoral T cell infiltration, MHC class I and STAT1 as biomarkers of good prognosis in colorectal cancer. Gut. 2010;59 (7:926–933. doi: 10.1136/gut.2009.194472. [DOI] [PubMed] [Google Scholar]
- Soung YH, Lee JW, Kim SY, Park WS, Nam SW, Lee JY, Yoo NJ, Lee SH. Somatic mutations of CASP3 gene in human cancers. Hum Genet. 2004;115 (2:112–115. doi: 10.1007/s00439-004-1129-3. [DOI] [PubMed] [Google Scholar]
- Thome CH, dos Santos GA, Ferreira GA, Scheucher PS, Izumi C, Leopoldino AM, Simao AM, Ciancaglini P, de Oliveira KT, Chin A, Hanash SM, Falcao RP, Rego EM, Greene LJ, Faca VM. Linker for activation of T-cell family member2 (LAT2) a lipid raft adaptor protein for AKT signaling, is an early mediator of alkylphospholipid anti-leukemic activity. Mol CellProteomics. 2012;11 (12:1898–1912. doi: 10.1074/mcp.M112.019661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsujino T, Seshimo I, Yamamoto H, Ngan CY, Ezumi K, Takemasa I, Ikeda M, Sekimoto M, Matsuura N, Monden M. Stromal myofibroblasts predict disease recurrence for colorectal cancer. Clin Cancer Res. 2007;13 (7:2082–2090. doi: 10.1158/1078-0432.CCR-06-2191. [DOI] [PubMed] [Google Scholar]
- Ullenhag GJ, Mukherjee A, Watson NF, Al-Attar AH, Scholefield JH, Durrant LG. Overexpression of FLIPL is an independent marker of poor prognosis in colorectal cancer patients. Clin Cancer Res. 2007;13 (17:5070–5075. doi: 10.1158/1078-0432.CCR-06-2547. [DOI] [PubMed] [Google Scholar]
- Van Meter ME, Kim ES. Bevacizumab: current updates in treatment. Curr Opin Oncol. 2010;22 (6:586–591. doi: 10.1097/CCO.0b013e32833edc0c. [DOI] [PubMed] [Google Scholar]
- Waldhauer I, Steinle A. NK cells and cancer immunosurveillance. Oncogene. 2008;27 (45:5932–5943. doi: 10.1038/onc.2008.267. [DOI] [PubMed] [Google Scholar]
- Watson NF, Madjd Z, Scrimegour D, Spendlove I, Ellis IO, Scholefield JH, Durrant LG. Evidence that the p53 negative/Bcl-2 positive phenotype is an independent indicator of good prognosis in colorectal cancer: a tissue microarray study of 460 patients. World J Surg Oncol. 2005;3:47. doi: 10.1186/1477-7819-3-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson NF, Ramage JM, Madjd Z, Spendlove I, Ellis IO, Scholefield JH, Durrant LG. Immunosurveillance is active in colorectal cancer as downregulation but not complete loss of MHC class I expression correlates with a poor prognosis. Int J Cancer. 2006a;118 (1:6–10. doi: 10.1002/ijc.21303. [DOI] [PubMed] [Google Scholar]
- Watson NF, Spendlove I, Madjd Z, McGilvray R, Green AR, Ellis IO, Scholefield JH, Durrant LG. Expression of the stress-related MHC class I chain-related protein MICA is an indicator of good prognosis in colorectal cancer patients. Int J Cancer. 2006b;118 (6:1445–1452. doi: 10.1002/ijc.21510. [DOI] [PubMed] [Google Scholar]
- Wen Y, Wang CT, Ma TT, Li ZY, Zhou LN, Mu B, Leng F, Shi HS, Li YO, Wei YQ. Immunotherapy targeting fibroblast activation protein inhibits tumor growth and increases survival in a murine colon cancer model. Cancer Sci. 2010;101 (11:2325–2332. doi: 10.1111/j.1349-7006.2010.01695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SY, Sales KM, Fuller B, Seifalian AM, Winslet MC. Apoptosis and colorectal cancer: implications for therapy. Trends Mol Med. 2009;15 (5:225–233. doi: 10.1016/j.molmed.2009.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.